Stephenie’s Classical Hodgkin Lymphoma Story
At 26, Stephenie was nearing the end of her master’s studies at the University of Georgia when she developed some unusual symptoms like bumps on her neck. She thought nothing of it, but her sister pushed her to get examined which led Stephenie to make an appointment at her university’s health center. Her doctor was thorough in his exams and tests, which led to Stephenie receiving a Hodgkin’s lymphoma diagnosis as a young adult.
Her life rapidly changed as she found herself making appointments to begin cancer treatments while at the same time taking finals and writing her final term paper to finish her master’s program. Less than a week after graduating, she began chemo and would go on to try two other chemotherapy regimens as well as two stem cell transplants.
Today, Stephenie celebrates 5 years of being in remission and shares her cancer story with us, including the importance of doctors providing individualized cancer treatments and care, dating while receiving cancer treatment, experiencing graft-versus-host disease, being a patient advocate, pushing on when cancer treatments fail, and her advice to others on their own cancer journeys.

- Name: Stephenie P.
- Diagnosis (DX):
- Symptoms
- Bumps along the neck
- Night sweats
- 25-pound weight loss
- Age at DX: 26
- Treatment:
- Chemotherapy
- ABVD
- ICE
- Brentuximab
- Radiation
- Stem cell transplants
- Autologous
- Allogeneic
- Chemotherapy
If I can help one person get through their journey, then sharing my story is the least that I could do.
Stephenie P.
- Symptoms & Diagnosis
- Chemotherapy
- Stem Cell Transplant
- Considering a stem cell transplant after unresponsive chemo
- Preparing for a stem cell transplant
- Describe your experience with getting a stem cell transplant
- Did you have a hospital stay?
- Is it normal to stay in the hospital post-transplant?
- What were the results of your stem cell transplant?
- How did you process your cancer metastasis?
- Second Stem Cell Transplant
- Getting a second stem cell transplant
- Finding a stem cell donor
- Describe discovering your sister was a match
- Switching medical care
- Receiving radiation before stem cell transplant
- Did you develop graft-versus-host disease?
- Taking maintenance medication to retain donor cells
- What was the prep like for your second stem cell transplant?
- Survivorship
- Reflections
Symptoms & Diagnosis
Tell us about yourself
My name is Stephanie. I am a Hodgkin lymphoma survivor for 5 years now. I’m still getting back into a lot of my hobbies. I had to do a lot of after-cancer rehab. I have 2 beagles, spend a lot of time at home, cook a lot, and do a lot of baking.
When did your symptoms first occur?
It was back in 2015. I think it was around the beginning of the year, I started noticing I got these bumps on my neck. As the months passed by, they weren’t going away. I think I waited 3 or 4 months before I actually went to the doctor to check out the lumps in my neck.

I was at the University of Georgia at the time getting my master’s degree. I went to the university health center that they assigned to every student. I went to him and said, “I have these lumps on my neck and they’re not going away. I haven’t been sick or anything, so I don’t know what’s going on.” He asked me all these other questions like, “What other symptoms are you having?” I said, “Well, I don’t think I’m having any other symptoms really.” Then he started asking me questions like, “Have you been having night sweats?” I said, “Well, yeah, I have been getting really hot in the middle of the night.” He asked, “Are you sweating so much that you’re soaking through your clothes?” I said, “Yeah, actually. It’s never been that much before.” Then he asked me if I was feeling more tired than usual. I said, “I don’t know. It’s finals and I just ran a half marathon.”
I didn’t really take those things into account that those could be symptoms that all added up to something else. I don’t even know if I would have gone to the primary care doctor at all if my sister hadn’t pushed me to do it because I went to go visit her during that time and I said, “I have these lumps on my neck.” She was looking at them and she’s like, “You should get that checked out.”
Examining the symptoms with tests
He wanted to do some other tests after that. I said, “Well, what could this be?” He listed off a lot of things that it could have been. I just remember the last thing he said was cancer. I was so surprised because he was just my university physician. I don’t know how many cases he gets like this or how often he sees something like this, but I’m really grateful that I was assigned to him because I feel like any other doctor would have been like, you’re young, it’s probably nothing. I was really grateful that he took it seriously.

He listed off a lot of things that it could have been. I just remember the last thing he said was cancer.
He gave me the next steps and he was very quick about it. I feel like a lot of times you’re waiting around for the next step. But he was like, “Alright, today you’re going to go and get more x-rays. Tomorrow I’m going to schedule you for this.” So there was no in-between time working with him. If I can give a shout-out to Dr. Kevin Sanville at the University of Georgia, he literally saved my life. I’m so grateful.
Accelerating testing due to imminent insurance changes
It was a complicated time for me because I had just turned 26, so I only had that month left of being on my parent’s insurance. I think that’s part of why he wanted to speed it up so that I could get all that testing done and it’d be covered.
We did x-rays, I had my first CT scan, and then I had a follow-up with him where he went over all the results from those things. He said, “There’s a good possibility that this is cancer.” We had to move on to getting biopsies.

It’s good being in a university town. There’s a lot of doctors, a lot of medical practices there. He sent me over to do the biopsies, we got the results back, and then he set me up with an oncologist who was in town. Luckily it was a practice that’s all over the state. They knew that I was graduating so I wouldn’t be there for my entire treatment, so they made sure to set me up with somebody I could still transfer easily with wherever I went.
Getting tested before beginning cancer treatment
I had 3 biopsies so that they could be certain. They took one out from my neck, from my underarm, and then I did the bone marrow biopsy and it moved really fast after that. To get me ready for chemo, they had to get all these other tests done to make sure that my body could handle the chemo. I had to do a pulmonary function test to make sure my lungs were good. I went to a cardiologist to get an echocardiogram to make sure my heart was good. There were a bunch of doctors I had to go to before.

I had to go see my dentist too. That really freaked me out because they said chemo can mess with your gums and your teeth. My teeth were expensive. If you ask my mom, she’ll say she paid $6,000 for my braces. I remember making an emergency appointment with my dentist. That was a crazy experience, going to your dentist and saying I need you to check me out because I’m about to go through chemo.
My dentist was on top of it. Unfortunately, his sister was diagnosed with breast cancer so he knew when things happen, they have to happen fast. My dentist had the office on vacation that week and he was like, “Everybody’s out of the office.” I was freaking out, so he opened the office just for me and he did everything himself. I left with a huge bouquet of flowers, too. It was very nice.
Describe being told you have cancer
The way I found out I wish was different because it was actually from my surgeon who did the biopsies. He called me a few days afterward and said, “Yeah, we got the pathology and it looks like it’s Hodgkin lymphoma. You probably want to follow up with your oncologist.”
I was sitting in bed recovering from the biopsy, so I was just on the phone with him. I didn’t really know what to do. I was at my apartment by myself at the time. My roommate wasn’t home so the first thing I did was I called my sister. She was living in New York at the time and she was working at a corporate job so she knows that when I call, she needs to answer. She said that she was in a meeting, but she ran out into another conference room to take my call.
» MORE: Reacting to a Cancer Diagnosis
I didn’t know what to do because I didn’t get the news from my oncologist, so I just waited for my roommate to get home. We made a plan because I was like, I know a lot of people are going to want to know what’s going on, but it’s going to be really frustrating for me to keep telling them over and over and getting all the people’s reactions. She was like, “I’ll help disseminate the information so that you don’t have to deal with all that.” Then she took me out to dinner.
I did go to the oncologist the next day so I didn’t have to wait that long before we figured out what the next steps were. I just really wish that the surgeon had done the correct procedure and waited so that I could get the news in my oncologist’s office.
Chemotherapy
Where did you receive medical care?

I started out at the office that they had there in Athens, then eventually I graduated and had to move out of my apartment. The easiest thing was for me to move back home with my parents. Luckily, there was an office that was 15, 20 minutes from my parent’s house so I transferred over to them.
Describe your first oncologist visit
There’s no such thing as “good cancer.”
That was a blur. I had two of my college friends come with me because I was away at school, so my parents didn’t come. They came with me to absorb all the information that I could not absorb. They said, “We want to start treatment as soon as possible.” They gave me the whole “Hodgkin lymphoma is a blood cancer, so we’re really good at curing those. You’ll do 6 months of chemo and you’ll be good.” I got that line, “You got the good” cancer. That’s all I remember.



There’s no such thing as “good cancer.” There are so many different types of cancer and everybody’s journey is different. No matter what, even if you don’t have to do chemo or you don’t have to do radiation, some people have to get surgery. It’s different for everybody and it’s hard on people in different ways. There is nothing good about getting a cancer diagnosis, so I can’t believe that doctors still say that to people. I guess it’s their way of trying to make you feel like everything is going to be okay but there’s a different way that you can do that.
Juggling finishing school and beginning treatment
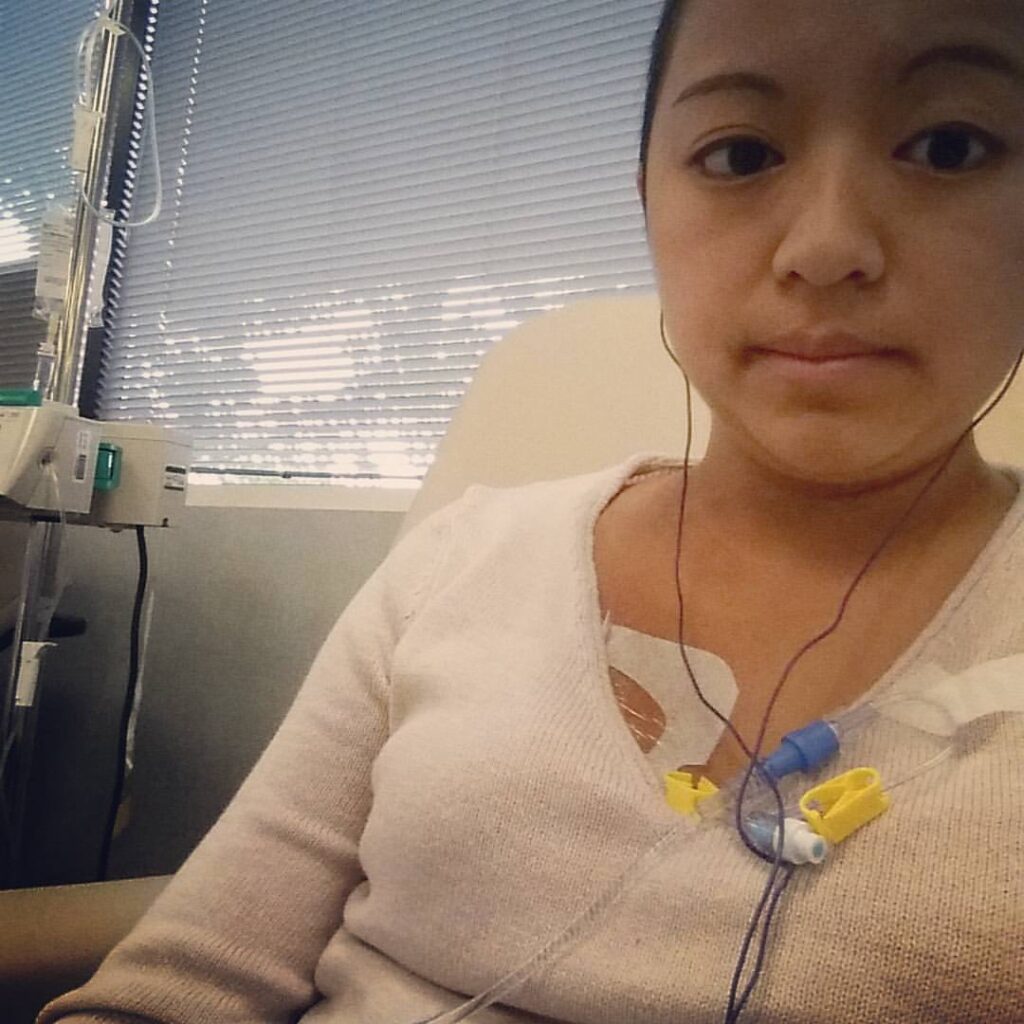
After that, we had to schedule my port placement, and then they talked about my chemo schedule and doing 6 rounds of ABVD which would take 6 months. I feel like it was different for me because I was in my master’s program and I still had to graduate. I had to reschedule all my finals with my professors and it was my last semester. I had to do my final term paper.
There were all these things that we had to do for graduation, and I was getting inducted into an honor society. Not only did I have to start scheduling all these appointments and surgeries, but I had to also try to do school on top of that. It was a little hectic. Luckily my professors were really understanding, so it all worked out.
I graduated Friday and I started chemo on Wednesday.



They actually wanted me to start chemo before graduation. I think graduation was May 8th. I remember that because it was my sister’s birthday and they wanted to start chemo the week before that. I was like, “Can I just graduate first and then start chemo?” Luckily, they said we can do that. I graduated Friday and I started chemo on Wednesday.
Did you have any side effects on chemo?
Starting treatments, I really did not know what to expect at all. I just went. It wasn’t as bad as I thought it was going to be. It was pretty easy. I arrived at the cancer center, then they knocked me out with diphenhydramine. I woke up and I was done for the first few months. The side effects, luckily for me, were very little.
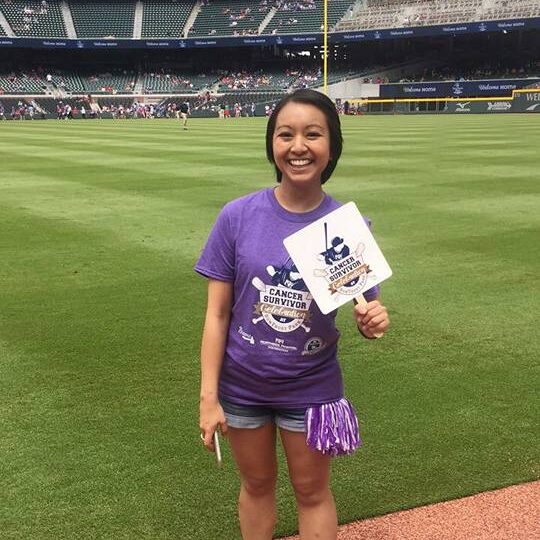
I did lose my hair after the first month of treatment. I was putting off shaving my head because my aunt is a hairstylist and I wanted to try cool things before I had to shave my hair off. We did cute short hairstyles and we did purple hair for Hodgkin. It was fun.



» MORE: Hair Loss and Regrowth After Chemotherapy
I didn’t get too nauseous with ABVD. I think the first time my nausea got really bad was my third treatment. I did get really tired. I tried to stay active. I had a very busy schedule all the time just because I was in graduate school. I was used to being on the go a lot so I still kept a pretty busy schedule. Then after a month or 2, I had to start pulling back because I was getting so tired all the time. I’m not a nap person at all, but I would sleep so much. I think those were the biggest side effects for me during chemo.
Changing chemo treatments
The first protocol that they did with me was a scan and they said that nothing had really improved, so we had to move on to the second round of treatment, which was a different chemotherapy regimen. We did a scan after that too, and it still showed no improvement.
The second chemotherapy treatment that they had me on was the ICE regimen. That stands for all the all the chemo drugs they give you. That was tougher because it was multiple days of chemotherapy instead of once every 2 weeks. It was more tiring because you’re getting more drugs.
Learning to live with uncertainty
I was just rolling with the punches at that point. Before I got diagnosed, I was a really organized, scheduled person, and I realized really quickly that that wasn’t going to work for this. I had to learn how to live with ambiguity, uncertainty, and, whatever they threw at me. I took it and figured out a way forward. I was like, alright, let’s keep rolling. What’s the next step?
Stem Cell Transplant
Considering a stem cell transplant after unresponsive chemo
That’s when they started talking about possibly having to do a transplant. I got all this research about transplants. I was hooked up with The Leukemia & Lymphoma Society, so they gave me a lot of information and people to talk to about transplants.

This was something I’d never heard of before. I’d heard people get live, solid organ donations, but I didn’t know anything about stem cell transplants or bone marrow transplants. It was a lot of talking to people and getting their experiences.
I was on brentuximab during that time just so that they could keep everything at bay. Then they referred me to the transplant oncologist so it was more appointments and more education on what stem cell transplant would be and how to get me ready to get to that point.
Preparing for a stem cell transplant

The first transplant I got was an autologous stem cell transplant. That’s when they extract your own stem cells from you and put them back into you. I’m not a sciencey person, so I try to understand it as best as I can. I had to do these self-injection shots of filgrastim because that’s what makes your stem cells grow. I did that for 5 days. After that, you have your collection day where they take all of your stem cells out. It involves sitting in a chair all day and it’s like giving blood, but they put it through this machine that sorts out all the blood products and all the stem cells, and then it puts the blood back into your body.
It’s a long process and I was there for a long time getting my stem cells collected. There’s a certain amount that they need to collect from you before they start the rest of the process. I was hoping that they had enough that I only had to do one collection day because I heard people had to do 2 or 3 days of collections. I only had to do one day of stem cell collection.
Describe your experience with getting a stem cell transplant
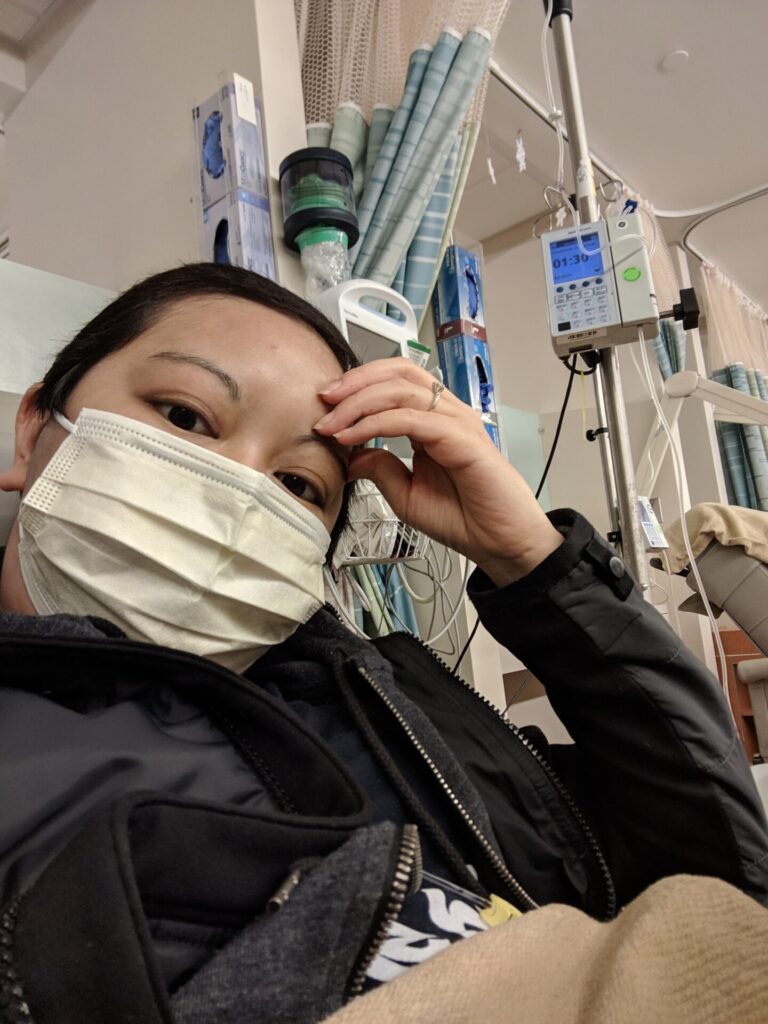
That was tough to get ready for the stem cell transplant. Not just the stem cell collection, but there are days of high-dose chemotherapy that you have to go through. It was different drugs that they gave me at that time. Those were long days in the chair at the hospital. I think there were 3 days of high-dose chemotherapy before my first transplant.
The thing that was the toughest was for all of the transplant stuff, they don’t use your port, they use a tri-catheter port because you need so many things going in you at one time. I had to get that placed too. That was part of getting ready for the stem cell transplant. After you get that placed, you cannot go into public places anymore. You can’t drive. After I got that placed, I was dependent on everybody around me. You have to have a caregiver 24/7 and that’s so hard for a lot of people to find. Luckily, my mom was able to take FMLA off from her work so that she could stay with me.
Then we had another obstacle where we were about an hour away from Atlanta. My mom could not drive that far, so not only did I have to have a caregiver, but I also had to have a driver who could take me to the hospital every day. You’re at the hospital every day for all the pre-transplant stuff before you’re even admitted to the hospital.
It was crazy. I had to put out this blast to all my friends and say, “These are the days I have appointments. I need a driver in the morning, and a driver in the afternoon.” We had this calendar where people would sign up. Georgia is pretty spread out, so people were driving from the other side of the state to come pick me up and take me to the hospital. It was literally the whole village that needed to help me. That was really tough because I’ve always been on an independent streak. Begging people for that help, I felt so bad.
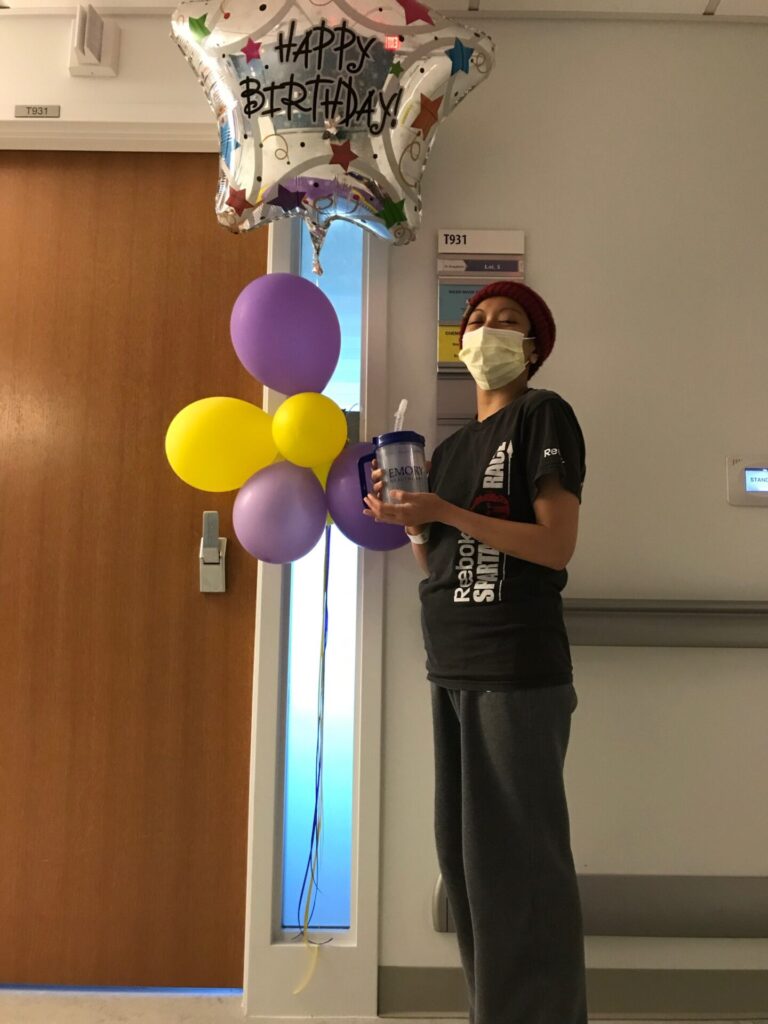
Did you have a hospital stay?
The first stem cell transplant was rough. There are so many protocols when you’re in the hospital. Since I didn’t have that transportation back and forth to the hospital every single day, I was admitted for the first 100 days of my transplant, so I was in the hospital for a long time. It was really rough because you can’t sleep. Every 6 hours there was something that somebody had to do. Every 12 hours there was something somebody had to do. I had to get woken up in the middle of the night just to get blood work done. It was impossible to get any sort of rest in there.
I think about halfway through, my port actually got infected so they had to remove that. I had to spend the rest of the time in the hospital getting stuck with needles every day so my veins just got shot. I remember one night it took 3 nurses and 17 sticks to get my blood sample for the night, and every night, you had to do blood work. It was intense but I had somebody visit me every day.



My best friend would come every day after work. She would be there with me at the hospital every night. I just love her so much. She really got me through that. She came on the day of the transplant and she decorated my room. She put photos everywhere. I had a lot of people stop by that first day that I actually got my transplant. It was nice that I always had visitors, but when they leave and you’re there by yourself in the middle of the night, it’s tough.
Is it normal to stay in the hospital post-transplant?
I think usually you just stay in the hospital because, after your transplant, your white blood cell count goes to 0. Your immune system has to build back up and usually, they will discharge people after your immune system has built back up. Getting that blood work every day and then hearing the numbers, you’re just like, oh, I still have so long to go, was tough.
After my first scan post-transplant, they found that the cancer metastasized to my bone, especially in my spine.
What were the results of your stem cell transplant?
It was clear very soon after that it hadn’t been the effect that they wanted. After my first scan post-transplant, they found that the cancer metastasized to my bone, especially in my spine. I actually had to go to radiation after my transplant which was another experience.

How did you process your cancer metastasis?
I don’t want another young Asian girl to go through so much that she doesn’t need to just because we have to be treated in facilities that weren’t made for us.

It was tough to hear, but I feel like what’s really hard is getting other people’s reactions to it, especially my parents and family members. My parents are refugees from Vietnam, so there’s a language barrier and they don’t totally understand everything. Then there’s that constant thought in their head, Why is this happening?
It was a lot of trying to manage other people’s emotions really. I thought medicine in the US is made for people’s genetics who were born here, who are from here. Medicine was not built for people like me whose genetics are from across the world where things are different. That’s something that doctors haven’t really realized, that an Asian patient reacts differently to a lot of things than a Caucasian patient would. I felt that it was important for me to continue so that they could figure it out. I don’t want another young Asian girl to go through so much that she doesn’t need to just because we have to be treated in facilities that weren’t made for us.
Second Stem Cell Transplant
Getting a second stem cell transplant
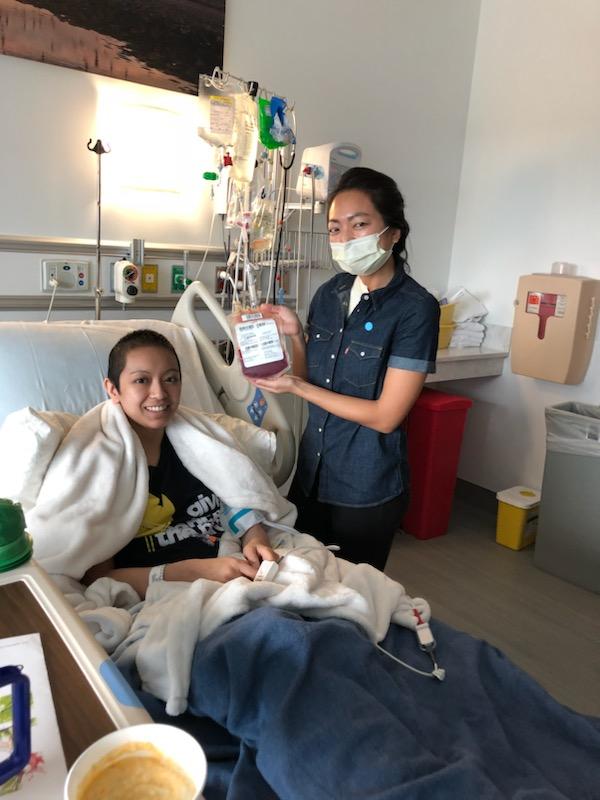
It was obvious that we had to move to the next level of stem cell transplants. The first transplant I had was an autologous stem cell transplant because they were getting the stem cells from my own body. The second transplant that I got was an allogeneic stem cell transplant, which gets stem cells from a donor.

That was the next step, was to do the transplant with the donor. That’s the part that scared me because I’ve worked with Be The Match before, and I was part of a big push for getting more diverse donors into the registry. It was a little scary because I knew that there weren’t going to be a lot of options for Asian people.
Finding a stem cell donor

Once again, my community came through and all my friends who were still at the university had a big Be The Match registry drive targeted towards getting Asian people to sign up. I can’t imagine being in that position where you’re depending on somebody else to save your life. But there’s people out there, they’re just not in this registry and you can’t find them. That was a scary part of it.
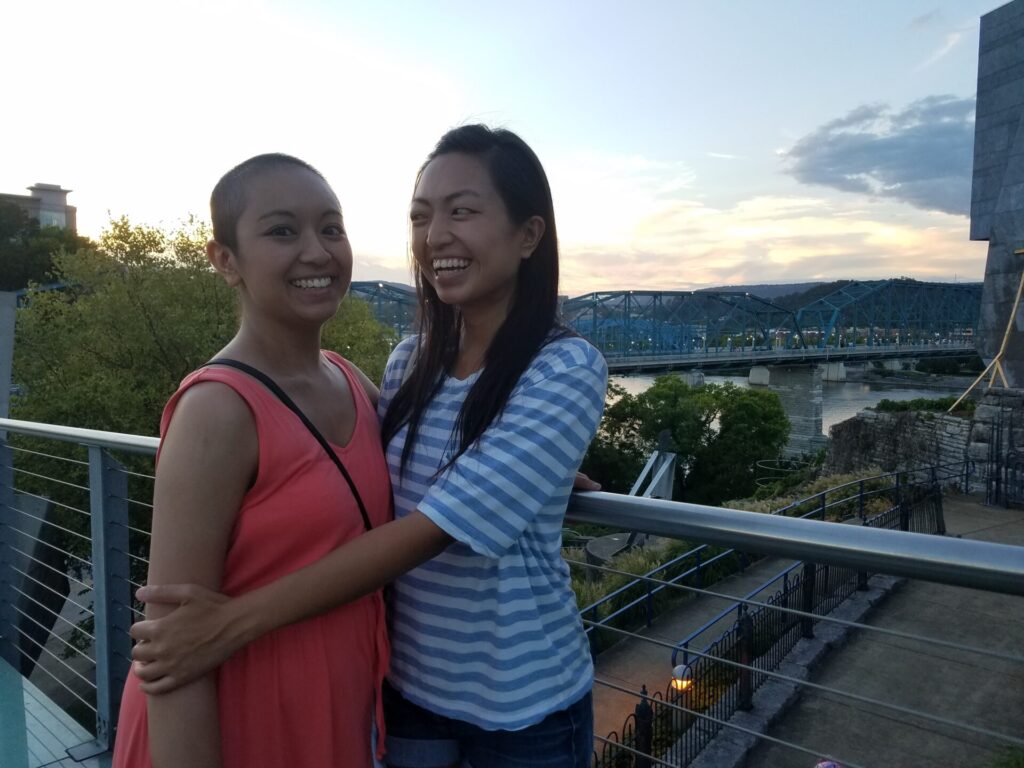
To find a donor, they ask that any family members who want to see if they’re a match for you can do that. My mom got tested and my sister got tested and I wasn’t really thinking that it would work out because the way that genetics work, I only have one sister. The chances that she would be a perfect match for me were not great. Then at best, my mom would only be a half-match for me so they could do half-match transplants, but the chances are of course going to be better if you have a 100% match. Luckily me and my sister are 100% matches.
Describe discovering your sister was a match
I remember getting the call when I was at work. Usually, when I was at work, I would pick up my phone and close my office door and immediately people would get worried. I picked up the phone and it said Emory calling. They said, “Your sister is a 100% match.” I started screaming.
After I got off the phone, I opened my office door and all my co-workers were standing there and they were like, “What happened?” Luckily it was good news, it was exciting. I don’t know if my sister already knew, so I called her too and said, “They just called and told me that you’re a 100% match.” She was really excited too. That was a huge relief because I really didn’t think that she would be a perfect match. People said, “You and your sister are basically twins.”



Switching medical care
I’m really glad that I advocated for myself and said this isn’t working for me.
I didn’t really have a good experience with my first transplant. The clinic was very full. It was very rushed. If I had questions, I felt like I couldn’t ask anybody. It wasn’t a good experience, so I didn’t want to do a second transplant with them.
I went to a different clinic to get a second opinion, and I went through my second transplant with them instead. I think that was a big change in my care. I’m really glad that I advocated for myself and said this isn’t working for me. I need to be somewhere else because my second transplant was the same process.
» MORE: How To Be A Cancer Patient Advocate

Receiving radiation before stem cell transplant

My sister had to fly in and she did all the stem cell collection. While she was doing that, I was doing high-dose chemotherapy still. Then I also had to do 4 sessions of total body radiation before the transplant could start. I was also admitted to the hospital before my actual transplant started. That was nice because I would already be there. I didn’t have to be transported back and forth being so tired from total body radiation all the time.
Did you develop graft-versus-host disease?
I had a better idea going into it since it was my second one. It had different challenges than the first one. With my second transplant, since it was from a donor, that’s where graft-versus-host disease comes in. My graft-versus-host was mainly in my skin and in my GI tract. It affected my eyes a little bit. Those were the worst side effects.

With the skin, it gets really red, itchy, flaky, and inflamed. They gave me this steroid cream and I was piling tubs and tubs of steroid cream on my arms and legs. It was everywhere. Arms, legs, stomach, back. Luckily, it didn’t get to my face. I didn’t even think about that.
My eyes would get really dry. Even now, really bright sun or bright lights, my eyes are super sensitive now. Along with those problems, I had that stomach ache feeling all the time. I couldn’t eat anything really. It was tough to get through that. Eventually, once your body starts accepting the donor cells more, the symptoms go down and they give you medication to manage it.
Taking maintenance medication to retain donor cells
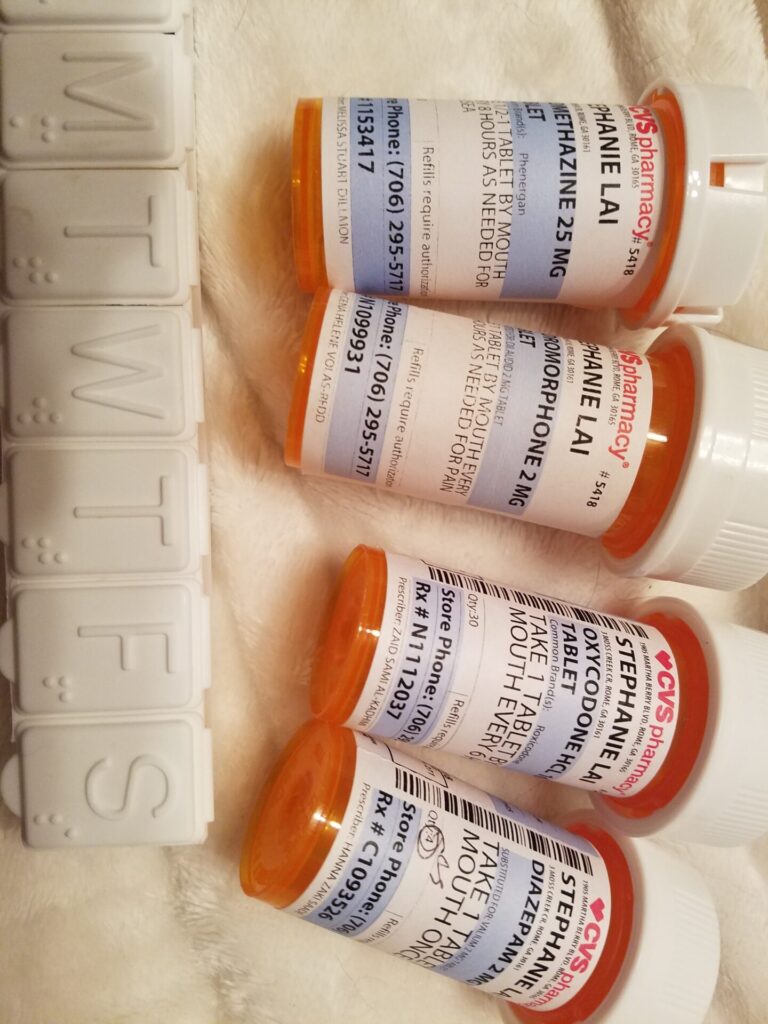
After that transplant, there were several medications that I had to be on for a few years afterward to make sure that my body wouldn’t reject the donor cells. Everything eventually calmed down with all of that. It was a lot of maintenance treatments with the medications and they’ve continued me on brentuximab. I think that was their miracle drug at the time. Everything cleared up. I was warned that, if I get sick the symptoms might flare up sometimes, which I’ve seen this past year. My skin has gotten really dry again. Luckily, nothing as bad as it was before.
What was the prep like for your second stem cell transplant?
The stem cell transplant, with all the prep for this second stem cell transplant, they actually have to get you into remission before they do the stem cell transplant which I feel like they should have done with my first transplant, which is also a reason I decided to go to another clinic.

With all the high-dose chemotherapy, we did the scans and found out I was in remission. That’s when they scheduled me for my stem cell transplant. It was a little bittersweet because you get the news that you’re in remission, but then you still have to plan for another 100 days in the hospital.
Survivorship
How did you react to hearing you were in remission?
I actually just got a phone call from my doctor because I had gone in for the scan and all the blood work and she didn’t want me to wait until my next appointment all the way in Atlanta. She gave me a call and told me that there was nothing they saw. They didn’t see anything on the scans so she was like, “We can declare you in remission and get you ready for your stem cell transplant.”

I still was skeptical because I was like, I’m in remission, but I still have to do this stem cell transplant and the last stem cell transplant didn’t really go as expected. I knew that I just had to keep going and whatever the result at the end would be we would just play it from there.
Describe your recovery process post-transplant
It was tough. There were a lot of quarantine days because your immune system is still so low that you don’t want to be in a lot of public places. I was recovering at my parent’s house. My mom took more time off of work to see me through the second stem cell transplant. It was a lot of trying to get my appetite back up, get active, and get back into normal activities. There’s also a lot of follow-ups. Even after I got discharged from the hospital, I was still going there. It started out once a week and then after a while, twice every 2 weeks, and then eventually you get to be discharged forever.

Dating during cancer treatments
I met my husband through a popular dating app that my friend had signed me up for. It was about 6 months after I was already in treatment. I was already very much in my cancer era. I didn’t really want to date, but my friend forced me out there.
I was very straightforward. I was like, “I have cancer. I’m still going through treatment.” He was very receptive and understanding. The first time we met was in the wintertime, so I was wearing a hat. He was like, “Just take your hat off.” I was like, “No, I’m good.” It was an interesting time, but I think we were only dating a few months before I went to my first transplant. It moved very fast because of where I was in my treatment. That’s why I was so straightforward when I first started talking to him because I knew that I had to do this and he couldn’t get in the way. Either he was in or out. I didn’t have time to waste and luckily he was on board.
I was really grateful for that because I was going through grad school and dating during college and school is completely different. I felt like I was in a place where life was becoming very real. I knew that I didn’t have any time to play around anymore. I needed something serious. It really weeded out everybody. It was easy because, once that C word comes up, people either run to help you or they run away. That sorted out a lot of things in my life, not just in the dating department, but also with friends and unfortunately some family.



How long have you been in remission?
I’ve been in remission since February 2018, so it’s been a little over 5.5 years.
What was life like after remission?
After my second stem cell transplant and knowing that I was in remission, I started to try to get back into the swing of things and become a productive member of society again. I wanted to use my master’s degree that I had to finish before I started treatment.
» MORE: Learn More About Cancer Remission

It was a lot of learning that I had to do dealing with being a cancer patient, even though I don’t look like a cancer patient. Trying to find work that I was able to do. Even going through getting married and having a wedding. There are a lot of things that as a cancer patient, I had to take into account. It does become part of all these other parts of your life in some way, shape, or form.
What is survivorship to you?
Some people who haven’t had cancer will say that once you’re in remission, you’re all good. That’s really not how survivorship is. There’s a lot that goes into it. Not only did I have to do a lot of physical therapy, but I had to do a lot of mental therapy. Talking to my therapist all the time, and working on my mental health were very important.
Cancer does become intertwined with a lot of aspects of your life if not all of them. Just because you’re in remission doesn’t mean that you don’t have to stop thinking about it. You just don’t think about it as much. There are still triggers and obstacles that you come across post-cancer that will remind you that was something that you went through and that you have to do things a little differently now maybe because of what you’ve been through.
» MORE: A Guide to Cancer Survivorship Care Plans for Hodgkin Lymphoma Patients



There are things that I think about now whenever I’m doing something. If I’m traveling, I can’t be on my feet too long, so sometimes I’ll have to get a wheelchair at the airport. There are different things that you have to adjust to. The important thing is that you’re still here, you’re still alive, you’re still doing it. I guess cancer just likes to remind you to appreciate life a little bit more.
Did you preserve fertility?
I did see a reproductive specialist before my first chemotherapy session. It wasn’t stressed to me the importance of doing any kind of egg freezing because I had a blood cancer and a lot of patients are able to do the first round of treatment and move on with their lives and conceive and have children. That was the mindset that they led me to believe.
With the timing of everything, there just wasn’t enough time to think about doing egg freezing. I was young at the time, so I was like, I’ll bounce back. Then, of course, my treatment did not go as planned. Unfortunately, I didn’t have that to fall back on.

That was another thing that I was very direct about when I first met my husband. I was very clear that not only do I have cancer, but there’s probably a good chance that I won’t be able to have children either. He was very receptive to that. His family has a lot of adopted children in their family. He was like, “I know all about adoption and I’ll be on board just as long as you’re healthy.”
We did meet with another reproductive specialist after I was in remission and we did testing to see if I could conceive. That was when I was told that I was already in menopause, which is probably why I was sweating so much at night. There was an option to do an egg donor and have a surrogate, but we just didn’t feel comfortable going that route so our plan is to adopt. There’s still a lot of research that we’re doing and a lot of saving up that we’re doing because not being able to conceive your own child is very expensive. That’s our eventual goal is to adopt a child.
Reflections
The importance of understanding that everyone’s cancer journey is unique
I think the most important thing that I learned was that there is no comparison with cancer. Every person is different. Every journey is different. Even if you have the same exact diagnosis as somebody else, you could be going through completely different things. It’s your own journey and you have to figure out a way to keep going no matter what. Nobody else is going through it but you and it’s a lot of trying to make people understand, a lot of managing emotions. I didn’t realize that when I told people I had cancer I would have to comfort so many people.
It’s very eye-opening to see who really cares about you. It really tells you who’s going to be a true friend. Cancer is the only thing that’s not going to lie to you. It’s going to tell you how it is with everybody. It’s your own journey. You can have bad days.
I hated when people told me that I needed to stay positive. Some days you just want to curse the world and be in your bed all day. Take what you need. Do what you need to do. Nobody else knows what you’re going through, so you have to advocate for yourself. Let people know. I like to share my story because people look at me and say, “You’re young, you’re healthy,” but they don’t know what it took to get there.
Even if you have the same exact diagnosis as somebody else, you could be going through completely different things. It’s your own journey and you have to figure out a way to keep going no matter what.
Learning to listen to your body
I’ve been extra careful nowadays, especially post-COVID. I live in Georgia. It gets really hot, so I will sweat at night, but sometimes it’ll be a really hot day and I might sweat a lot that night. It’s a trigger that reminds me that this is what happened last time. Be on the lookout. That’s one of the things that cancer has taught me is how to listen to your body and what it’s telling you. I find myself very much more aware of how my body is feeling.
Since the beginning of this year, I’ve had this lymph node that my husband will catch me touching on my neck where my other lymph nodes were. I subconsciously check myself all the time. Every little thing can be triggering. It’s really hard to get out of that mindset. My doctor has told me several times, “That’s just an overreactive lymph node. You’re going to feel it. It’s nothing to worry about.” But I made her schedule me for a scan.

That’s one of the things that cancer has taught me is how to listen to your body and what it’s telling you.
I think it’s important to listen to your body, but also recognize that sometimes a cold is just a cold. I have this trust in myself now where I know that this could be just a cold, but maybe this is something else. I think there’s some different feeling in your body that lets you know, this is not normal. As long as I don’t get that feeling when I get a cough or when I get a cold, I’m good, but I think that one overreactive lymph node really freaked me out because I wasn’t used to that.
Being a patient advocate
With all the follow-up care and meeting with different doctors, there is a lot of educating them on how to treat a cancer patient, a lot of repeating questions, and a lot of explaining to them what your scars are and what your radiation tattoos look like. I think it’s also a good learning experience for doctors who haven’t had to deal with young cancer patients.

I have had a lot of doctors who, after meeting me, they’ll go do their own research about how to best provide care for a cancer patient. It’s frustrating having to retell your story all the time when you know that they could just read your history, but my history is so long that it’s just one of those things that you have to deal with every time you see a new doctor.
Even the form that you fill out when you get to the doctor’s office is like, “Do you have a history of cancer?” [I mark] yes, but they look at my age, and because I’m Asian I don’t look like I’m 34. They look at me and they’re like, “She’s young, I don’t need to check out these sections.” Then later when I tell them “Yeah, I’ve had cancer,” they’ll bring up that page and say, “Oh yeah, you marked it here.” I hope it brings awareness so that they make sure that they read the entire chart before talking.
I haven’t had any other major issues where that would be a problem. But there are some things when it comes to them prescribing medications and things like that, they find out that I’m on all this other medication and then they’ll realize, “Oh yeah, we’ve got to find something that won’t react to these medications.”
Do you still follow up with doctors post-remission?
I still have a regular medical oncologist that I see every so often. I think since I was recently discharged from my transplant oncologist, those appointments will probably go away. I do have to keep up with the cardiologist because the treatments are hard on your heart, especially being a young patient. There’s so much time for any radiation scarring that could become worse over time I have to continue to follow up with a cardiologist, a pulmonologist, and a dermatologist since my skin was so bad.
Rehabilitating after cancer
When I was getting diagnosed at first, I thought that I was going to be getting chemo and that was it. Chemo affects your entire body, so you have to continuously make sure that the rest of your body is still able to handle the treatment. There’s a lot of monitoring every part of you, even things I didn’t know that they did. I didn’t know that you could get a CT scan of your brain.
It was a lot of different tests and things like that even post-treatment trying to rehab from cancer. I had to do a lot of physical therapy. One of my medications was giving me really bad hand tremors, so I had to do a lot of hand exercises and relearn how to write. Even simple things that people take for granted, like being able to sit up from a sitting position, or stand up from a sitting position. I had to practice that so many times because I was falling over. It’s a lot of recovery.

I still can’t be as active as I used to be. Before I started treatment, I ran a half marathon, and I don’t even think I could walk a mile now. It’s a lot of recuperation from treatment.
What have recent scans shown?
I’m clear. Since that last scan for remission, they’ve been monitoring blood work. If anything was wrong with my blood work, then they would move to scan. Luckily, it’s been good.
The importance of sharing your cancer story
If I can help one person get through their journey, then sharing my story is the least that I could do.

A lot of people ask me why I like to share my story so much and why I’m so open about what I’ve been through, and what I’m going through. When I was getting diagnosed, there was really nothing that gave me that personable experience of what it’s really like to go through and that’s why I like to share my story. I was trying to find people’s stories online to see what it was like, and I could not find anything. I think it’s really important to share your story, and what you’re going through, and it really helps people not feel so alone.
I can’t name a lot of young adults or Asian patients. I really like to advocate for people who have the same background as me because it is a very grueling process. I feel like a lot of research needs to be done on different kinds of cancer care depending on your genetics. I want people to be able to find my stories and what I have to say because it’s so much more comforting hearing it from cancer patients themselves. If I can help one person get through their journey, then sharing my story is the least that I could do.
More Hodgkin Lymphoma Stories
Jessica H., Hodgkin’s Lymphoma, Stage 2
Symptom: Recurring red lump on the leg (painful, swollen, hot to touch)
Treatment: Chemotherapy
Riley G., Hodgkin’s Lymphoma, Stage 4
Symptoms: • Severe back pain, night sweats, difficulty breathing after alcohol consumption, low energy, intense itching
Treatment: Chemotherapy (ABVD)
Amanda P., Hodgkin’s Lymphoma, Stage 4
Symptoms: Intense itching (no rash), bruising from scratching, fever, swollen lymph node near the hip, severe fatigue, back pain, pallor
Treatments: Chemotherapy (A+AVD), Neulasta
Brescia D., Hodgkin's Lymphoma
Symptom: Swelling in the side of her neck
Treatment: Chemotherapy: 6 rounds of ABVD





