Starr’s Stage 4 Colon Cancer Story Highlights the Importance of Second Opinions
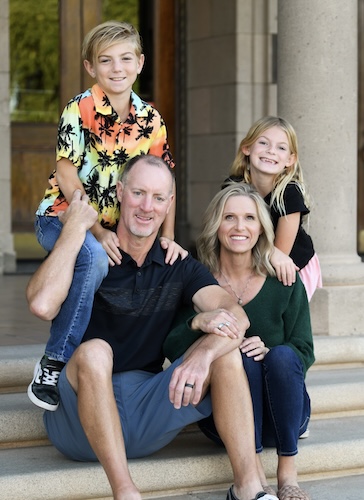
At 44, Starr was living a busy, joyful life centered on her kids. “I’m most passionate about my kids,” she said. “Whatever they’re into, that’s what we’re doing. So whatever sports or school activities we’re going to, we’re always running kids somewhere, doing something with them, or having friends over.” She felt healthy and strong, but that changed when she was diagnosed with stage 4 colon cancer that had already spread to her liver and other areas. Her journey toward remission highlights self-advocacy, community, and a whole-body approach to care.
Interviewed by: Carly Knowlton
Edited by: Chris Sanchez & Jeff Forslund
It all began with mild abdominal pain that didn’t feel right. Even though Starr was young and seemingly healthy, she trusted her instincts and insisted on getting scans after her primary doctor thought it could just be a UTI. Those scans revealed multiple liver masses, setting off a flurry of ER visits, biopsies, and the life-altering words: “stage 4 colon cancer.”

From the start, Starr understood that conventional medicine was crucial, but she also embraced alternative therapies and integrative medicine strategies. While her first oncologist focused solely on aggressive chemotherapy, Starr listened to her body and her intuition. She sought multiple opinions, discovered targeted therapy, and explored supplements, nutrition, and emotional wellness. This approach not only helped her endure treatment but also prepared her for two major surgeries, which successfully removed her colon and liver tumors.
Throughout the process, Starr leaned into self-advocacy. She didn’t stop at one opinion; she asked the hard questions, researched options, and refused to settle for a plan that didn’t feel right. Her persistence led to care that respected her voice and ultimately helped her move into remission.
Starr’s reflection on awareness is equally powerful. Colon cancer doesn’t always require a family history or obvious risk factors. Starr exercised, drank her green juices, and maintained a healthy weight, but she still got cancer. Her story is a gentle but firm nudge for everyone to listen to their bodies, stay proactive, and seek medical advice even if they believe they’re too young or too healthy to get sick.
Today, Starr calls herself a survivor and a thriver. She’s committed to living her days with gratitude and presence. She celebrates being able to take her kids to school, enjoy nature, and fill her calendar with meaningful experiences. She wants to remind us that while colon cancer might change your life, it doesn’t define it. You can nourish your body, advocate for yourself, and still live fully.
Watch Starr’s video and scroll down to read through the transcript of her interview for more on her story. You’ll learn about:
- How she felt healthy, but still got stage 4 colon cancer
- Why Starr refused to settle for one doctor’s plan
- The whole-body approach that changed everything
- How self-advocacy can save more than your life; it can save your hope
- Living fully after colon cancer remission
- Name: Starr S.
- Age at Diagnosis:
- 44
- Diagnosis:
- Colon Cancer
- Staging:
- Stage 4
- Symptom:
- Abdominal pain
- Treatments:
- Chemotherapy
- Surgeries: colectomy, hepatectomy, lymphadenectomy
- Targeted therapy
This interview has been edited for clarity and length. This is not medical advice. Please consult with your healthcare provider to make informed treatment decisions.
The views and opinions expressed in this interview do not necessarily reflect those of The Patient Story.
- My name is Starr
- When I first started feeling “off”
- The moment everything changed
- What side effects I experienced
- Finding the right care team
- I was able to get surgery
- The value of multiple opinions
- How my diagnosis impacted my kids
- The hardest part of my diagnosis
- How my identity has shifted after my diagnosis
- Reaching no evidence of disease
- My support system
- What I want others to know
My name is Starr
I’m 45 years old. I was diagnosed last year with colon cancer. Stage four, because it metastasized to my liver and other locations. And I live here in Arizona.
I’m most passionate about my kids. Whatever they’re into, that’s what we’re doing. So whatever sports school activities we’re going to, we’re always running kids somewhere, doing something with them, or having friends over. Our lives revolve around the kids, which is how it should be. I love it.
When I first started feeling “off”
I was having a little bit of abdominal pain, and I thought, “Okay, well, this just doesn’t feel quite right.” As soon as I got the abdominal pain, I was like, “I’m going to urgent care.” So it was like two days. So I’m glad I didn’t waste time.
They thought it was UTI. I went to my primary school. I got a scan, and it showed all these masses in my liver. She wasn’t too concerned because of my age. Just being young. And I was healthy, too, but I wanted to do a CT or MRI or PET scan or something. And she said, “Okay, well, to ease your mind. Yes, of course, we’ll do the scan.”
The moment everything changed
That’s kind of a life-altering moment for sure. But I went to my follow-up appointment to go over the scan with my doctor, and she said that, you know, I almost had your husband come in with you for this to go over this, but because she personally knows my husband. But let him come in, and she said, You need to go to the emergency room right now. I have someone there. They will meet you.
So she got me right into the emergency room and set me up with somebody so I didn’t have to wait. And then they did the biopsy there at the hospital, and I found out very quickly. So it all happened really fast. They said, “It’s cancer in your liver, and it’s not the primary location. It actually started somewhere else.”
So that was all of a sudden. Not only did I have cancer, but I had metastatic stage 4 cancer. And it didn’t even start in my liver. It’s spread. It’s in other locations in your body as well. So, I just remember being in the hospital, and thank goodness my friend was with me, and she’s like, I’m going to get your husband down here now. He’s coming down. And it was very scary.
When you hear the words “stage 4” and “terminal,” that’s almost an out-of-body experience.
My treatment plan
My first oncologist was just focused on chemo. Regarding surgery, she was like, “Let’s not even talk about it, because we’re not there. You’re not even close to surgery. It is not an option. Maybe it will be, down the road, but for now, it’s in too many locations and the masses. We need to get the tumors down.”
I did five different treatments for chemo. One is a targeted therapy. I did the intense chemo for eight rounds.
What side effects I experienced
The biggest side effect was the most intense fatigue that you can imagine. I mean, even just talking, I’m sitting there trying to talk to somebody, and it’s just too much effort. Just, you know, keeping my eyes open. I had so much fatigue and nausea. I didn’t want to eat. I lost a lot of weight — over 30 pounds. And I didn’t have a ton to spare.
I also had pretty intense neuropathy in my feet. It’s still there. It could be permanent. I’m working on trying to fix that.
At one point, my skin was peeling off my hands and my feet because of one of the chemos that I was doing. It didn’t really hurt, but it was just really creepy to have your skin just falling off your body.
Right now, from the targeted therapy, I have a red rash. The skin is not like it should be. All through my back, my face, my chest, my stomach. So that’s an ongoing one.
I wouldn’t just be tired but exhausted beyond belief, and I would do the chemo treatments. So it would be like a week of just being down. I’m on the couch, I’m on the bed. I’m not going anywhere. I’m not doing anything. I’m not really eating due to the nausea. Because if I eat, then I throw up. So I want to avoid that. And then after that week, I just start feeling better. More normal. And then the second week would be closer to normal life, but still tired and all that.
But literally half the time, I was just completely not there, just not living my life. And it was really hard. And for my kids to sit there and see their mommy on the couch and go, “We’re going to go out and play,” and I couldn’t even get up to go out there and be with them. So I was losing a lot of time with them.
It was over four months total; I did eight rounds of that. And then after that point, I switched oncologists.
Finding the right care team
My original oncologist wanted to just continue that treatment regimen. And what I kept on hearing from not just him, but also from my second and third opinions, was that this is the standard of care. You continue doing chemo until it stops working, and then we switch. And to me, that didn’t sit right in my brain. So you want me to continue doing something that feels like it’s killing me.
I met my current oncologist at City of Hope, Orange County. He gave me information that I didn’t know about. “Hey, your liver is enlarging because of the chemo.” My oncologist never said that. When I went to a second opinion at MD Anderson, they gave me information that my oncologist hadn’t told me either, that it was also in my peritoneum and lymph nodes. The communication wasn’t quite there with the first one.
He recommended that I stop chemo. We talked about targeted therapy, and that’s what I did. And everything changed after that.
I would take six pills a day. Three in the morning, three at night. And then the biggest thing was I would get infusions every other week.
I was able to get surgery
Every past oncologist told me, “You know, surgery is not an option. Continue with chemo.” But I was able to have the surgery thanks to the targeted therapy.
I started with the new oncologist at the end of November 2024. And I had my first surgery at the end of January. Just two months later. He was able to remove the colon, lymph nodes, and the left side of the liver. And then we waited two months. And then in March 2025, I had my second surgery, which took care of the right side of my liver. It actually had more tumors in it.
But the amazing part is that in both surgeries, when they took out all of the cancer, it was between 95% and 100% dead already. These numbers are amazing. I see numbers that are between 10 and 30% and those are already great numbers. And then when I had the second surgery, 99 to 100% of the cancer was dead.
So the targeted therapy was working. And they just went in with the surgeries and got it out.
I was there for 4 or 5 days. You know, it was an intense surgery. They did a lot. And I have the scar to prove it. I got my warrior scar; I deserve it.
Luckily, I had friends with me. My husband kind of rotated because it was out of state. All my care has been out of state; it’s not just 15 minutes down the road to the hospital or something. To get to the cancer center, I would have had to drive for hours or fly. But it was great to have. I needed support from my husband. Being in the hospital, that’s not fun. A lot of people have a recovery time. I mean, I’m still recovering at six months out. Having all that done to your body is a lot. So just recovery time was a lot of couch and bed time, that’s for sure.
I was not in the mood to eat. They did a good job of getting me up. You know, day one, moving around. I didn’t really want to a couple of times, but they got me moving around, which I think was really best for me. This is good for me. Keep on going. But eating, getting food into my body, was difficult.
My kids made this big welcome home sign. Mostly my daughter did it, but my son helped. But yeah, they made this great sign. It was after my first surgery. I got to come home, and then they were just standing there with the welcome sign, and that was really sweet. I cried, of course.
The value of multiple opinions
I recommend getting a second, even a third opinion. You know, technically, I started with my small-town oncologist. I was sure I wasn’t going to stay here in a small town. Then I went to San Diego and got another opinion in Texas, and then went back to California, where I am now.
So, absolutely get second opinions. Get third opinions if you can. I also called a bunch of other places that I never got in with because they were so far out. So I was looking at other people calling, making other calls, because I just didn’t feel right.
I think that I would have been doing that intense chemo for months, and who knows where that would have led me. It would have knocked me down so much that I couldn’t recover and move on to the next thing. Or maybe it just would have been, yes, more chemo and months worth of that agony. And then maybe the doctor would finally have switched me to this other targeted therapy, and I could have ended up in the same place. I don’t know. But I do know that I would have wasted time.
I did call a cancer coach. And it was interesting. She gave me a lot of information. “Hey, do you want to travel to New York and get a third opinion?” And that helped me open my mind to the possibilities. Wow, I really don’t have to just do what this one doctor in a lab coat says, just because they’re the doctor. There are other options. And she was talking about all these things and possibly even getting treated in other countries. She opened my eyes to different trials and things out there that nobody was telling me about. That helped me be a little bit more courageous and open to the idea that I don’t have to just listen to this one person. “Yeah, you know, you’re doing chemo, and it seems like the tumors are shrinking.” That’s great. But you don’t have to just listen to one person.
How my diagnosis impacted my kids
That was a big question: how much should we tell them? I wanted to be open. My kids were nine and 11, and I wanted them to know what was going on. I wanted them to know why their mommy was on the couch all the time, why I didn’t feel good. And they needed to know that I needed their help.
The main thing was, yes, I missed out on a lot of time. We would try to do things around the couch, or maybe do a puzzle or watch movies. We’d try to do whatever activities we could. But it was harder missing their games and not being able to take them to school and having my husband do that instead. Just missing out on a lot.
But we did our best. And I made them into little runners. They would run and get mommy a blanket, a pillow, water, or food. They were great helpers, but I wanted to be as open and honest as the kids could understand, but not terrify them, because I was terrified that I was going to die. And so I didn’t. I said, “Mommy’s sick.” And yes, people do die from cancer, but I don’t think that’s going to be me. So they were going to think that mommy’s going to be okay, but I’m just not the same right now. And I’m going to need your help. And they stepped up.
So in a way, it’s kind of a little gift. It’s kind of good for them because they learned to be more empathetic and more sympathetic. So learning a little bit more responsibility, needing to help out more, carrying things because I couldn’t carry anything. They were carrying everything for me. So in a way, they’ve grown a little bit from this, too.
The hardest part of my diagnosis
The hardest part was the weight of getting the initial diagnosis. Stage 4 terminal cancer. What does that mean? Am I going to beat this or not? That was really low.
After going and seeing that second opinion, when they told me, “Oh, we would do the same thing,” and I hoped I’d walk away with a magic pill or something for me, but they didn’t have anything for me, and then learning that it was also in my lymph nodes, which in my mind meant that I was done because it can travel anywhere — that was a really low point. And that’s when I made goodbye videos to my kids, which was hard.
I’m glad I did, because I can look back at them and think, “Wow, I was on the verge of saying goodbye to my kids and my husband.” That was probably the lowest point — coming to terms with having to make these videos.
I had actually put on makeup and fixed up my hair so that it was a good video for them. I didn’t want them to think, “Mommy looks really sick and bad.” They were going to have those videos forever.
I told my husband, “You can remarry, but I know you’re not going to.” He responded, “I’m not getting married again. I’m glad I made it so wonderful this first round.”
So I made those videos, and I’m glad I did, because I have them, and I can look back and be like, “Wow, that was me in a really not a good place to come to that point, to say goodbye.”
How my identity has shifted after my diagnosis
My identity has changed immensely. Not only my lifestyle, but also starting with that. Like the things that I eat, I put in my body what I put on my body. I avoid processed food and eating out a lot. Cutting out alcohol, cutting down on sugars and meat.
But the biggest thing is that my outlook on life is completely different. When I was sitting there, you know, just wanting to go outside and just sit outside, and I couldn’t do that. So now, I treat every day like it’s so precious. I want to squeeze so much out of every day. I have to do this, I have to do that. What’s my to-do list? Got to go to work. Got to get the kids to school. Got to do. Gotta check off that list. Now it’s like, I get to take my kids to school. I get to go to work. I get to go to the grocery store. I get to watch a movie. I get to go outside and listen to birds and waste time.
And so my biggest realization is that you don’t know how long you’re going to be here. And people say that all the time, but it doesn’t sink in until you truly face death. And this could all be over very soon, was what was going through my mind. So when you have that, then you just really appreciate everything.
And now I’m in remission, I’m filling my calendar with all these places that I want to go, things I want to do, friends I haven’t seen. I am just filling it up with things that I really want to do. Versus, wow, why did I fill up my calendar with stuff I didn’t really want to do or waste time doing, when I could have been enjoying more time with my kids or my husband or just reading a book?
I’ve definitely gotten more in touch with myself and my emotions. My whole identity has really shifted to being grateful, taking care of my body, and helping others. Now, that’s what I want to do, pay it forward. And my outlook on life is so much better.
Reaching no evidence of disease
I had a clear first scan after my second surgery, and it showed nothing on there, which was amazing. It’s funny. I didn’t even let that enter my mind because I was just thinking, “We just want to see that the tumors are gone.” But in my mind, it didn’t add up to the possibility that I could be cancer-free. Like, I didn’t let myself get my hopes up.
I finally talked to my oncologist, and he said, “Yes, we don’t see anything, but we have to do these other bloodwork tests.” I remember I was at Sea World with my family, and I got the email, and thought, “Should I open it now? Because this could be good or bad. Okay, I think it’s going to be good. But either way, I want the information. I’m doing well, and I think it’s going to be good.”
I just looked at it and I saw the number zero, indicating no tumors. And that was the moment I thought, “Wow, I think I’m in remission.”
I had my appointment the following week, and then I was like, “Can I say I’m in remission?” And he said, “Yes.” So I knew it a little bit. And it was slow, it wasn’t like, boom, a moment you faint or like scream or something. It was definitely wonderful to hear those words out of his mouth and then to share them with everybody.
I immediately called my husband and a couple of close friends. I sent it to my girlfriend star squad, those girls who have been helping me through this and taking care of me. I let them know. And then I was like, “I’m going to put it on Instagram and tell the world, because this is great news.”
It’s still sinking in, but yeah. It’s amazing.
My support system
My husband, my kids, they’re the reason why I’m here. I fought so hard for them. I want to see my kids grow up. I want to experience all that. And it’s wonderful. I was in the mindset for a while that I’m not going to see them even drive or go to their first dance, or first kiss. And I believe that I will now.
I had my star squad, the smaller group, 12 women, in a group text. It would be like, “Okay, who’s going with Starr to this treatment?” “I’m going to drop off some food.” “Do you need any help with the kids?” Words of encouragement. And then I had two or three friends who were just there every single day. How? Constantly checking in on me. Showing up, even being there when I didn’t know I needed them.
Talking through things and just having that girlfriend connection that you need. So not only taking care of me physically and all the things that I need, but mentally, it was just to let emotions out.
What I want others to know
One of my books talks about radical remission, radical hope. This thing is amazing. It just gets into not only supplements and good food, but also all these other things that you can be doing. Nourish yourself as a whole, not just physically, but also emotionally, spiritually, and mentally. It’s your outlook. Oh my gosh, that could be half the battle right there.
I had stage four terminal cancer; I could have thought that I’m not going to make it. Not to say that I didn’t get in that mental space, of course, I did at some portions throughout this, but I’ve tried to stay as positive as possible. And I think that really, really helps.
I read in these books about people experiencing spontaneous remission. Reading about somebody who was literally put in hospice and they were expected to die in a week or two — but they don’t, and they’re still living many years later. And really, if they can do it, I can do it.
People want to hear that. People need to hear that. Just because you’re given this diagnosis doesn’t mean that you’re going to die. You can beat it. You can live a much longer life than the doctor said.
You’re your own statistic. You are your own person. You can really do a lot of things in your life, rather than just taking chemo and radiation or even just food supplements that you’re putting in your body. There’s more that you can do. And I want people to know that you can empower yourself. You can really change the odds. Those stats in my mind went from, “Oh, you have a 15% chance to live to 85 or 90, to: I expect to be here in five years.”
I really have the mindset and the changes that I made. I want people to know that it’s not a death sentence. People are getting cancer younger and younger. Even though you’re young and you think you’re healthy. And that’s what I thought I was. I drank the green drinks. I went, I exercised. I kept my body weight down. And I thought I was healthy, and wow.
Cancer made me really look at my life and realize that I had a lot of imbalances. And I thought, “Maybe I should address those. This is cancer; it is my wake-up call. Let’s not focus on the fact that I have cancer. Why did I get cancer in the first place? What are the things that I can change in my life? To not only beat the cancer. My goal now is to stay in remission, to not let it come back.” And so I need to really nourish my body in multiple ways.
At first, it was uncomfortable. I am a survivor, I am a warrior, and I am a thriver. And I’m proud of that because I’ve been through a lot. What’s scary about it is that at my next scan in three months, I could have cancer back. You know, it can come back at any point. I really do believe that I’m going to be okay. But there is that chance that it’s going to come back and that I will need to continue this battle. But survivorship to me is just a wonderful feeling. And I hope that other people take some hope from this, that this can be you, too. You can do it. And you can be a survivor, a thriver, and a warrior too.
And in the meantime, whether you have cancer or not, just live your life.

Inspired by Starr's story?
Share your story, too!
More Metastatic Colon Cancer Stories
Raquel A., Colorectal Cancer, Stage 4
Symptoms: Frequent bowel movements, pin-thin stools, mild red blood in stool
Treatment: Chemotherapy
Steve S., Colorectal Cancer, Stage 4
Symptoms: Blood in stool, changes in bowel habits, feeling gassy and bloated
Treatments: Surgery, chemotherapy, monoclonal antibody, liver transplant
Jessica T., BRAF Mutation Colon Cancer, Stage 4
Symptoms: Severe stomach cramps, diarrhea, vomiting, anemia (discovered later)
Treatments: Surgery (hemicolectomy), chemotherapy
Jennifer T., Colon Cancer, Stage 4
Symptoms: Weight loss, coughing, vomiting, sciatica pain, fatigue
Treatments: Surgeries (colectomy, lung wedge resection on both lungs), chemotherapy, immunotherapy
Kasey S., Colon Cancer, Stage 4
Symptoms: Extreme abdominal cramping, mucus in stool, rectal bleeding, black stool, fatigue, weight fluctuations, skin issues (guttate psoriasis)
Treatments: Surgeries (colectomy & salpingectomy), chemotherapy











One reply on “Starr’s Stage 4 Colon Cancer Story Highlights the Importance of Second Opinions”
Hi, can you share the details of your treatment please? Pills / chemo etc. My husband got the same diagnose. Colon plus meta to liver. No symptoms at all! Found by accident before his 50th birthdays. No surgery as an option – we heard the same. He is on chemo ftom Oct 30 2024.