Doreen’s Stage 2A IDC Triple-Positive Breast Cancer Story
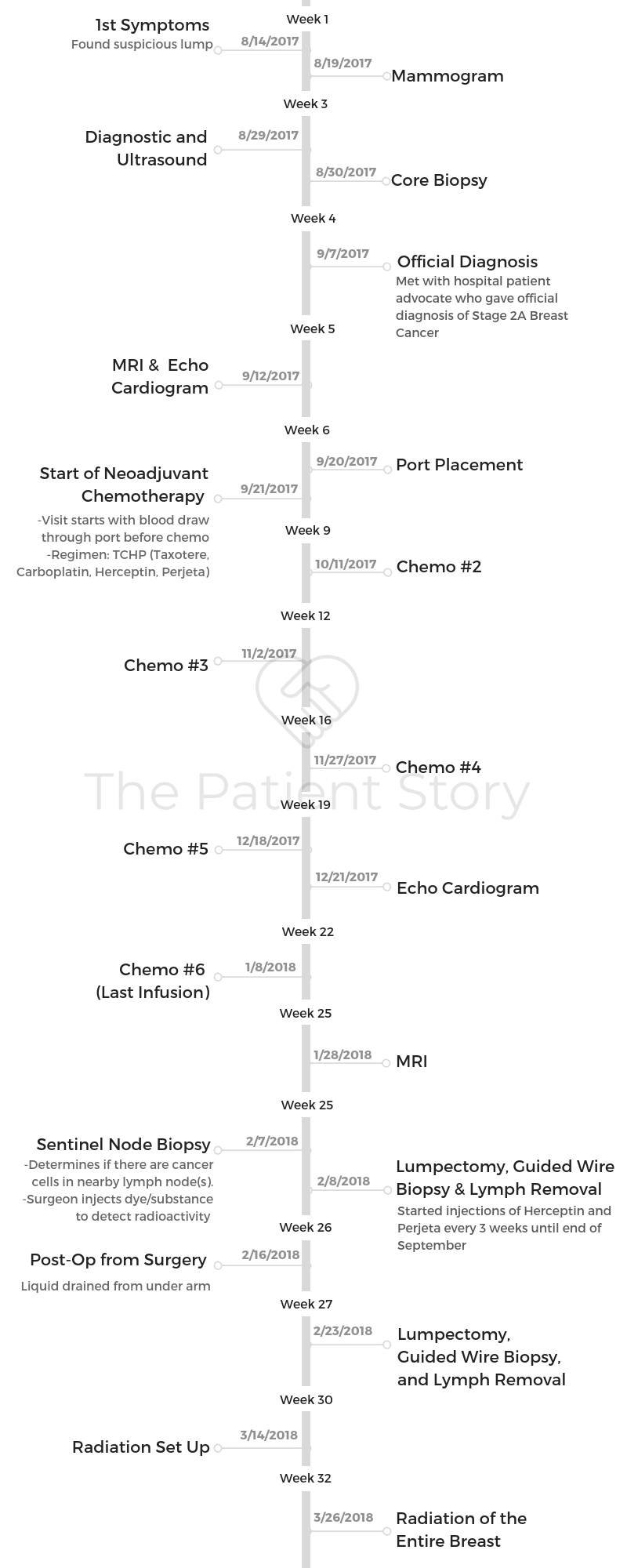
Doreen shares her stage 2A triple-positive breast cancer story, diagnosed after she found a lump in her left breast. She details undergoing and recovering from TCHP chemotherapy, a lumpectomy, and radiation therapy.
In her story, Doreen also highlights how she navigated life after the breast cancer diagnosis, losing her hair, how she managed work through treatment, and the importance of keeping a sense of humor.

- Name: Doreen D.
- Diagnosis:
- Breast cancer
- Invasive ductal carcinoma (IDC)
- Triple positive
- Staging:
- 2A
- 1st Symptoms:
- Lump in left breast
- Pre-diagnosis tests:
- MRI
- Echocardiogram
- Treatment:
- Neoadjvuant Chemotherapy: TCHP
- Taxotere (docetaxel)
- Carboplatin
- Herceptin (trastuzumab)
- Perjeta (pertuzumab)
- Lumpectomy
- Radiation
- Neoadjvuant Chemotherapy: TCHP
- Diagnosis & Tests
- Treatment Decisions
- Chemotherapy & Side Effects
- The TCHP chemo regimen
- Describe how TCHP chemo went
- What were the chemo side effects?
- Describe the side effect cycle
- What helped you physically with side effects?
- What helped you deal with side effects emotionally?
- How did you hear about medications that would help prevent side effects?
- Did doctors and nurses ever give advice about side effects?
- What was the response to chemo?
- Doreen's Video on Surgery Prep & Recovery
- Surgery (Lumpectomy)
- Doreen's Video on Radiation
- Radiation & Side Effects
- Hair Loss
- Talk about the hair loss
- What motivated you to finally cut it the first time?
- When did you shave it all?
- Describe the emotional part of hair loss
- You had to learn how to draw in your eyebrows
- Your hair hurt as it fell out, especially your eyelashes
- Did you wear wigs?
- Did you try cold caps to save your hair?
- Work & Finances
- Mental & Emotional Care
This interview has been edited for clarity. This is not medical advice. Please consult with your healthcare provider for treatment decisions.
Be open to anything that comes to you, I think, because during this process you’ll meet a lot of people that you never thought you’d meet and have conversations you never thought you’d have.
I think you need to let those happen. Know that you’ll get through it.
Doreen D.

Diagnosis & Tests
How did you get diagnosed?
I’m not quite sure whether they were symptoms or not in terms of what I was looking for, but 2 years before diagnosis, I started to gain weight and gained almost 20 pounds.
I had gone to my doctor and mentioned to her about it. I’m pretty active. I work out anywhere from 5 to 6 times a week. I don’t eat bad. I don’t have any of those big issues, so I’d gone to her and started talking to her about that.
Her response to me was that I was just fat and if she had a nickel for every person that came in there and told her that they had thyroid disease, she’d be rich.
My response back at that point was I never mentioned thyroid, nor did I mention anything that had to do with it. I mentioned more that I was trying to figure out what was going on.
Eventually, I found a doctor who’s a little more alternative and deals with athletes. We did a bunch of blood tests, and he mentioned to me at one point that some of my markers were coming back looking possibly like cancer, but he couldn’t be sure or couldn’t tell what it would be or what that was like. Of course, that’s in the back of my head.
I was away traveling on a work trip, taking a shower, and found a lump on my breast that was kind of shattering in terms of just the fear that went through me, not knowing what it was.
I started calling doctors and the mammogram center, trying to figure out what I need to do. Trying to get my gynecologist to order the right test for me, and after maybe 5, 6, 7 different phone calls, finally got an order for a test, which ended up being the wrong one.
I had to do a little background research and find somebody else who would actually listen to me, pay attention, and order some tests for me. That ended up being another 7 days from then.
By the time they actually did the right mammogram and ultrasound, the next day I was sent for a core biopsy. Through the core biopsy, they had found something that looked aggressive and scary. They checked my lymph nodes.
At that point, I knew I had cancer and wasn’t quite sure what stage it was or how bad it was. All I knew at this point was it wasn’t in my lymph nodes, and nobody’s actually telling me I had cancer.
From that, they had started to put down on the calendar my surgeon consult, my oncologist consult, and then when they’d give me my diagnosis consult.
What were you thinking or feeling before the official diagnosis?
Nobody’s really saying I have cancer yet.
There’s no reason they would give me a surgery consult first and foremost, or an oncology appointment. The next day I was flying to Italy for one of my really good friend’s weddings.
My close friend who was staying with me knew I was going for an appointment, and I mentioned that I thought I might have cancer. She’s like, “No, you should be good. It’s probably not cancer,” She pretty much pretended like she didn’t hear that. I’m like, “No, it’s cancer.”
I got a lot of that kind of feedback instantaneously, but it was something that was in my head and something I couldn’t really talk about. I didn’t want to ruin my friend’s wedding.
The hope was if this was it, I would only have to do lumpectomy and radiation. I had all these things going through my head at that time that I tried to wipe out of it.
I think I was lucky that I was somewhere else in terms of a foreign country that I’d been to before. I could just mentally keep myself busy.
How did you process the diagnosis?
I landed, and the next day I had an appointment set up with what’s called a patient advocate at [the medical center]. She’s a breast cancer survivor, so I brought a friend with me because I knew it was probably going to be messed up.
We went into the room, there was a little bit of small talk, and I said, “Let’s not do that; let’s get down to the results of this.” I’m a little bit stressed out, to say the least.
She gave me the diagnosis. Of course, I cried. My friend cried. We started to talk about what the next steps were.
I already had my surgery consult. They definitely told me the stages, and I had no idea what that meant or how bad it was. When you look at the scale of things 1 through 4, I was a 2A, so in my mind it was better than 2B.
It had no correlation to anything, but that’s how I looked at it. I was just like, “Okay, does that mean chemo?” Then the chemo thing came out. I’m like, “I need to do chemo, I need to do this, and I need to do that.”
At that point, my advocate is like, ‘Take one day at a time. There’s a lot that’s going to come at you.’ You don’t think about it in that way. You don’t realize the enormity of what’s to come and hit you.
»MORE: Processing a cancer diagnosis
What were the next steps?
That’s where we sat, and the next stage after that was my surgery consult. So I think that was it. It might have been an MRI.
I can’t quite remember, but either way, there was one or the other that happened. Within that week, I had a surgery consult, I had an MRI, an echocardiogram, I had my port put in, and I met with my regular oncologist.
It was just things coming at me at all speeds in 5 days.
Describe the breast biopsy
Hurt like hell. It’s through a needle, a hollow needle almost. It’s long but not thick. They used local anesthesia.
It took about a half hour at the most from beginning to end. My mass was right above my nipple in the right quadrant, and you could feel it. It was relatively big. It was 2 to 3 centimeters.
I think there were 3 different things that they took out, and the woman that did it told me about what she was going to do. They take out the pieces of the inside the core of the cancer, and they come out in little tubes almost. They put each of those into a separate tube and do the diagnosis through that.
Chemo was the scariest word
Absolutely, chemo was the scary word because you think about stage 1 people, and not to belittle it, but it seems simple. In the scheme of things, it was just getting an operation, having a small thing taken out of you.
Then radiation, which is not fun, but it’s better than chemo hypothetically. At least that’s what people will tell you.
It seemed like a bigger ordeal because you think back to your parents’ chemo — I hate to put it that way, but before pills that would help you not puke or poop, it had to be even more miserable.
I think because the patient advocate had mentioned to me that I don’t want chemo before I left for vacation, in my mind I’m like, “Okay, if I have chemo, I’m doomed. That’s just the worst-case scenario.” Little did I know that maybe stage 4 was the worst-case scenario, but I didn’t know stages existed then.
Treatment Decisions
Your biggest questions
I didn’t know there were stages. I didn’t know there were positive or negatives for estrogen [and] progesterone. I had no idea any of that existed.
For chemo, it was [a question of] how long, because I didn’t have a gauge of what that looked like either or what that would feel like.
At first, I don’t think I asked a lot of that kind of question. It was more of, “Now, what is the plan? How do we do it? Am I going to die? How bad is it?” The simple stuff. That was where my head was at with the patient advocate.
By the time I got to the surgeon, she filled in a few more dots for me. I don’t think I knew how long or what that process was yet, but my surgeon is one of the best. I felt really comfortable with that.
She laid out things really easily. She answered any questions I had, and at that point, I didn’t really know what I should be asking.
Luckily, I have a cousin who’s a surgeon who was on the phone with me and her, so that helped a lot in terms of her asking questions and telling me about that later.
How did you choose hospitals?
I think it was decided for me, to be frank. I’m at the same place I get my mammogram every year, and my patient advocate was from CPMC Sutter Health.
When it came down to that, before I even got the diagnosis, they were setting me up with people in the network.
I just asked her who was the best and who she would go to, and she picked for me. That’s how it came about. I didn’t really question any of it.

Did you consider switching medical teams?
I didn’t even think about it, but when I met each one of my doctors — when I met my surgeon, I knew she was super smart, direct, and to the point.
Everyone in the office was great, so I had a good feeling. I don’t expect my surgeon to be warm and fuzzy. I want to be someone who’s going to be badass and get that shit out, and be as great at that as possible so that I know hands down, I’m fine.
I did do a little bit of research on the backend of anybody that knows her. I know a lot of people that work at hospitals. She’s one of the best. I was confident with that. My oncologist was wonderful.
There’s another guy that’s also an oncologist in her office who I met. I was a little bit like, ‘Hmm, I’m not sure I like him.’ It ended up being one of my favorite people.
All the nurses were amazing. I didn’t question any of that because I felt like they knew what they were talking about, and they didn’t sugarcoat anything. My communication style was more like that.
By the time I got to my radiation person, I really didn’t feel it, and I realized that I really didn’t have to be with him that often. It was once a week, and he’s the best at plotting where the rays go.
If I was going to do it again, I would probably go somewhere else. Maybe. But it wasn’t as drastic, and it didn’t mean as much to me there because the 2 people that actually gave me radiation every day were wonderful.
It becomes, “Do I want the best person I can find in the best place I can find with the best machines?” Yeah, I do.
Did you research your doctors?
I’m part of Bay Area Young Survivors, and so that group has been good to kind of bounce off who people have used. With the radiation oncologist, I had 2 names, and I sent both of them out there.
I got pretty much a 50-50 of the group liking both of them without many issues. I had maybe 1 or 2 talking about the impersonal piece, but that’s less important to me.
»MORE: Cancer organizations and nonprofits →
Chemotherapy & Side Effects
The TCHP chemo regimen
It was the neoadjuvant chemotherapy regimen of TCHP:
- Taxotere (docetaxel)
- Carboplatin
- Herceptin (trastuzumab)
- Perjeta (pertuzumab)
Describe how TCHP chemo went
I usually would go on a Thursday. I wanted to have enough time over the weekend, because I worked through chemo. I’d go in on Thursday morning at 9:30.
They go in. Through my port, they’ll take out blood to check all my levels. That will be [checked] in house. All my levels will come back, and then they will figure out what they needed to do for each one of my chemos in terms of my body weight, blood pressure, and my blood chemistry.
They would put it all together in house in terms of the chemo, and it would come out in bags. I would get it in that order: TCHP.
The taxotere was the first one. It would be hung up in a bag, and I would just sit there and work from the office. I had my friends go with me. I would have one friend each time.
They would go through each one of the bags. It would take 4.5 hours total. While that was happening, I would also talk to the doctor.

My oncologist would come in. We’d talk about everything that was going to happen or was about to happen for that first one, what to expect, and what I should possibly be ready for, which was good.
I really like knowing more of the ‘tell me what’s going to happen’ because I want to be ready for it.
It’s like turbulence. If they get on the speaker and say we’re going to go through a rough patch, I’m ready mentally. That’s how that day went.
There was another doctor there, who was also an oncologist, who’d come in and deal with more of the everyday stuff like fears, any questions I have, or anything I didn’t get answered from the first oncologist.
Then they just keep checking on me, changing the bags throughout the day after that, and at the end I would go home. I couldn’t really eat during it. I would mostly drink fizzy water. That’s where my obsession started for that.
Then the first day I was fine. I could go to the gym and be okay. The next day I had a lot of nausea, diarrhea, that kind of stuff.
»MORE: Read more patient experiences with TCHP chemo
What were the chemo side effects?
- memory loss
- loss of focus
- loss of taste
- nausea
- fatigue
- diarrhea
- sore throat
By the second cycle, my nausea would start as I’m getting my infusion. They started to put another chemical — I don’t know what it was — into my infusion bag so that it would help, but I still was nauseous, and diarrhea would start that day. Those were constant through the whole process. [It was] only better during the third week.
Sore throat, swallowing — that was usually the first couple of days. Then I started using Biotene (mouthwash) the day before chemo, the day of chemo, and the day after, and I didn’t have any issues with that after.
The food thing sucked. Not being able to taste food was the worst. I had super smell, and I could smell everything that would be amazing. Then you take a bite, and it was like eating bark.
That’s mentally challenging and physically challenging because you’re trying to survive. You’re trying to be productive, you’re trying to get out when you can, you’re trying to do things, and you’re trying to have as real of a life as possible. Then you can’t eat normal things.
I did a lot of protein shakes. Jello. I don’t have a sweet tooth, and now I do Ice cream became my best friend. I became an expert at that, so it’s just trying to get over that piece every week.
It was like that until the third week, when I could start to taste again. That was across the board, that one symptom. The diarrhea, fine, you deal with it. The nausea, you deal with it. I could be downplaying this for other people that that’s horrible for, but for me that wasn’t as bad.
Describe the side effect cycle
The first round for me was the worst. First and last were the worst. It started to hit me Saturday. I’d really start to feel it. It was more sore throat, which I ended up finding a solution for (Biotene mouthwash).
The nausea was constant for me, even though I was taking pill. I wasn’t throwing up, but I was nauseous. The diarrhea was constant for me. I had tons of pills for those.
Kind of feeling crazy at times. I would not know what I’m doing or where I’m at. I would have to sit down a lot. Got a little tired, and then after that, it was more of losing the memory, losing words, not being able to find them.
Getting tired, having to sit down a lot, that kind of thing. Not being able to focus on my work like spreadsheets. [It was] horrible, so I got a lot of the easier stuff to do.
But I would absolutely fly weeks 2 and 3.
I used Purell like a gun. Third week is good. Then you go back in again, and by the second cycle, I had lost my hair 2 weeks in. My eyebrows I kept until the end. Eyelashes fell out the last one.
Food became unpalatable. Probably the second cycle was when I lost all my taste. I’d lose that for anywhere from 10 to 12 days. I’d have 2 days of feeding frenzy!
What helped you physically with side effects?
- Biotene mouthwash (sore throat and swallowing)
- Exercise
Protein helped, and exercise helped me. Actual exercise. It doesn’t have to be anything big. It’s just moving, because I felt it moved the chemo through my body faster.

What helped you deal with side effects emotionally?
Being around friends and choosing not to talk for a lot of the time.
Sometimes it was not talking to people, not going out, watching bad television. Other times it was somebody coming to pick me up and drive me around. “I don’t care where you’re going,” is what I said to my friends.
So many people call you and ask “What can I do? How can I help?” I couldn’t come up with anything. After a while you kind of figure out what you need.
It’s like if you’re going for an errand, come pick me up. Getting into the car is hard. Getting out of the car is hard. Walking normal — hard. Thinking — hard.
But you could still be with somebody and not say anything and roll through it. For me that was huge.
Being around that community for me was enormous. Not hiding so much. I think that you have to absolutely do that. Not saying you shouldn’t hide when you need to, but as much as possible, getting out with people that are not a lot of work for you.
How did you hear about medications that would help prevent side effects?
I went to chemo bootcamp. Most frightening. That was one of my bad days. Before chemo started, they bring you into the oncology office. This nurse that’s new comes in and goes through each one of the drugs you’re taking.
She goes page by page into all these things that are going to happen to you. It’s this long list of horribles. You’d go through page 1, 2, 3, and that’s like, “First drug, here you go.”
I’m like, ‘I don’t want to do this anymore,’ and she’s like, ‘I have to legally go through it.’ I’m like, ‘Okay. So for these 4 drugs, all of these things are the same. Can we agree on that?’
I started to fast-track whatever we needed to do, and after a while I just stopped listening to her because I couldn’t handle it.
Mentally, I couldn’t get into all these things that are going to destroy my body, so I just tuned it out. That was horrible.
Then my friend took me for drinks. It was like 2 in the afternoon. We just went drinking. That’s how I dealt with that piece.
Back to the other stuff, that’s where I learned what was going to happen to me hypothetically. From there, I’m part of some Facebook groups that are for triple-positive.
I just started following threads and asked questions there. You get instantaneous answers. That’s where I found a lot of solutions to simple things, and I would just try something. If it worked for me, great. If it didn’t work for me, it was gone.
Did doctors and nurses ever give advice about side effects?
Sometimes, like the diarrhea and the nausea. That would come from the doctors, so I had special pills for those. I ended up for the first time ever buying one of those weekly Monday to Friday [pill cases] because you can’t remember shit.
I couldn’t remember the labels of anything either, and all the drugs have 2 names. There is the normal name and then the simple name, which is not simple, but it starts with a letter.
Each one of my drugs, beforehand I’d take a big marker and put “D” for Decadron and “C” for another like Colace or something. I would label them that way, and then on my notes I would just put “C” and “D” and write it out that way. I’d have a reminder in my phone as well, because chemo makes you stupid.

That’s the way I would lay those out. Those drugs were given to me by my doctor. Then Imodium was part of that, too.
When these don’t work, that will work last. But everything that the doctor gives you is much stronger than anything you can get out in the field, so I did a lot of that.
My talks with the doctor every 3 weeks, I’d say, “This is what’s working. This is what’s not working. Do we have anything else I can do?” Then they would suggest stuff, or I’d start taking things.
Then I’d email and let them know, “Is this going to get in the way of anything we’re doing? Is this good? Is that bad?” They would instantaneously pretty much get back to me in a day. I was lucky I had a good team.
What was the response to chemo?
I had a complete response from chemo, which means that they couldn’t find the lump by the time I was ready for surgery and had an echocardiogram.
I had 2 echocardiograms and 2 MRIs in that time of my chemo to look and see where we’re at in both of those stages, in terms of my heart and also the size of the tumor. There were scans before chemo, during chemo, and before the operation.
Doreen’s Video on Surgery Prep & Recovery
Surgery (Lumpectomy)
Preparation for the guided-wire biopsy
I had to do a needle biopsy first, called a guided-wire biopsy. That setup [was] horrible. No way to sugarcoat that. The day before, the night before you go in, they put this tiny needle into your nipple, and that hurts!
That lights up the stream for where the cancer would flow into your lymph nodes. From that, they can tell what lights up, and that will be what they take out.
For me, you could see it on the screen. They showed it to me afterward: 3 of them lit up. The next day you know they’re going to take out at least 3 when they go in there.
That doesn’t mean they’re cancerous. It just means they’re lit up, and that’s the path the cancer would travel if it’s traveled, which is scary when you think about it.
Describe the actual guided-wire biopsy
The next day you go in, and the needle-guided wire is what they need to do next. They gave me Valium because I was stressed out, and I’ll take a Valium any time they offer it when I’m in the hospital.
We went downstairs. The 2 ladies that were in one of my tests along the process were the same ladies that were doing this. I think they were the ones that did my core biopsy, actually.
They put you in the mammogram machine, which crushes your boob. This time it was sideways, so it was more like this, because my cancer was on this side. They numb it a little bit, but not enough is the thought.
Then they put this paper-thin wire into the spot where your tumor was. You can see that happening all while you’re doing it, so you’re looking at a screen watching a wire go into your boob, feeling the pain of that first and foremost.
When they take that out, the wire is still stuck in your boob, so you can look down. I’m like, “Can I look at it?” They’re like, “You sure you want to see that?”
I’m like, “I absolutely want to see it because it’s hopefully a one-time thing.” There’s a little wire that goes, and it came out to here. They ended up taping up and putting on my boob.
The lumpectomy was next
I went in for surgery. That was the best part because I get to sleep for that. There’s not a whole lot of talk. I just went in, you lay on the table like Jesus, and then you’re out.
I didn’t stay overnight. It was a 1-day surgery. Once I was fine, I left. They told me that they got all the margins and there was nothing in my lymph nodes.
From there it was just rehab. I slept a lot that first day, but since then it’s been more rehab in terms of arm mobility, physical therapy, that sort of deal.
It wasn’t a mastectomy or anything like that. It was small and disappeared pretty much [after chemo]. I didn’t have to worry about that.
Because the lymph nodes were clean, I didn’t have to worry about anything after that either. Both of those pieces very lucky. Just a lumpectomy. I didn’t have any of the history either, so I didn’t have the BRCA gene.
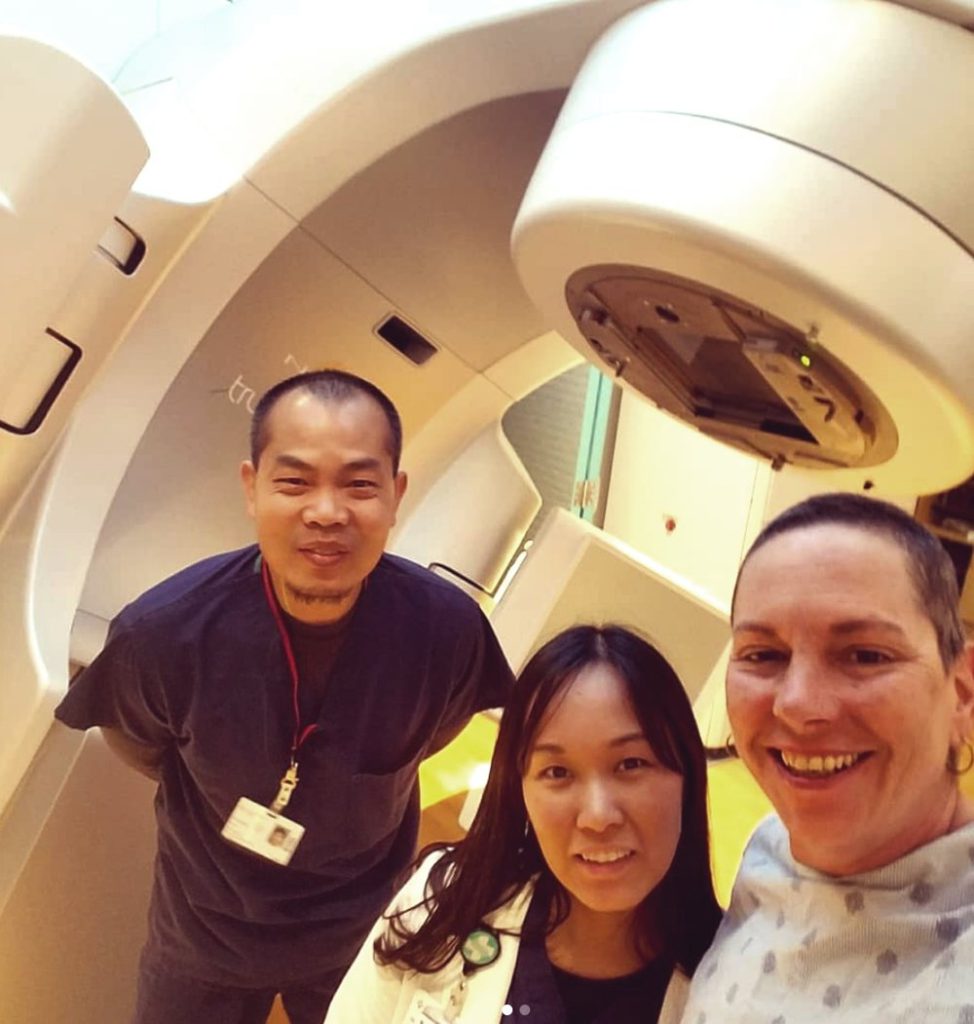
Doreen’s Video on Radiation
Radiation & Side Effects
After surgery you had radiation
I think it was a month or a month and a half at most. So 6 weeks is probably max. I started going to get the setup probably at 4 weeks. I met my radiation oncologist. I learned what was going to happen. I found out how long I would have to go.
Then they tell you whether it’s a full boob or just partial spot. I had full boob. I think I didn’t grasp what that meant or anything. All my big questions were more about my heart and lung because it’s on my left side.
They talked about how the plotting works, and I still don’t grasp the understanding of the technical piece of it, but I was lucky I only had to go for 4 weeks.
If I had to go for as long as they initially thought (8 weeks), I don’t know if I would have survived as well mentally and skin-wise.

Describe the radiation process
There’s an initial meeting that talks about what they’re going to do, what it’s going to look like, and how they’re going to plot it out.
Then they go away and plot it out in terms of the different layers of radiation, how close it’s going to get to where they need to go, and which angles they’re going to take with the beams to be able to hit it the best way.
You go back after that, and they do a setup for you. You get into a different machine. They tattoo you, and that’s going to line you up to everything in the room so they can get you in the exact spot that they need to.
That morning you start, you go in, and it’s probably 30 to 45 minutes. They get you in the right spot, they take pictures over and over again, and then they finally radiate you. For me I had 3 on one side, 3 from the other side.
You lay down in a huge machine. They prop you up, which is kind of funky. I didn’t realize that until you kind of look around, so you’re off the ground probably 4 feet, 4.5-half feet.
There’s a machine behind you that’s almost like an MRI machine that comes up and around over you. When they’re doing films, there’s a bounce board behind it, so they’re both coming out and around you. It’s pretty much showing your boob to everybody.
I have a gown on my right shoulder, and it goes down to my waist. They put a blanket on me up to my waist, and that whole part is open from there.
You look up, and there are lasers in the ceiling. There’s lasers to each side of you. Then the machine has lasers. Then there’s lights that I can see that will tell me when the laser’s on and when it’s not on.
Also, I have a box taped to me, too. I don’t know what the box does. I think it was more of the measurement of where my breath was. Once that hits a certain level, that’s when they can radiate me.
»MORE: Read other patient experiences with radiation therapy
What were the biggest side effects from radiation?
In the beginning, everyone tells you that radiation isn’t as bad as chemo. I personally hated radiation, mostly because chemo was something I could manage and work through, and it was rational thinking for me.
Radiation was every day, Monday through Friday, 5 days a week for 4 weeks. It’s not very long.
For me, I had to hold my breath during radiation to be able to push my boob up high enough that you’re not hitting any of your lungs and heart, so of course now you have that in your head as you’re doing the radiation of, “It’s going to ruin my lungs. It’s going to hit my heart.”
Then the machine is imposing. It’s enormous, it goes around you, things are coming from the ceiling, and the people that are techs helping you are running out of the room while you’re sitting there.
It’s just danger. Danger, but you’re still on that table. You’re the one being affected by it. For me, that mental game was a lot harder. Then when they lay you out, they marker you.
Mine was from underneath my underarm up to my chest bone, all the way down underneath my boob, and I didn’t realize that whole piece would get red.
I just didn’t think about it till week 2. I started getting really red there. It’s a constant burning that doesn’t go away. Now I have the incision underneath my arm, which is now burning along with the rest of my boob and my nipple.
You put on lotions every night, every day. Then you have to wash all that off in the morning, because you don’t want it on there when you go in. It’s just a game of constantly being sore and red like a full-on burn.
It wasn’t fun. It was mental, and it’s physical because of the burning. Then there’s the other piece of being exhausted. You hit a wall. I was more exhausted than I was at chemo.
You had to go to physical therapy
I worked out after. I didn’t do a lot, but I’m an idiot and had fluid on the incision for the lymph node biopsy that started to build. It got more and more pressure, so it ended up being 80 ccs of fluid, which is apparently a lot.
They had to go into the scar and drain that. Another needle process, which is not fun. 7 on the Richter scale. I had to have that happen twice to me.
The first time, it was probably because I was working out. Second time because the pocket’s there. They had to drain it, so I had those 2 things.
With the actual lumpectomy, no issues. It’s right around my nipple. But the most problems I’d been having is with the actual clot underneath my arm. That stops any mobility overhead, and then it started to cause some tightness through my peck. On top of that, then you add radiation.
Radiation also tightens all of this. The mobility becomes worse once radiation starts. I started radiation a month after surgery.
You still had to get infusions after radiation
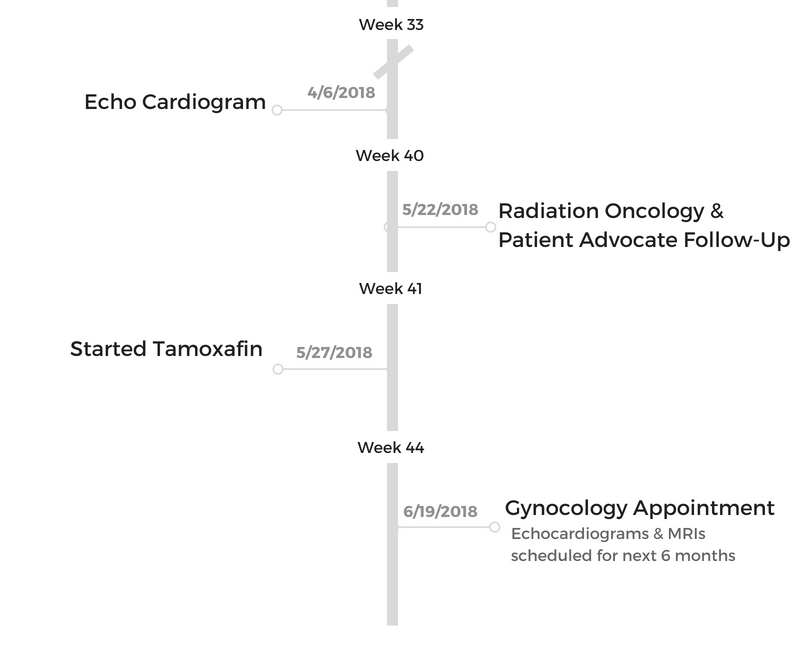
After radiation ended, I went for my infusion. I was still getting infusion of Herceptin and Perjeta because my chemo is estrogen- and progesterone-based.
It’s fueled by estrogen, which we naturally make in our body, more so as females. Now that just blocks it. It was part of my chemo the whole time.
It was the last 2 that I would do. It’s a “non-chemo chemo,” is what I call it. I do that every 3 weeks until end of September.
How long will you take hormone blockers?
Because I’m not menopausal yet, I don’t know if that’s going to kick me into it. I take a pill for 5 years or until menopause, and then they give me another pill for another 5. So total of 10 years on hormone blockers, which should kick me into menopause.
Those will be every day for 10 years or until something better comes around. I’m trying not to go down the Google path of that yet. because everything I read about tamoxifen is horrible.
I’m hoping maybe something will come out better in that 10-year period that won’t be so damaging to my system.
Hair Loss
Talk about the hair loss

My hair was down to my waist. Big, Italian hair! Not big-big, but I have a lot of hair. Thick eyebrows, eyelashes for days, that kind of thing, so yeah, it’s a vanity issue.
I worked out. I didn’t want to look as manly; I guess that’s the best way to put it. It makes me more feminine, I thought. That has always been my thought process around my hair.
That could be a security blanket. At this point, it doesn’t bother me anymore because I’m so used to it, but it was huge.
Losing your hair and that whole process around it, it’s a big one. That now shows everybody you’re sick. Whoo. That was big.
When I had gone into my first chemo, I started talking to the nurse who was giving my infusion, and I said, “What do you think? When do people normally lose hair on this? Because everybody has a different cocktail.” I did the whole WebMD and every single site and looked at when you lose it. Of course, they were saying quick.
Other people were saying not so quick. She had told me 2 weeks. That frightened me because that was quick. I questioned it, then she moved to maybe a month. I asked her to tell me the truth, and it ended up being 2 weeks.
»MORE: Dealing with hair loss during cancer treatment
What motivated you to finally cut it the first time?
That first week, I had my hair in a ponytail, and then I brushed it a little bit. Second week, my hair started to fall out in the brush, so I stopped brushing it. Put it up into a hair tie.
I’d wake up, and there’d be clumps of hair in my bed. Then I’m like, “Maybe if I don’t touch it, it won’t fall out.” It just looked horrible, so at a point, I was talking to one of the owners of my gym. He’s like, “Fuck it, I’ll just shave your hair.”
I’m like, ‘I don’t know if I’m ready for that.’ It was almost 2 weeks. Then I went home, and a big chunk fell out onto the floor. I texted him. I said ‘All right, let’s do it.’ He said, ‘I’ll bring my clippers in, and we’ll do it.’
I let my friends know I’m going to do it at the gym. This is the time. Probably 10 of my friends came. The guy that was initially going to do it didn’t do it. He wasn’t there, so I looked at one of my other friends, and I’m like, “How are you with clippers?”
He’s like, “I’ll do it.” Great. [We] went out to the patio porch and started with fun hairdos — mohawk and half my head — and then just shaved the whole thing and had a couple beers.
Just shaved it. It was probably a little bit longer than what it is now. It was probably what they call a 4-clip. That was 2 weeks in.
When did you shave it all?
From there, it started falling out more and more. By week 3, one of my other friends came over and shaved my head for me. That was it. I went completely bald.
I still had really big eyebrows and eyelashes, so I just bought a lot of earrings with my girlfriend, Elise. We went out and bought some cheap hoop earrings, and I just rocked it.
I work for a tool company for construction, and 4 guys in my office are bald. I have to walk in now one day with hair and the next day bald. I started taking pictures with all the bald guys at work.
It was called ‘Project Baldy.’ Any time I travel out in the field and guys are bald, I’d get another picture and get another picture. I asked advice for shaving heads, and that’s kind of the way that I dealt with it mostly.
Describe the emotional part of hair loss
It’s more the sick part, I think. Right now my hair is short. It’s not what I want, but it’s cute, and I’m cool with it because it feels like I’m doing this intentionally.
Being bald puts you into this whole other place of being the sick person, and that just makes me feel less viable.
I just don’t want to feel like the sick person. I don’t want to feel like that weak person that’s gonna die. It puts you that much closer to being what you don’t want to be.
It’s not even the imagery for anybody else. It’s the imagery of yourself looking into the mirror that’s so bad. It’s horrible seeing that and trying to figure out how do I make this me? You’ve just lost who you are right there in one second.
Everything you’ve seen yourself to be is gone. You’re still there, but it’s not who you imagine yourself to be. It’s bigger than dressing up for Halloween.
It’s like not many people put a bald cap on as a female. It’s not cute. Everything you’ve ever been told is never that.
I think the good part was for me was embracing it and just, “This is who I am now.” Finding ways to make it fun.
You had to learn how to draw in your eyebrows
I’m so not “chicky” either. I went to Sephora. There’s this one girl that did a really good job with her eyebrows, and that was what I was focused on.
I’m bald and looking at her eyebrows. She’s looking at me, and I’m like, “Can you help me?” She’s like, “What do you need?” I told her I needed eyebrows and needed them to look good.
She brings out this stuff, and I’m like, “You need to show me how to do it. I don’t want you to do it for me. I want you to show me how to do it.”
She spent so much time with me. [She] taught me how to do it. [It] was amazing. I gave her a huge hug at the end and have been doing it ever since. Hopefully the eyebrows come back, but right now it’s not as important.

Your hair hurt as it fell out, especially your eyelashes
Yeah, itchy. My head would get really itchy.
The worst part was my eyelashes. My eyelashes hurt a lot when they were falling out. You wouldn’t think as small as they are that they’d be as painful, but it was like little spikes.
Did you wear wigs?
They have a bunch of free places that you can go to that they’ve donated wigs, and of course they’re granny wigs. Horrible, horrible granny wigs. I did the whole “mom” style. Really short, blonde — and I’m not blonde at all.
I tried on afros and all sorts of stuff. I ended up with one big, huge for-real afro that I thought I would wear out one night for fun. I didn’t. I brought it back.
I tried to find anything that would look like me. I went to even nicer places. Beautiful wigs. I just never felt like myself, so I just never did it because of that.
Itchy. Hot. It was too much work. I ended up wearing scarves around my head. Luckily, it was winter, so I wore a lot of big scarves just kind of over half my head. That was fun.
Did you try cold caps to save your hair?
My stuff started to fall so fast. I talked to the lady there. It seemed like a lot of work. You have to have somebody with you for a couple hours beforehand. Then hours afterward. It was so expensive.
If I spend $2,000 over the time that I’m doing this to save my hair, it seems stupid, vanity-wise, for me.
Other people have done it, and good for them. But I’d rather take that $2,000 and go on vacation when everything’s done. That’s what I did. Hawaii!
Work & Finances
Doreen’s video on working during treatment
Did you work through chemo?
When I was diagnosed, I called my boss right away when things looked funky.
I said, “Look, I have some stuff going on. It doesn’t look good. I’m not sure what that means yet. It could possibly be cancer. I’m not sure, but I’ll let you know when that happens, and we’ll talk about what that looks like.”
When I was diagnosed and had my full plan, I called him and said, “This is what’s going to happen. This is how it works. These are when it’s scheduled. I’d like to still work through it and see if I can do that, because I think keeping busy is going to be better for me than wallowing and thinking about cancer all the time.”
That was my thought process. I have 2 jobs, and it was like that for both. My other job is at the gym at night, so that becomes another piece of the pie. How do I stay awake for that long? Can I handle it for that long?
My gym was amazing in terms of that and said, ‘Any time you need coverage, we can do that.’ I used that as much as possible, but I also used the gym as a place that would keep me involved, keep people on me, and keep people seeing me and helping me mentally.
I would work out with them and teach them. I could teach from seated position if I needed to. I spent a lot of time sitting down and talking to people from there or getting up, walking over, helping them, and sitting back down.
But I had desk work, too. For my desk job during chemo week, I’d work up until the day of chemo. From chemo, I would work from there, so I could just do emails and phone calls during chemo. That was perfect. Then that Friday I was usually pretty clear, so I could do that and work.
The week after I couldn’t fly, and I couldn’t be on the train or anything like that, so I’d work from home during that week. Then that following week I would fly.
I would get on the plane. I would wear a mask, and I would fly places. I wouldn’t fly any more than 2 hours. That was my goal. As long as my white blood cell count was fine, I was free to do that.
As time went on, I would be able to do it the second and third week. I could keep things together; I could answer emails. I could do my work, but I couldn’t do anything super detailed. Looking at Excel spreadsheets took me really long periods of time to focus.
I was pretty open with the people that I worked with, like, “I can do this, but I can’t do this. If you could take this for now, I can work on this for now.” I picked up a lot of the smaller stuff, the less-detailed stuff, the busy work. That was good.
Once I could travel, I didn’t have to do a lot of that busy work. All I had to do was be supportive and helpful and be able to come up with things in my head. I would mostly write those down or know them pretty well.
Did you work through radiation?
I did not work through radiation.
I worked through my first week of radiation, and right now I’m on disability. My disability is 2 months total.
Now, I’m starting to heal and be able to stay up later than 8 at night. Usually during radiation, I would sleep probably at 11 p.m. and take a nap.
Then I would pass out narcoleptically around 8 p.m., then wake up at 2 a.m. and be up all night. There are different cycles of not sleeping and sleeping.
How was dealing with insurance during treatment?
I have a high deductible. The low deductible insurance was more money in the long run because people apparently don’t use all their insurance, shockingly.
[For] my insurance, I had a full all-in from September to December. I spent about $20,000 on top of my insurance, so that’s pretty shitty because that’s including what I pay for my insurance monthly.
That was my partial deductible. It falls into this co-insurance, and that was also all out-of-network. Out and partial was $20,000. So now that reset in December.
Through my work we deal with a company called Compass. I would send all my bills that I paid to the lady at Compass, and she would go and check them. Things that had not been marked off, she would deal with.
I had a lot of confusing back and forth with her. I think partially because they’re confusing and partially because the insurance companies are confusing.
A piece of it was I couldn’t focus because of the chemo, but it all worked out in the end.
Mental & Emotional Care
What were hard parts of cancer you didn’t anticipate?
I think the hardest part about cancer is that in the beginning at least, it’s not about you. It’s about everybody else.
It’s like trying to make them feel comfortable. It sucks, and it’s lame. People are shitty sometimes. The death stories and the stories about people they know who have died of cancer, the rambling of stupid stuff.
That was the worst part. I think the baldness is less of that, but it opens up the door for random people to start telling you cancer stories and death stories.
I started getting a little bit East Coast on them. I would have conversations with people who’d start stories, and I’d be like, “You’re not telling me a death story, are you?”
That whole baldness brought out a lot of that stuff.
Did anything surprise you?
A lot. Everybody says this, but there are people who stick around, and there are people who go away. I was surprised by the way people deal with it and make it about themselves.
I’m surprised that random strangers who have come up to me, mostly good in terms of seeing me, seeing me bald, knowing what’s going on, and directly asking me if I have cancer, which is strange.
I’m surprised by how encompassing it is. A constant. There’s not been in 9 months a week that I have not had an appointment. Still going through that.
That’s a lot. If I knew that before and people told me that, you don’t understand the enormity of it.

A sense of humor is important
You have to [make jokes]. You have to. When people see me drinking and say, “Should you be doing that?” I’m like, “What’s that going to do? Give me cancer?” Then they get all awkward.
The best thing my oncologist told me — I think it was in cycle 5 of chemo — she’s like, “You need to use your cancer card.” I was like, “I don’t know. It just doesn’t seem like I should.”
She’s like, ‘No, this is the time. Use your cancer card.’ I’m like, ‘I don’t even know what that means.’
She’s like, ‘Use it when you need to get out of things, or you just need something and you’re not getting it, or just use it. Use the cancer card.’
Any advice to people who’ve just been diagnosed?
Use all the things. Anything that’s been suggested in terms of free services or trying things out. Try everything. See if it fits for you.
Don’t just listen to people. I think you have to make your own decisions. And cry at will.
I don’t care about a lot of stuff anymore. Not as important. Like, eh. I eat what I want. I drink what I want. I’m not worried about those things yet.
Be your own advocate
You have to. If I hadn’t pushed on along the line, it would be bigger and worse. I had already been diagnosed, and I’d already started chemo when I got a call back from the secretary of my [original] gynecologist’s office, seeing if I wanted to come in for a mammogram.
I’m like, “Have you not seen any of records that were sent to you? Because of you guys, I had this, this, and this happen to me. And I have breast cancer. I think you guys should know that you did not help me in any way. In fact, you were a block to my health care.”
Another example is there was this shot. It was something different. It’s a shot that they were going to add to my regimen that would make you horribly poop. It was going to be explosive diarrhea.
I did all this research at the end, and I said, “Why do I have to do this? These are all the side effects. How is that going to help me if it’s a 1% chance [of helping]?”
We started a debate back and forth, but for me it was more of the I’d hear it, then I’d sit on it, sit on it for a couple weeks, and come back with it. I needed to absorb it first.
As long as you’re thinking about it, coming back and talking about it, and you’re getting the response that you either need or the response that at least makes you understand a little bit more, then I think you’re okay.
But if you’re not getting that, you need to seek it elsewhere. Do it.
Be prepared for the sudden drop-off in care and attention
That shift is hard. It’s like, bink, you’re done, and there’s less care, which is weird. I feel better that I’m not that important, right? It’s a double-edged sword of it’s cool, but it’s hard.
Another thing I guess I didn’t realize for myself is that I now am a lot more open about talking about things than I ever was, because people along the line would ask me questions about cancer in general or how I’m doing and that kind of thing.
Before, I’d just be like, ‘Yeah, I’m fine.’ Just throughout the whole process, I would tell people, ‘This is how I feel. This is what it feels like. This is what’s going on. This is why I’m in the process.’
Draw boundaries with people
I didn’t draw boundaries that made other people feel comfortable after a while. At first, it was like I realized it was all about them, and it had nothing to do with me.
Then I stopped getting into those conversations with people. The conversations I had as I got through more were more for my benefit.
For me to think about stuff, it was less about making other people feel comfortable. I think it was an interesting shift. I don’t know when it really happened.
You’ve got to feel that out for yourself. Everybody’s got to go through whatever’s comfortable for them.

Inspired by Doreen's story?
Share your story, too!
Invasive Ductal Carcinoma
Amelia L., IDC, Stage 1, ER/PR+, HER2-
Symptom: Lump found during self breast exam
Treatments: TC chemotherapy; lumpectomy, double mastectomy, reconstruction; Tamoxifen
Rachel Y., IDC, Stage 1B
Symptoms: None; caught by delayed mammogram
Treatments: Double mastectomy, neoadjuvant chemotherapy, hormone therapy Tamoxifen
Rach D., IDC, Stage 2, Triple Positive
Symptom: Lump in right breast
Treatments: Neoadjuvant chemotherapy, double mastectomy, targeted therapy, hormone therapy
Caitlin J., IDC, Stage 2B, ER/PR+
Symptom: Lump found on breast
Treatments: Lumpectomy, AC/T chemotherapy, radiation, hormone therapy (Lupron & Anastrozole)
Joy R., IDC, Stage 2, Triple Negative
Symptom: Lump in breast
Treatments: Chemotherapy, double mastectomy, hysterectomy




