Cat’s Stage 2B IDC & DCIS, ER+ Breast Cancer Story
Cat shares her story of stage 2B breast cancer, getting diagnosed after feeling a lump in her left breast. She details how she got through a bilateral mastectomy, chemotherapy, hormone therapy, and recovery.
Cat also highlights how she managed hair loss, what support was most helpful to her, and how she dealt with parenting while going through cancer.

- Name: Cat L.
- Diagnosis (DX):
- Breast cancer
- Invasive ductal carcinoma & ductal carcinoma in situ
- ER+, PR/HER2- in left breast
- Age at DX: 33
- Staging: 2B
- 1st Symptoms:
- Lump in left breast (actually turned out to be 2 that were close together)
- Treatment:
- Surgery
- Bilateral mastectomy with expanders placed
- Exchange surgery
- Fat transfer surgery
- Chemotherapy
- 4 rounds
- Hormone therapy
- Surgery
The biggest thing you can do for me in this process is don’t ‘at least’ me. That means no, ‘Okay. At least you’re stage 2 and not 4. At least you’re alive. At least…’
That drives disconnection.
You don’t have to have magic words. You don’t have to try to fix it. You can’t. You can just say, ‘Dang, that’s really hard.’
Cat L.

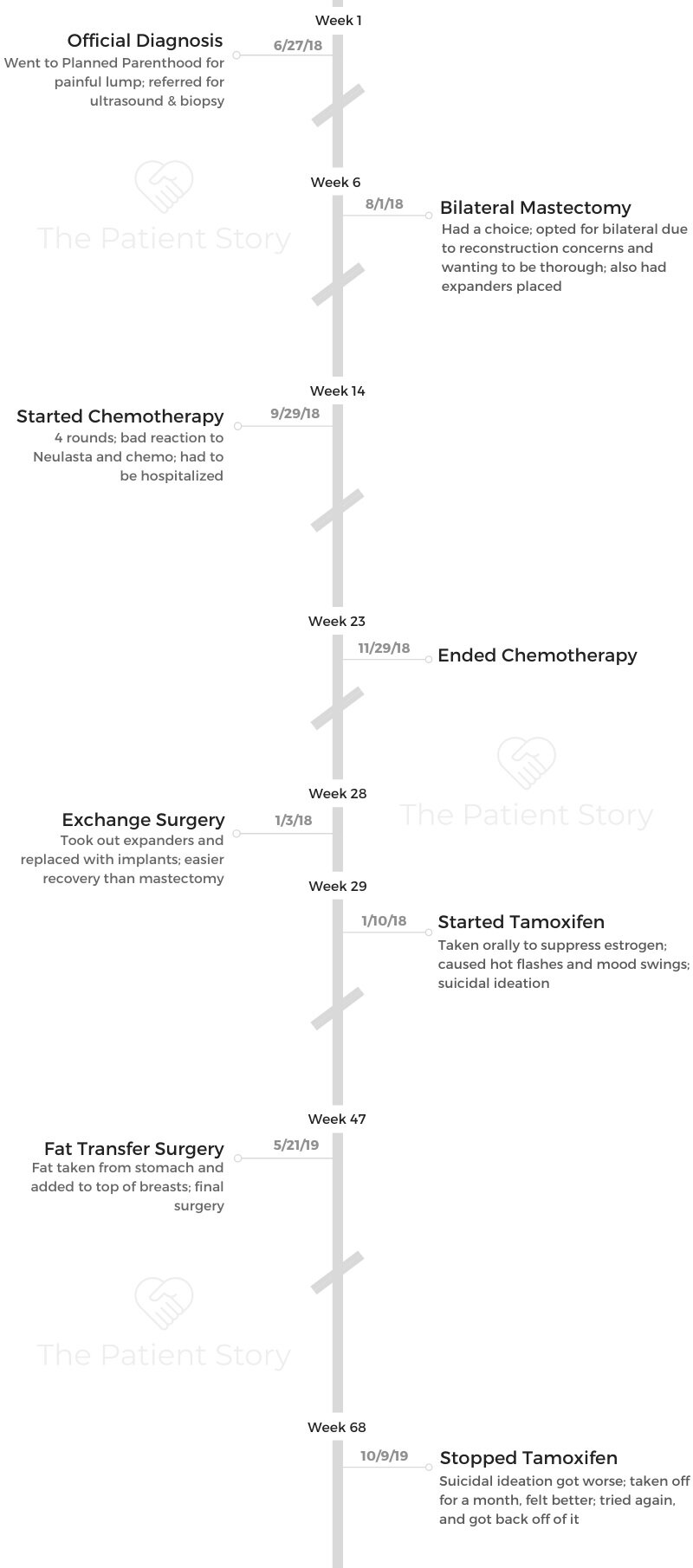
- Diagnosis
- Mastectomy
- Chemotherapy
- More Treatment
- Support & Emotions
- Can you talk about your support system?
- Do you have advice for people who want to help but don’t know how?
- How has cancer affected your relationship with your fiancé?
- What’s it like being a parent with cancer?
- What’s your “new normal"?
- How do you manage the fear of recurrence?
- What advice do you have for someone who has just been diagnosed?
This interview has been edited for clarity. This is not medical advice. Please consult with your healthcare provider for treatment decisions.
Diagnosis
What were your first symptoms?
I started to get a bunch of pain in my left breast. I had pretty fibrous breasts before all this. I would find little lumps here and there, but this one was huge. It was about 7 or 8 cm. I was getting pain radiating from the center of it. When I felt it, there was clearly a lump.
My boyfriend at the time felt it as well and told me I should go get checked out.
How did you get diagnosed?
At first, I went to Planned Parenthood, and she referred me to an ultrasound place. I went there, and the guy there said, ‘I can’t diagnose you with cancer, but it really doesn’t look great.’
He took me back and showed me what it looked like. He sent me to a biopsy place, where they did a biopsy on the left breast in my lump and on the right breast as well, because I had little calcifications in my right side.
How did you process the news of cancer?
I don’t remember the moment I was diagnosed, but I remember the moment after the ultrasound. I knew then that I had cancer.
He didn’t diagnose me obviously, but he said, “This is what cancer looks like.” I got out of that ultrasound and just started crying. I was a mess the whole way home.
»MORE: Patients share how they processed a cancer diagnosis

Describe the biopsy
That was not something I was prepared for. I thought they were just going to numb me real quick, go in with a tiny needle, and be done.
I had brought my 40-pound bag of school books and stuff because I was in school and was going to study while I waited. They told me I wouldn’t be able to carry that to my car. I also had to go pick up my kid later, and they told me I wouldn’t be able to lift her.
I went back, and they put needles in my left and right breast to try to numb them. They have this big needle that’s hollow. It pulls out a piece of the biopsy.
The first pass was okay, but by the second one, I wasn’t numb anymore. I felt the second one, and I was in a lot of pain. They quickly stopped and gave me more numbing medicine.
Then they took me back, and I had to lay on my left breast, which was in a lot of pain. I had to lay flat on this machine while they dangled my right breast down.
You’re on this machine, and your breast is in this little hollow cavity in the machine. They went in with a needle from the side after they had numbed it again. After that, I had to get up and do a mammogram.
They had someone behind me, and I fainted during the left one because it hurt so bad. They lifted my bag to my car for me. People had offered to come with me, but I was like, “No, I’ll be fine.” I didn’t know it was going to be that big of a deal.
Mastectomy
How was the meeting with the surgeon?
I met with my breast surgeon and plastic surgeon. I hadn’t met with my oncologist yet because I didn’t need radiation or chemo before surgery.
I got diagnosed at the end of June, and I went on a trip for 2 weeks in July to see my family. They said it would be fine if we waited. I didn’t want to schedule my surgery until I was done with my summer semester in school, so we waited until August for that.

What made you decide to do a bilateral mastectomy?
I had a choice. I could keep my right breast and nipple, but I couldn’t keep either on my left side. The whole thing had to go.
I decided to get the full mastectomy because I had breastfed before, and it was going to be impossible to recreate the shape of my right breast with an implant because it was much lower and not round. I was worried about it because of the calcifications, too, so I got the full bilateral surgery on August 1, 2018.
What was the preparation for the mastectomy?
The preparation was having to go buy Hibiclens. It’s a special soap you use all over your body, especially on your chest, for the whole week before.
The prep for the surgery was really just a lot of mental prep, though. My boyfriend and I went on an 8-mile hike the week before.
We took really pretty pictures and just did life. I thought then that I was just going to get a bilateral mastectomy and be done. I thought I’d get a free boob job and be done with it.
The day of the surgery, my stepmom flew out. She got me special t-shirts, and we went to the hospital. My stepmom, my ex-boyfriend, and my boyfriend all went back with me, which was super awkward, too. My stepmom and boyfriend ended up staying in the room with me.
The anesthesiologist came in, and I decided to get a pain block. It’s kind of like an epidural for your upper body. I got that done right before surgery, and it was painful, so of course I passed out.
How did the surgery go?
Surgery was very successful. They got all of my breast tissue. They took some lymph nodes from my left side, too, so they could biopsy those.
They found out I actually had 2 separate tumors. The invasive ductal carcinoma was 5 cm, and the in situ was 3 cm. I was a combination type. I didn’t find that out until after the surgery.
I also had expanders put in during the surgery, and once a week, my surgeon would fill them with fluid. They weren’t painful, but they were uncomfortable.
How was the recovery in the hospital?
The hospital recovery was really rough. Again, I don’t handle pain really well. I had one of those plastic beds that’s supposed to make sure you don’t get bed sores, but I was only in the hospital for one night. I kept slipping down the bed, and you can’t use your chest muscles after surgery.
They kept telling me to use my stomach muscles, but it kept spreading up to my chest, so I couldn’t sit up on my own. My stepmom stayed on the couch in the hospital room with me and put her arms behind my back so that I could just sit up.
I fell asleep at 8 p.m., and they didn’t wake me up to give me painkillers. When I woke up in the morning, I was screaming because it hurt so bad. I didn’t feel like the nurses did a great job. I don’t remember much else other than that.
How was recovery at home?
Recovery at home was rough, too. I had drainage tubes on each side. My left side tubs were more painful than even the stitches I had across my chest. I had about a week or so recovery at home. My stepmom took care of me.
We would call my plastic surgeon because I was just in so much pain. He would ask us to send pictures, and he said it looked normal. I ended up back in the hospital because I was in so much pain.
I recently found out that my stitches, which are supposed to create a hammock for your breast, just didn’t heal properly. Recovery for me took about 2 or 3 weeks in total. It was a slow process.
Chemotherapy
How did you find out you needed chemo?
We got my oncotype back for my tumor, and the oncologist said I had a 16% chance of getting an incurable type of cancer, which seems kind of low, but the general population has a 2 or 3% chance.
She gave me some options. I opted to do chemo for 4 months. I don’t remember which drugs I got because I was out of it at that point and was scared and sad. I didn’t know I was going to need chemo. That was hard. My boyfriend and I both cried.
What were the chemo infusions like?
I wore my chemo crown, which was a woven, golden crown, and my chemo shirts to each infusion. The first time I went, I had all my hair, and I felt fine that whole day. Then I went home, and they had given me a pack of Neulasta. It increases your white blood cell counts.
After that is when I started to go downhill. I got really really sick. I was throwing up, I was dehydrated, and the bone pain was so bad. I gave birth naturally by choice, and it was worse than that.
It felt like my hips were expanding and my bones were breaking. That week, we were in and out of the hospital maybe 10 times.
For the chemo infusions after that, they halved my dose of Neulasta. The infusions themselves were always really pleasant. It was open, and there were other people you could talk to.
Volunteers walked around with snacks. It was hard, though, because I was always the youngest one there. There was never anybody my age.
Even with the reduced dosage of Neulasta and switching to the infusion, I still had a horrible reaction. It wasn’t as bad as it had been, but I still had to be in the hospital.
Describe the hair loss
After that, my hair started to just come out in clumps. My boyfriend was out of town that week. My ex-husband came over, and we shaved my head as a family that night with my kid.
We shaved it into a mullet first and stuff like that. We went out to dinner, and then I went home. My boyfriend came home and brought me a wig. He would wear it during my chemo treatments and make people laugh.
Describe experiencing the hair loss
Hair loss wasn’t emotional for me at first. It was just another thing I knew was coming and that I had to do. The thing that gave me anxiety was seeing clumps just come out. Being able to grab my hair and just have it come out was so strange.
After a while, it started to wear on me because people could tell I was sick. I was really tired of people being able to tell I was sick.
The loss of my eyebrows and eyelashes was incredibly rough. I didn’t have to shave my legs, though, so that was nice!
»MORE: Dealing with hair loss during cancer treatment
More Treatment
You had the exchange surgery next
The exchange surgery went really well. I didn’t have to have drainage tubes. It was so much easier than getting my breast tissue removed.
The expanders would turn and move, and they were so uncomfortable. The surgery corrected that, and I finally had implants.
I still struggled to do stuff, and it was frustrating. I got really depressed during that time because at that point, I just wanted to get back to my life. It went really well, but emotionally, it was tough.
You started tamoxifen
Tamoxifen suppresses your estrogen, and it’s just a pill you take. My tumor was ER+, so I started that after the exchange surgery. I didn’t need radiation, so that was good, but tamoxifen was very rough.
I went into menopause. I had bad hot flashes and crazy mood swings. I didn’t really notice it a whole lot because I had my exchange surgery around that time, too.
I was on tamoxifen for about 11 months. I started to get really bad suicidal ideation. I couldn’t get out of bed, shower, or do anything. I went off of it for a month, and I felt so much better.
They put me back on it, and I was having the same problems. I went to the hospital and told them, “I’m not going to do anything, but this is happening.”
They took me off of it immediately, and currently I’m not on anything. I feel more like myself.

You have post-mastectomy chronic pain syndrome
In May of 2019, I had a fat transfer surgery. That was my last surgery. They took fat from my stomach and put it up top to just kind of shape things out. I couldn’t get it done during the exchange surgery because I lost too much blood, so they waited until May.
After that surgery, right where my left drain had been, I started to get extreme spiderweb pain across that portion of my body. I ended up in the hospital again. I’ve been to the hospital for that about 5 times. I had a doctor basically tell me I was a pain pill addict at one point.
I went and saw my plastic surgeon in November of 2019, and he said I have post-mastectomy chronic pain syndrome. I’ve done acupuncture, chiropractic care, yoga, massage, and it’s just still not getting better.
I went and saw my oncologist, and she referred me to a different plastic surgeon. She started me on an ibuprofen regimen, and I’m supposed to get PT/OT soon because I’m getting frozen shoulder syndrome from it now.
I have a consultation for a stellate ganglion block soon. It’s basically like an epidural for your neck and shoulders. I’ll get that done hopefully soon. It’s still a relatively new procedure, but I hope it’ll work for me.
Support & Emotions
Can you talk about your support system?
My biggest supporter was my boyfriend, who is now my fiancé. We met at a brewery a few months before I got diagnosed.
Our dogs got tangled up, and we started talking. He, without knowing me super well, took care of me. I stayed at his house. He flew my family out, cooked, cleaned, and supported me all while working a full-time job and traveling for work.
My ex-husband was a very good support as well. He took my daughter for a good 80-90% of the time during my chemo because I couldn’t care for her myself.
My stepmom and dad both traded places coming out for that entire period of time. My best friend came out for a whole week and took care of me, too.
Without them, I would’ve been in an assisted living facility because I just could not take care of myself. I couldn’t do it alone. They were invaluable to me. Emotionally, I don’t know what would’ve happened to me without them.
I’m also part of a group called The Breasties. I’m an ambassador for them now, and they were a great support, too. It’s been so important to have that. Because I’m so young, it’s very difficult to find people my age who understand chronic disease.
The women truly understand what I’m going through, and that’s amazing.

Do you have advice for people who want to help but don’t know how?
The biggest thing for me was “at leasting.” I got it from Brené Brown. She has this video on empathy vs. sympathy. I made all my caregivers watch this video.
I said, “The biggest thing you can do for me in this process is don’t ‘at least’ me. That means no, ‘Okay. At least you’re stage 2 and not 4. At least you’re alive. At least…’” That drives disconnection.
You don’t have to have magic words. You don’t have to try to fix it. You can’t. You can just say, ‘Dang, that’s really hard.’
Connect with yourself and how you feel when you’re at your worst, and understand that that’s how the patient is feeling.
Sometimes somebody just needs you to validate their feelings and for you to just cry with them.
How has cancer affected your relationship with your fiancé?
We already communicated really well. We work really well together. We talk about everything. It was very difficult, though. We had known each other for 2 months, so he went from an equal partner to a caregiver.
It wasn’t sexy. He stuck with it, though, and loved me so much. I still gave him love in ways I could.
After we were done with chemo, which was the hardest part, we said, ‘We need to connect.’
We traveled. We went to Washington, Little Rock, and we went to see both our families. We went camping, hiking, biking, and to New York. We just got back from Costa Rica. Travel has been a great way for us to connect and get to know each other.
»MORE: What kind of support cancer patients say helped the most
What’s it like being a parent with cancer?
It’s incredibly difficult. When I was diagnosed, I thought about what letters I would write to her if I wasn’t here. I wanted to write her a letter for the day she went to college, got married, or had a baby. I wrote all those in my head.
Once you’re done with it, you think you’ll be done, but you’re never done. For her, she knows what chemotherapy was. She was allowed to wash her hands, touch my breasts, and see them the whole time.
I didn’t hide it from her because I didn’t want it to be mysterious. She does get confused, and she sometimes thinks that everyone has to get chemo when they get older.
My ex-husband would bring her over and let her sleep over, and he would sleep on the couch and take care of us. It was really sweet.
»MORE: Parents describe how they handled cancer with their kids
What’s your “new normal”?
I want life to hurry up. It’s very much rushed in my head. Before my boyfriend proposed, I was very upset that he hadn’t. It just feels like there’s not much time left.
My new normal is being so happy that I’m cancer-free right now (as far as I know), but I’m also always on the lookout and preparing myself for the day when they say it’s back.
It’s both amazing and awful at the same time. It’s amazing that the first time I was able to run in the woods after all this, it felt like the first time I’d ever run before. That part is incredible. I’m able to see the world through new eyes. Everything is more beautiful and heightened. It’s also stressful, though, because you never know if it’s going to come back again.

How do you manage the fear of recurrence?
I exercise a lot. I do HIIT classes, boot camp classes, barre, and I mountain bike. I go to therapy once a week as well.
I talk with my fiancé about it when I’m feeling upset. I call him and my family and talk. I meditate every morning and night. If I need a day to just not do anything, I just take it.
What advice do you have for someone who has just been diagnosed?
Ride the waves. Ride the emotional waves and talk. Talk to anyone and everyone you can about it, because you need to get those feelings out. You can’t bottle them up.

Inspired by Cat's story?
Share your story, too!
Combination Type Breast Cancer Stories
Symptom: Sunken in nipple of right breast
Treatments: Double mastectomy, chemotherapy (AC-T), radiation, hormone therapy (tamoxifen, Zoladex)
Symptom: Lump in right breast
Treatments: Lumpectomy, double subcutaneous mastectomy, hormone therapy (tamoxifen)
Margaret A., IDC & DCIS, Stage 2B
Symptoms: Pain in left breast, left nipple inverting
Treatments: Double mastectomy, chemotherapy (AC-T), radiation
LaShae R., IDC & DCIS, Stage 2B, ER+
Symptoms: Lump in breast, pain
Treatments: Chemotherapy (Taxotere and cyclophosphamide), proton radiation
Dee D., Metastatic Breast Cancer, IDC & DCIS, ER+
Symptoms: Inability to produce milk on the left breast while breastfeeding, breast pain (palpable and radiating to the back), lumps in the breast and armpit
Treatments: Chemotherapy (AC-T), surgery (bilateral mastectomy & axillary lymph node clearance), radiotherapy, hormone therapy (Zoladex/goserelin), aromatase inhibitor (letrozole), targeted therapy (Kisqali/ribociclib)
Cat L., IDC & DCIS, Stage 2B, ER+
Symptom: Pain in left breast radiating from lump
Treatments: Bilateral mastectomy, chemotherapy, hormone therapy (tamoxifen)




