Allison’s Stage 2C Colorectal Cancer Story
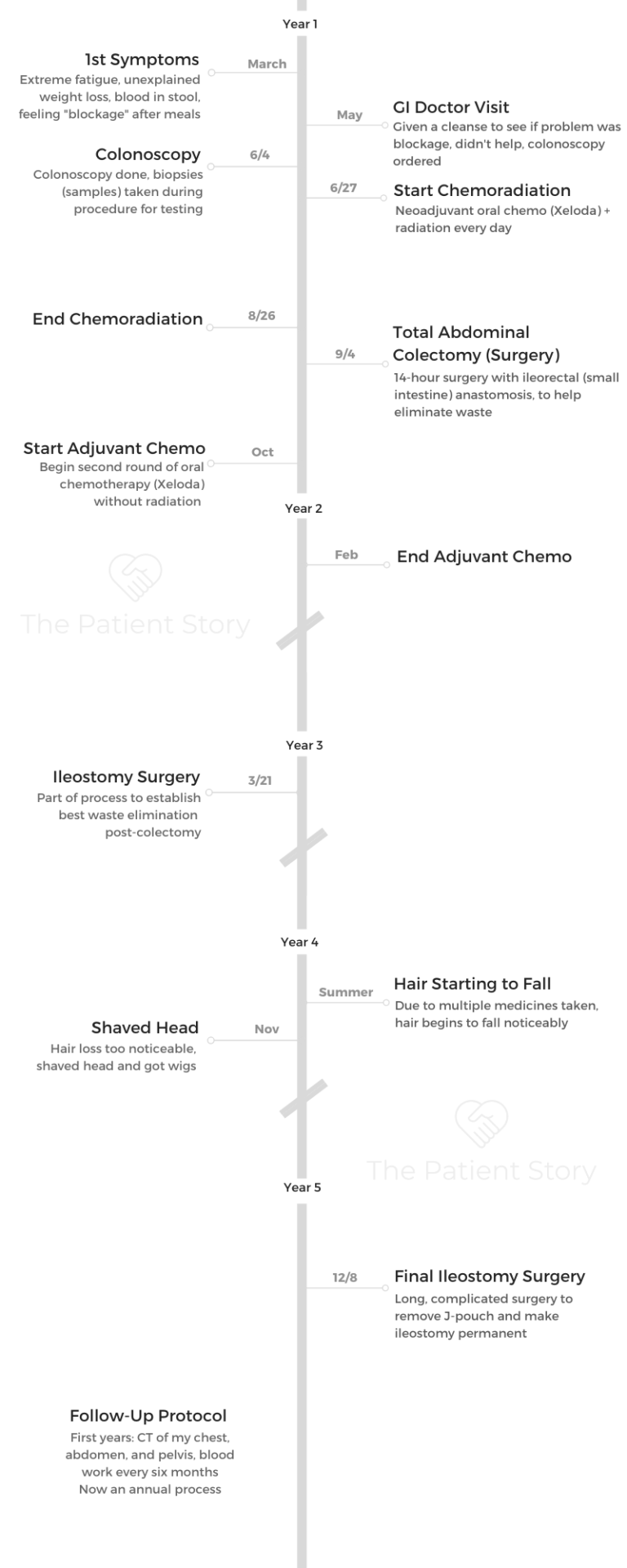
Allison shares her stage 2C colorectal cancer story, which began when she was diagnosed at just 32 years old. She details undergoing treatment, concurrent radiation and oral chemo, a colectomy, chemotherapy, and surgery.
In her story, Allison, who’s now a colorectal cancer patient advocate, also highlights the quality-of-life issues that impacted her most, including managing the issue of fertility preservation, the impact of the cancer diagnosis on her relationships, and finding her cancer community.
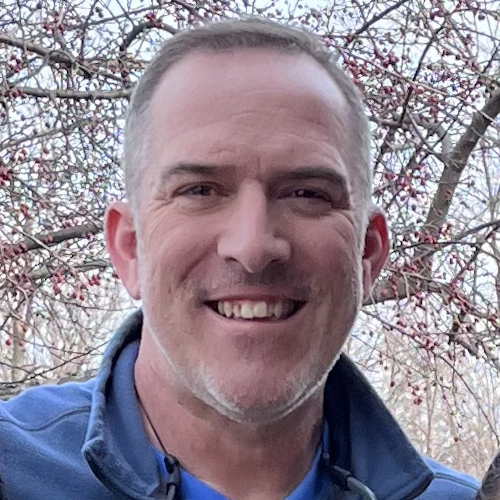
- Name: Allison R.
- Diagnosis (DX):
- Colorectal cancer
- Stage 2C
- Age at DX: 32
- 1st Symptoms:
- Weight loss (unexplained)
- Severe fatigue
- Blood in stool
- Feeling of blockage after eating
- Treatment:
- Concurrent radiation and oral chemo pill (Xeloda or capecitabine)
- Total abdominal colectomy (surgery)
- With ileorectal anastomosis
- Chemotherapy (Xeloda or capecitabine)
- Surgery (to make ileostomy bag permanent)
- Post-Surgery: Ileostomy bag
- Diagnosis
- Treatment Decisions
- Chemotherapy and Radiation
- Surgery (Colectomy)
- How did they assess how and when to move forward with surgery?
- What was the prep before surgery?
- Mentally preparing for surgery and overall treatment
- What do you remember of the actual surgery (colectomy)?
- Tip: have caregivers give updates through surgery and treatment
- Describe waking up from the surgery
- Recovering from major surgery
- Guidance for others on recovery
- Surgery and Ileostomy Bag
- Second Chemo (Xeloda)
- Reflections
This interview has been edited for clarity. This is not medical advice. Please consult with your healthcare provider for treatment decisions.
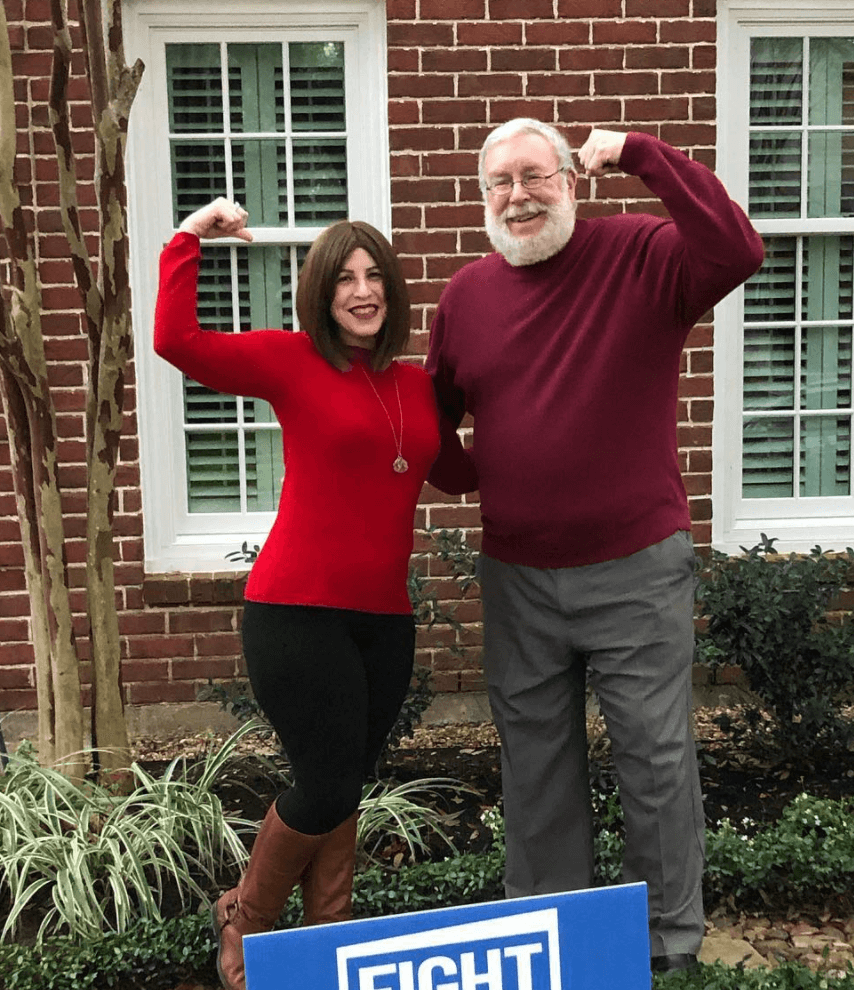
It’s one day at a time. Nobody’s journey is the same, so what you might struggle with, someone else might not struggle with.
But you’re not alone, and take it one day at a time. [These] are the lasting messages I hope can help other people.
Allison R.

Diagnosis
What were the first symptoms?
I was just your average person living life to the fullest, working, having fun with my friends. I actually have Crohn’s disease, so I’m really in tune with my bowel habits. I have taken all sorts of medicine.
At that point, I had been in remission for quite some time, so a year and a half earlier I had the cleanest colonoscopy I’d ever had in my life.
I was in the best shape of my life. I was eating well and working out 5 to 7 times a week.
Over the course of a few months, I started to notice subtle changes. I thought the weight loss had to do with my Zumba I was doing, but then there was severe fatigue and increased blood in my stool that I hadn’t really seen before.
The biggest symptom was the fact that I felt when I ate, it felt like something was getting stuck in me. I had never had a blockage in my life for any reason. I was having these symptoms that were unusual for me, so I scheduled an appointment with my GI doctor. I was lucky I had a GI doctor.
Describe the X-ray and colonoscopy
I was supposed to have a colonoscopy maybe a year later. Because of the symptoms I was telling her, instead of scheduling a colonoscopy right away, she had me drink some stuff that helps clean you out to see if maybe I had a blockage. She did an X-ray, and I drank some of that stuff. I felt good for maybe a day.
That was alarming to her, so she scheduled a colonoscopy for a week after that. I remember waking up, and she said, “I found something. I don’t know what it is. I don’t think it’s cancer, but we took some biopsies.”
That was what led up to me getting screened. Those symptoms, but also me being my own advocate, are the reasons why I got the screening that I needed.
Also, knowing my body really well. A lot of people don’t necessarily pay attention when they go to the bathroom, but I did.
Describe the colonoscopy
In human terms, it’s not the most pleasant experience, but I experience it as a full cleanout of your body.
It’s one of the screening methods for GI doctors to see if anything’s going on in your colon. Essentially, you have a day or 2 of clear liquids.
The day before the procedure, you have to drink this bowel prep. You have to drink this prep that cleans you out. When I say cleans you out, it’s very similar to if you go and get a colonic.
You drink this stuff and go to the bathroom, so by the time you’re done drinking, the only things you see are very clear liquids that are coming out when you go to the bathroom.
That’s so when a GI doctor goes in and does a scope, they put this device up to look in your colon to look for abnormalities — any inflammation, any polyps, any redness or irritation.
They can only do that if you’re clear. There’s nothing that is blocking their view from the insides of your colon.
Do you go under for the colonoscopy?
I always insist on having anesthesia. One time I had a colonoscopy without, and I felt it. There is local anesthesia and a more advanced anesthesia you can get. Those are options you talk to your doctor about, and I always insist on getting that because I don’t want to feel any pain.
There’s extra precautions with that. They have an anesthesiologist come in and talk to you. It is based on your provider and what they suggest, but personally, without giving medical advice, I always want the anesthesia that will put me out so I don’t remember.
I essentially wake up after, and I’ve felt no pain. I don’t really remember anything that happened to me.
How long did the colonoscopy biopsy results take?
Then 2 days later, I got a call from my GI doctor to come to her office as soon as she could give me those results.
Describe how to cope with waiting for results
That wait time was probably on the top 5 list of most stressful things in my life besides cancer, because mentally, not everyone hears “cancer” when they wake up from a colonoscopy. Some people are diagnosed during the colonoscopy. It depends.
She mentioned the word. “I don’t think it’s cancer, but I did some biopsies.” Some people, that day of the procedure, get diagnosed, but anyone who has to wait for any sort of results… I dived into work. I tried to distract myself. I kept myself busy as much as I possibly could.
But in the back of my mind, I’m hearing, ‘Cancer. Cancer. Cancer.’
It’s the fear of the unknown. Your life is in the hands of someone else and not yours.
»MORE: Dealing with scanxiety and waiting for results
Describe what happened at the GI office
She’d never called me before, so the fact that she called my cell while I was at work during the middle of the afternoon — I get the phone call, and I know. She didn’t even have to tell me. I know that I’m about to go through the worst journey of my life, the biggest challenge I’ve ever faced.
I walk over to her office from work. I work in a research lab, so I was in the middle of a project and told one of my friends that there was an emergency. Could they take over? I walked across the street on the phone with my mom and was crying. I got to the office. They put me in a separate room.
That’s when my life changed forever.
I was told I had stage 3 colorectal cancer and I should try to find an oncologist and surgeon as soon as possible. Because I had had the colonoscopy a year and a half earlier that was clean, they thought it was pretty aggressive.

How did you process the diagnosis?
I don’t think I did. For maybe a minute, my life flashed before my eyes. I had experience in my lab with different cancers and whatnot that I did as far as research was concerned, but I never thought cancer would happen to me.
I vividly remembered flashbacks from when I was a kid to a day earlier or a week or month or year earlier, to all these great times I had. Then I stopped myself from that and realized, “Okay, I’m tunnel-visioned.”
I need to do what I need to do to find doctors so they can get this cancer taken care of, out of me, and prepare myself for the fight of my life.
It’s really fight or flight in a way. I was sad, don’t get me wrong. I cried for probably days after, even hours after, even when I was sitting there.
But I knew that I was young, I was healthy, I was strong, and I could get through this.
Treatment Decisions
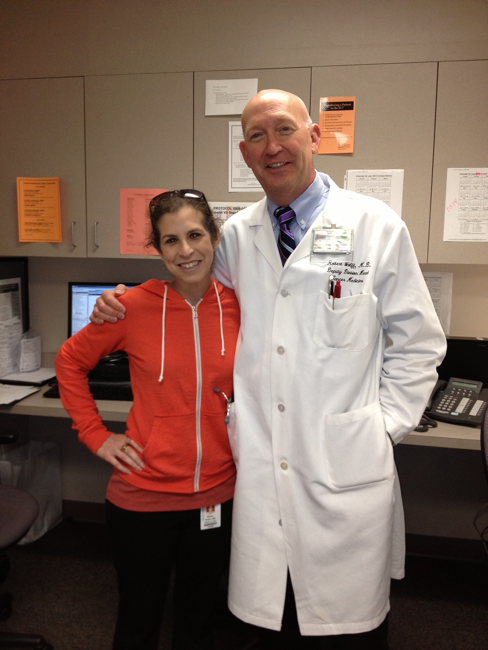
How did you find your medical team (oncologist and surgeon)?
I’m a little bit different because I work in the Texas Medical Center, so I went home, and I process the information. What I did was I asked friends, I asked colleagues, and I asked people who I knew who had any sort of experience with cancer about the best institutions possible.
I got as many opinions as I could get. I got 3 opinions at different institutions. Let me tell you, maybe the treatment was similar, but the surgical options were very different.
I also knew of a friend of a friend who I had thought had just gone through colorectal cancer treatment, so I reached out to my friend to connect me with this person. I knew nobody that had colorectal cancer, and I definitely didn’t know anybody young.
This girl was a year younger than me in my high school, so I reached out to her, as well as my best friend who worked in cancer research, to try to get as many opinions as possible.
It’s one of the hardest things because you want the best care. I tried not to go to Google because there’s too much information out there that possibly could be unreliable. I really tried to find people who knew people who had gone through any sort of cancer and ask them, “Okay, who do you suggest? What do you think?”
I took tons of notes. I was just lucky that someone that had worked in my research lab was working in colon cancer and the GI department at MD Anderson, so they had a suggestion for somebody. I worked at Baylor College of Medicine, so I knew people at Baylor who could help get me in.
If you don’t have connections, reach out via social media to maybe someone who knows somebody, because when you’re diagnosed, people just want to help you.
One way that people can help you is to give you suggestions on whom to see. Who best to help you than someone who’s gone through the journey themselves?
What helped you decide which medical provider to go to?
All the hospitals I went to were amazing. All the doctors were amazing, but it was one thing that my oncologist said to me that made me want to go to him.
It was, ‘Allison, you are young. I don’t want you to feel like you’re just a number. I want to make sure you understand that I am caring for you and you only. When I’m looking at your chart and treatment plan, it’s for you. I don’t want you to get lost in the cracks. Here is my cell phone number if you need anything.’
I have yet to use that cell phone number, but that level of trust that he had in me made me have that in him. I don’t think every doctor would give their cell phone number to a patient, but I think he knew I wasn’t going to call him all the time.
In these big institutions and cancer centers, you get a medical record number. You feel you’re one in a million people being treated there.
But knowing that he wanted to ensure that I would not get lost in the cracks and my treatment, my case, me as a person mattered. That’s why I went to that oncologist and got my treatment at MD Anderson.
What was the treatment plan?
I had the first real appointment with my oncologist and my surgeon. Standard of care for someone with my diagnosis was going to be 5.5 weeks of combination chemotherapy and radiation, a little bit of a break, then surgery.
Surgery could range for so many different things. It just depended on what they found inside. Surgery and then chemotherapy again.
That’s very, very broad, but that’s what standard of care was for colorectal cancer. I say colorectal cancer because my tumor was not only in my colon, but also in my rectal area. It was a 13-centimeter tumor they found that wasn’t in just one organ.
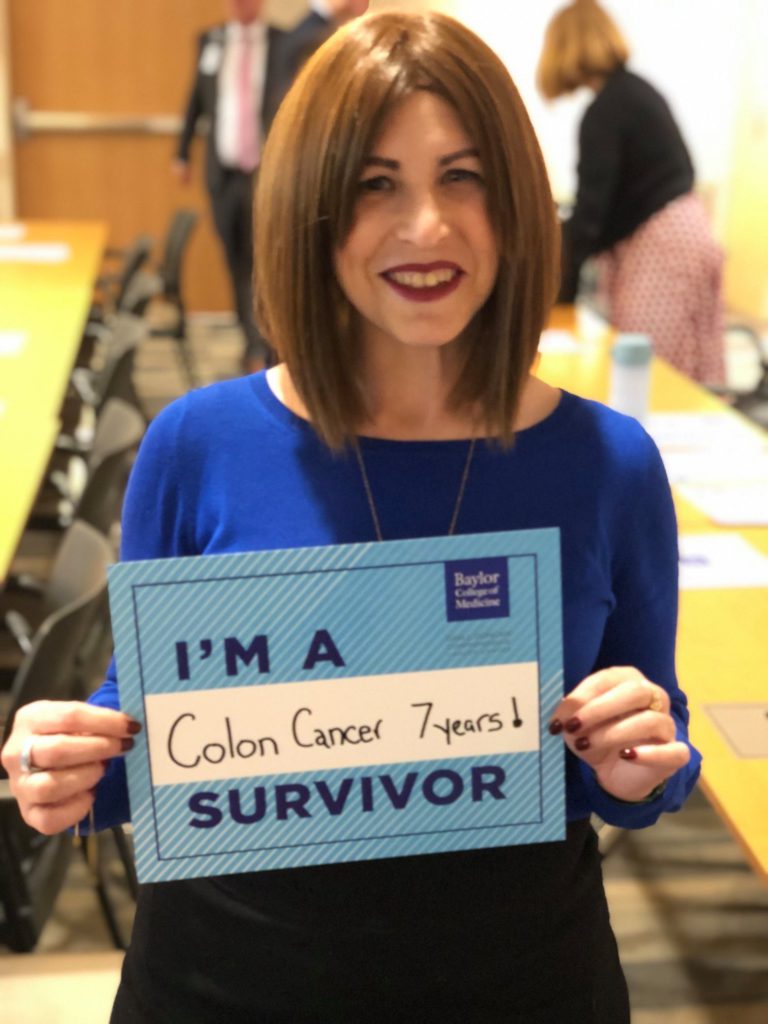
How did it get restaged from 3 to 2C?
I went through radiation and chemo without knowing anything, so that’s another fear. You don’t know. I had my scans, obviously, but I had no idea that cancer is growing in me. Is it not growing in me? You don’t know if your treatment is actually working.
It wasn’t until I had my first surgery after that in September that I was opened up that they realized the lymph nodes they first thought were involved were only inflamed. It was just inflammation.
It had not gotten into my lymph nodes or spread in my body, so it was downgraded to 2C, which is better. It’s always better to be downgraded than upgraded, and it’s rare that it happens.
Chemotherapy and Radiation
Overall treatment
I don’t want to say my chemotherapy was easier than others, but it was.
It wasn’t IV chemo. It was a pill chemo. I still had lots of different side effects.
The same time I was going in for radiation every day, I was also taking this chemotherapy drug. It’s to tackle the cancer in 2 different ways at once.
Every day I was working through this, but 5:30 p.m. I would go over to the hospital. They tattooed me when I was first diagnosed, and I would get radiation to my abdominal area, specifically targeted to where my tumor was. At the same time, I was taking this chemotherapy.

Oral chemo pill
It was called Xeloda. It was regimented. It was quite a long time ago, but I think I took it once a day. I took it throughout the whole time I was doing my radiation. They might have ended it a week earlier than the radiation because of the side effects I was having.
Chemo side effects
My neuropathy got quite bad. Nausea was really bad. You go in often to see your doctors to see if you need to continue on and to see if the side effects and quality of how you’re living are worse.
At that point, while I had been diagnosed and started my chemotherapy and radiation, I was gradually losing a lot of weight.
In order to really do well during any sort of cancer treatment, you have to have some weight on you to be able to fight the effects of all the drugs that you’re having to take.
What helped prevent or lessen those side effects?
Sometimes it’s hard to lessen side effects. They can give you medicine for some of the side effects, but then there are side effects to those side effects. So trying to figure out what worked best for me.
Gloves to help me with the cold and hot sensitivity. I was taking anti-nausea meds and meds to help me sleep because sleep would help. It was one day at a time.
Describe the radiation and side effects
It was 5 times a week. You can’t really control your bowel habits at one point toward the end of that radiation, because it’s pumped into your body.
Whatever tools I could have in my bag of things to help I used. It was a lot of talking to other survivors and patients that helped me figure out what would work best.
They told me to invest in adult diapers, so I did. I invested in adult diapers, and I want to say the last few weeks of radiation, I had to wear those. It’s very hard at that point to control your bowels. The first 2 weeks, it was fine. I was like, “This is no big deal. I’m going to be fine.”
But it got tough, really tough, towards the end.
The one thing they don’t necessarily tell you or don’t explain as well as I would like is the radiation also causes burning, depending on where it is. This is essentially radiation to your skin.
Your personal parts could be red, irritated, could get blisters. There’s creams that might help. I can’t remember all the names of the creams my doctors gave me, but I know the burning and redness would eventually get better. But it was really painful to go to the bathroom anyway.
What helped with the radiation side effects?
What I’m putting in my body made a difference as far as eating. I asked my doctor to refer me to a nutritionist so I could better know. What I was putting in my body would help combat what was essentially coming out.
They told me to do kegels. People say, ‘Oh, I don’t have to do that.’ Oh my gosh, life changing. They really make a difference.
They helped me control that part of my body later on in life throughout the treatment.
They said to do it, and I didn’t necessarily believe it. These muscles aren’t necessarily being used, and they’re being affected heavily during your treatment.
If you don’t use it, you lose it. The more you use it and the more exercises you do, the better outcomes long term.
When a doctor says to do something, if you don’t want to or quite understand, ask why. I was very much that patient that was like, “Why do I have to do this?” Once they explained it, then I was like, “Okay, 100%. I will do it.”
You get so much information all at once that you think you can ignore something, and it turns out to be one of the most important things you can do to help with your long-term side effects.
»MORE: Read other patient experiences with radiation therapy

Surgery (Colectomy)
How did they assess how and when to move forward with surgery?
I didn’t get a scan. Based on their research and since this was standard of care, they knew about how long your body needed to recover in order to go in for surgery.
There was no scan in there because they didn’t want to give me extra radiation to my body since I had just been heavily radiated.
What was the prep before surgery?
You go in, they look at your heart, and they review the anesthesia and review all the surgical options. They don’t know what they’re going to find when they go in, so they could do this or that. They review all the things they could do (surgically) with you.
This is crazy to talk about now, but back then it was a very emotional night. My parents and I sat there and filled out my last will and testament and what would happen if I didn’t survive that surgery.
I tell my story so publicly so often, but that one moment the night before my surgery — filling all those forms out, thinking I might not make it off the operating table — was tough, but it was much needed. As a researcher, I knew if anything happened to me, if I had organs that could save someone else, I wanted them donated.
The little possessions and stuff I had, I knew where I wanted to leave them and what I wanted to do. That moment was a true, real, emotional moment for me and my parents. That’s something that is a requirement when you’re going into a surgery like I had.
It’s a real moment that can be a struggle for anybody. You have the fear of the unknown, but you’re also filling out these forms in case of. That’s scary for anybody, but especially somebody young.

Mentally preparing for surgery and overall treatment
The physical readiness is important, but also the mental aspect of it is really important. The first appointment I had with my doctors and team, I asked to speak to a psychologist. That was the same time I asked to speak with someone who had gone through treatment, who’d know what I was going through.
Psychologically, I had talked to not only a professional but also a human being who’d gone through it, so that helped me mentally prepare for what I was going to wake up to or not wake up to.
I’d never had any major surgery in my life, so not knowing what was going to actually happen — was I going to have dreams? A tube? How was my life was going to change?
The mental aspect of it, I wanted to go in mentally able to handle whatever I was going to wake up to.
What do you remember of the actual surgery (colectomy)?
It was 14 hours of surgery. It was very long. As you can imagine, those surgeries are complicated. They get a lot of people involved. Every 2 or 3 hours, they go out and tell my parents.
Tip: have caregivers give updates through surgery and treatment
I had a huge support system — friends and families who wanted to get updates about what was going on the whole time. I knew I wasn’t capable of doing that, so I created an email list.
This is helpful for all patients. I created a Listserv, essentially, of all people who wanted updates. My dad was in charge of updating people.
As he was getting updates from the surgeon and surgical team, he would then send an update to the people who cared about me and the people who wanted those updates.
It took the burden off of me and my mom, who’s very emotional like me.
Getting constant phone calls was the last thing that I would need after surgery. It’s stressful for everyone involved — the patient and the caregivers — so those constant updates they were getting, they in turn were sending out to my support system. Then they would send their messages, and my parents would read that to me.
Describe waking up from the surgery
I remember waking up. I was in a holding room. There were pictures of Disney characters all around me, and that’s just where they happened to put me in the time being. I woke up to my parents, and I was very, very groggy.
They had given me an epidural for pain management, which we had talked about before. I was told that it would be used. The problem was it was used, but it was only successfully able to work on one side of my body. It happened to be not the side where I had gotten a temporary ileostomy, so I woke up groggy and in extreme pain.
There were tubes and drains all over. I had an NG tube (nasogastric). You name it, if there’s an opening your body, I had a tube in it. I moved finally to my permanent room. The main things that I remember are looking down and seeing staples, seeing this foreign object to me, which was an ostomy bag.
At that point, I was told they were able to create an internal J-pouch, and I had this temporary ileostomy that they’d have ostomy nurses help me with. Their goal was to get the pain under control and get me up walking.
The sooner I walked, the better my recovery would be, though it was the most pain I’d probably ever been in my life and will have in my life, I hope.
Recovering from major surgery
Getting up, I was in obvious pain, as anyone would be who had any sort of major surgery. That next day after I had my surgery, physical therapy came into my room and said, “Allison, it’s time to get up. The sooner you get up, the sooner you can get your NG tube out, and the sooner we can get this drain out.”
You have to get your bowels moving again. That’s the whole goal of all this. You get to see something in your ileostomy. You celebrate little things like that.
Day 2, I was in so much pain that I was like, “I’m not getting up.” But then I remembered that if I did, I would get out of there sooner. I remember I sat on the edge of my bed for a little bit. They’re super patient with you.
I sat up on the edge of my bed, stood up, held my IV pole. At that point, I still had the epidural. It wasn’t working on the one side, so I had extra pain management on top of that.
I think I walked outside of my room, walked a few steps around, and then I went back in. Every day, it gradually got better.
Motivation for me was, I don’t know if I was the youngest person on my floor — I assume I probably was — but you see these older people lapping you on that floor. Everyone is trying to get out of there, and everyone’s trying to recover just like you are.
Every day you see the same people. I’m like, ‘If that 60-year-old can do it, then I can do it.’
Really, it was motivation from not only the PT, doctors, and myself; it was seeing others and how they looked progressively better and better each day that got me out of my bed daily.

Guidance for others on recovery
You have to go in trusting whoever’s going to be opening you up. Normally, your body is going to go through changes. You’re going to be in pain. Your body’s going to have to get used to whatever organ has been affected.
Just being patient with yourself is something that I try to tell people, because you want to get better as fast as possible. That’s just not the norm for most cancers and for colorectal cancer.
It involves your bowels and your bowel habits. That’s a fundamental thing that we all have to deal with on a regular basis. When someone messes with that surgically, it’s not going to happen overnight. I talk to people all the time, and they ask, “Does it get better?”
I remember being that person asking others, “Does it get better?” And it does. You just have to be patient, listen to your doctors, and adhere to what they’re saying.
As much as I didn’t want to get up and walk around, even after I went home after the surgery, I had friends and family come over, and we’d go for small walks in the neighborhood.
It was not only to get me out, but to get me moving, because you’re in control of your body. What you do to it and how fast you recover — part of it is out of your hands, but a lot of it is also in your hands.
Being patient with yourself and your body is really important.
Surgery and Ileostomy Bag
Surgical options
A colon resection is usually standard. Depending on where your tumor is, it might not be able to do just a small resection. It might be more. If it’s rectal, they might do the ileostomy or colostomy.
Researching your surgical options is one of the most important things you can do as a colorectal cancer patient. You’ve got colon, rectal, and you’ve got anal. You have all 3 different types of cancer that are in that area.
Things have changed over time. They couldn’t do laparoscopic surgery necessarily back then. I wasn’t a candidate, but now it’s done a lot more often and at a lot more hospitals. The recovery time and healing from that is a lot easier than if they have to open you.

The need for a stoma and ileostomy bag
You have multiple surgical options. Sometimes you get laparoscopic surgery, where they can do a colon resection. Due to my Crohn’s and history of inflammation of the colon, they had me do an open surgery.
They cut me from the mid-chest area down to the very tip of my vaginal area. They opened me up and realized that they couldn’t just do a colon resection.
Usually depending on your stage, it’s different with different options.
Quite a few people with rectal cancer — since my tumor was in my rectum as well — a lot of the surgical standards are they take a part of your inside. Then they make an opening on either your right or left side, and they call it a stoma. It’s a diversion from your intestines.
Essentially, your inside are on your outside, and there’s a bag attached to them. That’s where your waste flows. Instead of going from your mouth into the toilet, it now goes into this either ileostomy or colostomy bag.
That is in an effort for your body to heal. You just had this major surgery; everything has to heal. Then the next surgery, which is what I had, is to put you back together. Then that ileostomy is reversed.
Getting an ileostomy bag v. J-pouch
Because I had had Crohn’s since I was 12 years old, the amount of inflammation they found on my colon when they opened me up, my colon sort of fell apart in their hands. My surgical wishes were to have a J-pouch if possible. I did not want to have an ileostomy.
Since they took out my whole colon, they couldn’t do a colostomy bag. They could do a temporary ileostomy, take what was left in my abdominal area, and stretch it to make something called a J-pouch.
The recovery is to let that heal before you do chemotherapy so that your body can get used to your new organs again, and your digestive system can start working again with a lot less time from when you eat to when you get rid of whatever waste you have.
Life with an ileostomy bag
I still deal with it day to day now with the permanent one, but you have to adjust your diet. You have to deal with now having this external, essential organ on the outside. You have this bag you attach to it. You have to change that sometimes daily, sometimes every 3 days, and sometimes once a week.
You have to figure out what appliance — and I say appliance because it’s a bag you attach. It can be a 1-piece or 2-piece. You have to figure out what best works for your body so that you don’t have leakage.
If you can imagine when you’re eating, that waste isn’t fully being digested because you don’t have a part of your organ anymore, your colon and intestines. It can burn your skin. It can create irritation.
We could talk for another hour on an ileostomy, colostomy, and all that stuff, but the main point I’ll make is to try and find an ostomy support group that’s local or online.
Sometimes you have people who have 30 years experience with an ostomy. I’d be like, “What’s going on? My food’s moving through me too fast. What do I do?” They’d give me tips and tricks I’d never heard before.
Also, I was lucky that MD Anderson had a wound ostomy clinic. I was in the clinic sometimes daily, trying to figure out the best appliance and bag that would work for my stoma, because every stoma is unique. Wound ostomy nurse, ostomy support group, and then you have all these companies that supply all the products.
A lot of times when you call those companies, they’ll send you free samples, starter kits, and they’ll have a nurse either with the ostomy, usually, or a certified wound ostomy nurse who can provide guidance to you as well. They’re very caring. They really care and want to help you.
That was a huge struggle for me. I now am part of an ostomy support team at MD Anderson. When someone gets an ostomy for the first time, I go and talk to them because I had all these preconceived notions about it, but my life is better because of it.
Second Chemo (Xeloda)
Describe the second chemo
It was the same schedule without the radiation this time. At this point, I’m still recovering from the surgery [while] taking the chemotherapy.
I was having the normal neuropathy, skin changes, nausea, all that sort of stuff. There was joint and bone pain.
The weight loss and weight gain journey
Eating was one of the most important things for me because throughout the journey so far, I had lost 40 pounds. I was trying to eat as much as I possibly could so that my body was healing.
Nutrition is key with all different kinds of cancer, but really I didn’t purposely lose that weight. My doctor was like, “Eat whatever you’re craving. You need that nutrition to make you feel better.”
I listened to them. Obviously, my diet is much more regimented now. Then they were like, “We need you to eat and gain weight.” I don’t really eat Skittles anymore. I was craving Skittles, and my mom got me a 5-pound bag of Skittles. I would just eat them because that’s what I craved.
Also, Doritos, I craved them, so she would get me jumbo packs of Doritos. Whatever I had a craving for food, my mom was the best. She’d be like, “Okay, I’m going to go get it right now!” I gained a little bit of weight back, but also I was trying to eat.
With the ileostomy bag, the nutrition changes a lot. A lot of fiber or less fiber. I ate banana, rice, applesauce, and toast (the BRAT diet) quite a bit just to get things started and to move.
Gradually, I could introduce other things into my diet. In that recovery period and subsequent chemo, it’s really about healing and whatever you can do to make that easier on your body.
»MORE: Tips on food and drinks to help during chemotherapy
Follow-up protocol
I know once they went in for surgery and they removed all that stuff, they said I had clean margins. I was essentially cancer-free. After that, every 6 months, I was getting scans. After the chemo, I had a scan. Everything was clear and looked okay.
It was every 6 months I had my blood drawn. They’d get different markers, and I’d have a CT of my chest, abdomen, and pelvis. Now it’s yearly.
Reflections
Hair loss (unique situation)
I’m sort of a unique case in the fact that I had active inflammation from my Crohn’s disease, so I was put on some medicines that maybe 5% of people on that medicine lose that hair. It was a combination of a lot of different medicines that made my hair fall out.
»MORE: Dealing with hair loss during cancer treatment
It grew back, but then it fell out again. I’m dealing today with it growing back. I wear a wig on a regular basis. Most people notice. I don’t know if everybody does. Most people know it, but there are different things I’m doing now to have the hair grow back.
When your body goes through trauma combined with different medicines, combined with a medical history like mine — unfortunately, my body just was like, “Boom, done.”
I lost all my hair everywhere. Slowly but surely, things started coming back once I got off most of that medicine, but it’s a very, very slow process.
Top questions you get as a CRC ambassador
People want to know about the recovery time, when they can go back to work, or if they should tell their coworkers. I get a lot of questions about recovery time. They say for some surgery — it’s definitely depending on the surgery — usually it’s a few weeks, 4 to 6 weeks, maybe 2 weeks, depending on what you have.
Patience. Don’t rush back to a job or to doing certain things sooner than your body is ready to. Talking to your provider about what you can and can’t do is really important.
How did you approach the issue of fertility preservation?
Another piece of the puzzle is — and we didn’t necessarily talk about it because sometimes it fits with people’s treatment plans — with a younger population, I had the option to freeze my eggs at the very beginning of my treatment. But then I got very, very sick. That option went away.
I had to ask for that because there wasn’t a fertility specialist at the time at my hospital. I’m a very big advocate, and people ask me, “Should I do this or that?”
If you’re going to get radiation to your body, 100% you should look into fertility preservation, be it via egg, or they can move your ovaries out of the field. There are so many things they can do now if you want to have children in the future. If you’re young, ask for that consult on that first appointment that you go to.
No matter what age you are, you still want to have a quality of life after you’ve gone through all this treatment. If that means you want to have a family, you have to explore all of your family-building options before you start this long, arduous journey. For some people, it’s not that long. For others, it lasts for a very long time.
You want to at least know what you’re in store for. For me, it’s something also that’s emotional to talk about. I didn’t get to freeze my eggs because I got very sick, but it was an option to do. They could have done it within 12 days, so it wasn’t really too much time to have to wait before I started my cancer treatment.
Now, at this point in my life, I’ve looked into foster to adopt and other options, and I will have a family one day. It is not going to be genetic.

Long-term impacts of cancer
You’ve got to think about everything. My life has changed drastically. Even at 32, I was still the party girl, having fun with life. I finally had been like, “Okay, I need to meet somebody decent, settle down, and have all these hopes and dreams.”
I think you have to think long-term when you’re diagnosed with any sort of cancer, but what do you want your life to look like? I just want to have a long, happy life.
The things that made me happy before are not the same things that make me happy. I surround myself with people whom I know care and love and support me and were there for me during my cancer journey.
Do you want to have a family? What job really makes you happy? Take care of your mental health. There’s financial toxicity also that happens with patients, especially young patients who are just starting out their career or are in college.
You have to navigate the whole issue of insurance. That dream house that you might have been saving for, those savings might now be going toward cancer treatment.
In the long-term, you’re alive. Where you’ve living, if it’s not the big house on the block, it’s a condo that works perfectly fine. My attitude has changed about all of that.
How did cancer impact your relationships?
Relationships get tested a lot during this whole journey. When I was first diagnosed, I had been dating someone. They left. They couldn’t handle it. They were like, “Peace out. Good luck.”
I didn’t have time to think about dating and relationships at that time. Okay, I dived into my cancer diagnosis. But the people who were there for me during my entire journey, some totally surprised me.
Some people totally stepped up. Some people I thought would be there were not there.


Then my parents were my lifesaver. My mom was at every appointment. My dad was by my side every night after I had surgery, along with my mom. I think you realize the people who care about you, the people you want to have in your life, and the people you surround yourself with.
It totally changes during and after cancer. It’s surprising that a lot of those people who were there for me are still in my life, but a lot of my best friends are fellow cancer survivors and people I’ve met throughout my journey I connected with for support. Those people just get me like nobody else.
A lot of them don’t live here. They live all over the world, but they are some of my best and true friends. I know they will be my friends for life.
»MORE: What kind of support cancer patients say helped the most

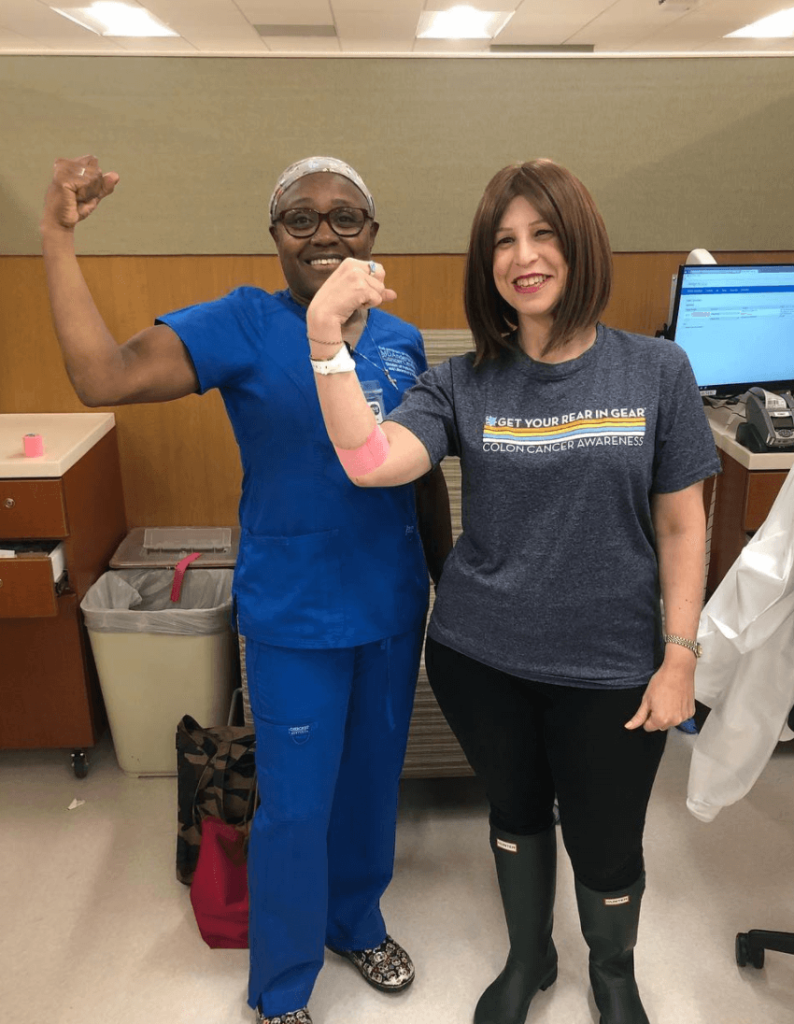
Finding your cancer community
When I went to my psychologist, I was like, “Are there any support groups out there?” I went to the ostomy support group. That was great, but I wanted to connect with other young adults like me, other people like me.
They told me about some nonprofits. I got involved with some of those. There are a ton of colorectal nonprofits. The first thing I did when I was trying to find some locally, I was like, “Colon cancer support Houston, Texas.” That’s when I went to Google. Google is good for that.
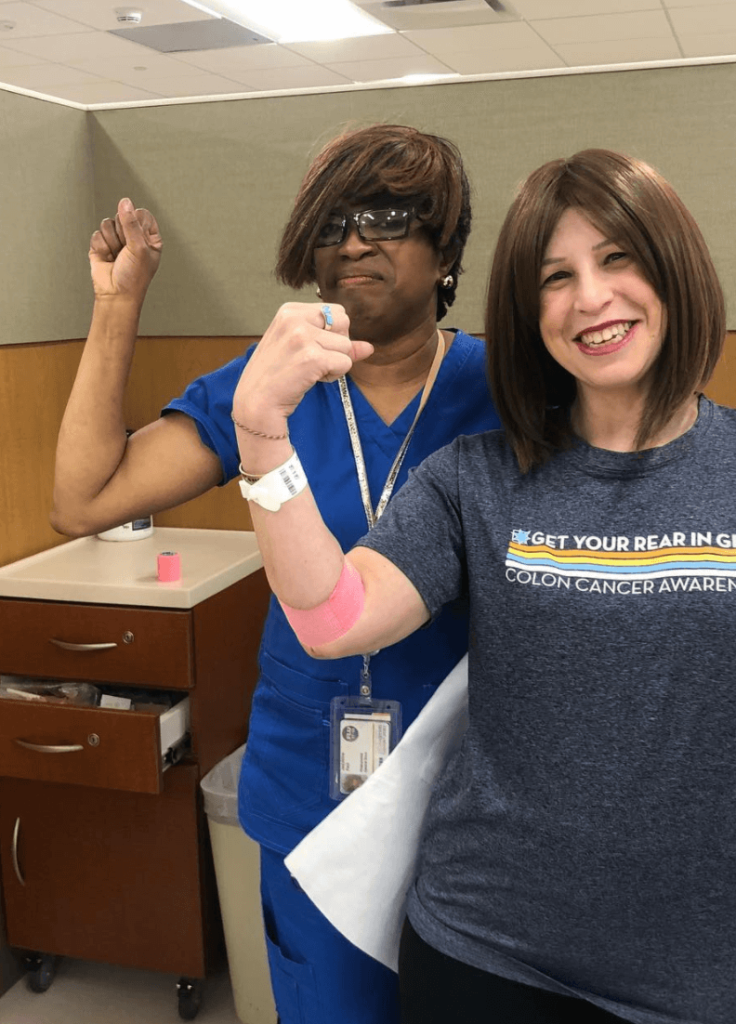
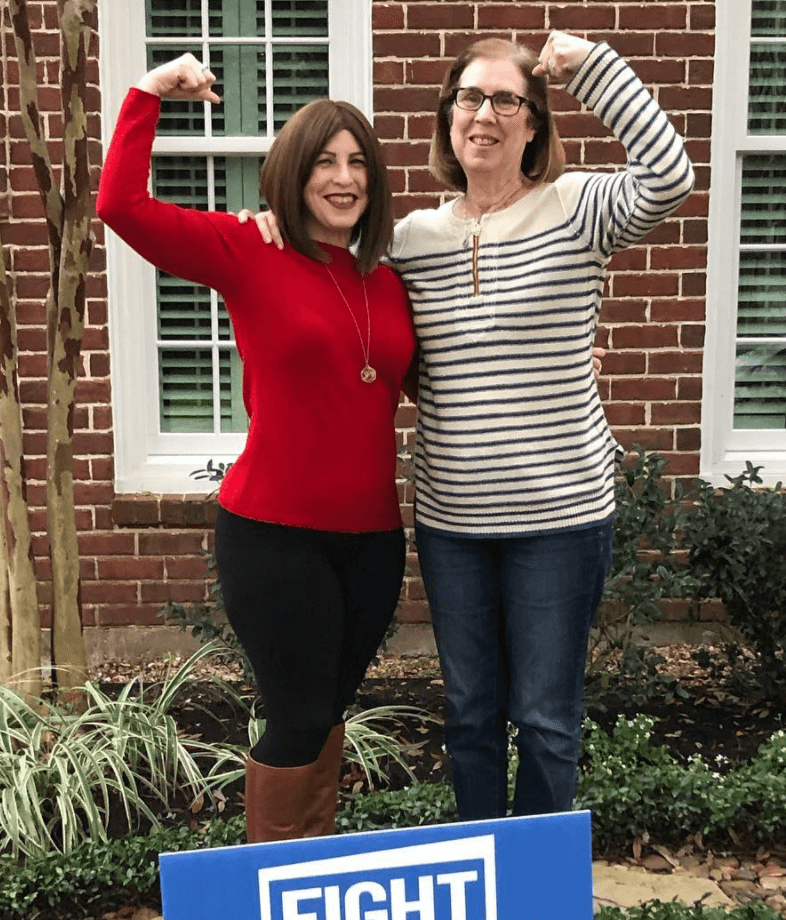
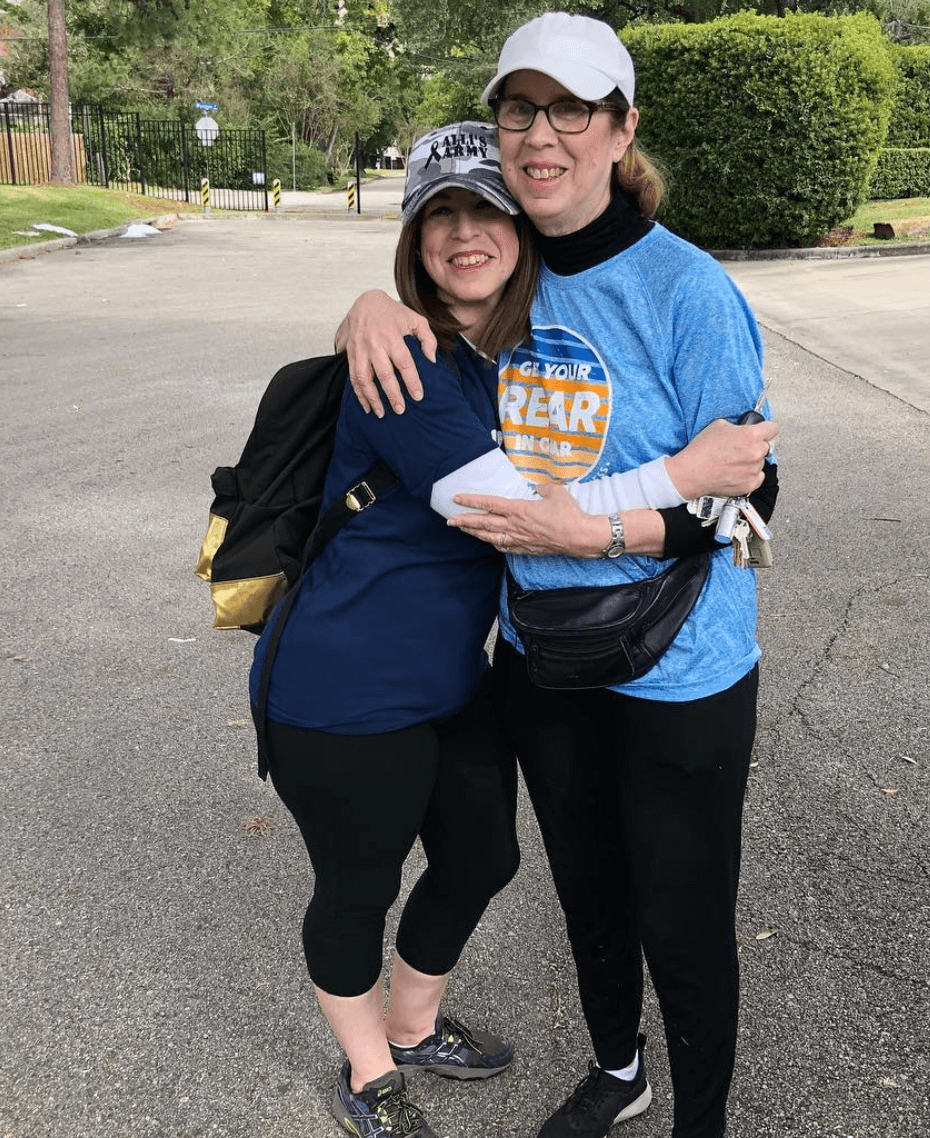
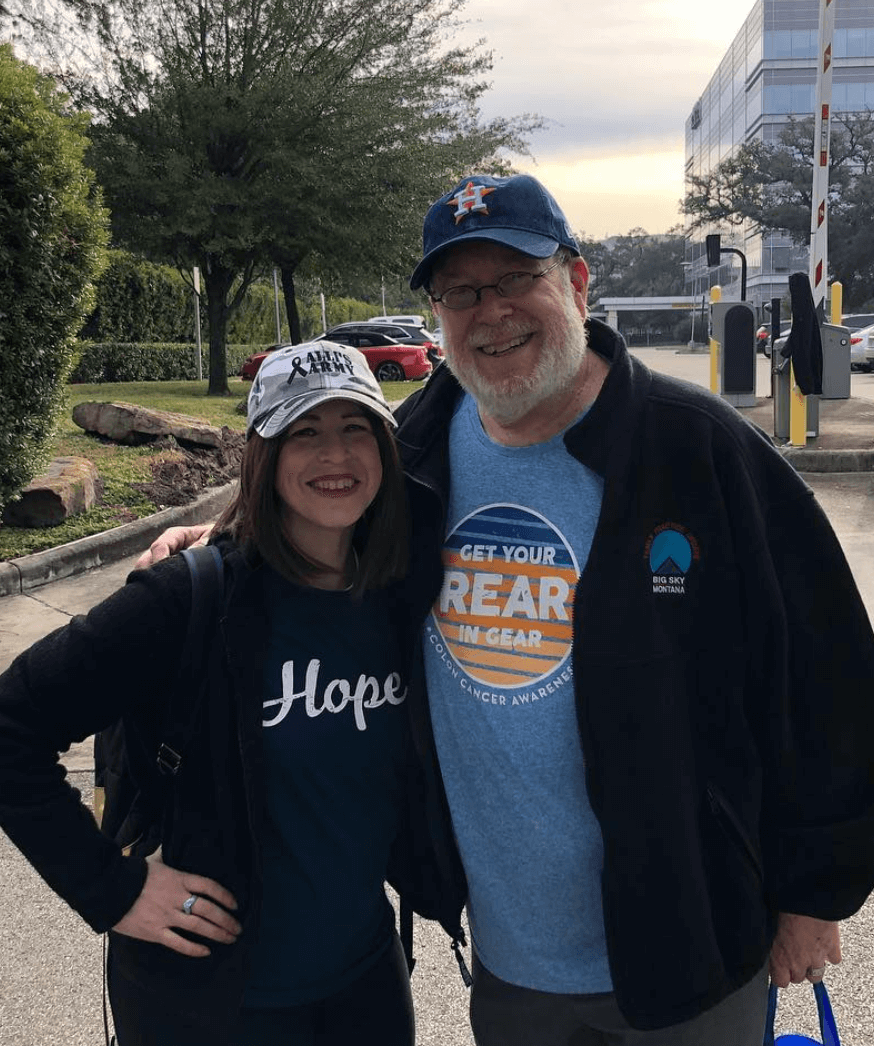
I found a race called “Get Your Rear in Gear” in Houston. I wanted to meet other survivors like me. It was a way for me to meet other patients and survivors, but also give my support system — the friends and family who wanted to do something for me but there was really nothing for them to do — to be there for me on this one day.
It was during my treatment that I did that. Also, there’s ways to connect online to other patients and survivors. There’s a group called Blue Hope Nation. There’s something called Colon Town. Essentially, that’s where you can connect with people who just get you and local support groups.
No matter where you are in your cancer journey, the support doesn’t stop just because you’re cancer-free. Survivorship and the long-term side effects are sometimes the true test of you as a person.
I got involved heavily with the adolescent young adult movement by joining an advisory council at MD Anderson.
Emotional support during cancer journey
It was emotional. My mom was a breast cancer survivor. When I was a teenager, we all had to chip in and were her caregivers, along with my dad. I had a little bit of experience with cancer.
When I was first diagnosed, my mom was obviously crying like I was. She said, “I wish it was me,” because of my age. I remember clearly saying, “I don’t wish it was you. You went through it once. I’m strong, and I can handle this because I have you guys.”
My parents were forced to be strong for me. Also, I wanted to be strong, but I also needed to be emotional and cry and let all that fear out. If I kept it in, it would have probably negatively affected the treatment and my path to getting better over time.
Last message to others
You’re not alone. I thought I was alone when I first started. I looked around the waiting room and didn’t see anyone who looked like me. But if you search and you reach out to people like you (The Patient Story) or me, we can connect you to the resources you need and people who will help you throughout your journey.
Even though you’re surrounded by your amazing support system of friends and family, you can get very lonely at times. When you connect with someone else who gets it and gets you, then you can get the support you so badly need to get through this journey.
It’s also one day at a time. Nobody’s journey is the same. What you might struggle with someone else might not struggle with, but you’re not alone.


Inspired by Allison's story?
Share your story, too!
More Colorectal Cancer Stories
Monica D., Colorectal Cancer, Stage 1
Symptoms: None; caught at a routine colonoscopy
Treatment: Surgery (low anterior resection with temporary diverting ileostomy)
Edie H., Colorectal Cancer, Stage 3B
Symptom: Chronic constipation
Treatments: Chemotherapy, radiation, surgeries (lower anterior resection & temporary ileostomy)
Shayla L., Colorectal Cancer, Stage 4
Symptoms: Stomach sensitivity, food intolerances, exhaustion, blood in stool
Treatments: Chemotherapy, surgery (hepatectomy)
Tracy R., Colorectal Cancer, Stage 2B
Symptoms: Bloating and inflammation, heaviness in the rectum, intermittent rectal bleeding, fatigue
Treatments: Chemotherapy, radiation, surgery
Paula C., Colorectal Cancer, Stage 3
Symptoms: Painful gas, irregular bowel movements, blood in stool, anemia, severe pain, weight loss, fainting spells
Treatment: Surgery (tumor resection)
Nick S., Colorectal Cancer, Stage 4A
Symptoms: Change in bowel habits, size & consistency, blood in stool, abdominal pain, fatigue
Treatments: Surgery (sigmoid colectomy), chemotherapy (capecitabine, oxaliplatin), immunotherapy (bevacizumab, pembrolizumab)