Tina’s Stage 3A ER+ Invasive & Lobular Breast Cancer Story
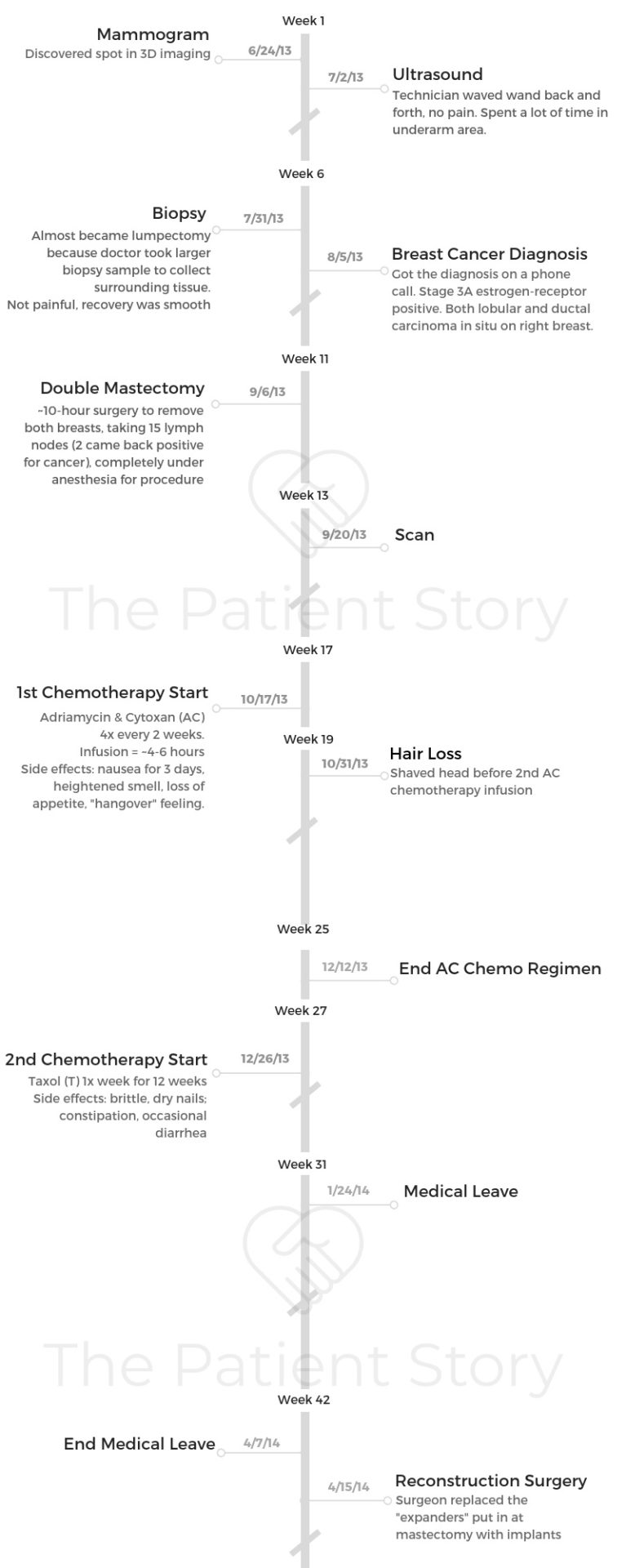
Tina shares her in-depth story on getting diagnosed with stage 3A breast cancer after noticing a sunken nipple. She details undergoing a double mastectomy, chemotherapy, radiation, and hormone therapy.
Tina also highlights how she managed through the trauma of losing her hair, dealing with work and finances through treatment, and the importance of self-advocacy as a patient.

- Name: Tina C.
- Diagnosis:
- Breast cancer
- Ductal carcinoma in situ and lobular carcinoma in situ
- Estrogen receptor positive (ER+)
- Staging:
- 3A
- 1st Symptoms:
- Sunken in nipple on right breast
- Treatment:
- Double mastectomy
- Chemotherapy
- Adriamycin & Cytoxan (AC)
- 4 times every 2 weeks
- Taxol
- 1 time a week for 12 weeks
- Adriamycin & Cytoxan (AC)
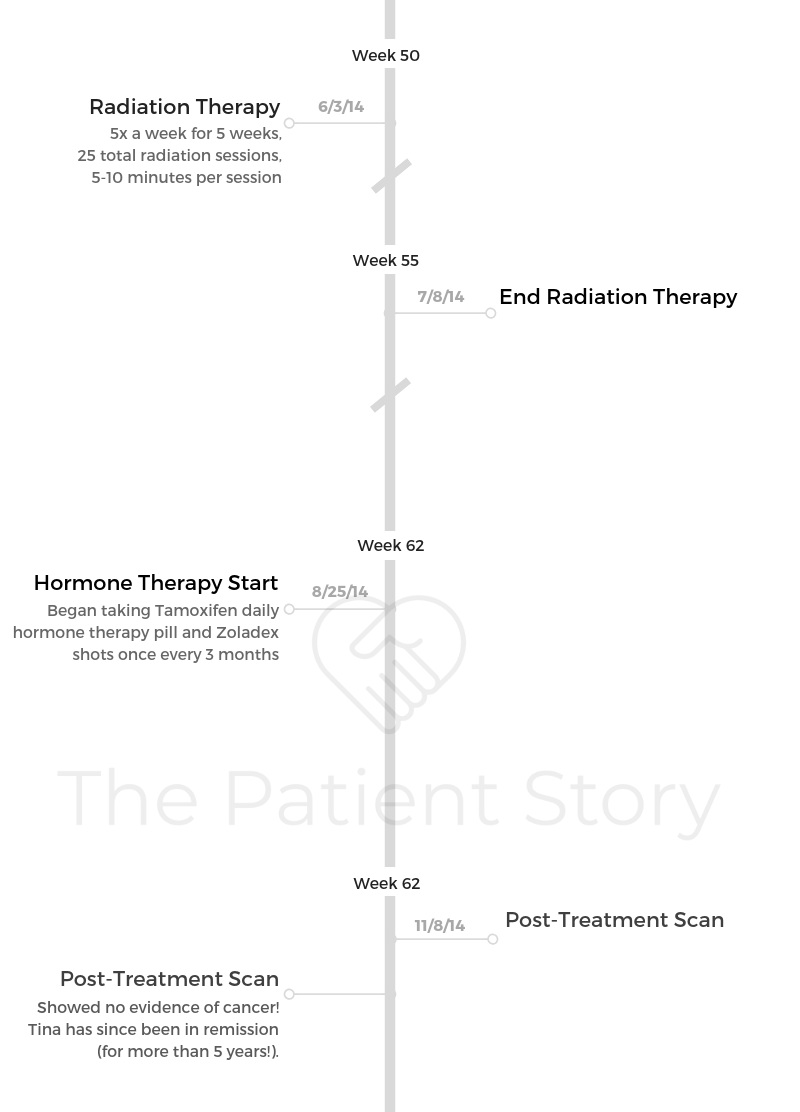
- Radiation
- Hormone therapy
- Tamoxifen: 1 pill daily
- Zoladex: 1 shot every 3 months
- Diagnosis
- What were your first symptoms?
- Describe that first primary care visit
- Differences during this mammogram
- It moved quickly to a diagnosis
- Describe the mammogram
- Describe the biopsy
- What do you remember most of the biopsy?
- How was the wait for test and biopsy results ("scanxiety")?
- How did you deal with the wait for answers?
- Describe the moment you got “the call”
- How did you break the news to loved ones?
- Do you remember how your oncologist described to you what 3A estrogen positive means?
- You had both lobular and ductal carcinoma in situ
- Treatment Decisions
- Did you get a second opinion?
- How did you find your oncologist, surgeon, and radiation oncologist?
- How did you decide who to go to for treatment?
- Describe the treatment center you went to
- What did you like about it?
- Did you make the decision to undergo a mastectomy?
- Did you have a choice to pursue chemotherapy?
- Surgery (Double Mastectomy)
- Chemotherapy
- Reconstruction Surgery
- Radiation Therapy
- Hormone Therapy
- Hair Loss
- Work & Finances
- Support & Care
- How did you manage the mental and emotional stress during treatment?
- It’s hard to slow down for many. Any tips?
- Were there big surprises during treatment?
- Finding your community
- Were there moments you had to self-advocate?
- How important was it to have caregivers around?
- Any advice on how to ask for support?
- Survivorship
This interview has been edited for clarity. This is not medical advice. Please consult with your healthcare provider for treatment decisions.
It’s definitely a roller coaster. There’s going to be ups, and there’s going to be downs. In some ways, you’ll appreciate the journey. Looking at it on the other side is just totally different. It’s amazing, and you just appreciate more, but it’s not easy.
You have to talk to somebody if you find yourself just staying in a down place. You need to.
Tina C.

Diagnosis
What were your first symptoms?
I remember at my wedding thinking something just seemed a little different with my breast. That was in April of 2013.
The nipple on the right side had sunken in a little. I thought, “Oh, that’s odd or strange,” but I really thought, “Oh, getting old sucks,” even though I was 37.
In my mind, it didn’t really click, even though my mom has had breast cancer 2 times. It was always a lump, so I just ruled it out for a little while.
Another couple of months passed. Something happened with someone at work, totally unrelated to breast cancer, but it just made me take inventory of my own health.
I was like, “You know what? This hasn’t changed with my breast. I don’t know what’s going on, so I’m just going to go have a talk with my OB-GYN.”
Describe that first primary care visit
I went in about June and had a conversation with her. She said, “It’s probably nothing, but let’s just get it checked out.”
I had a mammogram when I was 30, and I had one when I was 33, so I had a pretty good baseline at that point in time.
She scheduled my mammogram pretty soon thereafter. I went in and got the mammogram. It seemed normal, so everything seemed to go the way it had in the past, except I got a call back about another week or so after the mammogram that something was abnormal and that I needed to come in. That was definitely unique to what had happened in my previous mammograms.
Differences during this mammogram
For the second mammogram, my husband went in with me. From there, they did an ultrasound. They had never done an ultrasound before.
They were spending a lot of time in my armpit area, which I knew enough about my mom’s diagnosis to know that that’s where your lymph nodes are. Something’s obviously unusual.
They wouldn’t tell me anything while I was lying there, so I had to wait until the doctor could come and officially read it. He came in and said, “Well, I know you know something’s not right.”
They needed to do a biopsy. I could choose to either do a needle biopsy or meet up with a surgeon and have a surgical biopsy.
Because of my mom’s history, I did choose to meet with a surgeon and go that route. From there, I did do the biopsy. I think that was in probably late July.
From that biopsy, I woke up to my breast surgeon telling me, “I think you need to get your mom’s records.” That was the first thing I woke up and heard.
That was on a Thursday. I took Friday as a mental day. Then on Monday, I got the official diagnosis that it was cancer.
It moved quickly to a diagnosis
It escalated pretty quickly. It was good that everyone took me very seriously, even though I was 37.
I think that me having my mom’s diagnosis gave me some credibility. Nobody second guessed what I wanted to do. Everyone was very obliging of what I needed to do.
Describe the mammogram
The mammogram was just a normal mammogram, where it squeezes one breast at a time. I’m not very large-chested, so I never had any pain or any issue.
Nobody really reads you the results right then and there. Certain clinics have different procedures, but the one I was at, they definitely waited. Your actual doctor talked to you about it, or sometimes you get the thing in the mail later that everything was okay.
The ultrasound was a wand going back and forth, back and forth. They were looking at the breast with the wand, but they were spending a lot of time in my underarm area. Then another person would come in.
I think the hardest part was nobody would talk to me, so it was really frustrating. I’m a human being sitting here. Can’t you at least just tell me what is going on?
I understand that there’s procedures. Different people read different things, and only certain people can also tell you what’s happening. I was not naïve enough on this case to know that there was probably a problem.
It felt very frustrating to lie there. I remember lying there with the ultrasound wand and just having a tear go down my face because I knew something was happening, but nobody would talk to me.
»MORE: How to be a self-advocate as a patient
Describe the biopsy
It actually ended up being almost a lumpectomy because when she got in there, she could definitely tell things weren’t right. She took more than what a tiny needle biopsy would’ve done. It is almost like she performed a lumpectomy and tried to take the surrounding tissue as well.
It wasn’t very painful, and my recovery wasn’t very hard. It was the tip of the iceberg, so emotionally it was very hard and very difficult, but physically it wasn’t that big of a deal.
I’ve had so many surgeries. I think it was just local [anesthesia], and I went home later. It was an in and out. Obviously, the mastectomy is totally, totally different.
I had some bandages and dressing to change. I remember more the emotion than I remember the physical part of it.
What do you remember most of the biopsy?
Just to hear, “Get your mom’s records,” was truly, truly eye-opening. I always felt in my heart that me getting breast cancer was definitely possible, but my mom was 46 when she was diagnosed. I never in my wildest dreams thought I would be in my 30s. I don’t know why. I just thought that seemed crazy.
I thought if it would happen to me, it would happen later in my life. My mom did get her records in order and get everything sent over. I spent the weekend calling everyone that I loved and telling them, “Hey, this is likely going to happen.”
It was very emotional, but it did allow me to process it with a bunch of people a little bit before I even heard the official diagnosis.

How was the wait for test and biopsy results (“scanxiety“)?
Each was probably a couple weeks. It seemed the wait got shorter the more engrossed it was. From the first mammogram to the second mammogram, it was probably a couple weeks.
Each thing just seemed to take some amount of time. It was probably 6 to 7 weeks from that point to get the full diagnosis. I had my biopsy on a Thursday. I got my official diagnosis the following Monday that it was cancer. By the end, things were moving rather rapidly.
»MORE: Dealing with scanxiety and waiting for results
How did you deal with the wait for answers?
I tried to just live my normal life. I had been promoted in February of that year, so I had still a relatively new job. I really just tried to immerse myself in work and my life. Not trying to worry about it so much, but then everything had to change once it became a cancer diagnosis.
Leading up to that point, I felt like I just tried to — I don’t want to say ignore it, but just tried to remain calm and just be myself as much as I could.
Describe the moment you got “the call”
I’m sure my story’s not too unique to anyone else’s. Even with having the doctor tell me on Thursday that, “Hey, get your mom’s records,” there’s still just this glimmer of hope that everything is for some reason going to be okay and not a cancer diagnosis.
I went back to work on Monday. I think I got the call 3:30, 4:00 in the afternoon from the doctor. I walked away from my desk. I remember them saying, “You have cancer.”
It’s just the hardest thing. The whole world stops. Everything that you felt and hoped and wanted to do — just everything just suddenly changes.
I often say it’s just a line that’s drawn. You can never go back to that pre-period. It’s just different from that point forward, so life as I knew it definitely changed. For the next year, everything definitely changed.
It is that raw emotion. It just really comes back and takes you back to that very day that you found out.
»MORE: Processing a cancer diagnosis
How did you break the news to loved ones?
My husband actually worked at the same place as I did, so I emailed him and was like, “Hey, we’ve got to go.” I’m sure he knew at that point.
Plus, everything leading up to it. In the car I was able to just be sad and let it all out. I waited to tell everyone at work maybe a week, just to give myself some time to process it.
We actually set up a meeting. I had a good discussion with my boss. At that time I was leading a team of about 10 people, so we invited the whole division basically. My boss framed it up like, “Hey, we are a family, and sometimes families go through tough times.”
It was good to have their support from the very beginning, understand what was happening, and to hear it more from me and not hear it just through the grapevine.
I’m definitely more of an honest person who’s just going to tell you what’s happening. Let’s find the best way to treat it and to move on.

I think it was probably the hardest for my mom. She was living in Michigan, and I was living in Chicago suburbs at the time. For her to be 7.5 hours away, she definitely felt a lot of guilt.
She felt like she caused it or it was because of her genetics or something. She had a really hard time dealing with it at the beginning.
I remember one of my aunts who lives in the same hometown emailed me and said, “Your mom is really not taking this well. She’s blaming herself. She’s just not doing good.”
I called her, “Hey, I heard that you’re not taking this well [and] that you’re blaming yourself.” She’s like, “Yeah.” She got really quiet.
“Well, I can’t worry about you doing this. I don’t blame you.” I told her I didn’t blame God. I just told her, “Hey, we just have to deal with this. We just have to move forward and deal with this.”
I released her of those feelings. She could come to terms with it. [She] just supported me in the best way that she could from that point forward.
She couldn’t obviously make it to everything, but she came and stayed with me for a week during my mastectomy and my first chemo. Definitely, she was the hardest one to break it to, outside of my husband.
»MORE: Breaking the news of a diagnosis to loved ones
Do you remember how your oncologist described to you what 3A estrogen positive means?
I tried to negotiate with him.
Tina: How about 2C? There’s not a lot of difference between 2C and 3A.
Oncologist: No, it’s really 3A.
Tina: Yeah, but 2C just sounds so much better.
I remember having that conversation with him, but the size of the lobular mass that I had [was bigger]. I also had ductal cancer. It is crazy that I had 2 kinds of breast cancer.
I don’t even have the same cancer that my mom had, which is even crazier. That was very interesting to learn. My mom had triple negative; that’s a very tough type to have, and it’s usually very ferocious.
Mine is some blessing. I had multiple conversations, I remember, talking to my breast surgeon.
Tina: Well, is this a better kind to have then?
Breast Surgeon: The fact that there is a treatment that after chemo can help you, then yes. That is the better thing.
We had our conversations about it, and the fact that mine is hormone receptive — there are drugs that can help me post-treatment — was a good thing to have and to understand, even though that drug for many people comes with a lot of side effects.
You had both lobular and ductal carcinoma in situ
Yes. Lobular is like spider-web crazy, and that’s actually what pulled the nipple in. Ductal was more like a lump in the ductal gland. That’s the kind my mom had.
Ductal typically forms a lump, but the lobular is just this mass of a spider web, and it’s just messy random things growing together. Both were on that same right breast.
Treatment Decisions
Did you get a second opinion?
I think they were still staging it at that point in time. With the fact that I had a surgeon, it wasn’t just some needle biopsy, and that she got in there and clearly could see something — I guess I felt that this with my mom’s prior history, too, that we just need to move forward.
I was pretty clear with my surgeon from the beginning, like, ‘Hey, if this is going south, I want a double mastectomy. That’s just what I want.’ She was always very accommodating of what I felt I needed.
How did you find your oncologist, surgeon, and radiation oncologist?
I lucked out. I just felt most all my surgeons fell into place. It seems my OB-GYN had worked very closely with the breast surgeon that I had, and I really her. She worked very closely with a plastic surgeon. He was really great to work with for reconstruction.
She also was familiar with an oncologist, so that’s how I got in touch with him. They were all in the same network or same hospital, because they all shared the same operating rooms and different things.
The only one that I bucked the trend on was my radiation person. After a consultation, my husband was, “No. I’m not allowing it.” I just had this feeling, and then he verbalized what I felt. He was just like, “No, we’re going to get somebody else.”
How did you decide who to go to for treatment?
I’ve talked to other survivors, and it’s amazing. I always say, “Listen to your gut.” You want a smart person, and you want someone very capable. You do want good bedside manner. I’m not saying that’s most important, but you do want some good bedside manner.
[The first surgeon] took 2 personal calls during my consultation, left me with an iPad, and said, “It’s this, but it’s not.” I was like, “Well, what part is that? What part is not?”
I was also like, “If you can take 2 personal calls to an appointment that means the world to me, then I don’t think it means the world to you.” I think you just have to find a doctor that you feel is as invested in this, in your cancer journey, as you are.
If you don’t have that feeling, you should get a second opinion. You should talk to somebody else. There’s always options.
They might not be as convenient, but you should always look into options if you don’t have the feeling that they’re on your team.
Describe the treatment center you went to
It was fairly newer and fairly mid-size probably. It was part of Advocate Hospital, which was a bigger network in Chicago, but it was one of the outlets for it.
What did you like about it?
I would definitely say for me it was convenient. I don’t feel people should just make a choice based off of conveniency, but it was convenient to get to for still trying to work and still trying to have some normalcy to life.
I knew other people who would go downtown Chicago from the suburbs, but you’re talking maybe a 2-hour drive there, 2-hour drive back with traffic, depending on the time of day. It was on my way home from work. I could schedule things easier with my lifestyle.
I actually felt the caliber of doctors was amazing, the people that I had. I don’t know if I just lucked out with the team that I got, but once I had that team, I really felt they were a dream team. They just all gave me such great advice. They even advocated for me.
I ended up taking a medical leave at one point in time because my oncologist asked me tough questions, and I needed it.
Oncologist: Who’s your advocate at work?
Tina: My manager. She cares about me.
Oncologist: No, no, no, no. I’m not talking about caring. Who is your advocate at work?
Tina: I don’t have one.
Oncologist: Well, then I really need you to consider taking a medical leave.
He just put it in very black-and-white terms that I needed to hear. He was very resolute, like, “You need to consider this.” He wouldn’t tell me necessarily what to do, but he would always put it in a way that was black and white.
Sometimes when you’re so confused in the whole process, you do need someone that tells you [how] it is. I’ve always felt like that’s how he would treat his friends. That’s how he would treat an aunt.
He would do the same thing to any one of us, so I just appreciated his candor and his honesty all the time.
Did you make the decision to undergo a mastectomy?
I definitely was an advocate for it, in that my one side ended up having lobular and ductal. Lobular was pulling the nipple in and was a hot mess inside there. I think lumpectomy would never even have been an option for that side.
I just didn’t want to have to worry. I wanted things to be symmetrical. In my mind, my mom had a lumpectomy, it came back, and then she got a double mastectomy. That just meant some more peace of mind for me.
But I understand their statistics. Everything’s always changing. Maybe it’s not necessary, but for me I did have peace of mind doing it. No one ever really questioned it, and it wasn’t a difficulty at all.
Did you have a choice to pursue chemotherapy?
My oncologist showed me a piece of paper, and I used to think that I liked statistics, but then he made me realize I’m not sure if I do.
He told me if I did no chemo and no radiation, my chances of dying from cancer in the next five years were 50%. That’s pretty humbling news, so in my mind, that’s not an option.
Surgery (Double Mastectomy)
Describe the prep before the (double) mastectomy
I remember going in early in the morning, talking with the anesthesiologist, and them wheeling you back. It was a really long surgery. Between taking both breasts, checking the lymph nodes, and then putting expanders in, it was about a 10-hour surgery, maybe 11, which is a very long time for anyone to be under.
I even had my in-laws come and stay with my husband because I was worried about him just being there by himself for so long, too. They came and were part of it, which was amazing to have that support. If it’s a double (mastectomy), just plan that things can take a very long time.
Describe the double mastectomy
I understand some people start off with chemo to see if markers are shrinking and different things, but in my case, they wanted to do the surgery first. They did the double mastectomy right after Labor Day. Within a month of my diagnosis, I had the surgery done.
They took 15 lymph nodes on the one side, and then the other side they took off as well. Of the lymph nodes, 2 came back with cancer in a macro way and then 2 micro, but definitely 4 were impacted by cancer.
The good news is there were 11 that were not, and that was pretty much the extent of the cancer, from the scans and everything else. The surgery was very challenging.
It’s just a testament to being in a weird position for so long. There can be other side effects, actually. My toe hurt for a couple of days, which is crazy. I’m not saying that’s going to happen to anybody else. but just the way that they position you and being under for so long, you know it’s a long time.
I remember coming back to the room, and at first I felt really great, but I still was probably under the pain medication, everything that they had given me. Then a wave of just feeling nauseous and horrible. Then a nurse came in and said, “You look so pale; we’ve got to give you something.” I had to take some more medicine.

That first night was pretty rocky, and I spent 2 nights in the hospital. On that third day, I went home. By then I was ready to go home, but that first day and a half, it’s really tough.
I have never been in a hospital since I was an adult, so it’s just difficult to have someone come in your room and check on you every couple of hours.
Those machines, when your legs are moving and making noises, it’s just a whole different world. Some people are maybe more used to it from having surgeries as an adult, but for me it was definitely a learning curve.
»MORE: Read more patient experiences with surgery
What were the side effects after surgery?
You’d go home with drains that had to stay in for 2.5 to 3 weeks. Then you had to go in and see your surgeon. They put expanders in at the same time to get the skin ready for the upcoming implants.
The whole mobility thing was really, really challenging. Mentally I felt fine. I wasn’t really tired afterwards. I could walk [and] do things, but just learning how to eat cereal or just put on a shirt was very, very challenging.
I wanted to wear button-down shirts because it’s just really difficult to get anything over your head and raise your arms.
I remember eating cereal with my left arm because I felt [like] a caveman, but I felt a caveman either way, whether I eat with my right hand or my left. It was just crazy to relearn some things that are so simple.
I did these “Itsy Bitsy Little Spider” exercises all the time to run your fingers and stretch your mobility. I definitely took it seriously and tried to work on all the exercises they had you do.
When you’re in the midst of it, you just feel, “Am I ever going to be normal again?” It’s definitely a very slow and gradual journey. From that point forward, it takes a long time to feel right again.
How long did it take to recover?
The first week at home, my mom was with me, so she did all the cooking [and] all the laundry. It was very helpful to have someone there, because I couldn’t lift. I was very limited in what I could do.
I don’t even think you can even lift a half gallon of milk. You’re probably not even supposed to. You’re very limited in what you can lift and how much weight your arms can raise.
I couldn’t take a shower because of the drains, so that was really difficult. Had I thought things through, I would’ve maybe cut my hair shorter, knowing I was going to go into chemo and do that next. Just because the showering part or having to take a bath is so much more complicated, and obviously brushing your hair is really difficult.
It’s pretty humbling to be 37 years old and having your mom give you a bath and comb your hair and do all those things. You’re an independent woman, so it’s really difficult and humbling. But I made it through, and all I wanted to do was shower. It was my end goal.
I do remember when the bandages came off, and at that point in time, my mom had stayed with me for a week. My best friend had come and stayed with me for 4 or 5 days, so I was finally alone. The weight of it all was just enormous.
Seeing myself with just this body I didn’t recognize, the emotional toll of it — that was really hard. Probably more than even the physical part of it.
Describe the drains
They fill with fluid, but you had to measure the contents [to see] how much was draining. I had a little checklist, and we had to get it down. When they finally got to a certain amount low enough, then the drains were able to be removed.
Basically, it was tubing inside of you that connected to this little bulb. For me to leave the house and go do anything, I had to pin the [tubing] together. I didn’t want them showing, so I had to hide them in some way.
What were the expanders put in during the mastectomy?
They put in these expanders, and then they would fill them every week or every 2 weeks. I’d go in and see my doctor, he put a little more cc’s [of fluid] in [the expanders] each time to gradually stretch the skin so that next April I had the exchange surgery. Then those expanders came out and actual implants went in.
Chemotherapy
Describe the surgery to put in the port (used to deliver the chemo)
I didn’t have any issues with it. You could shower. I think you could go swimming, even though swimming was obviously not advisable. You could do whatever and live your normal life.
To me, it was more so I just felt like an alien. If you just have this weird thing sticking in your upper chest, your clavicle area, it just looked weird. I just felt like I looked like a mutant or not a human.
But it really was convenient because, obviously, they don’t have to find veins every time, and you don’t have all that. I was fortunate I never had any infections or any issues with it. It actually was quite a convenience once I look back and look at it now.
What was your chemotherapy regimen?
Chemotherapy regimen:
- Adriamycin & Cytoxan (AC)
- 4 times every 2 weeks
- Taxol
- 1 time a week for 12 weeks
I did 4 rounds of Cytoxan and Adriamycin, or the Red Devil, which is the really tough kind. They have to test your heart just to make sure it’s strong enough before they give you that stuff.
That was 4 times every 2 weeks, starting in mid-October 2013. Then I finished up Thanksgiving weekend. After Christmas, I started the Taxol or Taxotere, and I did 12 rounds of that. That was every week.
How long did the chemo infusions take?
They would do blood work to make sure your levels were fine, so my white blood cell count. The potassium is often an issue. They’d run a series of blood tests to make sure you’re okay, and then once that came through clear and your doctor could see it, then they would clear the chemo drugs for me.
Usually from the time I got there till the time I left, it was probably 4, 5 hours. Other people would get different infusions. I was just getting the Adriamycin at the time, Cytoxan, or the Taxotere, so I was just getting that.
They usually push through Benadryl at the very beginning, so you’d get this wave of feeling sleepy before I would even start, and then the chemo would drip usually for a couple of hours. Then you were good to go.
At the time, I’d have to come back the next day and get a Neupogen shot, which helps curb infection chances, but now I think they’re doing that even on the arms. People go home with it now, whereas at the time when I was doing it, I had to come back in the next day.
Describe the side effects of the chemo
- AC:
- “Hangover” feeling
- Heightened smells
- Nausea
- Loss of appetite
- Taxol:
- Brittle, dry nails
- Constipation
- Occasional diarrhea
I had really bad nausea. First time I did the Adriamycin-Cytoxan, I went in, probably administered about 10 or 11 in the morning. By the time I got home, it was early afternoon, and by 4 that afternoon I just felt horrible. It felt like a hangover, and you had no idea when or if you were going to throw up, but you just felt you were going to throw up. I felt that way probably for 3 days.
My smells were really heightened to me. My cousin was there, and she was making pancakes. I didn’t even know pancakes had a smell, but it was the most horrible smell ever. I was like, “Oh my gosh, I have to leave this level of the house; I can’t even handle it.” I was taking the anti-nausea meds that they gave me, but it was almost like I was behind, and I could never get ahead.
I would not have any hunger. I am always hungry, but I had no hunger. For me to eat maybe a teaspoon of Cream of Wheat and maybe a cracker in a day was enough. I had to force myself to even do that.

Usually by about the third day, I’d start to get hungry for something again, and then I knew it was out of my system. I tried to walk and keep active because movement is definitely good. You want to keep your body moving.
You want to drink as much water as possible, but even water I ended up hating. I ended up switching to sparkling water — it tasted so much better — and ginger ale. I tried to do different things. Even today, I still hate Ice Mountain water. It reminds me of my chemo at the hospital because that’s the water that they gave you there.
Then with the Taxol, I didn’t have as many of the food issues. I felt I could pretty much eat normally. The cumulative of the effect of the chemo was definitely brittle nails, and I tried to put Sally Hansen “Hard as Nails” every other day. I put tea tree oil on my nails. I didn’t end up losing any nails, but you could just tell they were really brittle and really dry.
I definitely had issues with constipation. It was sometimes you’d go from diarrhea to constipation even in one week. It was just a crazy roller coaster of things.
I think emotionally I just felt a little less stable with the Taxol. I just felt more anxiety.
Again, it could have just been the cumulative effect of chemo and just the whole weight of everything. I definitely felt just more vulnerable than I ever had emotionally.
What helped with the chemo side effects?
- AC:
- Emend for nausea
- Taxol:
- Constipation: MiraLAX, prunes
When I talked with other survivors that had been through chemo, they describe this Emend, which is a stronger anti-nausea. Then I talked to my oncologist about it, and he prescribed that for me rounds 2, 3, 4, and that made a huge, huge difference for me. I still didn’t feel good. I was still tired, just unbelievably tired.
The diarrhea wasn’t as common. I do remember constipation to be more so an issue, and I remember MiraLAX. I remember buying prunes. I remember my doctor telling me, “Try this; try that.” At one point, literally praying to my grandma, who had passed away, and just being like, “Will you please help me?”
That was pretty hard. I just went to a point where I don’t know what to do. My body just doesn’t seem to be working. That’s pretty tough. After I prayed to my grandma, everything seemed to get kicked into gear, so I think she’s taken inventory up there. It was really tough to handle all that part of it [and] just try to be somewhat normal.
You feel like you can go anywhere, or is that going to be the moment where nature’s going to strike and you need to go? That was difficult.
»MORE: Cancer patients share their treatment side effects
Reconstruction Surgery
Why did you decide to pursue reconstruction surgery?
I was 37 years old. I’d only been married a few months at the time of my diagnosis, so for me to feel as close to what my “normal” was, I did want some kind reconstruction.
It’s very personal. I did the implants, and I guess I always felt if it wasn’t meant to be or if it didn’t take or there was infection, I would have gladly walked away and just been fine with it, too.
But it was worth a shot to try to make me feel, in my mind, what was as ‘womanly’ as possible — to what I was before my cancer diagnosis.
I definitely have scars, and I did use nipple tattooing by my plastic surgeon about 6 months after the actual surgery. Seeing those tattoos and seeing a vision of something that looks in my mind somewhat normal, that’s actually when I got a lot of tears because I felt at that point in time I had come full circle.
Today with a bra on, I don’t feel I look any different than it’s been before. I’m very pleased with the results and how everything went.
But I do know a lot of people had a lot tougher times than me, or even infections and different things. Sometimes it’s not possible, with the skin, with radiation, and what the impact is.
Describe the process of the reconstruction surgery
That part was quite easy. You did all the fills (expanders), which stretched the skin, and then you got to the exchange surgery, which for me was April 2014.
I’d just gotten out of chemo about 6 weeks prior to that. I think the hardest part was as soon as you felt you accomplished something or were done with something, then it was a whole new ball game of something new challenging on your plate.
That surgery itself wasn’t actually too bad. I didn’t feel my recovery was too difficult or anything. I threw out the first pitch for the [Chicago] Cub’s baseball game about 3 weeks after that surgery, which is crazy. That was my fun fact, but obviously I felt fine enough to do that not that long after, with my doctor’s approval of course.
What was the tissue expander process?
They’re filling it with cc’s of fluid, and it’s just slightly expanding your breast area. When I came home from the surgery, I actually had little lumps — it was these tiny expanders — so I wasn’t completely flat-chested.
There was just this little bump in there, and then gradually over time they’re filling it up with these cc’s, but it was very, very hard. I’m a belly-sleeper, so you can’t even began to lay on that side of you. They’re bricks. When you get your implants in, then they take the expander out, but it’s created space and tissue and allowed that construction then to come in.
Then it feels more a normal breast. I can now lay on my stomach again. I can have the movements to me. The expanders are truly to slowly stretch the skin over time.
How did you choose between implants or flap surgery?
They did talk to me about that, but the recovery time was so long [for flap surgery], and they felt they could do implants. I just didn’t want another surgery. I felt that was the most advantageous to get me back my normal life.
Radiation Therapy
Describe the radiation therapy cycle
It was 5 weeks, 5 times in a week, so Monday through Friday. I would go around my lunch hour every workday. They had a setup time frame. They tattooed you, they traced it all where they need it to go, [and they] made a mold specifically for your body. That happened prior to the 25 rounds of [the radiation].
From the time you were in there, it was very brief. Most times it maybe took 5 to 10 minutes. It wasn’t a very long procedure. It took just as long to basically get changed into your gown and get all positioned than the actual process itself, so it was fairly quick.
Were there radiation side effects?
- Sunburn feeling
- Pain
I know a lot of people would get tired or have side effects, and maybe because I was coming off chemo and still improving for me, it wasn’t super tiring. I was feeling actually probably better than I had been just because the chemo had really worn me down.
I remember I bought aloe plants, and in addition to the medication that they prescribed, I put aloe plants on my skin each night. I drank aloe juice, and I tried to just heal my body as much from the inside with aloe juice.
I didn’t have my skin break open or have major issues, but it is crazy. Even though you’re done after 25 rounds, there’s still a reaction happening to your skin. About 3 days after my radiation, it was just really, really painful.
It felt like a million little pencil pricks or something. It just was really painful. I would either take an Advil, or if I was at home, I’d actually have a shot of whisky. Then it was done, and it was fine, but it did look like you have a sunburn on you where the radiation was being targeted.
Then it was pain pretty much after. The last few days were maybe more intense, so that’s what’s weird. Even though you’re think you’re done, you’re not really done.
»MORE: Read other patient experiences with radiation therapy
Hormone Therapy
How did your oncologist introduce the hormone therapy?
Because my breast cancer was estrogen positive, I was going to do some hormone blocking thing. Some people don’t react to well to tamoxifen, so there’s different kinds, different estrogen-blocking methods. He wanted to come and try me on the tamoxifen first.
Then my oncologist had just gone on some summit or medical conference. He had come back and said, “Well, they just did this study on people under the age 35, and they’ve shown a 7% greater chance of survival rate when they’ve done the Zoladex trial.” At the point, I was 38. He said, “I know you’re over 35, but I think it’s worth it for you to try this. I think this will be in your best interest.”
The Zoladex shot, I think, was actually started for a different cancer, and then they just realized that it does have some benefits for estrogen-positive recipients.
I started doing that shot. At first we did it once a month, and then we found that there was a time release one that we could do every 3 months. I’ve been on that the last few years. That essentially put my ovaries to sleep. Between the 2, there’s not a lot of hormones in my body anymore. Basically, it just tries to shut down all the hormone activity.

At first they talked maybe it will be 5 years. Now it’s sounding like 10 years, and I’m even hearing rumors people may be on this for life. Side effects willing — so far, I’m pretty good with all the side effects.
I still have hot flashes. I definitely have some moody PMS issues when I first was on tamoxifen, but I don’t know if it’s because I’m in full-blown menopause now. But I feel fine. I feel just like my normal self.
How often do you take tamoxifen and Zoladex?
The tamoxifen is a pill that I take daily. The Zoladex is every 3 months. Usually my doctor visits just coincide with that, and they check me out. I don’t have to get mammograms anymore because I literally have no breast tissue to examine, so they usually do a really detailed self-examination and then do the Zoladex shot at that same appointment.
Does the hormone therapy have side effects?
I feel like it’s harder to lose weight, but I have now taken a more serious role with it.
I do think with estrogen blocking and all the different things, my body is like that of a 60-year-old. Muscle mass and all that becomes more important, and it’s harder to lose weight just normally.
I have proven that it can be done, but it takes a lot more effort and work. I think that’s normal with aging, too, but definitely with tamoxifen, I think that’s an added impact.
»MORE: Read more patient stories of hormone therapy
Describe the post-treatment scan & results
[6 days after the scan is] when I got the results, so not too bad. I had it done on a Saturday and got the results on a Tuesday. Waiting over the weekend is always tough.
I wrote this in my blog that day:
Dr. Singh called me back, and it’s just funny how you can tell so much from the first greeting. He told me my scan was clean and all was good! Today is a good day. God is Good!!!
I was elated and over the moon! All that heavy lifting of chemo upon chemo and radiation after radiation had done its job.
Hair Loss
Describe the hair loss
It’s just so personal. You have this image of who you are, and when you have to change that, it’s very difficult.
I would just keep walking by this wedding picture of myself that was 4 or 5 months prior, and it was really hard to see this long, blonde hair in this picture and this mental image of myself, then to look in the mirror and not see that.

I got it cut shorter in preparation for chemo. I think it was late September, early October. Then with my first chemo, I think it was by the second chemo, 2 weeks after, I was definitely losing my hair.
I went in actually the night before Halloween on my way home from work. I ended up stopping at a Sports Clip and just said, “Cut all that hair off.” I think they ended up charging me a senior rate. I think they felt really bad for me.
But it just felt so much more normal for me to do it at a hair salon of any kind, just to see it on their floor and on their sinks.
That felt like where it should be. If I had seen it in my own sink, I think I would’ve been really disturbed or just too upset about it.
I had a shaved head. I’d gone for a wig consultation and had 2 different wigs, but I really loved my shaved head. It still had hair, and it still had some substance to it.
I wore that shaved head for probably a month to 6 weeks. Then it started to get just really patchy, and it just wasn’t uniform anymore.
I switched to wearing my wigs. Plus it was winter, so it was okay to wear something scratchy and hot sometimes.
Even during Taxol, my hair actually started to grow back near the end. I started to get peach fuzz. Then definitely by late March to early April time frame, it was starting to grow back very, very short. Very pixie. It just started growing and kept growing.
I found that it just wasn’t the same as before. I used to color my hair and make it more blonde, and it wouldn’t take the color. It just had a mind of its own for probably a year or so. It did what it wanted to do.
What did you wear when you were bald?
At home I wore beanies and hats. When I went out in public, though, when I went to work, I would typically wear a wig. I was on medical leave from mid-to-late January until early April. I was at home actually quite a bit, so it didn’t really matter what I wore. I did wear more beanies just because it was more comfortable.
Any advice to others on managing the hair loss?
I would say to cut it shorter in advance. Maybe that doesn’t mean shaving it, but I will say that, again, seeing it at a hair salon cut short just feels still somehow more normal than seeing it at home.
I would say have a little bit of fun with it. I did a hairstyle I wouldn’t have normally done, but I had fun with it. I know other people who did mohawks. I know people who just did funky things or colored it hot pink or unicorn.
But I would just say have a little bit of fun. The one thing that you can control is how it’s going to go, so maybe have some fun with it before it goes.

Did you know about cold caps (to try and save hair)?
There are people that do the cold cap. That wasn’t an option for me, but I would definitely look into it and see what that option is. I hear a lot more survivors talking about that option now. Every year it’s different.
There’s more advances. If hair loss is something that really bothers you or you want to talk to your doctor, I would definitely talk to them about that.
»MORE: Dealing with hair loss during cancer treatment
Work & Finances
How did you balance work and life during treatment?
I felt in order for me to be me, I still wanted to work, and that worked for a little while. Having the support and love of all my coworkers was definitely amazing.
Then I just got to a point [where] I just felt like I just couldn’t [work]. I was just really sad, and I just didn’t know what to do. I felt foggy and really not sure.
I remember going to a support group, hoping that others would talk about work-life balance. But so many of them were in their 60s. They were already retired. I got a lot of love and support, but I didn’t get that “how do you balance it all” thing.
How was the financial aspect of treatment?
They talk about being your own advocate health-wise. If you get a bill, it doesn’t necessarily mean you owe everything on that bill. Sometimes you have to just follow up and make the calls. Sometimes you don’t have energy either, so you need help to get through it.
Sometimes hospitals offer different people to help you navigate through that. One of the things I remember thinking was, “Oh my gosh, if this were my grandma right now, she would have probably paid $10,000 more than she ever needed to because this isn’t really a bill.”
This is just telling you an explanation of something. Sometimes I really had to call and get to the bottom of what I really do owe, even fighting things because sometimes the insurance wouldn’t pick it up until you connected all the dots for everybody.
I had to be my own insurance advocate a lot of times, but I was actually very grateful for what I had to spend [out of pocket]. I was very lucky. Very blessed.
Support & Care
How did you manage the mental and emotional stress during treatment?
I think it was that January leading up to my medical leave, I was sick. I wasn’t feeling good. I felt like I had a cold. I was trying to work from home a couple days a week, yet I was getting called. “Why aren’t you on this call? Why aren’t you on that call?” It was just very overwhelming.
I would say normally I could have handled all that stress; that’s just who I was as a person. When you’re going through all the chemo and the cumulative effect of it, you might not be able to handle stress like you normally can.
It’s okay if it’s not okay. If you need to talk to your doctor, which I did, you should do that. I do [appreciate] his sage advice telling me, “You really need to consider taking a medical leave.” For me, it was the best decision I’ve ever made.
It was close to 3 months at home, and I could protect myself from germs. My doctor just told me to do something every day that makes you happy. I thought that those were really powerful words.
Sometimes I would just make pizza from scratch with yeast and the bread dough. One day I made a pie, or one day I did an art project. I did yoga every single day on a videotape at home called Gentle Yoga.
It was self-care. I just took care of myself. I really did have to prioritize myself and my mental being. I felt like I’m doing everything the doctors need me to do. I need to take care of myself.
It wasn’t being selfish. It was doing what I needed to do for my body and just listening to it and slowing down. I’ve worked a pretty stressful, crazy job, and it just put a lot into priority for me.
It’s hard to slow down for many. Any tips?
I did this Gentle Yoga tape, and I used to think yoga was stupid. I really did. I was just like I don’t get it. I’m an endorphin junkie. I want to run. I just want my immediate fix. Just give me that. Honestly, I went into it with a whole different mindset during my treatments.
They talk so much on this yoga tape about surrendering and having this balance. It’s not only the push; it’s also the pull and the surrender, and just how important that is. Just being a net and letting it flow through.
All these things really resonated with me during my treatment, and something as simple as the breath and just focusing on it. It’s almost magical.
It was really transformative for me to just take that time and to truly focus on each breath and on just slowing down. It was good. Sometimes you have to.
I’m not trying to say that my job or anything led me to getting my cancer, but I feel one of the silver linings was just coming out of it with a greater sense of boundaries and a greater sense of balance.
Were there big surprises during treatment?
I think probably because I had seen my mom go through it, I guess not so much. My mom gets sick. [If] she goes on a cruise ship, she gets sick. She goes on a car trip; she gets sick. I’m just not that. She goes on any boat; she gets sick.
I was like, “I just don’t have that motion sickness thing that you have.” I thought I would be fine, genetics aside. Then she literally would get sick at 4 o’clock after her treatments, and I would get sick at 4 o’clock after treatments.
I don’t know what was genetic or what was what, but despite me going into it thinking I wouldn’t be my mom, I was exactly my mom in terms of throwing up at 4 o’clock. It was just crazy. That was probably the biggest thing.
I had witnessed so much with my mom going through it. She went through chemo 2 times, once when she was 46 and then once when she was 49. She did the red devil the first time, and then the second time she did the Taxol. I at least had some familiarity with it.
Finding your community
I ended up turning to Instagram because I met so many amazing people who are also younger and trying to balance and do that. That was a great support network. But truly I just made a decision.
I remember waking up after my doctor told me about, “Who’s your advocate?” I just woke up one day, and I was like, “I can’t do this. I’m doing everything I possibly can: chemo, radiation, surgeries, all this stuff, but am I really taking care of myself?”
I couldn’t answer honestly that I was if I continued to work.
Thankfully, I was in a position where I could take a medical leave and still get paid. I understand not everybody’s in that financial position.
For me, it was the best thing for me to do at the time for my body to just take a break. It was actually a really amazing time, just a peaceful time.

Were there moments you had to self-advocate?
Yes. I think at the beginning, my oncologist really wanted me to get chemo at his facility. I remember going in there, and it was just really sad. I had a friend who was getting an infusion for a different treatment at a cancer center at the hospital.
I just wanted to go there. I just felt that everyone had their private area, so I felt my husband could come with me.
For me, it just seemed much more of a natural place to get chemo than in this office with people lined up in chairs. It really was heartbreaking.
I remember working with the nurse navigator, and she helped advocate for me, too, but we eventually got my doctor to understand that I just didn’t want to get it done here.
If you feel very passionate about something, you definitely have to find people on the same team as you. You can definitely push, push back, and try to seek alternative options that meet your needs better.
How important was it to have caregivers around?
My mom was such a support for me, obviously. I just remembered that my first oncology appointment was horrible. The waiting room was horrible.
I remember getting into my car and calling her, just crying and crying and crying. You need that person that can just allow you to be and let you cry and let you get your feelings out.
Obviously, my husband was an amazing support. He helped me to be more normal and to feel more me. We would go for walks together, and it felt like each walk, each step, was closer to the finish line.
That was really great. He was really supportive of all the work ups and downs and everything that happened with the work aspect.

Then it’s the sisterhood. Breast cancer’s just really an amazing sisterhood. Everybody wants to help everybody else. I met some amazing women that I’m still friends with, and I continue to meet more people.
That’s what inspired me to start my podcast, DJ Breast Cancer, just to help people through and be that girlfriend’s guide. Just to tell them how I felt and to feel like they’re not alone.
If you have a best friend going through breast cancer, you could listen to this podcast and then also feel, too, “I can maybe be a better friend, because this can maybe start a conversation or could maybe help me be a better friend.”
Any advice on how to ask for support?
I think support comes in a lot of different ways, and for a lot of people, it’s different. It can be as formal as a support group. It can be talking to your doctor.
Cancer is not a do-it-yourself sport. You need a team. You really, really do, and you have to find people that are going to help you on the journey.
It’s okay if you take a day, and you just need some time to yourself. At the same time, you have to rely on other people. You need people to take you to appointments.
You don’t ever want to go to your first consultation appointment on your own. Don’t do that. Then for rides for chemo, you often can’t drive yourself back home. You don’t know how you’re going to react to the medication.
You’re going to need a team of people. Sometimes they can be your best friends, and sometimes it can be people that you meet at your support group. I had an amazing person, Sandy Clausen, who came into my life, and she took me to so many of my appointments. She was just my angel. She just helped me through so many hard times.
Unfortunately, she got metastatic and I lost her, so it was really hard. She’s actually [whom] I dedicated my podcast to. She’s just the example of support and women helping women.
You don’t have to know people. You can just feel, you just help them through, and that’s just what you do. She’s just an amazing example of that.
Survivorship
What does “life after cancer” mean to you?
Just really embracing life. It looks a whole lot different than before cancer. I just really enjoy living my life. It’s really important to me now to live my life fully and with a purpose. It’s not enough to just show up.
No, I have to be present, I have to be engaged, and I have to believe in what I’m doing. Try to help people and make them more aware about breast cancer and that it’s not an easy cancer.
It’s been dubbed, “You have the good cancer.” Well, no, I don’t. There’s no good cancer, and I won’t rest until something’s been done about it.
It’s just finding beauty in the simple things. Taking a walk. It is making a meal from scratch. It’s telling people that you love them. It’s just a lot more simple on this side than it was before. That’s, to me, one of the beautiful gifts of the whole journey.
How has it been managing menopause at such a young age?
I remember thinking, “I want to have my period. I don’t want cancer to take that away from me.” I got one period, and I was like, “Oh no, you can have it back!’
Then it was funny because I went on the Tazocin and the Zoladex, and it went to my wishes. Actually, I don’t miss that part at all. I would just say it’s the hot flashes. There are some mornings, between the hairdryer, the hot coffee, whatever outfit I picked out for the day, I’m like, “Save me right now or send me an iceberg, one of the two.”
But I don’t really miss having my period. It does change your dynamics; my husband and I thought that maybe we could have a family.
He has a daughter from a prior marriage. It definitely changes when you know you can’t. It’s just this finality thing. Okay, well, this is my life now, so you just have to make the best of it.
I have 2 goddaughters, whom I love to death. One is 13, and one’s going to be 3. I’m just determined that one day they’ll live in a world where they don’t have to worry about breast cancer.
I try to fight for that day and be active in causes that research breast cancer and are trying to make a difference.

Now for a fun story: both happened at Chicago Cubs baseball games!
I was on a train, actually going back to Michigan at the end of my chemo, and the hospital called me and said, “Hey, we picked your name out of a hat, and you’re going to go to some Pink Out game at the Cubs.”
I was like, “Oh, cool.” All I cared about was can my husband come with me, because I just didn’t want to go by myself. They’re like, “Yeah, we’ll get back to you on the details.”
Then a month later, they called me. I was just back at work just after my exchange surgery, and they’re like, ‘Hey, would you like to throw out the first pitch?’ I was like, ‘Yeah, that’s not even a question!’
I’m from this crazy sports family, so yes, the answer was yes. It was amazing. Obviously, you get nervous at a lot of different things, but it was the craziest feeling.
I went to the mound, and I never felt nervous. I just felt like I’m a winner.
This is just an amazing end to such a journey, so it was really awesome. It wasn’t a strike, but the catcher caught the ball. 50 Cent had gone not far before I did and made a total idiot out of him, so I’m like, “Whatever I do, I’m going to be better than 50 Cent.”
And I was. I’ve got that going for me, and Wrigley [Field] is just so historic and so amazing.
Then the next year, they asked me to come back for the Pink game and do the seventh-inning stretch with 2 of my survivor friends, one of whom was my friend Sandy, and then my other friend Ronnie. That was a great experience.
Looking back at it now, I’m even more fond of it because despite all the hardships we went through, we had that one day that wasn’t about cancer. It was just about fun and the Cubs and just being there. It was amazing.

Any more advice for people dealing with a new diagnosis?
It’s definitely a roller coaster. There’s going to be ups, and there’s going to be downs. I think it’s just hold on tight, and you may never get back to a complete normalcy, but things will get better. I think that’s all I can stress.
In some ways, you’ll appreciate the journey. Looking at it on the other side is just totally different. It’s amazing, and you just appreciate more, but it’s not easy.
It’s okay to have a bad day, and it’s okay to be down. If you find yourself staying there, then you’ve got to talk to somebody. Is it your doctor, is it your nurse, or is it a counselor? You have to talk to somebody if you find yourself just staying in a down place. You need to.

Inspired by Tina's story?
Share your story, too!
Combination Type Breast Cancer Stories
Symptom: Sunken in nipple of right breast
Treatments: Double mastectomy, chemotherapy (AC-T), radiation, hormone therapy (tamoxifen, Zoladex)
Symptom: Lump in right breast
Treatments: Lumpectomy, double subcutaneous mastectomy, hormone therapy (tamoxifen)
Margaret A., IDC & DCIS, Stage 2B
Symptoms: Pain in left breast, left nipple inverting
Treatments: Double mastectomy, chemotherapy (AC-T), radiation
LaShae R., IDC & DCIS, Stage 2B, ER+
Symptoms: Lump in breast, pain
Treatments: Chemotherapy (Taxotere and cyclophosphamide), proton radiation
Dee D., Metastatic Breast Cancer, IDC & DCIS, ER+
Symptoms: Inability to produce milk on the left breast while breastfeeding, breast pain (palpable and radiating to the back), lumps in the breast and armpit
Treatments: Chemotherapy (AC-T), surgery (bilateral mastectomy & axillary lymph node clearance), radiotherapy, hormone therapy (Zoladex/goserelin), aromatase inhibitor (letrozole), targeted therapy (Kisqali/ribociclib)
Cat L., IDC & DCIS, Stage 2B, ER+
Symptom: Pain in left breast radiating from lump
Treatments: Bilateral mastectomy, chemotherapy, hormone therapy (tamoxifen)




