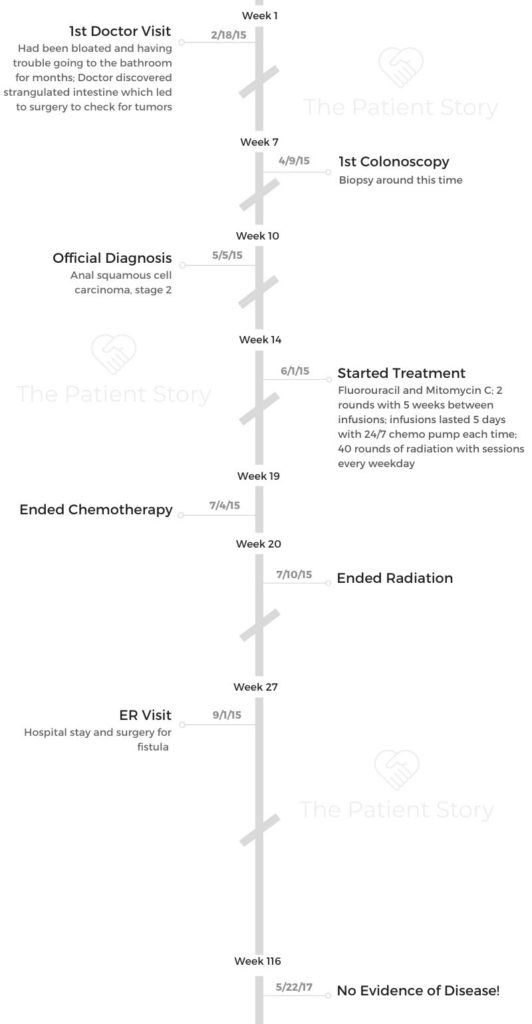
Daniel’s Stage 2 Squamous Cell Carcinoma Anal Cancer Story
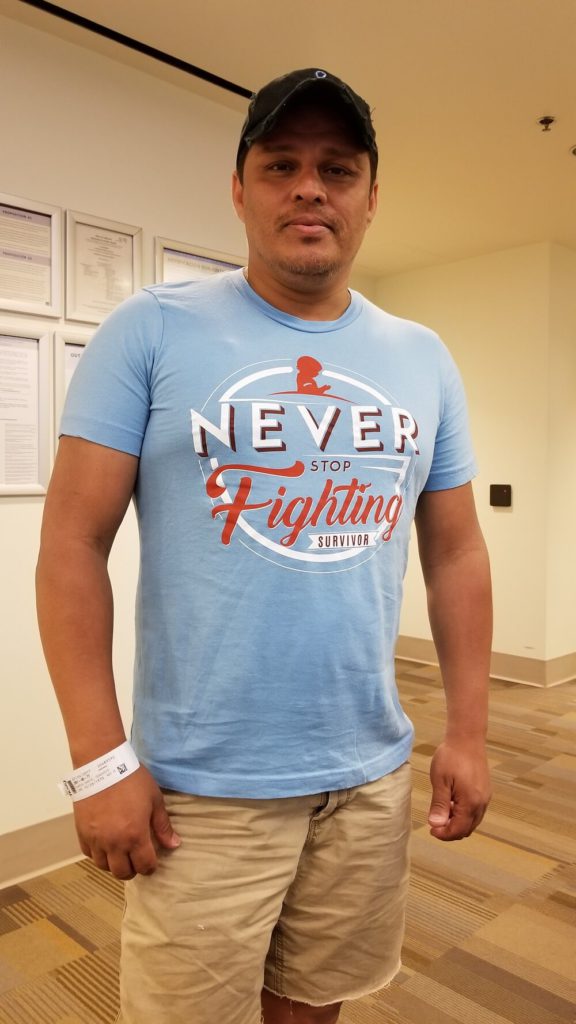
Daniel shares his stage 2 anal cancer story, a squamous cell carcinoma subtype, the most common (about 90% of cases). He describes how he got through treatment, from chemotherapy to radiation.
In his story, Daniel, now a healthcare advocate, highlights how he was able to get through the hair loss, the important of patient self-advocacy, and how the cancer diagnosis impacted his relationship.

- Name: Daniel Garza
- Diagnosis:
- Anal cancer
- Squamous cell carcinoma
- Staging: 2
- 1st Symptoms:
- Bloating
- Trouble going to the bathroom
- Treatment:
- Chemotherapy
- 2 rounds of fluorouracil and mitomycin C
- Continuous infusions for 5 days with 5 weeks in between each round
- 2 rounds of fluorouracil and mitomycin C
- Radiation
- 40 treatments
- Hyperbaric chamber
- 40 treatments
- Chemotherapy
Whatever you’re feeling right now is valid. Don’t apologize. Don’t change. If you’re scared, sad, or angry, feel it. Get through it, and then take charge.
Journal. Video blog. Record. Whatever you can do to keep up with your emotions. This might be the toughest thing you ever go through.
One day you’re going to want to go back and remember how strong you are.
Daniel Garza
- Diagnosis
- Chemotherapy & Radiation
- Reflections
- Were you prepared for treatment?
- Do you have any advice for someone about to go through treatment?
- Can you talk about the hair loss?
- How did you get through the lowest points?
- Can you share your advice about self-advocacy?
- How did the experience affect your relationship?
- What is your “new normal”?
- What do you want to say to someone who has just been diagnosed?
This interview has been edited for clarity. This is not medical advice. Please consult with your healthcare provider for treatment decisions.
Diagnosis
How did you know something was wrong?
It was summertime, and I worked promotional jobs. I was outside, running around a lot.
I started getting really tired all the time. I thought I was just working too hard. I used to not drink a lot of water either, so I attributed it to that as well.
As the year progressed, I realized I was having trouble going to the bathroom. I had started a new HIV medication, and it can cause diarrhea and constipation, so I thought that was all it was.

I was running around all day working and not eating well, so I decided to go on a diet. I started eating more fiber and fruits and things like that. I could tell in some pictures I took on a trip that I looked really bloated. I still thought it was the meds.
When did you first go to the doctor?
Early the next year, I was feeling sick all the time. I wasn’t able to eat because I felt bloated, and I was popping Tums like they were candy. I was basically on a liquid diet for 2 months.
I went to my doctor for my regular checkup. I weighed 180 pounds, and I hadn’t weighed that in a long time.
I have this reputation for loving tacos, and he was like, “Stop eating so many tacos!” He’s been my doctor for a long time, so he got onto me. I said, “I’m not. I’m on a soup and liquid diet!”
We get to the end of the appointment, and I asked him, “Did I ever tell you about my hernia?” He didn’t know about it, so he said he wanted to check it out. At this point, it was really big. He said I had a strangulated intestine.
He immediately set up surgery. Six weeks passed. It was supposed to get better, but I still wasn’t going to the bathroom. They gave me pain pills, and those were supposed to cause constipation, but I never took them.
When I went back to the surgeon, he checked and felt a mass. He sent me back to my primary, and he felt the mass, too.
He immediately called the doctor who is now my colorectal doctor and set up an appointment for me a few days later. I freaked out a little at that point because all these appointments were happening so fast.
When did you get the diagnosis?
I went in to get the biopsy done, and I was supposed to get my results in a few days. That was a surgical biopsy, and I don’t remember that. I just had to do a cleanse before. I was just feeling miserable at that point.
My stomach was bloated, I was in pain, and I didn’t want to go anywhere or eat anything. I called the colorectal doctor and asked when we would know my results.
He said, “If you can get here within the hour, I can see you. I have surgery after that.” This was a Tuesday, and I wasn’t supposed to get my results until Friday.
I knew when he was urgent about us getting there that something was up. He said there was concern for different areas: anal, colon, and rectal.
He told me my problem was at the front, near the sphincter, and that was why I was having trouble going to the bathroom.
How did you react to the diagnosis?
I’ve been doing HIV education for nearly 20 years. In all that time, I’ve never associated HIV with cancer. After the first colonoscopy, I started doing research on HIV and cancer.
Any presentations I’ve ever been to haven’t really mentioned cancer as being associated with HIV other than sarcomas, so I looked it up.
There are almost 30 different types of cancer that have a 25% greater chance of affecting HIV-positive people.
I had no idea. Among them, colorectal cancers are listed. Immediately after reading that, I think I knew I had cancer. I walked into the appointment with the hope that it was something else, but I thought it was cancer.
When the doctor told me, my first thought was my partner, Christian. We had been together for 3 years at that point. I thought, “I have to break up with him. He doesn’t need to go through this.” I just didn’t want him to have to deal with it.
Immediately after that, I thought, “How am I going to do this by myself? My family is all in Texas. What am I going to do?”
Then I thought, “Crap. I can’t go back to work!” I’m a workaholic, and part of my identity is all the work I do.
It never crossed my mind that I might die. The doctor would’ve said that. He would’ve at least brought the topic up if it were a possibility. He wouldn’t have said, “We got this.”
Not to mention, he’s adorable. No one that attractive would tell me I was dying. In my rom-com life, only an ugly doctor would tell me I was dying.
»MORE: Patients share how they processed a cancer diagnosis
What was your doctor’s general treatment plan?
I asked the doctor what he suggested. He wanted to do radiation and chemo. I’m pretty tough. It’s really hard to break me down, but at a certain point, it got really serious, and I started crying.
One of the coolest things any doctor has ever done was he got up from his chair, came over to me, put his hand on my shoulder, and said, ‘Look at me. We’ve got this.’
That was the first time a doctor said “we.” It was like we were in it together, so I said, “Okay. I trust you. Whatever you think is good with me.”
How did your partner react to the diagnosis?
On the way home from the appointment, we stopped to eat. When we were in the car on the way home, I looked at Christian, and I said, “This is the moment. This is your chance. If you want an out, I’m giving it to you right now. We can tell people I broke up with you or whatever you want, no judgement. It’s cool, but if you decide to stay, I need you to really stay.”
He said, ‘No, no, no, I’m in this. Don’t worry.’
Chemotherapy & Radiation
What was your chemo regimen?
I started chemo and radiation at the end of that month. One thing that went wrong for me was that my chemo doctor and my radiation doctor were not communicating correctly. They did my chemo and radiation concurrently. It was a lot for my body to handle, and I got pretty sick.
For chemo, I went in on a Monday, they hooked me up to a pump, and it pumped until Friday when they took it out. That was one week. Then at the end of 5 weeks, I did it one more time.
Basically, I did 2 rounds, 5 weeks apart, with the infusions lasting continuously for 5 days each time. I had to go back for nausea shots every morning during infusions.
Describe the radiation therapy
Right after chemo, I’d go in for radiation across the street. That lasted all of 15 minutes, and then I’d go home. Radiation was 40 rounds.
I got treatments every weekday. It was very automated and quick. I checked in with my card, and it sent them a notification that I was there. I changed clothes, went back, and it was over.
If I got there early or if they were running a little behind, you would run into another gentleman. It was interesting to see other people progress.
I took a photo every day for radiation, and you can see me go from a full head of hair to losing hair to bald. It’s neat to see now, but it was hard back then.
What side effects did you experience from treatment?
I lost my hair. I lost weight. From my initial 180lbs, I went down to 123. I was in a wheelchair for about a week because I was just too weak. That was the worst for me.
I became very sensitive to smells, even smells I love. I’m a citrus person. I love lemons and limes. Things like citrus, garlic, and other strong smells were intolerable. I couldn’t stand the smell of bleach. I had some restrictions about people coming to my house. I didn’t want anyone to wear perfume.

We found some really cool ways around the fatigue and nausea. I had a recliner couch and 10 pillows around me. I rested there a lot, and I was very comfortable. With smells, we were just really careful. People were great about accommodating me that way.
For my nausea, we got the wristbands that press on your pressure points. I wore those constantly the 3 months of treatments. A couple of months ago, I was cleaning out my apartment and found them. I started crying and threw them out.
After chemo and radiation, you had to deal with fistulas
My treatment ended on the 4th of July. I had some issues. I had 2 fistulas that appeared. I wasn’t completely out of the woods yet because of that. I did 40 rounds of hyperbaric chamber treatment.
The treatments were pretty cool. The chambers they had were the same ones that Michael Jackson had in his house. I was like, “Am I going to sing and dance when I come out of here?” I give it credit in the sense that it helped my body heal faster. It helped my skin and my hair.
You go in, and they pressurize the air for like 45 minutes. It wears you out. It’s tiring, but it was a great place to go in and sleep. It wasn’t stressful. If you get the opportunity to get one treatment at least, I recommend it. With the 40 rounds, the intention was to heal the wounds.
One of my fistulas was right in an artery. The artery dried out and broke. I bled out and almost died. We were lucky that I was 2 blocks from the hospital when it happened. I wouldn’t have made it if we hadn’t been so close.
I had a surgery on the fistula. They didn’t put me under. I was just numbed from my waist down. It was really cool. I was just talking to the nurse while I was in surgery.
When did you find out you were in remission?
In the middle of 2017, my doctor said I was 2 years out of treatment, so I could officially say I was in remission.
Over the years of having friends with AIDS, cancer, and other things, we’ve lost some people.
That’s all the more reason for me to not take my experience lightly. I’m grateful to have made it here and to be able to do the things I can do today.
Reflections
Were you prepared for treatment?
Absolutely not. Not at all. We were given a lot of sugar-coated information from the doctors at some points.
My colorectal doctor was really good about telling me things were going to be rough, but at the treatment center, they mostly gave me best-case-scenario information. I like to know everything so I know how to prepare.
Cancer patients usually try to put the best face forward for their families.
When I told people I had cancer, they were like, ‘Oh, my aunt Betty had cancer, but she was happy all the time!’
Bullshit. That is not possible.
She might have been positive, but there’s no way you can go through chemo and radiation and be happy all the time. It’s miserable.
I started asking people to please be honest about how they felt during treatment. Finally, I found people who were honest about it. That was so helpful.
Some people would say, “I felt awful! I had diarrhea,” or whatever, and I was able to say, “Thank God it’s not just me.”
Some guy friends going through something similar and I were able to talk about loss of sensation or sexual discomfort.
I was like, “Finally! People who are honest.” I didn’t want the false statement that they were cheery all the time. Don’t put that expectation on me, because I’m not.
That’s when my video blogs were so helpful. I would record one day and everything would be fine, and the next day I would be a wreck.
Having said all that, I don’t think all the information in the world could’ve prepared me. Even if I had seen my own videos beforehand, I still don’t think I would be prepared.
Everybody’s body is different. Your support system says a lot. Your view on life says a lot. I’m very optimistic about the universe and God. I felt confident that God would not give me more than I could handle.
Do you have any advice for someone about to go through treatment?
The one thing we should’ve done right at the beginning was to have a wish list. A lot of people are going to ask you, “What do you need? What do you want? Can I get you anything?”
You don’t always want to ask or have the energy to ask. Eventually, I made a wish list on Amazon of everything we needed or wanted during treatment and would send the link to those who asked.
Some friends set up a GoFundMe for extra expenses. That really helped. It took a lot of stress off of me to know there was a little bit of cash for emergencies. It helped me focus on getting better.
People don’t think about that as far as treatment, but if you’re not stressing about money, it really improves the quality of your treatment. Stress can take a toll on you.
I also set up some ground rules about what would make me feel better and what people were allowed to say to me. I would advise you to come up with your own boundaries.
I got tired of people telling me they were sorry. I was like, “Why are you sorry? I’m getting treatment. I’m getting better.” No one gave me cancer. Stop being sorry if you didn’t cause it.
I didn’t want people asking me how I was feeling. I was going through chemo and radiation, so how do you think I was feeling? People were allowed to ask how treatment was going or what the doctor was saying, but not asking about how I was physically feeling because the answer was always going to be, “Like crap.”
»MORE: What kind of support cancer patients say helped the most
I also set some boundaries as far as visitation. I set visiting hours that would work for me. I also mentioned my sensitivity to smells to people who visited. It was so helpful.
Also, don’t worry so much about other people’s feelings while you’re going through treatment. You can apologize in advance to your family and friends if you need to. I knew I was probably going to come off like a jerk at one point or another, and I apologized to them up front for it. It takes a lot of stress off of you.
If someone can’t understand that you’ve got chemicals pumping through your brain and your body, then that’s on them and not you. You don’t need to feel like you need to apologize every 5 seconds if you’re upset, irritated, or distant.
Can you talk about the hair loss?
I’ve always had a lot of hair. You probably couldn’t tell, but I could tell when it started coming out.
The first time I really noticed handfuls starting to fall out, I cried by myself. I didn’t tell anybody.
»MORE: Patients describe dealing with hair loss during cancer treatment
The next day, I got out of bed, and Christian goes, “Babe, you’re losing your hair.” I just lost it. I ugly cried.
I have a hair stylist I love. She’s been doing my hair for 10 years. I’ve followed her everywhere. I called her up and told her I needed her to shave it.
She lives like an hour and a half away from me, but she came down and shaved it for me.
She said, ‘It’s okay. It’s going to grow back.’ She was right. It’s grown back thicker, lighter brown, and curly.

How did you get through the lowest points?
The hardest part was being in that wheelchair. Having to get to the hospital and wait for a wheelchair was so awful. I didn’t want that to be my life. Not that I don’t think I would’ve adjusted to being in a wheelchair, but that was a confinement for me.
Seeing Christian feeling so helpless was really hard as well. I knew he felt like he couldn’t do anything except be there for me. I knew he was stressed.
We have some really good friends, and I would ask them to come over and take him out for a burger or something. I had to get him out of the house to decompress a little because I knew he was stressed, too.
That also gave me time to cry and be sad. I needed to be able to enjoy or experience my sadness and anger.
Get everybody out of the house. Sit down and cry. Damn the universe, be mad at God, get it out, and be done with it. All that sadness and anger is toxic for your body, so you need to get it out.
My mom has been dealing with Alzheimer’s for 12 or 13 years. I needed my mommy. I wanted her to tell me everything was going to be okay. Oddly enough, a few years ago when we went to visit, we were sitting at the table, and she had a moment of clarity.
She looked at me and said, “Have you been sick?” I said, “Yeah, mom. I have cancer.” She said, “Oh, you’re going to be okay.” I will hold that moment dearly forever.
Can you share your advice about self-advocacy?
Do your homework, and I don’t mean WebMD. Even do your research beyond the internet. Go and find somebody who had cancer.
Don’t listen to stories about Aunt Betty; go talk to Aunt Betty herself. Everybody’s body and experience is different, but still go and talk to someone. It helps to know that someone else survived and you can, too.
Make adjustments. Not everything has to be by the book. How you recover, how you take care of yourself, and how you cope is up to you. It doesn’t have to follow a formula.
Pay attention to your mental state. I had reiki done, and now I’m a reiki master. Meditation and medication helped me. Eastern and Western medicine came together for me. If something is wrong in your mental state, talk to someone about it or take it upon yourself to get it dealt with.
The most important thing that I learned is you need to trust your body. Your body will tell you what it needs.
»MORE: How to be a self-advocate as a patient

How did the experience affect your relationship?
We’re goofy. We make fun of everything and everybody — not in a judgmental way, but we’re just not so serious all the time. We’re not easily offended.
We were at the first chemo treatment, and we were making fun of something. We were cracking up. We were nervous, and we were using humor to make us feel better.
One of the senior nurses there said, ‘If you two can make it through this whole journey and you’re still laughing at the end, you’re going to make it as a couple.’ We took that very seriously.
Even in the moments I was defensive or angry and screaming, he’d be like, “Ah, shut up. Eat a taco.” I’d yell, “I hate you! Bring me a taco! But I still hate you!”
There was always a moment where one of us would bring the tension down a notch, and we would calm down. Then we would laugh about it.
On the last day of treatment, it just happened that the same nurse was working. We were still laughing. She said, “You’re still laughing. Good for you. You’re going to make it.” Here we are. We’ve been together for 7 years.
On the patient side, my advice is to give your disclaimers at the beginning: ‘I love you. Thank you. Forgive me when I get angry.’
Also, don’t take things so seriously. Take it day by day. I don’t mind cancer jokes. I didn’t want to be so serious about things. Yeah, I had cancer, but I was treating it. I didn’t want to think about the bad things that might happen.
From what I learned watching Christian, be patient and understanding. He was able to tell when my anger or frustration was just the treatment speaking. He knew I was exhausted. He knew when to water down the conversation so it didn’t get tense. He knew how to make light of it and when to.
More than anything, as a couple, enjoy every moment you can.
I know that sounds weird, but those intimate moments when you’re just laying there together, enjoy that moment. When there’s no nausea happening or tests being run or appointments to go to, enjoy the moment. Remember it’s just cancer, and you love each other.
»MORE: 3 Things To Remember If Your Spouse/Partner Is Diagnosed With Cancer
What is your “new normal”?
When I was younger, I had this idea that my lifespan was going to be 30 years. Then I was diagnosed with AIDS just before I turned 30.
Obviously, I didn’t die. During my 30s, I was a drug addict and alcoholic. I thought, “Okay. I probably won’t make it to 45.”
I got cancer at 45. Here I am now at 50. I’m very conscious about life. I believe that good and bad both have a place in my life. It’s what I make of it that matters.

I had that moment where I was bleeding out because of the fistula. I don’t remember, but there were two times in the hospital where I almost died. I’m not afraid of dying because I’ve been there at the door and didn’t get through. My friends and family say that God has a plan for me, and I surely believe that now. There are a lot of things I want to do.
Any time a door opens, I want to go see what’s inside. I’m very open. I love life. Life is wonderful — the good and the bad. If everything was good and lovely all the time, how boring would that be? I love a challenge, so life is a challenge now. I enjoy that.
I’m not thankful I’m alive. I’m thankful I have the strength and courage to do things and face things every day. I could be alive and not be able to do anything, but here I am.
I want to take over the world. Anything and everything I can put my hands on and learn from, I’ll do it.
What do you want to say to someone who has just been diagnosed?
If you’ve just been diagnosed with anal cancer, don’t worry. You’re going to kick its ass.
The first thing I would want to say is, “Whatever you’re feeling right now is valid.” Don’t apologize. Don’t change. If you’re scared, sad, or angry, feel it. Get through it, and then take charge.
Journal. Video blog. Record. Whatever you can do to keep up with your emotions. This might be the toughest thing you ever go through. One day you’re going to want to go back and remember how strong you are.
Inspired by Daniel's story?
Share your story, too!
Anal Cancer Stories
Daniel Garza, Stage 2
Cancer Details: Squamous cell carcinoma
1st Symptoms: Bloating, difficulty relieving himself
Treatment: Chemo, Radiation, Hyperbaric Chamber
...

4 replies on “Daniel’s Stage 2 Squamous Cell Carcinoma Anal Cancer Story”
Thank you for sharing. I’m half way through treatment, and had to stop temporarily because my wbc is too low. Been very sick. Mouth sores are the worst. I guess I should be somehow grateful that my Dr informed me it’s going to get much worse…. But you give me hope I will get through this, although I’m 20 years older than you.
I am diagnosed with anal cancer few months back now and am noy yet in treatment . I am very apprehensive and frightened of the long term damage as not having kids and erection not able to control my anal muscle are the 3 things which made me anxiously stupid as I have postponed the radio therapy . am in debilitating pain that even morphine doesn’t help but when I think the long term damage from the chemotherapy is nothing .
I am stupid and stubborn but mostly depressed .. anyone who can help by sharing their stories after chemo or radio ?
Thank you for sharing, Daniel. In September 2022 I started having ‘spaghetti poops.’ I went to my doctor and after pressure from me he finally referred me to specialists and in November 2022 I got the biopsy back – squamous stage II anal cancer. I began chemoradiation in December 2022, with my last session in January 2023. For me, the worst part were the burns around the front and back of my pelvis, which got worse for the 2 weeks after my last session. Also, the need to poop many many times each day/night and difficulty/pain urinating (the doc gave me flomax which fixed that.) I chose to not tell anyone except my husband and my sister, who both gave me amazing support and got me through it. My reasoning was I did not want people to feel sorry for me, combined with my being a bit of a loner. In retrospect, I wish I had told more friends and neighbors. Not for myself necessarily, but for my husband who was my caregiver. The caregiver definitely needs a strong outside support system, as you noted, Daniel. I had a digital exam in April 2023 and the tumor was gone. I hope in the next 1.5 years I can receive the same great news about remission that you did. Hugs!
Daniel. I just got daignosed and begin both chemo and radiation in 4 days on a similar schedule as you. Thank you so much for sharing your story because you speak your reality. Yours is the first story from a fellow older gay man about anal cancer that I could find. From my heart – thank you. Nobody really understands until they walk in your shoes in their own way. Peace my friend and may your remission be forever.