Survivorship and Song: John Rediscovers Joy After a Rare Salivary Gland Cancer
On most days, John thinks of himself first as a professional opera singer. He is a man who measures time in rehearsals, warm-ups, and the joy of the musical world he lives in. So when a small bump near his jaw appeared during a season of renewed health, it barely registered as a concern. No one, including his doctor, was envisioning a rare salivary gland cancer. His doctor scheduled a surgery and routine biopsy to clear it up. But a few days after the procedure, John’s world shifted when he heard the news he never imagined would follow something so ordinary. “It’s cancerous.”
Interviewed by: Carly Knowlton
Edited by: Chris Sanchez & Jeff Forslund
That moment touched off an unexpected and disorienting period. John, who had survived a heart attack and prided himself on resilience, suddenly found himself in the world of rare cancers. More testing and consultation with a specialized care team confirmed the diagnosis: salivary gland cancer (carcinoma ex pleomorphic adenoma), a type of head and neck cancer where cells in a long-standing benign tumor convert to cancer. The surgical team’s quick response led to neck surgery to detect if lymph nodes were cancerous, with the fortunate news that the cancer hadn’t reached his lymph nodes. “They wanted to act fast because it’s a high-density cancer, which can sometimes metastasize and be difficult to treat,” John recalls.

Radiation treatment was intense, requiring 33 daily sessions. The realities of daily therapy, loss of taste and smell, and the psychological barriers of eating purely for survival changed John’s daily habits and challenged his sense of well-being. Still, his career as an opera singer and choral performer went uninterrupted, a testament to John’s determination and vocal discipline.
Throughout his salivary gland cancer experience, John leaned heavily on his boyfriend, friends, and his wider musical community. He highlights Gilda’s Club and other support organizations as critical for emotional and practical help, especially for men. More than anything, John’s story emphasizes honoring support, resilience, and the importance of living as a “survivor of life, not just cancer.” He reminds all patients: “Cancer is cancer, no matter the type or how ‘mild’ it may seem. Surviving is surviving.”
Watch John’s video and browse his edited interview transcript below for more about how:
- Advocacy and specialized care are vital for rare cancers like salivary gland cancer, making it vital to seek multiple opinions
- Support systems, both personal (family, friends, partners) and professional (support groups), make a profound difference
- Every type of cancer is significant; “easy cancer” or “mild cancer” is a dangerous myth
- Maintaining identity and routine during cancer treatment can aid emotional healing and mental well-being
- John transformed from initial shock to embracing survivorship and planning a life of early retirement, travel, and continued musical achievement
- Name: John C.
- Diagnosis:
- Salivary Gland Cancer (Carcinoma Ex Pleomorphic Adenoma)
- Age at Diagnosis:
- 61
- Symptoms:
- Rapid weight loss
- Small lump under ear that became more pronounced and grew larger
- Treatments:
- Surgery: lumpectomy
- Radiation therapy
This interview has been edited for clarity and length. This is not medical advice. Please consult with your healthcare provider to make informed treatment decisions.
The views and opinions expressed in this interview do not necessarily reflect those of The Patient Story.
- My name is John
- The subtle lump under my jaw
- How we confirmed my salivary gland cancer [carcinoma ex pleomorphic adenoma] diagnosis
- How my diagnosis impacted me
- My treatment plan
- My radiation therapy regimen and side effects
- I rang the radiation bell
- The hardest part: loss of taste and smell
- I have a strong support system: my friends, community, and partner
- No evidence of disease: scan results and confidence
- What I want others to know
My name is John
I was diagnosed in June 2025 with a rare cancer called carcinoma ex pleomorphic adenoma.
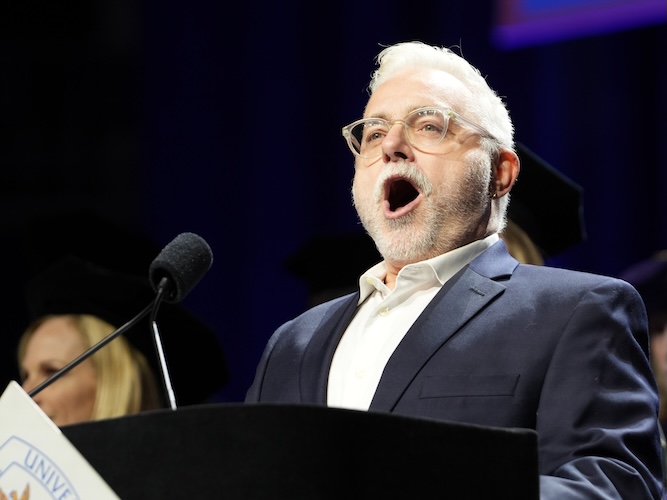
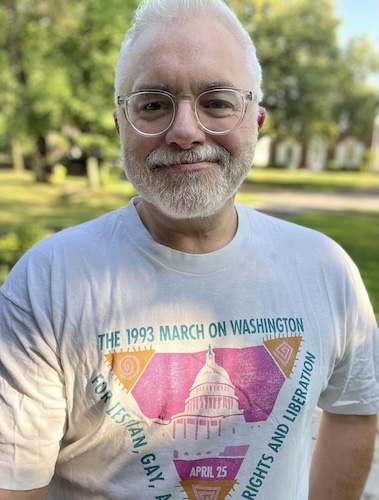
What I do for a living is where I find my joy. I am an opera singer, so anything voice-related brings me a lot of joy and passion. I have a social media presence where I talk about opera. I go to work and sing opera, come home, listen to opera, and talk about opera.
It’s what I do, I’m the opera man.
The subtle lump under my jaw
I didn’t initially know anything was off. I had a little lump under my neck for a couple of years. When I had a cold, I could feel it get a little bigger, but then it would shrink. It was about the size of a pea.
Over the last year and a half, that little pea became a bit bigger and more pronounced. I had also lost 50 or 60 pounds on purpose over a couple of years, so my face shrank and the bump became more pronounced.
I found an ENT and went to the doctor. He biopsied it, saying, “It’s probably benign.” The biopsy showed it was a benign tumor, but that it should come out because sometimes they later cause problems. We scheduled surgery to remove it.
Three days later, he called to tell me it was cancerous.
How we confirmed my salivary gland cancer [carcinoma ex pleomorphic adenoma] diagnosis
The cancer was rare because this type, carcinoma ex pleomorphic adenoma, happens when a benign tumor’s cells convert to cancer. That’s the nature of this cancer: the conversion happens after benign removal.
At first, we didn’t know exactly what kind of cancer it was. More testing was needed to make a clear diagnosis.
My ENT recommended I see a cancer ENT doctor who specializes in head and neck cancer. We did a CT scan and a PET scan and waited for the tumor board to review my case. The board meets every Monday to discuss cases and choose the best procedures.
They decided the best course was a neck dissection to remove as many lymph nodes as possible and determine if the cancer had spread.
A few weeks later, I had the neck dissection. The doctor said there was no cancer in any of the lymph nodes they removed. That meant subsequent radiation could focus on one localized spot instead of a wide field.
The surgery was successful. There was no pain, just a small scar. Healing took a week or two.
They wanted to act fast because it’s a high-density cancer, which can sometimes metastasize and be difficult to treat.
How my diagnosis impacted me
I was shocked. I absolutely was not expecting it.
I remember I was on the phone in my room, and the doctor was talking to me, and all of a sudden I couldn’t hear him anymore. I was just lost in the word “cancer.”
My family is large, but the only person who ever went through any kind of cancer diagnosis was my grandfather, who had pancreatic cancer when I was seven. Up until then, my family had dealt with heart issues, cholesterol, diabetes… conditions I’m familiar with.
Fourteen years ago, I had a heart attack, and that set me on a healthy trajectory. Cancer wasn’t really on my radar.
My treatment plan
By July or early August, my doctor said the course was to start radiation once I’d healed from the neck dissection. He said head and neck cancers generally aren’t treated with chemotherapy, and thankfully, I didn’t need chemotherapy, just radiation.
The challenge was timing. My contract year at the opera starts in August, right when rehearsals and preparations for opening night begin. I sing at the opera house, a church, and a synagogue, which are busy during High Holy Days. I had to consider how radiation would affect my voice, energy, ability to work, and whether I should just go on disability. But I wanted to start as soon as possible and get treatment out of the way.
He told me I’d need 33 sessions over about six and a half weeks, Monday through Friday.
After a short vacation in mid-August, I returned and started radiation immediately, continuing through late September.
My radiation therapy regimen and side effects
For the first week or two, I felt almost nothing; my mouth was just a little dry.
The first symptom was tooth sensitivity on the treated side, making brushing difficult. Then, mouth sores developed, making eating and swallowing painful. That side of my face became very red and swollen. My ear turned bright red, with sores inside it. I still feel a sound back there, waiting for it to heal.
The most profound effect was losing taste and smell. By the third week, food tasted like metal or chemicals, and then I completely lost both senses. Even now, they haven’t returned.
Thankfully, radiation did not affect my ability to sing. I fulfilled all my contracts at the opera house, synagogue, and church through the holidays. Some days were tough thanks to fatigue, throat pain, and body aches, but my workplace was supportive and never pressured me to come in.
Radiation became my daily routine. Treatments were at 9:30 a.m. I walked the dog, drank coffee (which tasted like nothing), biked or drove to the hospital, then did my treatment; just six or seven minutes. I’d return and start my day.
Once, I got the stomach flu for nine days and missed one day, but even when busy with temple singing for Yom Kippur, I arranged treatment around my schedule to avoid missing a session.
I rang the radiation bell
During radiation, you wait with others having treatment and develop relationships. I saw others ring the bell and say goodbye; I looked forward to my turn.
Last week was my final treatment, and I rang the bell.
The hardest part: loss of taste and smell
The loss of taste has been the most difficult part. During COVID, I lost my ability to taste for a week and thought I’d lose my mind. Now, unable to eat normally, it changes everything psychologically. I eat bananas and plain bread daily; food is flavorless or tastes bad, with a metallic or “vacant warehouse” chemical kind of taste.
It has been difficult, but life has thrown me challenges before, like a heart attack, losing a partner, and a severe leg injury. Each challenge showed me my resilience and helped me change my mindset to focus on positivity and what brings joy.
Remembering my resilience gives me confidence that I’ll get through this, too.
I have a strong support system: my friends, community, and partner
I have an incredible support network. Dozens of friends are around to help, including through a meal train (despite my loss of taste), people praying, and offering to help.
My boyfriend has been by my side every day, always asking how to help and making sure I get nutrient-dense food. My biggest strength is having him there for me.
I don’t know how people do this alone.
No evidence of disease: scan results and confidence
Hearing “no evidence of disease” felt incredible. I worried about spread, but the PET scan and neck dissection showed no cancer in the lymph nodes. This gave me confidence moving forward. I knew what I was dealing with and could focus on healing and ringing that radiation bell.
Now, I’ll see my ENT for follow-up in a couple of weeks, with scans and exams every three months for the first year, then every six months.
What I want others to know
When I was diagnosed, I read extensively and found out I wouldn’t need chemotherapy, and the cancer hadn’t spread. I thought I had an “easy cancer,” but that mindset diminishes the disease. Cancer is cancer, no matter the type or how “mild” it may seem. Surviving is surviving.
Nutrition during radiation is different. I eat healthy generally, but during treatment, you eat for medicine, not pleasure. When taste is gone, I eat for healing: protein drinks, soft and bland foods, and whatever my body can tolerate.
With each challenge, I ask what I’ve learned and how to look forward, not back. This experience motivates me to live a healthy lifestyle and plan for an early retirement, to enjoy life while still healthy.
Survivorship means continuing the life I’ve built and shaping my future; travel, new environments, and embracing change. I want to live as a survivor of life, not just cancer.
Being intimate and addressing changes in libido are part of healing, too. Finding someone understanding to talk to is crucial for physical and mental health. Gilda’s Club in Chicago is a great resource, providing emotional, physical, and financial support, nutrition and relationship classes, and more. Men and anyone with cancer should find organizations offering emotional and social support.

Inspired by John's story?
Share your story, too!
More Head and Neck Cancer Stories
Vikki F., Head and Neck Cancer (Nasal Squamous Cell Carcinoma)
Symptoms: Nosebleeds that persisted for years, nose changed in shape, nasal pain, migraines
Treatments: Surgeries (subtotal rhinectomy, reconstruction surgery including radial forearm free flap, bone grafts, and cartilage), chemoradiation
...
Alyssa N., Adenoid Cystic Carcinoma
Symptoms: Persistent jaw pain, lightning-like facial pain during the first bite of meals
Treatments: Surgery (tumor removal), radiation
...
Eva G., Oral Cancer, Stage 4
Symptoms: Sore on the tongue, which caused pain during eating and speaking; changes in the color and texture of the tissue where the sore was located
Treatments: Surgery (partial glossectomy, radical neck dissection, reconstruction), radiation
...
Teresa B., Recurrent Breast Cancer (Hormone-Positive), Oral Cancer (Lip Cancer), and Skin Cancer (Melanoma)
Symptoms: Lip cancer: chapped lips & a pimple-like growth on lip, breast cancer: enlarged left breast with lump, melanoma: none
Treatments: Surgeries (bilateral mastectomy with reconstruction, lumpectomy, craniotomy, Mohs, surgery, wide local excision), hormone therapy, radiation therapy
...
Kandi B., Adenoid Cystic Carcinoma, Stage 3
Symptoms: Fatigue, headaches, depression, occasional feeling of tongue being on fire or inflamed, appearance of tumor on salivary gland on tongue
Treatment: Surgery
...