Delishea’s Stage 4B Classical Hodgkin’s Lymphoma Story
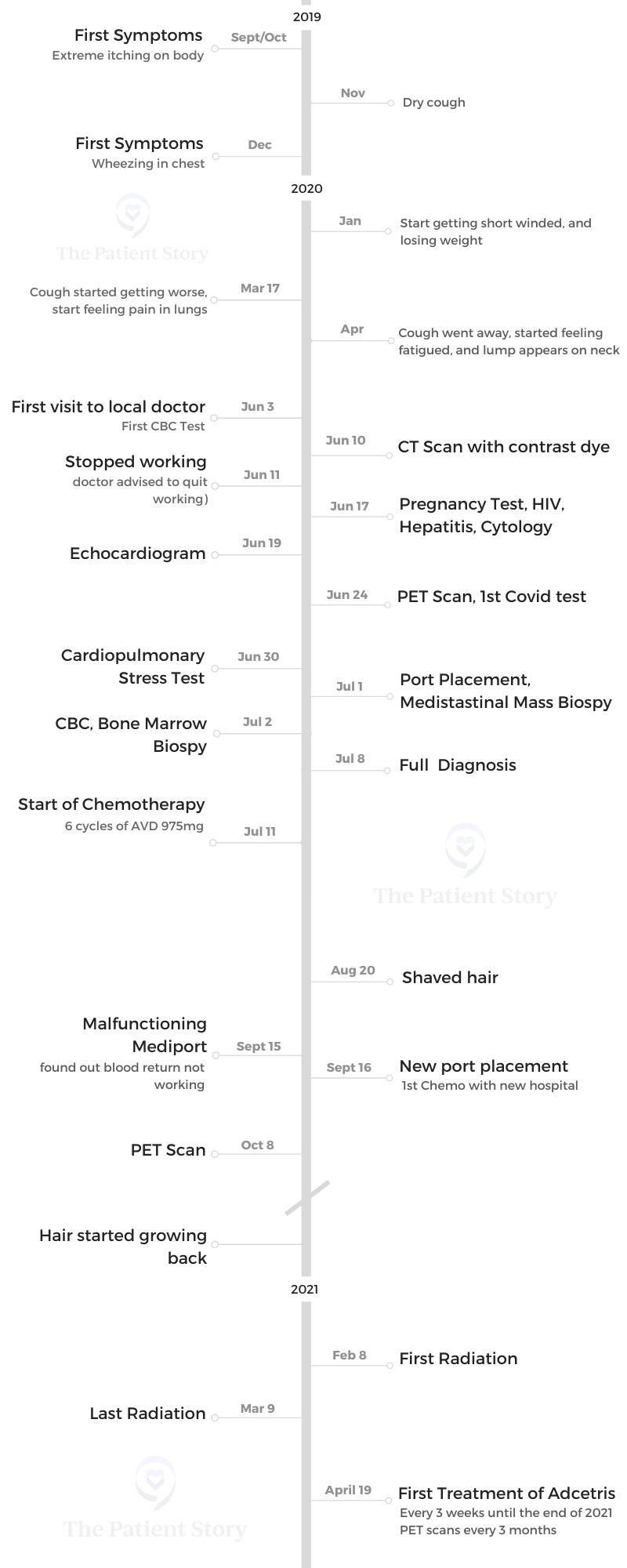
Delishea shares her journey of navigating stage 4B Hodgkin’s Lymphoma — from recognizing her first symptoms, getting diagnosed, undergoing chemotherapy, radiation, and then targeted therapy (brentuximab or Adcetris).
Her story takes us on an inspirational ride from small-town primary care diagnosis to big-city treatment and survivorship.
Read her in-depth story below and watch our conversation on video. Thank you for sharing your story with us, Delishea!

- Name: Delishea A.
- Diagnosis (DX)
- Hodgkin’s Lymphoma
- Stage 4B
- Age at DX
- 30 years old
- 1st Symptoms
- Extreme itching
- Dry cough
- Treatment
- A+AVD chemotherapy (Adcetris + Adriamycin, vinblastine, dacarbazine)
- Radiation
- Targeted therapy (Adcetris)
- Video Segment: Getting Diagnosed
- Life Before Cancer
- Getting Diagnosed
- 1st Symptoms
- First visit to the doctor
- Describing the CT scan
- When did you get your results?
- When did you think it was cancer?
- Describe the PET scan
- Being in a hospital during COVID
- Describe the moment you got the diagnosis
- Breaking the news of cancer and getting chemo
- How was the bone marrow biopsy?
- Hearing the full diagnosis
- Video Segment: Chemo, Radiation & Targeted Therapy
- A + AVD Chemotherapy
- Radiation Therapy
- Targeted Therapy (Brentuximab/Adcetris)
- Video Segment: Survivorship
- Support, Community, and Self-Advocating
- Other Stage 4 Hodgkin's Lymphoma Diagnosis Stories
This interview has been edited for clarity. This is not medical advice. Please consult with your healthcare provider for treatment decisions.
Video Segment: Getting Diagnosed
Life Before Cancer
Tell us a little bit about yourself
I’m Delishea. I’m from down South. I’m a Louisiana girl. There’s not really much to say. I’m a reader. I’m more of a fiction girl. I love stories, and I love pineapples.

Getting Diagnosed
1st Symptoms
I felt that something was seriously wrong, but I constantly tried to make an excuse.
My first symptoms were terrible itchiness, especially on my legs, that I would constantly scratch no matter what I put on there. I thought maybe it was dry skin, dermatitis, or some kind of skin problem.
The second symptom I noticed toward the end of 2019 was having a dry cough — not like a cold, whooping cough. After that, I started having a wheezing sound, which I later found out was because of the fluid from my lungs from the actual tumor.
Then I started getting really tired, fatigued, just really weak, and dizzy. What really brought me to the doctor was the lump on my neck. It’s years of symptoms and ignoring.
»MORE: Read more patient experiences with first symptoms of lymphoma
First visit to the doctor
I live in a small town. I’m so thankful that even though he wasn’t a doctor — he was a nurse practitioner who had his own office — he knew what he was doing.
When he saw where the lump was, he knew and said, “Okay, that’s not in the right spot.” He didn’t tell me he’s suspecting I have cancer. I’m grateful he didn’t make me panic. He said, “I don’t like where it’s at, so we’re gonna get some blood work.”
I got the blood work done the same day. He did a full CBC and tested it for Epstein-Barr. He already suspected what it was, but of course, he did not tell me then because I’m a young girl who’s just so panicked. Then he later scheduled a CT scan.
Describing the CT scan
It’s like in MRI, but they did it with contrast. They put something through your vein, which makes you feel like it burns. You go through the machine that looks like a big donut hole and scan your body.
In that visit, I knew something was wrong with me. I just went in a regular check, but by the end, the nurse asked me 3 times if I have had any kind of X-ray or surgery on my chest.
That’s when I knew that something was wrong, because she asked 3 times. Then I finally asked the X-ray tech, “Can you tell me what was wrong?” But he said he couldn’t.
That day changed my whole life. That was the big day.
When did you get your results?
I got them 9 hours later, but he didn’t give me the full report.
When I was back home, they called me and told me I need to bring somebody with me. They didn’t tell me what I got. I thought, “When they tell you you have to bring somebody with you, something’s up.”
From the partial report, he just wanted to see that I was okay. From the nurse I saw a week before, these reports don’t match up. My right lung was full of fluid, and the mass was huge. It was 17 cm. That’s why he physically wanted to check if I needed to be admitted to a hospital.
He leveled out with me on what we do, what we need to do, what we might need to do. But he said he would move me on to an oncologist.
He called different doctors he knew. Since I live in a small town, the next biggest place was 45 minutes away. He had to make those calls for me to get someone to examine me and tell me what I needed to do next. He was very good on that part.
»MORE: Patients describe dealing with scanxiety and waiting for results
When did you think it was cancer?
When I first came there and in the first exam, I didn’t think anything about cancer. He explained something about the lymphatic system, but I still wasn’t thinking cancer.
During the CT scan that same day, he brought up what looks like cancer — the mass. He initially wanted me to see a pulmonologist because of the mass on the chest, but the doctor told him, “No, you need to send her to an oncologist to look at the CT results.” That’s how I got schedules for it.
We were in shock, my mom and me. I didn’t cry. We sat in the car, and we still didn’t process it. I told my dad later that day, but he didn’t process it until days later.
Describe the PET scan
My first PET scan was very traumatic for me. When you’re in the process of getting diagnosed, you’re going through a whole bunch of tests. At that point, I had fluid in my lungs, so I was in pain.
The PET scan is like a CT scan, going through a hole. It looks the same for me, but with a PET scan, you have to sit an hour before. They have to do something with you. A fluid has to sit in you, and before you get the test, they make you go to the bathroom and pass urine.
The test itself is short. That was like 10 minutes. It’s the waiting before that is not, just like in a CT, but depending on if they do full body. I think they did skull to mid-thigh. I can’t remember. I had huge anxiety from it.
But once I went in, I cried because I was in so much pain. I was coughing a lot.
Being in a hospital during COVID
You will basically be by yourself while doing all these procedures. Your loved ones will just have to sit outside and wait for you. It was huge anxiety.
It was the worst time to be in a hospital.
Describe the moment you got the diagnosis
In my first hospital, there wasn’t a lot of communication. There were just so many tests that were bad. I had 2 procedures in 2 days in a row that I was under anesthesia and sedation.
They didn’t say yet what stage I was at. I got the port before they told me the complete staging.
They said, ‘You have a good cancer. It can be treated.’ But to me, cancer is cancer.
That’s the first thing I heard when my previous oncologist told me the diagnosis. “You’re young. It can be treated. You can do chemo.”
What was really traumatizing that not really a lot of people here talk about is not being able to have children later on. That’s one of the first things they told me. They just told me, “After this, you won’t be able to have kids. Here are the papers. Sign. You need this treatment.”
They tried to explain what it was, but I learned more about it through research, looking at things on my own, and explaining to my family because I wasn’t really getting a full explanation from the doctors.
»MORE: Patients share how they processed a cancer diagnosis
Breaking the news of cancer and getting chemo
I’m a very private person, but I was at the point where I didn’t mind people knowing. I didn’t want people to just check on me and be nosy.
Most people that knew about it were close family — like my mom, who was the patient advocate, my sister, dad, brother, and my aunt, who stayed to help in the house. If they told other people, I didn’t mind, but they respected my privacy.
Later on, when they found out, they were like, “Why didn’t you say anything?” But I’m like, “I don’t know. It’s a weird thing to bring up.”
»MORE: Breaking the news of a diagnosis to loved ones
How was the bone marrow biopsy?
It was hard because mine was back to back with another test, and I was still full of fluid in my lung.
When I think of bone marrow biopsy, I picture how I’ve seen it on TV, where they put this huge needle in, and you’re gonna feel it. I didn’t think you’re going to feel numb. Maybe that was just me watching too much TV.
It was actually not a bad experience. I didn’t feel anything like drilling in the needle or scraping the needle. It’s weird that you saw them put in something there, but you didn’t actually feel it. The actual tap wasn’t painful at all. It was just uncomfortable because I still have fluid on my lungs, but then I have to lay in there and be in the right position.

Hearing the full diagnosis
I found out that I had stage 4. That day, they actually told me, and then I found out on the phone that it spread a little bit.
That was the first time I actually cried. In my mind, I know nothing about cancer, but I hear stage 4, that it spread a little bit somewhere else, and I automatically think negative. That was big deal.
That’s when I really came into terms with, “Okay, I have cancer.”
I had a good attitude. I wanted to get the test and know what it was. You’d want them to have the answers right then and there.
Because when you don’t have the clarity of what it is, it’s a huge anxiety.
I had my family with me; my mom didn’t want me to be alone. My sister and aunt consoled me, and that was a huge thing.
Video Segment: Chemo, Radiation & Targeted Therapy

A + AVD Chemotherapy
Editor’s note: This is different than the ABVD chemotherapy regimen.
- Adcetris (brentixumab)
- Adriamycin (doxorubicin)
- Vinblastine
- Dacarbazine
How was the treatment described to you?
There wasn’t much communication. When I was in the chemo room, that’s when I asked, “What is this? What are you putting in me?”
What I really remember is the red kind, the “Red Devil.” That’s the one I remember the most, and that brought me to researching my treatment.
It was so nerve-wracking because you will use the bathroom prior to treatment, and in just a matter of hours, it becomes like that. I dread it because you’ll know there are other people getting treatment in the room and were in the same bathroom.
Your smell sensor also becomes so strong.
When you go through that process, you just want to do whatever it takes to get better — just give me whatever. Now I wish I took the time to research more and ask more questions.
Chemotherapy regimen
They gave me A+AVD, plus steroids. They also gave me Benadryl. [It was] 6 cycles, every 2 weeks.
When I first started out, it was on Fridays. Then when I changed doctors, it was every other Monday of about 3 and a half hours of treatment.
For my first doctor, we did pregnancy tests before I could receive the treatment. Later on when I moved to the other doctors, I had to get blood work and see my doctor before each treatment.
I moved to a new doctor because of the hurricane damage. It was actually a blessing in disguise because I moved to a better doctor in a bigger area, and they had a better treatment resource.
The whole experience got better for me.
Things that I wasn’t used to, even the small stuff — like having heated blankets, snacks, and drinks — was important.

Why is it important to a patient to have small comforts from home?
You want to feel comfortable through the process, because it’s long. You’ll be sitting there for hours. For some people, it might go shorter, but that’s still hours of you having something running through you.
For me, it felt very uncomfortable. It makes you feel kind of icky because you can smell the chemicals.
Sometimes the medicines can make you sleepy, but it’s the best sleep you’ll get. No one talks about the sleep disturbance sometimes at night, so at least you get your good sleep during the chemo.
Just being comfortable and making sure you have the snacks and drinks and whatever makes you feel like you’re just not alone — these things matter. The nurses are caring and attentive. I had nurses that would ask, “Do you want something? A snack? Do you want a drink?”
Those are little things that matter because it makes you not dread the thought of going to the hospital.
What makes a good doctor?
My oncologist and my radiology doctors were wonderful. They explain even the smallest things, things that you think are stupid, or just common sense questions. They stop and explain their care. They ask things about you as a person, like, “How are you doing?”
I know my doctor here was very attentive. He asked how things were back at home. He knew what I went through each visit. That’s a huge thing.
The huge difference is making you feel they care [by] explaining things to you, breaking it down, and not making you feel like it is a dumb question.

Describe the side effects
Sometimes you get the best sleep during the chemo, but I feel very tired during sessions.
Afterwards, that’s when I get my first meal. Before I could feel any of the effects, nausea, or anything kick in later, I’ll get a nice sit-down dinner. We would sit down and eat dinner and make sure I have something filling me, because steroids make you nauseous.
Some of the side effects for me were weight gain, fatigue, and my appetite kicking in. I crave carbs and sweets, which is frustrating because they tell you the opposite. You have to eat healthy, but the steroids makes you crave the worst thing.
I also had joint pains for my back, maybe because you’re not moving as much as you used to. You’re sleeping more; you’re lying down more.
Neuropathy is something I’m still dealing with today. Just a lot of other things, hair loss, the scratching, the itching that went away after my first treatment, the fluid on my lungs that eventually went away.
I did have problems with constipation and nausea, but it was a weird feeling. If I didn’t eat, it made me want to eat more. If I didn’t eat or if I ate too little, I get nauseous. If I ate too much, I get nauseated. It’s like I had to eat something, or I just feel very weak.

They also gave me Neupogen, which had other side effects, too. It can cause constipation, stomach ache, can cause problems with your kidneys. I didn’t experience any of that.
I try to stay hydrated, so none of that happened a lot. I was scared of that, so I made sure I was hydrated and made sure I was flushing it out days after chemo by drinking water.
Eating healthy during treatment
I changed the way I ate. Before, I would skip breakfast before all this happened. During the treatment, I will eat a huge breakfast, with eggs, toast, and fruit smoothie drink. I always made sure that it would have some protein in it, like eggs, fruit, and veggies.

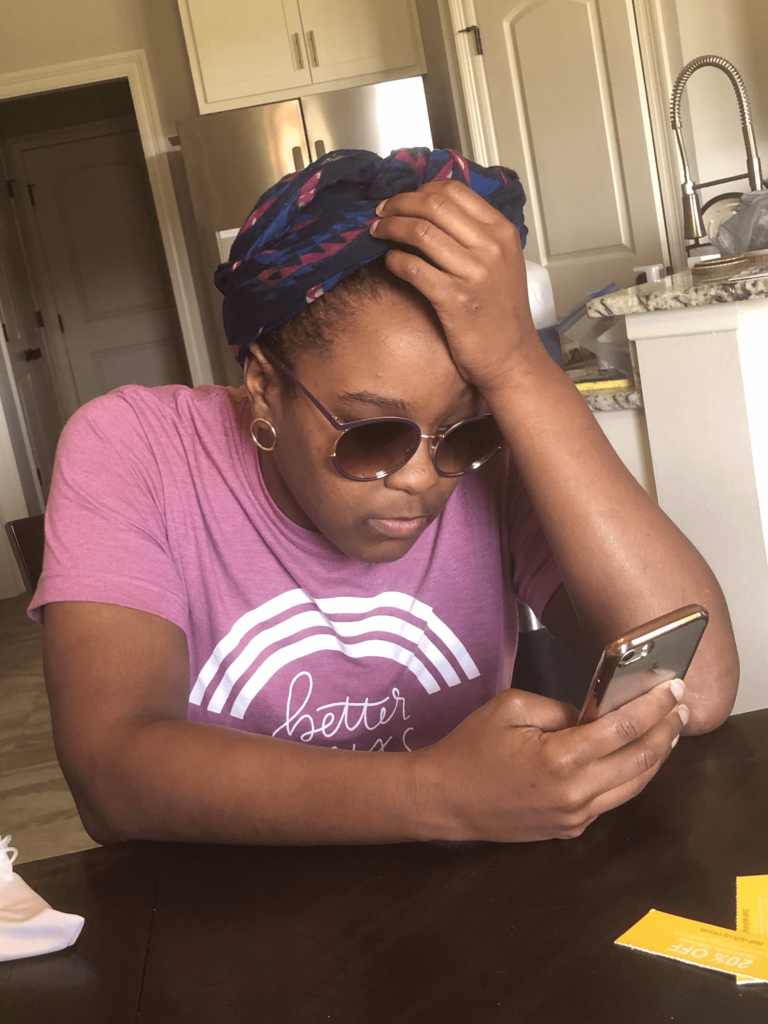
How did you deal with hair loss?
For me, it wasn’t a heritage. I hear some people say that it was very emotional, but for me, it wasn’t. I just didn’t want to see my family see it fall. I wanted to protect them from seeing that part, but they saw it anyways.
I had my hair in little twist locks. When it was time for me to wash my hair and undo the locks, it kept tangling. My mom kept asking me, “Do you want me to do your hair?” I said no, because I wanted to protect her from seeing that. That’s my mom, and I know my mom.
She did my hair. Finally, it was pulling from the roots. She stopped and asked, “Do you have to go ahead and shave it all off?” I’m lucky that our brother is a barber, so he knew how to cut hair.
I really didn’t want him to do it then. I wanted him to do it at the shop when nobody was there, but I needed it done then. My hair was falling, and I didn’t want to see it on my pillows or wake up to it. He shaved it all off, and then it wasn’t too bad for me because I actually started growing it back before treatment even ended.
I was very blessed. I asked my doctor about it and if it is normal to see your hair go back before treatment ends.
I wasn’t too attached, but I can say now presently, if I did lose it again from just the treatment I’m on now, then I think I will cry. I’ll be emotional about it because I’ve seen it grow back.
Tests in between treatments
Our place went through a hurricane, and that period affected my treatment. I had to do it over a long period of time, kind of delayed. Each one of my PET scans was pretty good. They showed the chemo is working. Everything’s working. I don’t know the exact size, though.
A possibility of radiation was discussed before the last PET scan. It wasn’t concrete yet. The doctor wanted to see first, but after the last PET scan, he said we would do radiation. Then that’s when he sent me to the radiology.
Radiation Therapy
Describe the radiation sessions
I had to do 20 sessions in 4 weeks. That was 5 days a week, and I got grade 35. It’s not a lot compared to other cancers and targeted radiation.
The process was fairly easy. They mold you, which was fun because they make a mold of you like in Play-Doh. From there, they would adjust the mold to really suit you. That’s what you laid in each day. You have to align up to those measurements each day to get a great targeted spot that they need for radiation.
Because they were targeting my chest, it had to be open and bare. Other than that, they made it really comfortable.
We listened to music, whatever music you want to listen to that day. Then you just let them do their thing. I really don’t have to do anything. They move you. You just come in, lay down, and listen to music.
Each session was about 10 minutes. Then, of course, there’s time to check-in, undress, and do all these things. Since they were doing my chest area, I just leave my pants on. They already have gowns in your dressing room. Overall, you spent an hour there.
What makes it longer is if they have to adjust you and your measurements. They might have to move you around to get that right area, because they have to make sure it’s right before the radiation and that computer start.
They try to make you feel comfortable so you don’t dread it. I’m doing it 5 days a week. I had a wonderful team, and I didn’t dread going. I really enjoyed them.
Radiation side effects
I did not feel any side effects during the process, but it came after treatment.
It is like getting sunburned inside. It’s not a great feeling because you can’t drink, you can’t eat, and it hurts like a cat clawing inside your throat. All they can do is make you comfortable.
I took aloe vera juice. They call it miracle mouthwash mix. Other than that, I can’t really do anything. I couldn’t eat anything. It was dreadful. Even water hurts to drink, and it lasted for about a week.
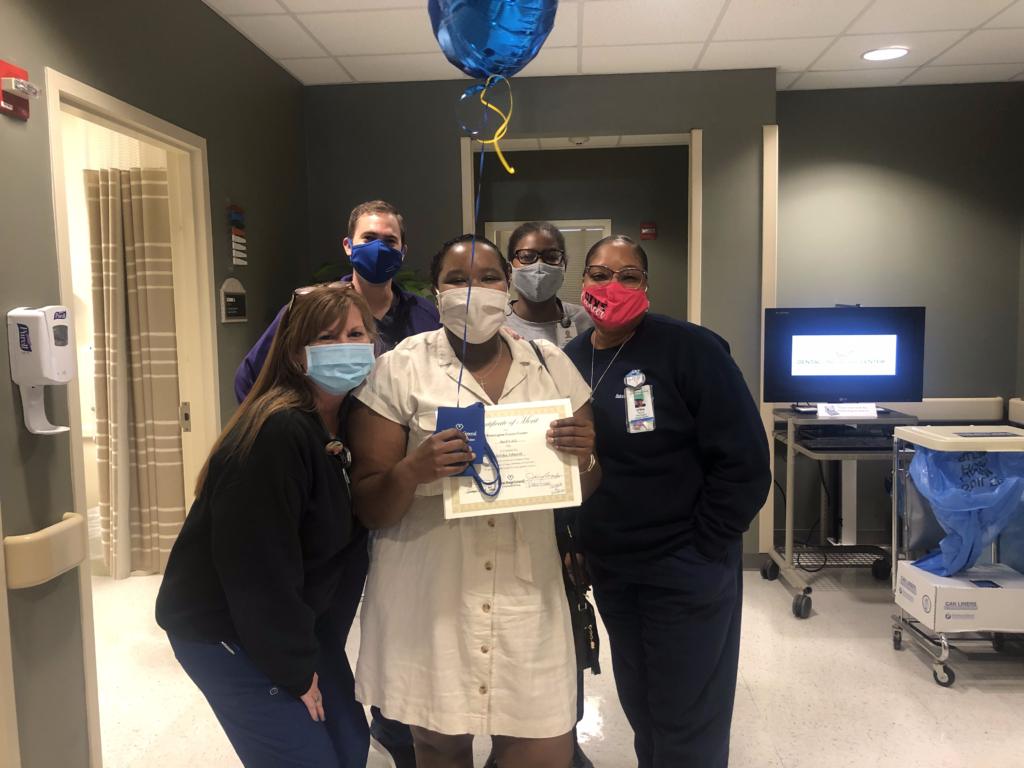
What it meant for you to finish radiation and to have support around you
That last day was such a wonderful day because they took the time out to make me feel special, like it was your birthday or something, because it was a good day.
The team was wonderful. They were caring, especially because I was going through it at a very young age. I didn’t see anyone younger, which is a good thing. Overall, it was a really good experience and a good feeling.
»MORE: Read other patient experiences with radiation therapy
Targeted Therapy (Brentuximab/Adcetris)

Adcetris treatment
It’s a targeted therapy. It’s given through infusion, so it was given through your port.
When you get chemo, chemo kills all cells, but this kills just the bad cancer cells.
It doesn’t really have any side effects so far. I just noticed some neuropathy on my fingers and my feet.
There’s a possibility of fatigue, hair loss, and all that, the same as chemo, but I haven’t experienced anything else so far. I get it every 3 weeks for 30 minutes, for 6 months to a year. I don’t know if it’s going to be until the end of the year.
How do you feel with the progress so far?
My progress has been going pretty well. I’ve had a PET scan at the beginning of the year, and from the end of the radiation, I had a CT scan.
My tumor has shrunk just from the radiation. I have one coming up in June, and we’ll see if it still feels strong. The doctor really wants to get it to a point where it’s steady — not growing, no activity, no nothing — to where they can just monitor me, and I won’t have to come in.
They just want to get me to a point where they can fully say that they treated it, because this cancer, like they said, is treatable.
They just want to make sure they do whatever possible before they let me go a little bit.
»MORE: Read more patient experiences with targeted therapy
Video Segment: Survivorship
Support, Community, and Self-Advocating
Describe how you helped protect your mental health throughout all of this
For me, it was my faith. It was just having faith. I believe in God. I’m a Christian, and that kept me steady, to not go over the edge and get to that deep hole. Sometimes your thoughts can lead to the end, but it was just about taking it day by day.

My faith and the really good support that I had helped me through.
Having people that surround you and love you and keep you grounded really helped a lot.
Importance of caregivers
My caregiver is my sister. From the beginning, it was my mom and my dad. They were a big help from the very beginning.
My mom, being a big mama bear, wanted to take me to all my treatments. She wanted to do everything, so I had to tell her to take a step back and make sure her health is okay.
Once I moved doctors, I stayed with my sister, who actually stays in the same area. I’m with her all the time. I didn’t have to worry about traveling or staying in hotels to be able to attend treatments.
Participating in clinical trials
My doctor had the option to give me something stronger, but he didn’t want to exhaust all the options out on this one time. Just in case it comes back later on, I have option 2 and 3.
That’s one of the reasons why he wanted to do the scan, to make sure it’s treated and gone and never comes back. I think clinical trials are very important.
If I ever get to that point where they didn’t have any other option, I would be open to doing it. Whenever I can, whatever I can, to be cured and treated — or if not cured, in remission again.
»MORE: Read more on FDA approvals of clinical trials
Getting treatment from small and big hospitals
It’s a big question of health care, like health insurance.
Before I got sick, before 2020 and the pandemic, or before we were in a stay-at-home order, I didn’t have any health insurance. It was because my job didn’t provide good health insurance. When I got laid off (I did get laid off during the process), my mom convinced me to get Medicaid.
Being a millennial, thinking that we’re going to just be gone 2 weeks, I didn’t want to, but then I just did what she said.
I didn’t think I had cancer then. I didn’t think I was going to need it. It did come in handy later on. Not being able to work because my doctor doesn’t want me to work was a big thing. It is just as real.
Since I live in a smaller area, while there are hospitals, everyone’s there for a hospital. But in the bigger area that I went to, they have multiple hospitals, and I could get treated at an actual hospital. It’s a big difference.
In smaller areas, you can probably still get treatment. The bigger areas attract the doctors that know more or have more experience in things like that, and that’s where the traveling comes in.
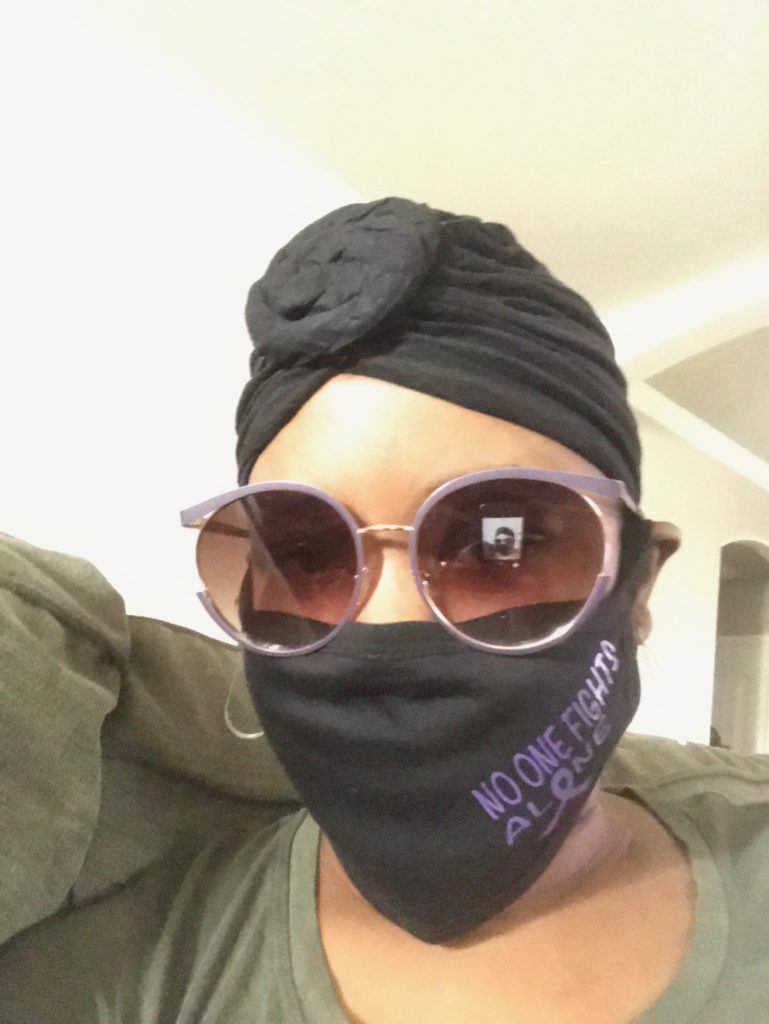
Message for other patients about speaking up
Listen to your body. I felt I need to speak up, but then I also thought, ‘Okay, they’re professionals. I’m the patient. They were trained for this.’ But also, you know your body.
You know when something is not feeling right compared to your other experiences before. I’ve made sure I spoke up and let them know whatever I’m feeling, so they can do what they needed to do.
In my situation, the process would have been to check it out, to get an X-ray, and they didn’t do that. That was on them. I made sure I spoke up, and they said they were going to note it in my chart and to slow the medicine down.
As I move to a bigger area where people have more experience, the nurse knew I’m not getting treatment. They did a port placement test to see what was going on, which they should have done before. That’s when they knew that the chemo is not going where it should. That’s another not-so-good story.
Just check with yourself. When you do not feel anything, or if you feel like everything — everything is valid.
Even the smallest thing that might be off, tell your doctor so they can know. It might be significant later on.

Just to give an example, I was having joint pains in my feet. My doctor noted it, and he adjusted my medicine [dose]. From 120 mg, now I get 80 mg.
Even the smallest thing, your doctor can make the changes that he needs or know [he] needs to note in your files and your paperwork so you can be better. You won’t have those huge side effects. Speak so they can make it more comfortable and come up with solutions.
Message to patients and caregivers
Just take it day by day, hour by hour, and evaluate yourself, your emotions, and everything.
If you just think about getting through the end, you just want to get through everything. You just want everything to be done, and you can start your life over.
Take your time. Do what you love. If you can’t work anymore, take that time to figure out what you like to do, and do it. That’s where I’m at now, figuring out. You just never know when it’s your time.

Inspired by Delishea's story?
Share your story, too!
Other Stage 4 Hodgkin’s Lymphoma Diagnosis Stories
Amanda P., Hodgkin’s, Stage 4
Symptoms: Intense itching (no rash), bruising from scratching, fever, swollen lymph node near the hip, severe fatigue, back pain, pallor
Treatments: Chemotherapy (A+AVD), Neulasta
...
CC W., Hodgkin’s, Stage 4
Symptoms: Achiness, extreme fatigue, reactive rash on chest & neck, chills, night sweats
Treatment: ABVD chemotherapy (6 cycles)
...
Amina V., Hodgkin Lymphoma, Stage 4B
Symptoms: Severe fatigue, shortness of breath, night sweats, bloating and stomach distension after eating, abdominal pain, little to no appetite, high fever, lump in the pelvic area
Treatment: Chemotherapy
...
Lisa S., Nodular Sclerosis, Stage 4A
Symptom: Extreme lower back pain
Treatment: ABVD chemotherapy
...
Dilan P., Hodgkin’s, Stage 4B
Symptoms: Night sweats, appearance of lumps on the neck and in the armpit, severe itching, fatigue
Treatment: Chemotherapy
...





