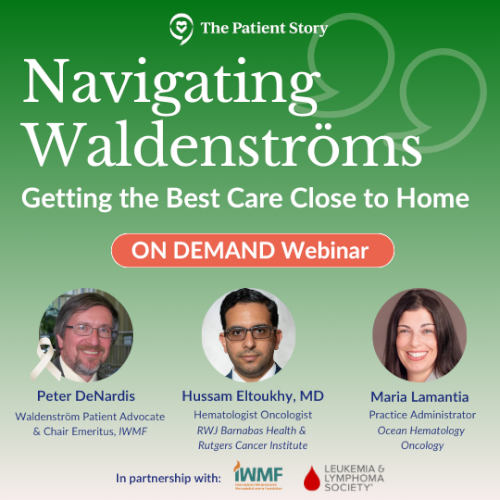
Navigating Waldenström’s: Getting the Best Care Close to Home
Unlock Better Waldenström’s Care – Right in Your Community!
Waldenström macroglobulinemia (WM) patient advocate Pete DeNardis, expert hematologist Dr. Hussam Eltoukhy, and practice administrator Maria Lamantia discuss the latest in community-based cancer care, personalized treatment options, and effective communication strategies.
Whether you’re newly diagnosed with WM or managing ongoing treatment, learn how to optimize your care, navigate “watch and wait,” and access clinical trials without leaving your local support network.
Effective Community Cancer Care: Learn how local treatment options can be both effective and personalized for Waldenström’s patients.
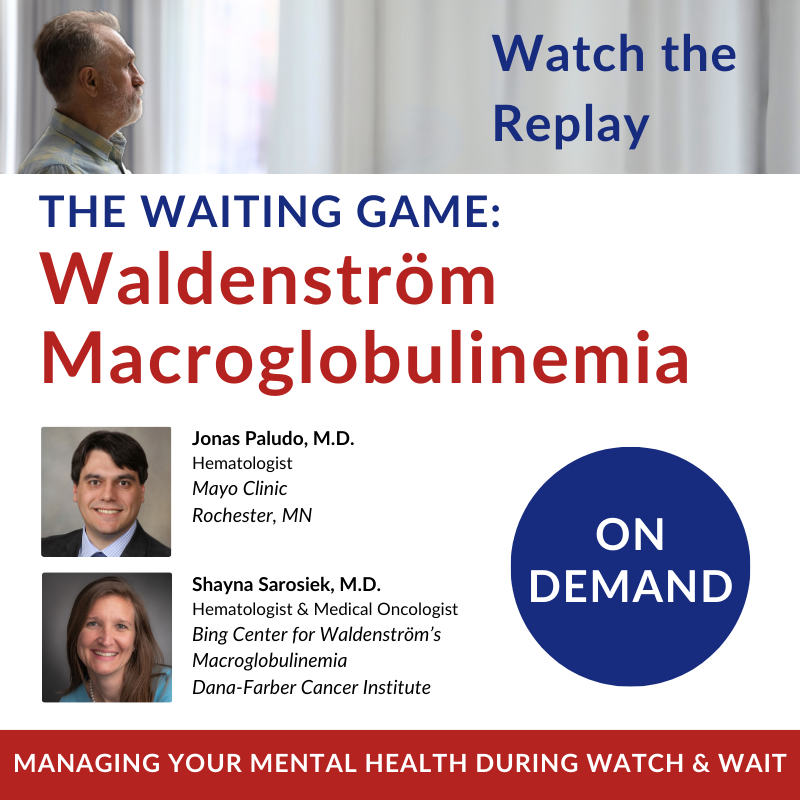
Navigating Watch and Wait: Get emotional and practical support for managing the uncertainties of the “watch and wait” approach.
Advocate for Better Care: Discover communication strategies to ensure you’re getting the best care from your local oncologist.
Latest Treatment Options: Understand new therapies and clinical trials that are available even in community settings.
Access to Specialized Care: Find out how collaboration with larger cancer centers can enhance your treatment journey.

We would like to thank The Leukemia & Lymphoma Society and the International Waldenström’s Macroglobulinemia Foundation for their partnership.
This interview has been edited for clarity and length. This is not medical advice. Please consult with your healthcare provider for treatment decisions.

Thank you to Pharmacyclics, an AbbVie company, for its support of our patient education program. The Patient Story retains full editorial control over all content.
Edited by: Katrina Villareal
- Introduction
- The Most Common First Symptoms of Waldenström’s
- Common Steps to Diagnose Waldenström’s
- How to Communicate with Your Primary Care Physician the Need to See a Specialist
- Deciding Whether to Go to an Academic/Research Center or Community Hospital
- The Biggest Challenge for Waldenström’s Patients Who Get Community Care
- Referring Waldenström’s Patients to an Academic Center
- Referring Waldenström’s Patients to Another Specialist for a Second Opinion
- What Waldenström’s Patients Should Consider in Choosing a Community Hospital or Provider
- Financial Benefit of Going to a Community Provider
- Monitoring Waldenström’s Patients on Watch and Wait
- How Waldenström’s Patients Should Talk to Their Healthcare Team About Their Symptoms
- Clinical Trials for Waldenström’s Patients
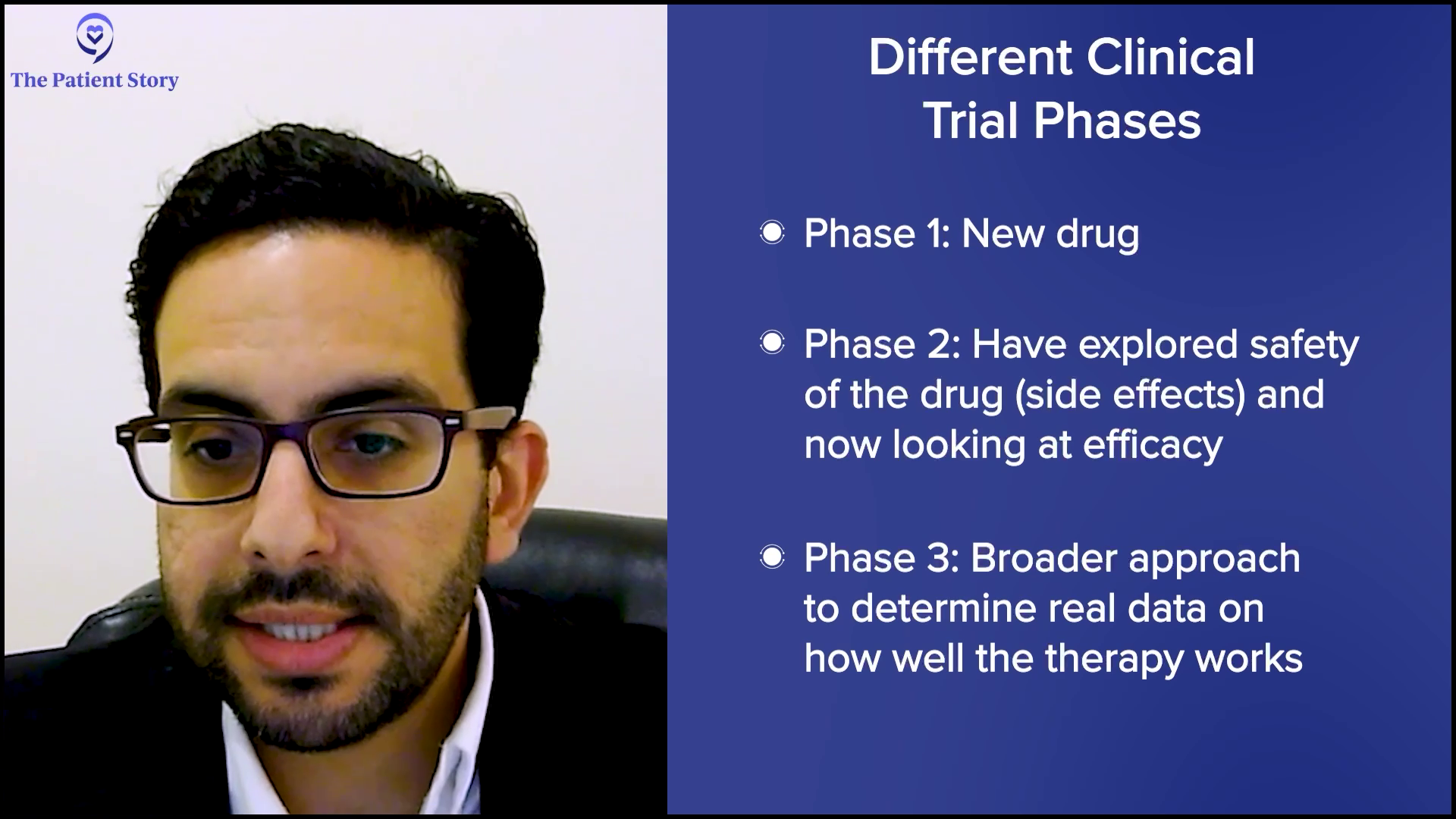
- Different Phases of Clinical Trials
- Busting Clinical Trial Myths
- Bringing Waldenström’s Clinical Trials to the Community Cancer Care Site
- Final Takeaways
Introduction
Stephanie Chuang: We know most Americans are getting their cancer care at their local hospital or clinic and not at the large academic institutions, maybe not regularly or not even at all. But you may also hear that for blood cancers like Waldenström’s, it’s important to see a specialist. What does this mean and how can patients and their care partners successfully get the best care?
I’m the founder of The Patient Story. I was diagnosed with a different kind of non-Hodgkin lymphoma, diffuse large B-cell lymphoma. When I was getting my 600-plus hours of chemoimmunotherapy, the idea came up: how can we help cancer patients and care partners navigate life at and after diagnosis? That’s what The Patient Story focuses on.
We aim to build community through in-depth patient stories. We reach millions of people every month. We build educational discussions in collaboration with amazing partners, like The Leukemia & Lymphoma Society (LLS) and the International Waldenström’s Macroglobulinemia Foundation (IWMF).
The LLS offers free resources like its Information Specialists, who are one free call away for support in different areas of blood cancer. The IWMF offers many support resources specifically for the Waldenström’s community, including dozens of in-person support groups around the world in addition to so many that are happening online.

We also want to thank our sponsor, Pharmacyclics, an AbbVie company, for its support, which truly helps us to host more of these programs for free to our audience. I want to stress that The Patient Story retains full editorial control over all content as always. While we hope that this is helpful, keep in mind this is not a substitute for medical advice, so still consult with your own team about your decisions.
This is sure to be an incredible discussion led by friend of The Patient Story and long-time advocate with the IWMF, Pete DeNardis.

Pete DeNardis: I’m chair emeritus of the International Waldenström’s Macroglobulinemia Foundation and a long-time volunteer for the organization. I’m a patient myself, was diagnosed in October 2003, and have had multiple periods of treatment and watch-and-wait status over the years. My treatment has included chemotherapy, radiation, monoclonal antibodies, and targeted therapies. Most recently, my WM has been behaving itself.
I live in Pennsylvania and my care is directed by a hematologist at a cancer teaching hospital. Over the years, I have had overnight stays in a university-based hospital and at local community hospitals in emergency situations. I will be joined by Dr. Hussam Eltoukhy and Maria Lamantia.
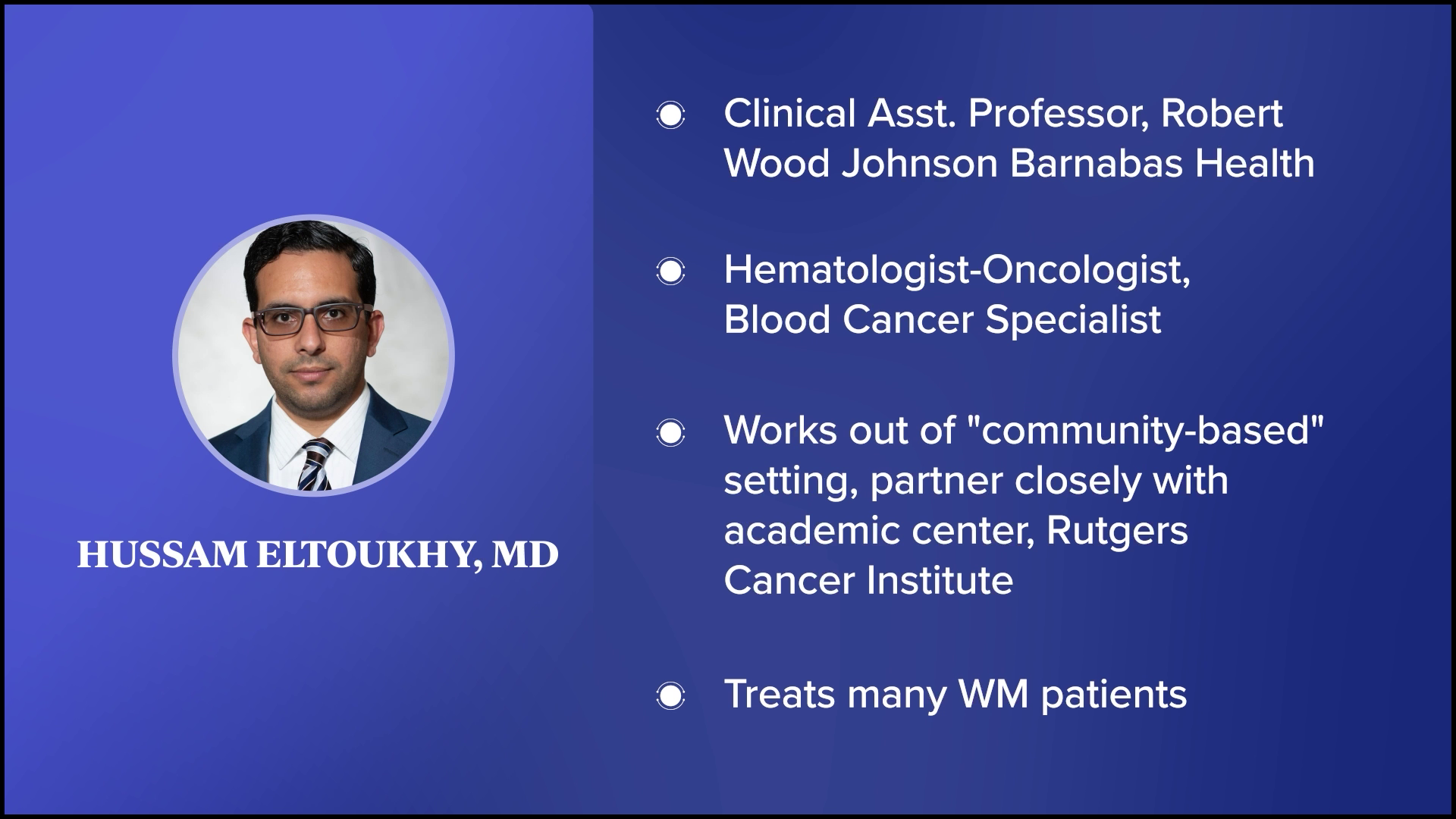
Dr. Hussam Eltoukhy: I’m a clinical assistant professor with RWJBarnabas Health and the Rutgers Cancer Institute of New Jersey. I’m a hematologist specializing in blood cancers.
My role is interesting. I work out of a community-based setting but in close partnership with our academic center, the Rutgers Cancer Institute, which gives me a very different perspective on treating patients. I have many patients with Waldenström’s and other conditions, and I’m thankful to be here to talk more about that.


Maria Lamantia: I’m so happy to work alongside Dr. Eltoukhy. We work together as a team. We have a wonderful staff and we treat our patients like family. Working alongside Dr. Eltoukhy, I see him take the time with his patients to answer all of their questions. We treat them emotionally and physically, so we need to treat them as a whole.
Pete: That’s fantastic. Patients need to have a good relationship with their healthcare professionals, especially for people with rare cancers like Waldenström’s, and to have a very caring and a very productive relationship. It sounds like you’re doing a fantastic job.
The Most Common First Symptoms of Waldenström’s
Pete: We want to get your perspective on how you approach Waldenström’s patients. Dr. Eltoukhy, can you describe the typical diagnostic journey for a patient with WM? What are the initial symptoms you usually see? Do you run certain tests when a patient comes in?

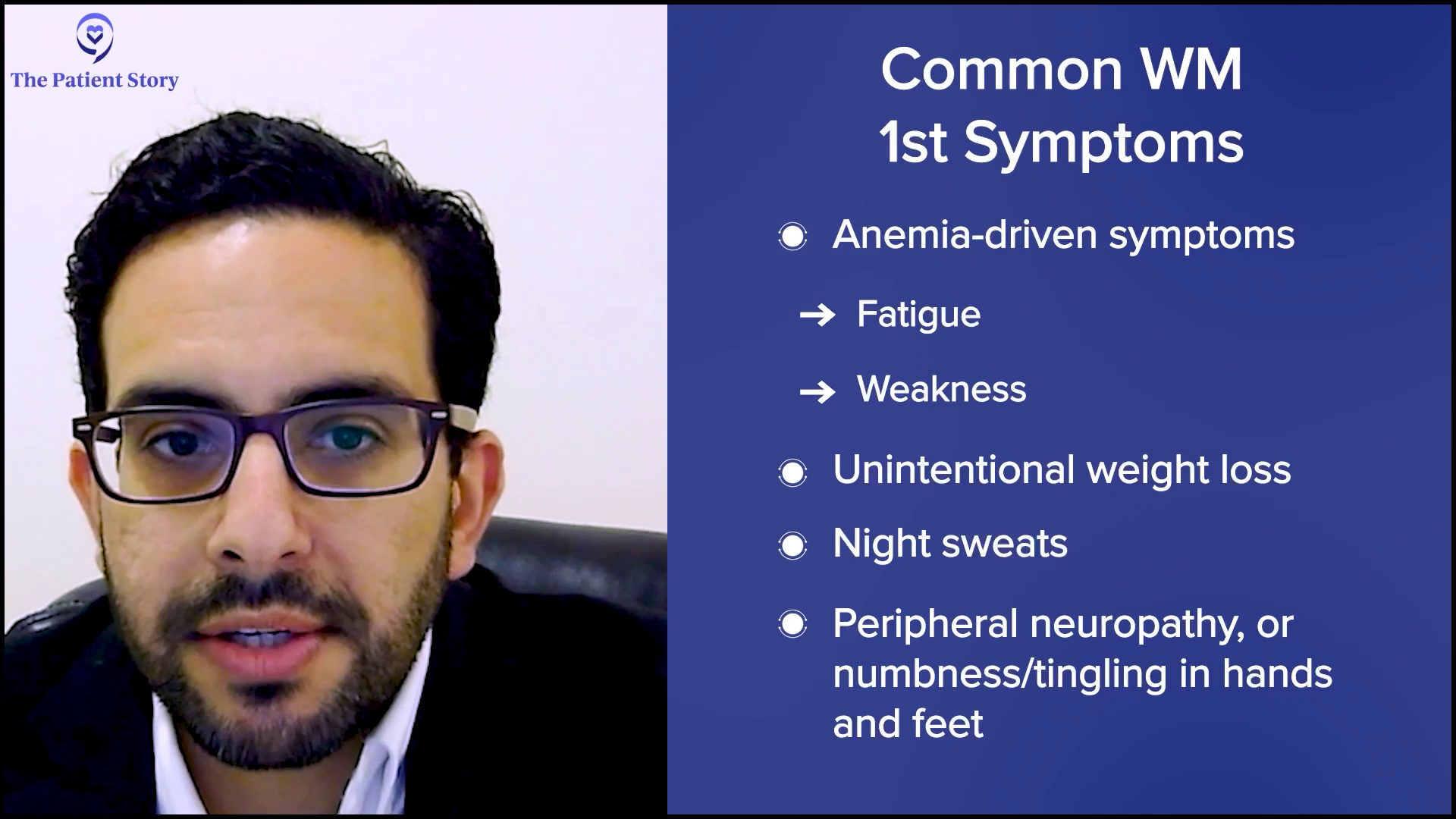
Dr. Eltoukhy: The diagnostic journey for a patient with Waldenström’s often can be prolonged because the initial symptoms are quite nonspecific and can mimic other conditions. The most common symptoms patients report are fatigue and weakness, which are most often due to anemia. Some patients may also experience unintentional weight loss, night sweats, and peripheral neuropathy, which presents as numbness or tingling in the hands and feet. In more advanced cases, symptoms related to hyperviscosity, like headaches, blurred vision, dizziness, or even nosebleeds may develop.
Common Steps to Diagnose Waldenström’s
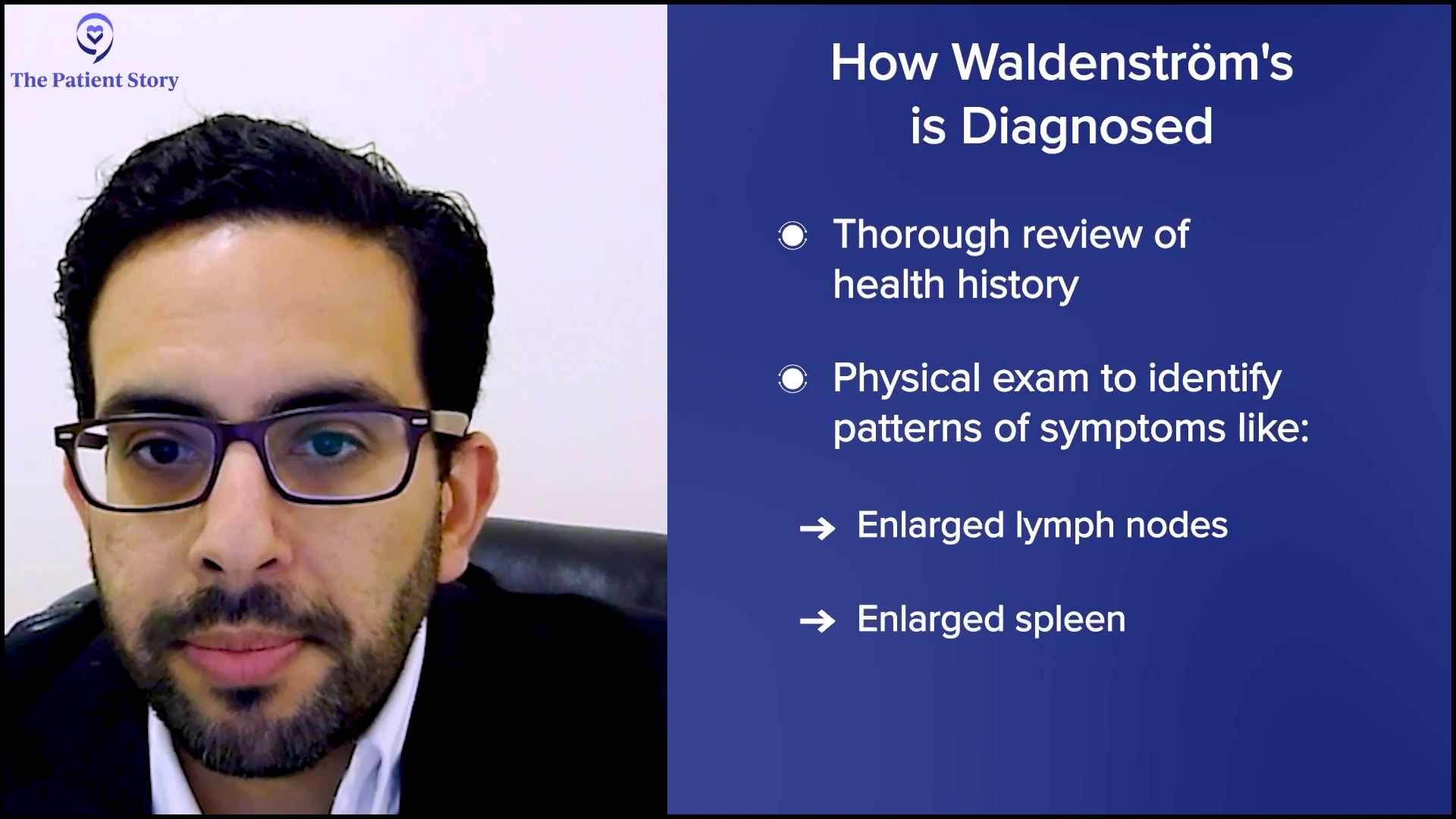
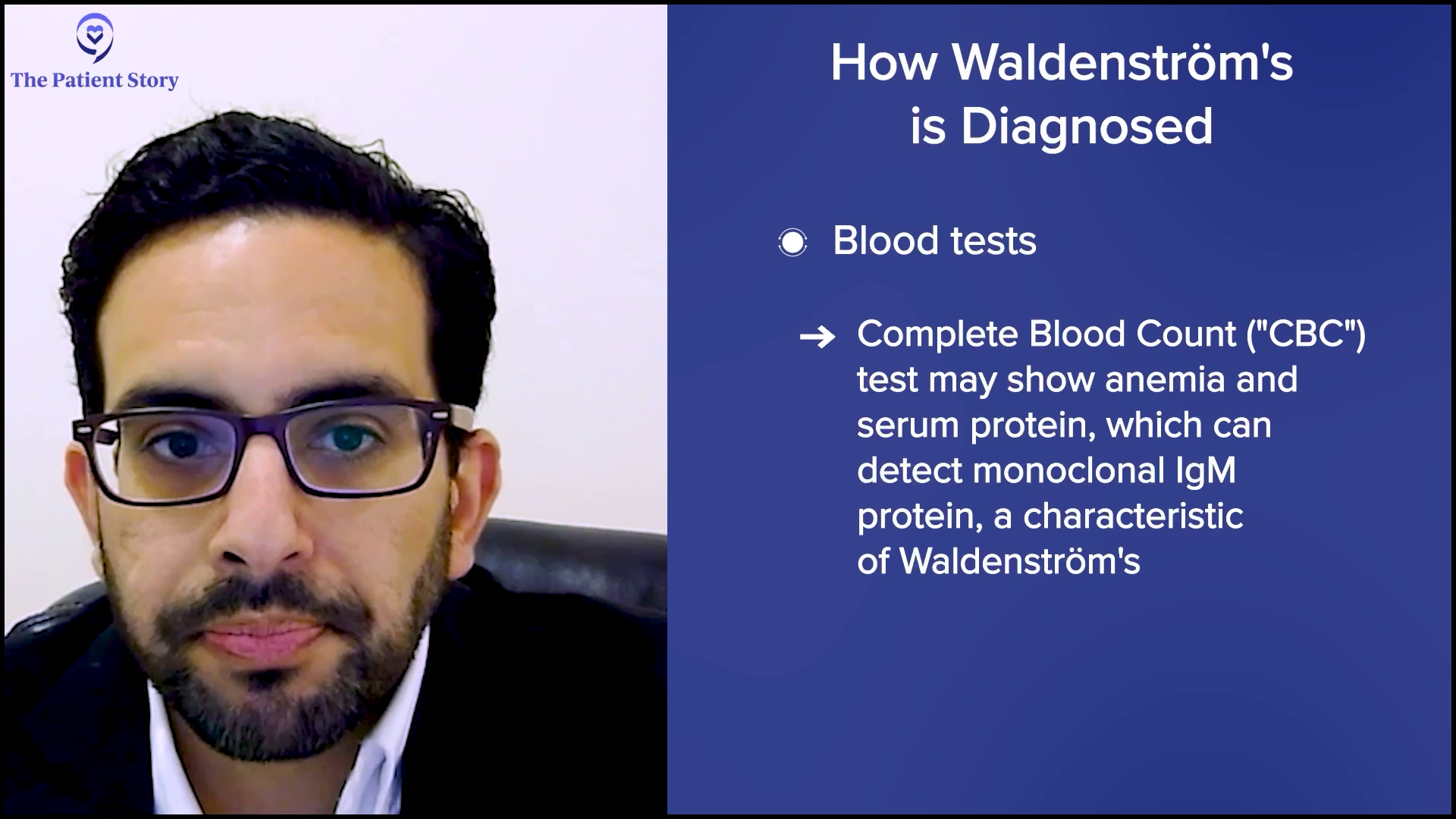
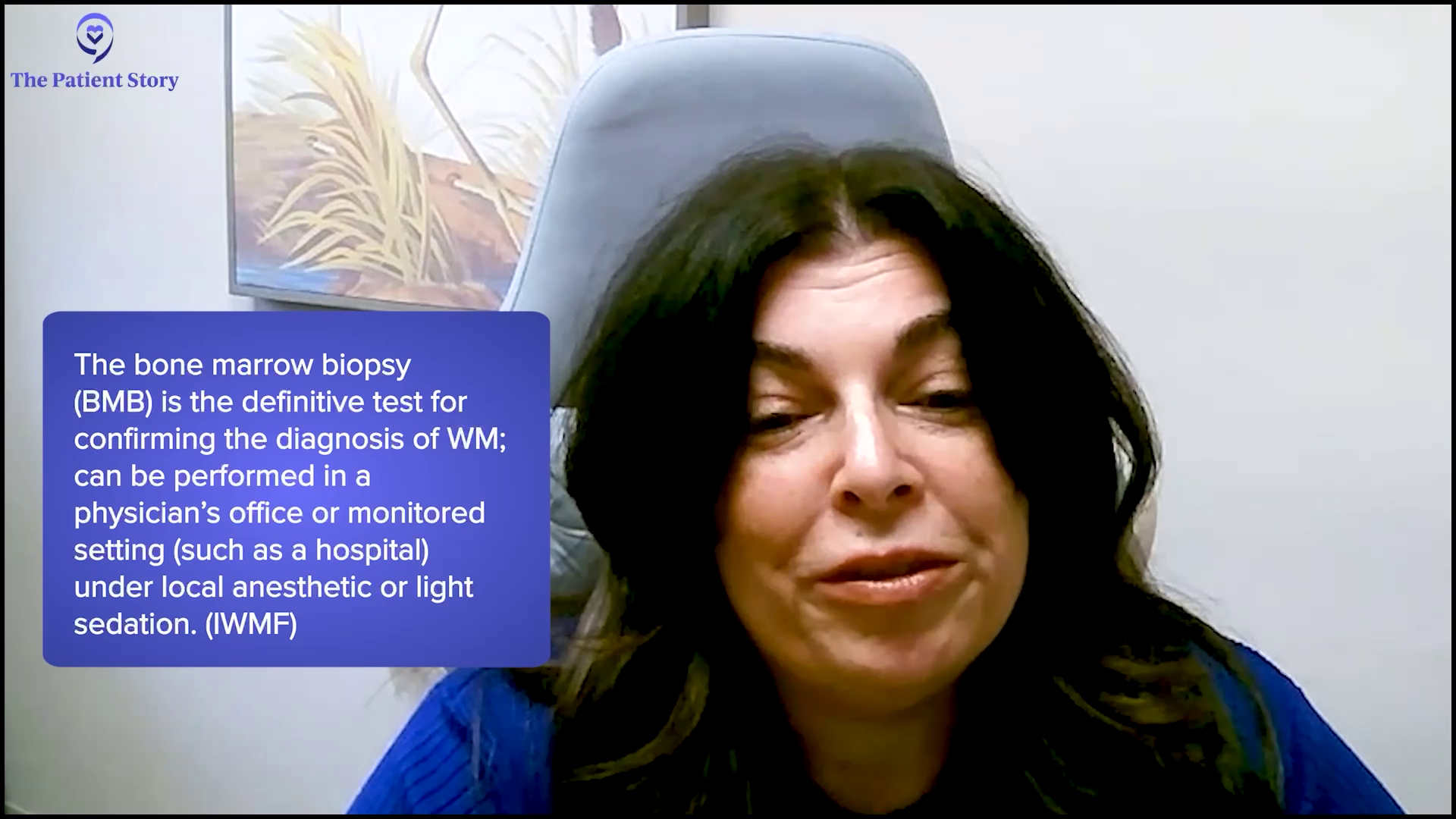
Dr. Eltoukhy: The diagnostic approach typically starts with a thorough history and physical exam, which is critical for identifying patterns of symptoms and any physical signs, like enlarged lymph nodes or spleen. From there, blood tests are usually the first step. A complete blood count might show anemia and serum protein electrophoresis can detect a monoclonal IgM protein, which is characteristic of Waldenström’s. Further testing with immunofixation and serum viscosity levels can provide more details.
Once Waldenström’s is suspected, a bone marrow biopsy is essential to confirm the diagnosis. It will show the infiltration of lymphoplasmacytic cells. The bone marrow can be tested for other things, like the MYD88 mutation, which is present in over 90% of Waldenström’s cases. Imaging studies like CT scans can be useful in assessing lymph node or organ involvement.
Diagnosing Waldenström’s requires piecing together clinical signs, lab results, and histologic findings. Because the symptoms can be subtle or overlap with other conditions, taking a comprehensive history and performing a thorough physical exam is foundational in guiding the diagnostic workup.

How to Communicate with Your Primary Care Physician the Need to See a Specialist
Pete: I can tell by your response that you have a lot of experience with Waldenström’s patients. You’re hitting all the high notes and the critical aspects of diagnosing someone with Waldenström’s. Sometimes the symptoms manifest over a longer time.
I had classic symptoms, but I didn’t realize it then. I kept on thinking it was something else and waited a long time before I saw my doctor. How can a patient best communicate their concerns to their primary care physician to ensure a timely referral to a specialist? How do we get people to understand that we should take this to the next level in terms of testing and analysis of what’s going on?
If something feels off… it’s crucial to report these symptoms accurately and thoroughly.
Dr. Hussam Eltoukhy
Dr. Eltoukhy: Interestingly, that happens a lot. When it comes to ensuring a timely referral to a specialist, one of the most important things patients can do is to be clear and proactive in communicating their concerns. First and foremost, patients should be their own advocates. If something feels off — like you’re having persistent fatigue, unexplained weight loss, night sweats, or any unusual symptoms such as numbness or frequent infections — it’s crucial to report these symptoms accurately and thoroughly. Even if the symptoms seem minor or unrelated, sharing the full picture helps the physician connect the dots.
It’s also helpful for patients to record their symptoms: noting when they started, how often they occur, and whether they’re getting worse over time. This level of detail provides valuable context that can prompt a physician to dig deeper and consider a hematologic cause like Waldenström’s.
In addition, there should be no hesitation to express concerns directly. If they feel their symptoms are not improving or are being overlooked, it’s perfectly appropriate to ask, “Could this be something more serious? Do you think I should see a specialist?” Open and honest communication ensures the primary care physician fully understands the patient’s level of concern and can make an informed decision about referring them to a hematologist. Ultimately, while I know that physicians play a key role in guiding care, patients who actively engage in the process and advocate for themselves help ensure timely, appropriate evaluations.
Deciding Whether to Go to an Academic/Research Center or Community Hospital
Pete: In many cases, an important aspect of receiving treatment is where you get treatment. Of course, what determines that could be where you’re located and what type of services are available to you. This brings up the conversation of cancer care in a community setting or a suburban/rural setting. What’s the difference between a community hospital versus an academic center or a cancer hospital? How can people best understand the difference between them? If it does make a difference, how do they know which one to go to?
Dr. Eltoukhy: When we talk about cancer care in general, especially for rare diseases like Waldenström’s, the setting where a patient receives treatment can be as important as the treatment itself. Broadly speaking, there are key differences between community hospitals and academic medical centers or more specialized cancer centers.
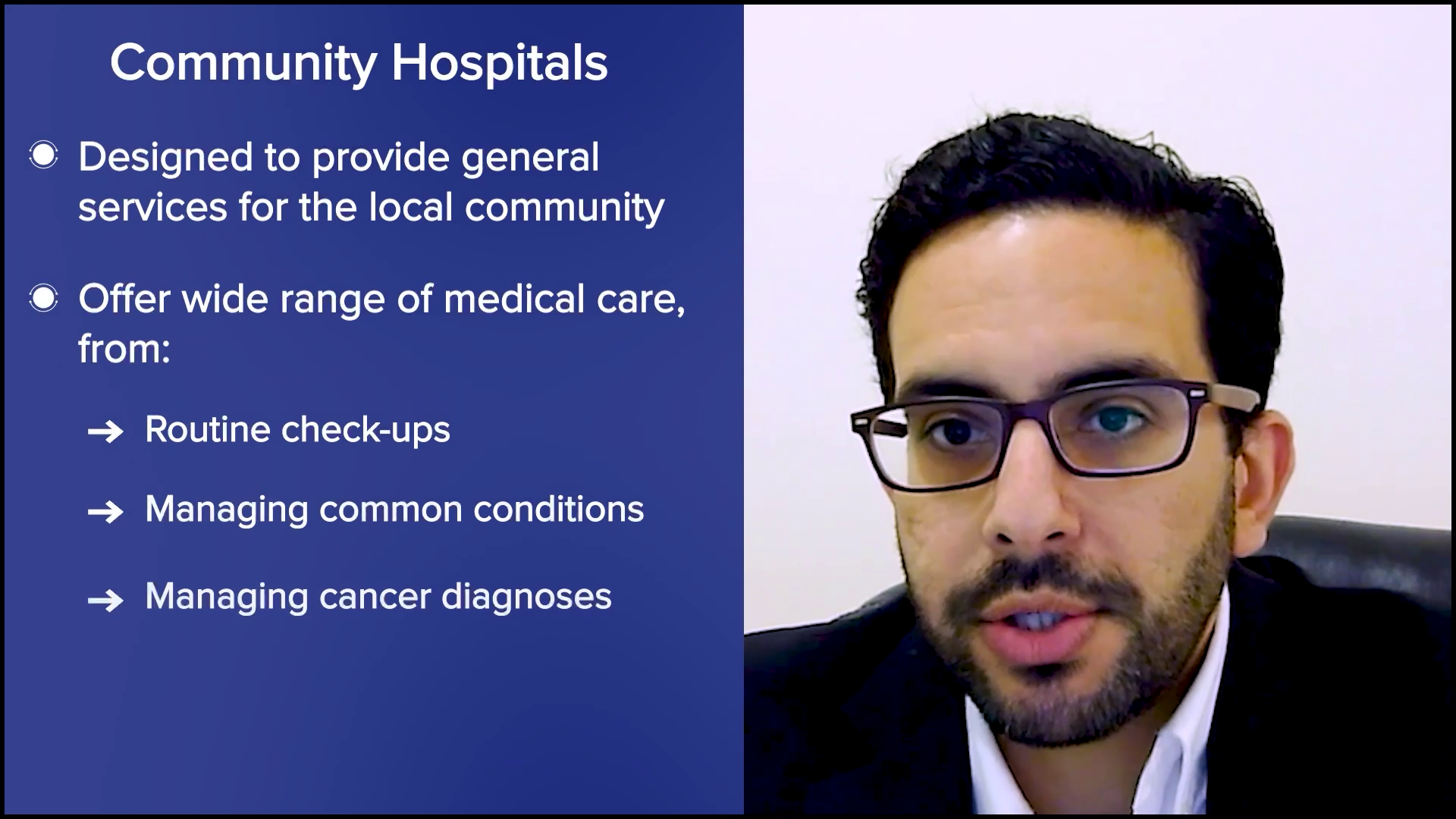
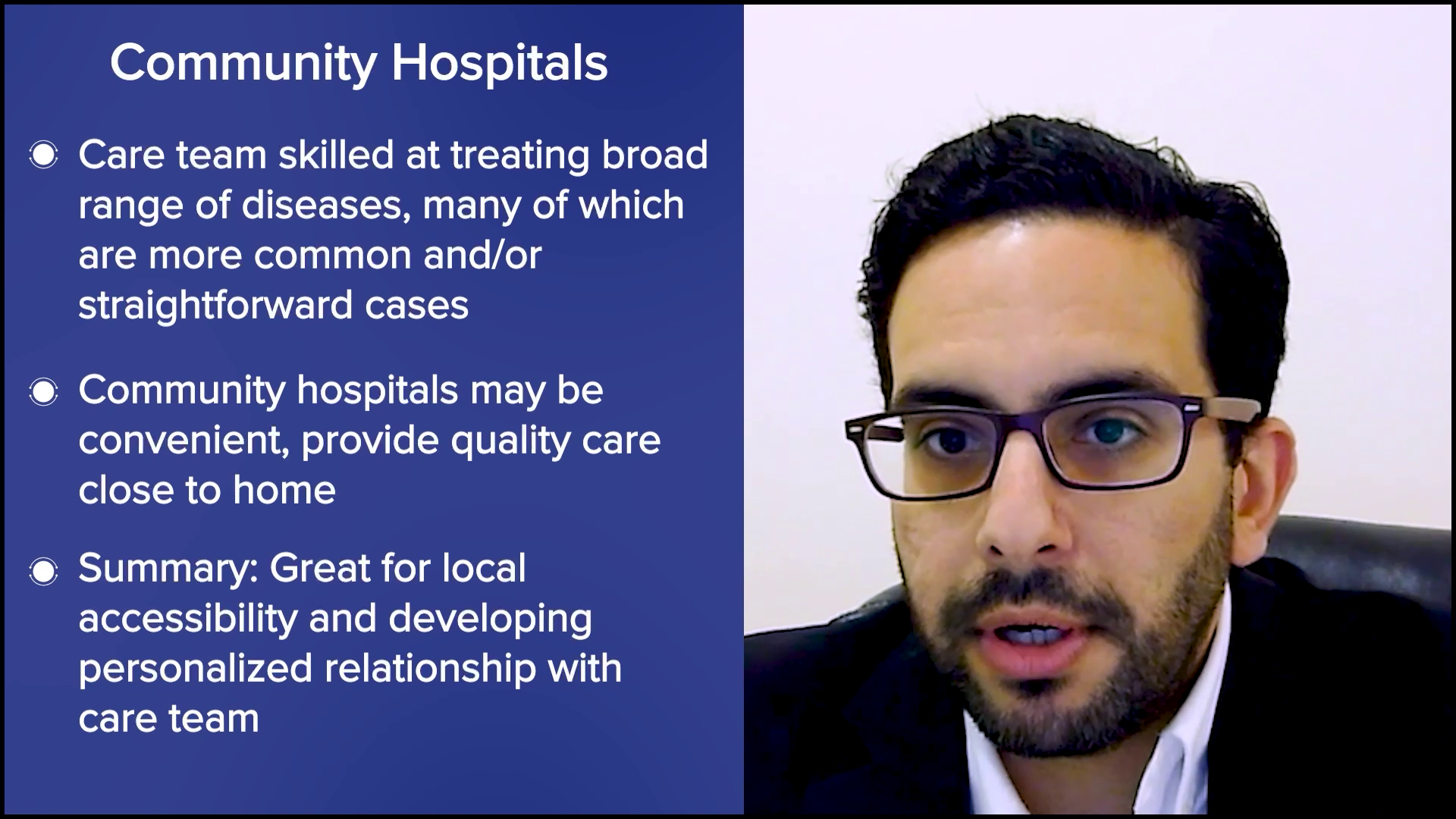
By design, community hospitals are designed to provide general health care services to the local population. They offer a wide range of medical care, from routine checkups to managing common conditions and even some cancers. The care teams in these settings are skilled at treating a broad spectrum of diseases. For patients with more common or straightforward cases, community hospitals are convenient and provide excellent care close to home. Accessibility is a big advantage because patients don’t have to travel far. They also often have a more personalized relationship with their care team.
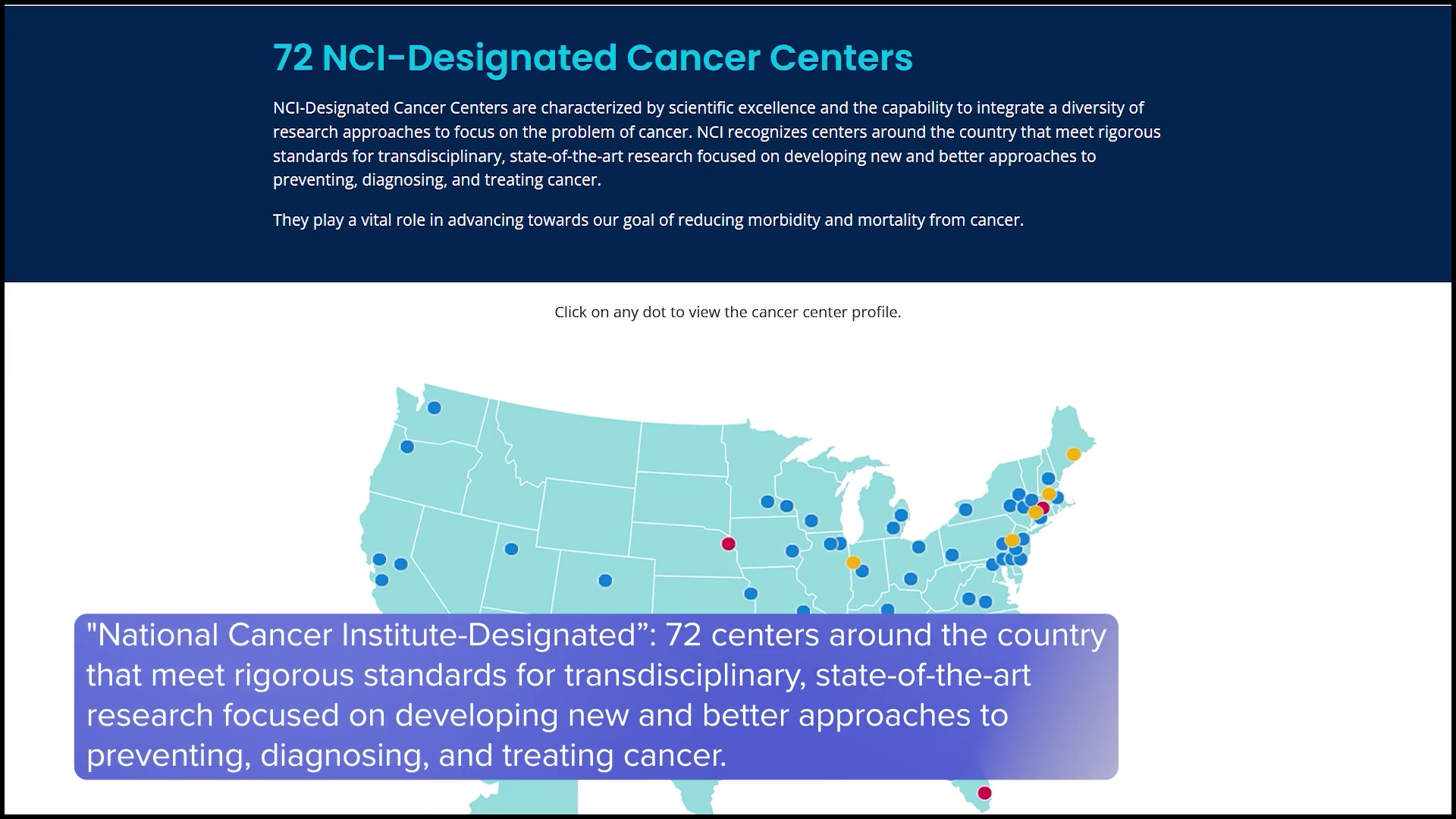
On the other hand, academic medical centers and specialized cancer hospitals focus heavily on research, teaching, and clinical trials, so these centers are often affiliated with medical schools and are involved in clinical trials, so they’re at the forefront of new treatments and therapies. Patients treated at these centers may have access to novel therapies that aren’t widely available in the community setting. Additionally, these institutions have multidisciplinary teams, which include hematologists, pathologists, and other specialists who focus specifically on rare cancers providing a more specialized approach.
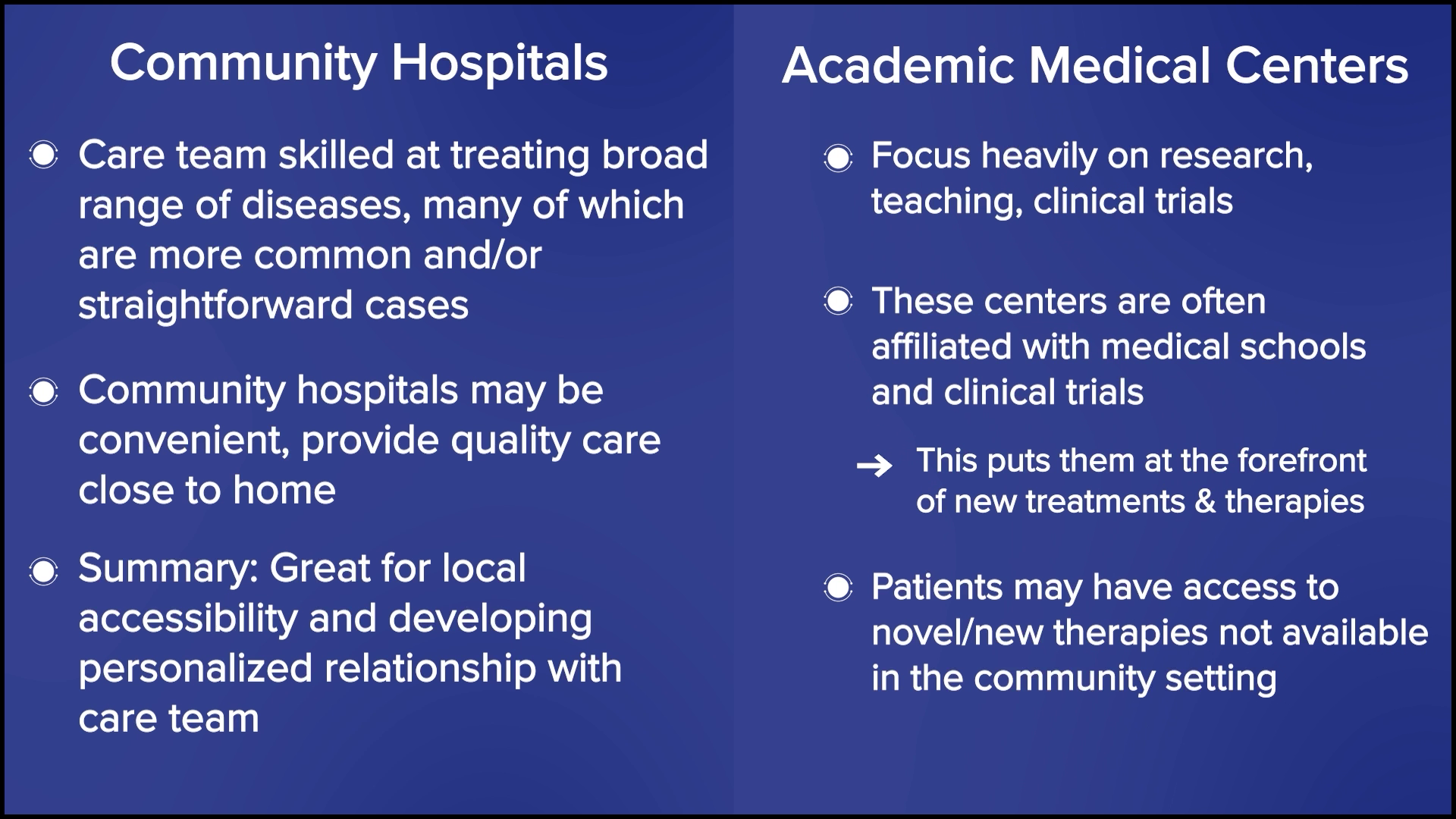
In terms of the patient population, your typical community hospital will manage more common cancers and straightforward cases, while academic centers are more in tune to see more complex, rare, or treatment-resistant cases. However, this does not mean that community hospitals cannot manage diseases like Waldenström’s effectively. Many do, such as ours, especially with proper collaboration and referral pathways.
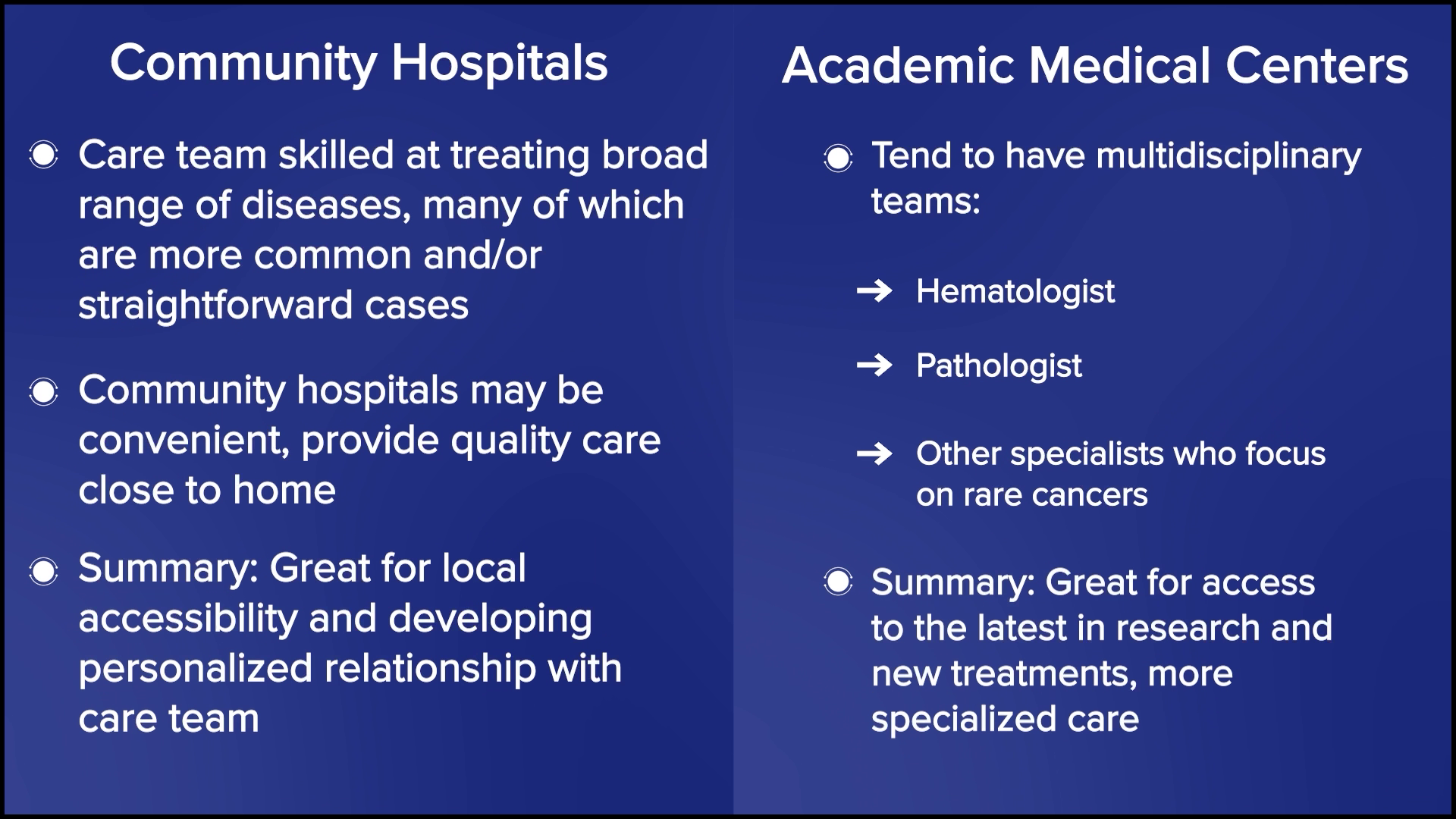
Ultimately, the best approach may involve a balance between the two settings. Patients might receive specialized consultation at an academic center while continuing their routine care and follow-ups in the community, ensuring both accessibility and cutting-edge treatment options.
Stephanie: Dr. Eltoukhy, I want to jump in very quickly as we have two patient perspectives about how they were able to figure out the best Waldenström’s care for themselves. Annmarie was diagnosed a few years ago and heard right away to see a specialist. Bob, on the other hand, was diagnosed in 1997, which was a very different time, and says the IWMF was instrumental in helping him link between a local care team and a specialist. Bob, what was it like trying to figure out your care almost three decades ago?
Bob B.: First of all, my local oncologist didn’t know about how I should be treated. With IWMF, we were able to get Arnie’s advice. There was some research going on at Scripps, MD Anderson, Lombardi Comprehensive Cancer Center, Mayo Clinic, and a couple of others. We visited a few places to go through the discovery of what might seem to make the most sense to be treated, bring that information back to my local oncologist, and allow him to be my quarterback.
Annmarie S.: If you’re lucky enough to go to a place with specialized care, that’s crucial in terms of them understanding the disease, diagnosis, different treatments, what future treatments can look like, research, and all the positivity that comes along with that. What’s challenging with Waldenström’s is general practitioners and hematologists don’t understand what it’s all about in terms of care and the next level of getting treatment, so they look at it more broadly as a cancer.

When you go to the next level and get a Waldenström’s specialist, they treat it more as disease management if you will. A lot of times, people cannot do that. Sometimes people are comfortable with the practitioner that they have. Utilize a facility that treats Waldenström’s and if you have to use your primary care physician or a general hematologist, have a Waldenström’s team as part of your overall treatment plan.

The Biggest Challenge for Waldenström’s Patients Who Get Community Care
Pete: In my situation, I go to a local university-based hospital because it’s as convenient as going to a community hospital. My condition is a little unusual even among rare cancer patients. What would you consider is the biggest challenge to providing cancer care in a local community setting, like in a rural setting?
Dr. Eltoukhy: One of the biggest challenges in providing cancer care in the local community setting comes down to the availability of resources. It’s not about the knowledge or expertise. We have highly skilled specialists dedicated to treating complex conditions like Waldenström’s. The challenge lies more in the infrastructure and support systems compared to larger cancer centers.

For example, while I can offer phase 2 and 3 clinical trials in my community practice, phase 1 trials, which are often the first step in introducing new therapies, typically require more specialized resources and are more readily available at larger academic or dedicated cancer centers. This includes specialized monitoring, regulatory oversight, and more intensive support systems.
Another significant factor is personnel. Larger cancer centers tend to have extensive multidisciplinary teams with dedicated staff for clinical trials, patient navigation, and supportive care services. In the community setting, we operate with leaner teams, so it can be more challenging to coordinate the logistics of complex care or get patients enrolled in trials as quickly as we’d like.
One of the biggest challenges in providing cancer care in the local community setting comes down to the availability of resources… It’s not that care is any less thorough, but the resources to streamline and support those processes are more limited.
Dr. Hussam Eltoukhy
It’s not that care is any less thorough, but the resources to streamline and support those processes are more limited. That said, working closely with the cancer center, as I do, helps bridge some of those gaps. We can offer high-quality, specialized care locally while collaborating with larger institutions to ensure patients have access to the full spectrum of treatment options when needed. The goal is always to deliver the best possible care, whether it’s in the community or at a specialized center.
Pete: That’s great. I like how you touched on clinical trials. We try to encourage patients in the Waldenström’s macroglobulinemia community to seek out clinical trials whenever they can. It’s good to know that even in a community hospital setting, patients can participate in a clinical trial.
Referring Waldenström’s Patients to an Academic Center
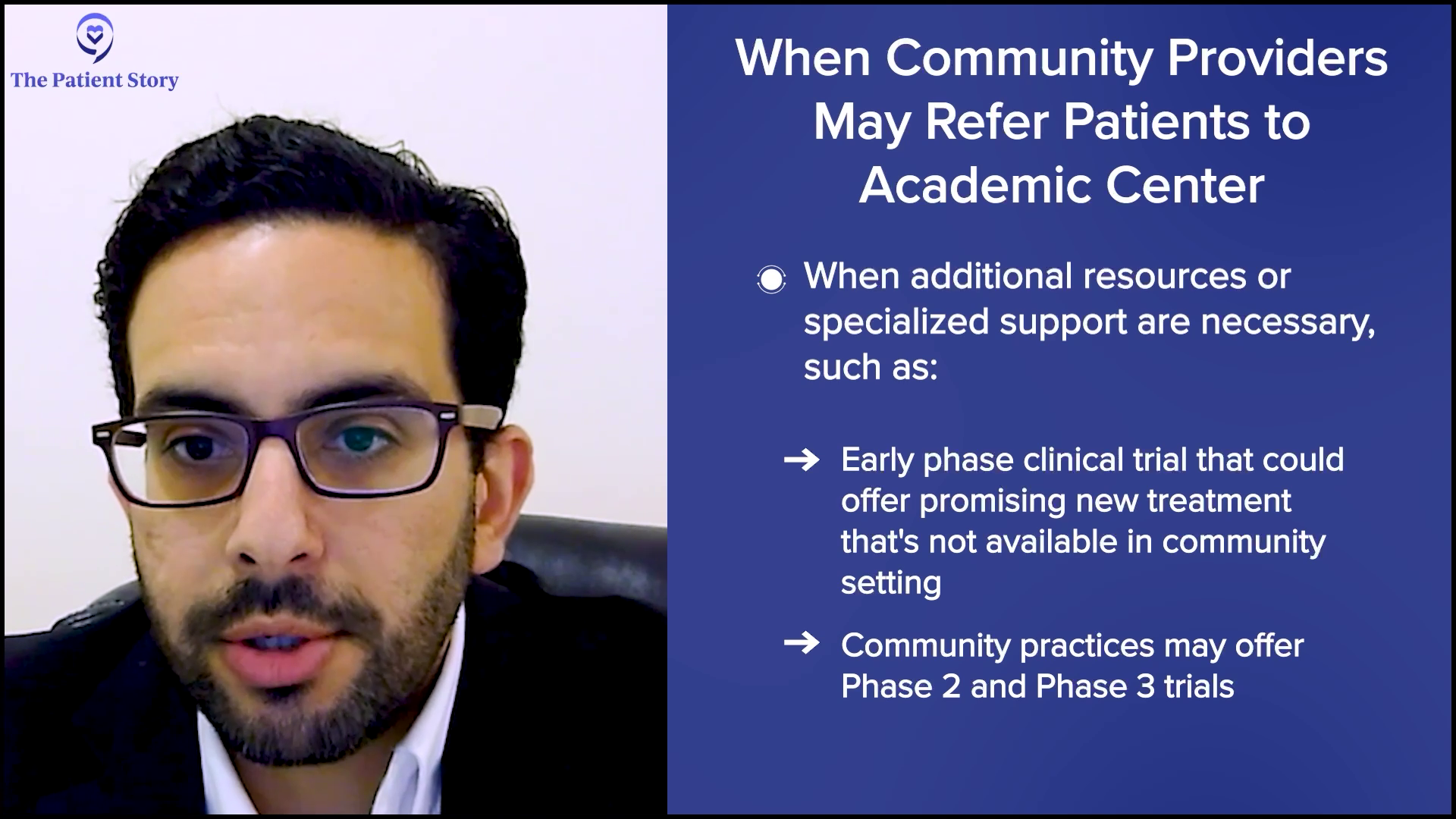
Pete: From a community setting, collaboration is important with larger hospitals when the need arises. Are there circumstances where you refer your patients to a larger center or to another hospital setting where there are more people with more extensive knowledge or more facilities that can tend to their particular circumstances?
Dr. Eltoukhy: Yes. As a blood cancer specialist practicing in a community setting, I feel fully confident managing a wide range of hematological malignancies, including Waldenström’s. My knowledge and expertise are not limiting factors when it comes to providing high-quality care for these patients. However, collaboration with our main cancer center and other academic institutions is vital to ensuring patients have access to the full spectrum of treatment options when needed.

Typically, there are two main circumstances where I would refer a patient to a larger center. The first is when additional resources or specialized support are necessary. For example, if there’s a clinical trial, particularly an early phase trial, that could offer a promising new therapy not available in our community setting, I would absolutely refer a patient to take advantage of that opportunity. While we do offer phase 2 and 3 trials locally, phase 1 trials are very specialized research protocols usually housed in these larger academic centers with the infrastructure to support them.
The second scenario involves treatments that require specialized procedures we don’t currently offer at our center. While this isn’t specific to Waldenström’s, right now, therapies like bone marrow transplants or CAR T-cell therapy are examples of advanced treatments that require more dedicated facilities and more specialized teams with highly specific protocols. These are scenarios where I would refer to the academic center.
Referrals are part of a collaborative approach… This partnership allows patients to receive cutting-edge treatments without losing the personalized, accessible care they value in the community.
Dr. Hussam Eltoukhy
That said, these referrals are part of a collaborative approach, so even when a patient is referred out for a specific treatment or trial, I remain closely involved in their care, coordinating with the academic center to ensure a smooth transition and continuity of care when they return to the community setting for a follow-up. This partnership allows patients to receive cutting-edge treatments without losing the personalized, accessible care they value in the community.
Referring Waldenström’s Patients to Another Specialist for a Second Opinion
Pete: In line with that, the IWMF provides a list of several dozens of doctors who are considered second-opinion doctors because perhaps they work at an institution that focuses solely on Waldenström’s, like Dana-Farber Cancer Institute or Mayo Clinic. Have you ever referred a patient for a second opinion because their situation is so unusual? And is that a common practice?
Dr. Eltoukhy: Yes, that is. Typically in the community, a lot of oncologists would be what we consider generalists, which means they treat a lot of different conditions. The referral basis for these doctors would be a lot more than me. Being a blood cancer specialist, while I don’t do it as often as I would if I was a generalist, I absolutely do on a regular basis. These come back to the patients who are treatment-resistant or unusual cases when we send out pathology and the pathology comes back blurring the lines between two different diseases, which happens quite often in blood cancers.
In our center at least, I collaborate very closely with the Rutgers Cancer Institute. We have combined tumor boards and I will refer patients. For most patients, first-line treatment will be the standard of care. No matter where you go, there’s somewhat of an agreement about what the standard of care would be.
Once you get to the second, third, fourth, fifth, and so on lines of treatment, that’s when I in the community setting or other doctors in an academic center usually go to other colleagues to get their opinion. Seeing me in the community doesn’t mean you don’t get the opinions of the other doctors in the academic center. I’m always presenting on these two boards, sharing the cases, and getting other doctors opinions. This shouldn’t be an ego thing. It’s more about giving the best care possible to the patients.
Pete: I can tell by your responses that you obviously are a doctor who has the needs and the health of the patient as the number one priority and I commend you for that.

What Waldenström’s Patients Should Consider in Choosing a Community Hospital or Provider
Pete: For patients who don’t require specialized care, can you describe how going to a community hospital could be in their best interest and benefit them?
Dr. Eltoukhy: There is a common misconception that community cancer care isn’t as high quality as what you’d find at a larger academic center, but that’s simply not true. For many patients who don’t require highly specialized treatments, receiving care in a community setting can offer distinct advantages without compromising the quality of care.
First and foremost, being treated closer to home means patients are in a familiar environment surrounded by their support system, such as family, friends, and their local community. That comfort can play a huge role in how patients cope with a cancer diagnosis and treatment. It feels like you’re in your own backyard, which can make the entire experience less overwhelming. But it’s not just about convenience.
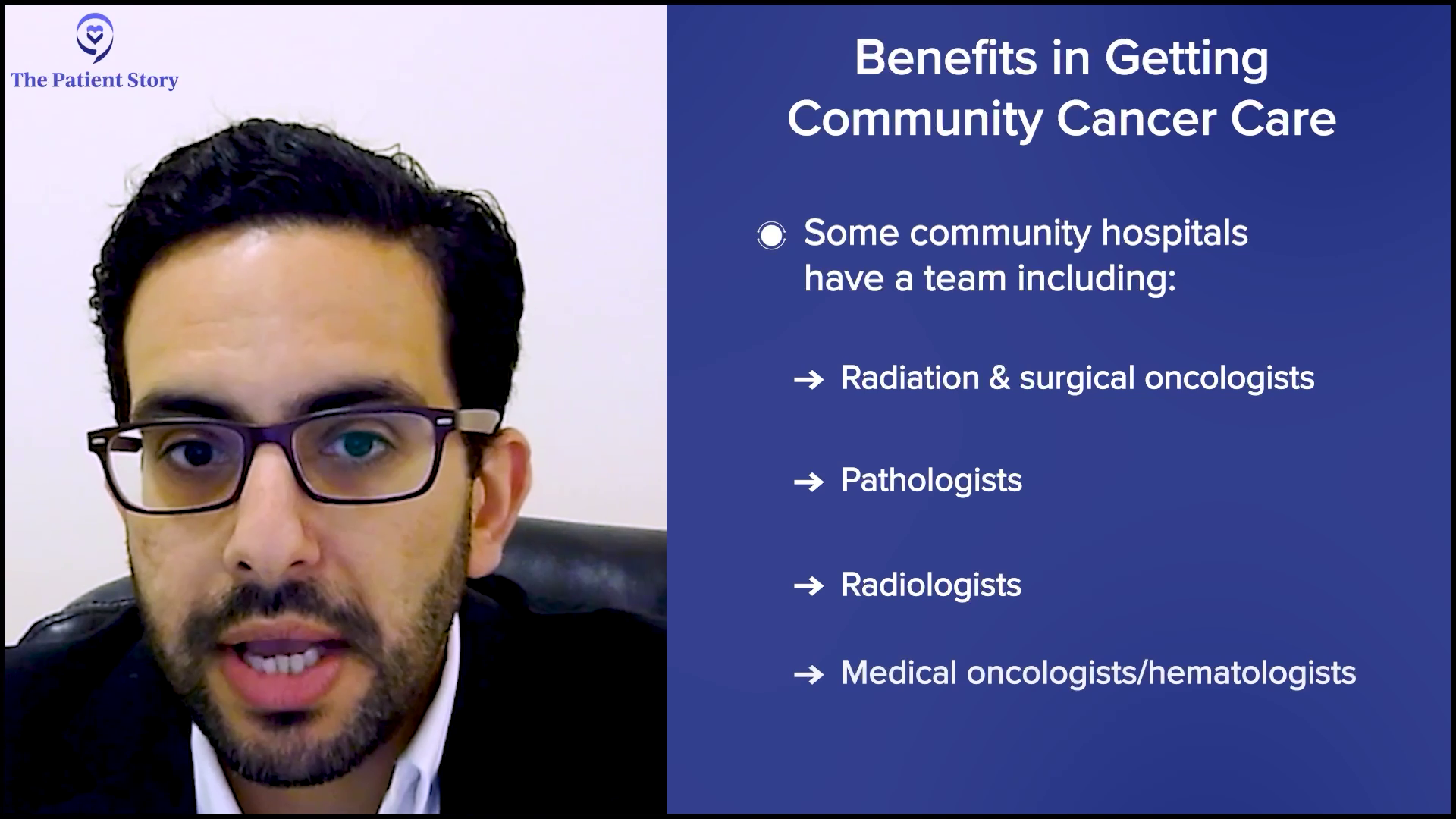
Our community cancer center is equipped with a multidisciplinary team, which is essential for providing comprehensive care. We have radiation oncologists, surgical oncologists, pathologists, radiologists, and medical hematologist-oncologists all working together. We regularly hold tumor boards where complex cases are discussed collaboratively, ensuring that multiple expert opinions shape each patient’s care plan.

For disease sites where we may not have a dedicated tumor board locally, we seamlessly collaborate with our main cancer center to ensure every patient benefits from the collective expertise. Even though patients are receiving care in a local familiar setting, they’re still getting the benefit of a specialized collaborative treatment. It’s not one doctor in isolation. It’s a coordinated team effort to provide the best possible outcomes. For many patients, this combination of high-quality care and the comfort of being treated closer to home is honestly the ideal scenario.
Maria: We offer also procedures in the clinic setting for those who are a little frightened to be in a hospital setting, like bone marrow biopsies. We have very skilled, qualified staff to assist Dr. Eltoukhy and we’re able to do those right in an office setting, which is helpful for patients who have that fear of going to the hospital.
We’re conveniently located right on the same campus as the Community Medical Center, so knowing that the hospital is close by is very comforting and convenient for our patients. The building that we’re in is comprised of oncology-based physicians, so it’s a one-stop shop as well and all of the doctors collaborate with Dr. Eltoukhy.
Pete: It’s great. That does sound like you have an ideal environment.
Financial Benefit of Going to a Community Provider
Pete: No offense, but people tend to think less of a community-based hospital when you’re providing the same quality of care as if they went directly to a university-based hospital. But then on the flip side, is there a cost savings for the patient for going the community-based hospital route? They’re getting the same standard of care, but is it more affordable for certain patients to do that?
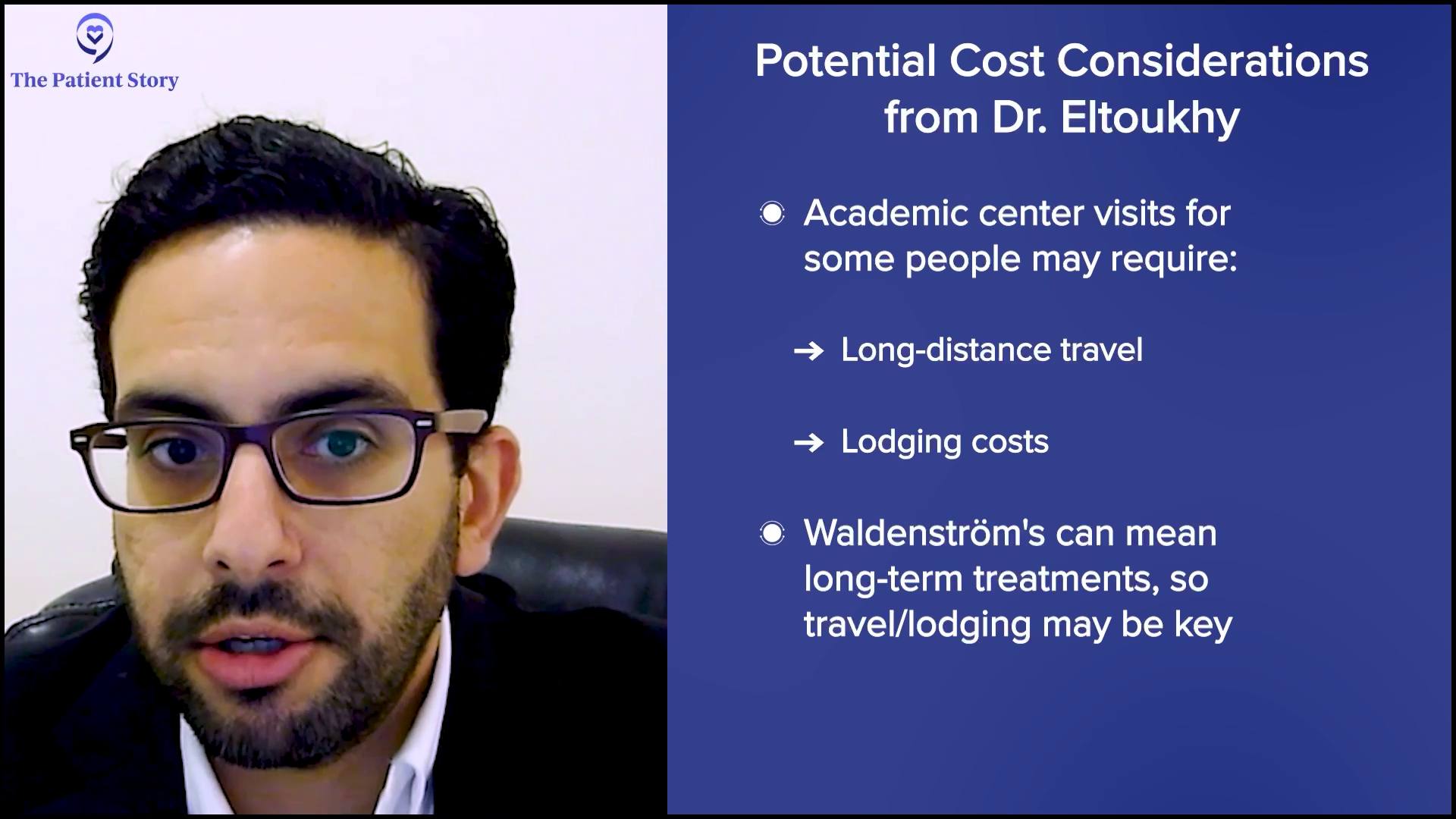
Dr. Eltoukhy: I do think so. Care at a community hospital can be often more affordable and accessible for patients and that’s an important factor when considering treatment options. One of the biggest advantages is the reduced financial burden related to travel and lodging. When patients are treated closer to home, they don’t have to worry about the added expense of traveling long distances, taking extended time off work, or even arranging accommodations closer to a larger academic center. This alone can make a significant difference, especially for patients undergoing long-term treatments, such as patients who have Waldenström’s.
From a healthcare cost perspective, community hospitals can also offer more cost-effective care without compromising quality. Administrative and operational costs tend to be lower in the community setting and that can translate into lower out-of-pocket expenses for patients. Additionally, treatments and services provided locally often come with fewer facility fees compared to larger institutions.
Another important factor to consider is insurance coverage. Community hospitals are typically well-integrated with the local insurance networks, which makes it easier for patients to access care that is covered under their plan. This can help minimize unexpected medical bills or any out-of-network charges that might arise when seeking treatment at larger, more specialized centers.
From a healthcare cost perspective, community hospitals can also offer more cost-effective care without compromising quality.
Dr. Hussam Eltoukhy
Ultimately, by offering high-quality comprehensive care in a local setting, community hospitals provide patients with financial and logistical advantages, and this accessibility ensures that patients can focus on their treatment and recovery without the added extra stress of significant financial strain.
Pete: I was having significant issues early on. Because of my insurance and health situation, I had to decide whether I should go out of state for the next level of care to resolve my issues at the time. Fortunately, what’s in place is if it becomes serious enough, you have a very good support network in your local community hospital, but you can reach out for a second opinion to centers of excellence and that’s important for people to understand. You don’t have to travel, especially if you can’t do it physically because of your health situation. The resources are there. You just have to work with your medical staff and coordinate that.
Monitoring Waldenström’s Patients on Watch and Wait
Pete: From your perspective and your experience, what are key considerations in monitoring disease activity for patients who are on a watch-and-wait status? How often do you follow up with them? What do you typically do in your practice?
Dr. Eltoukhy: For patients with Waldenström’s who are on a watch-and-wait approach, regular monitoring is essential. This strategy is common because many patients are asymptomatic at diagnosis or have very slowly progressive disease. This disease usually doesn’t require immediate treatment. However, just because treatment isn’t starting right away doesn’t mean the disease isn’t being closely managed.
In my practice, follow-up appointments typically occur every three to six months, depending on the patient’s specific situation and how stable their condition is. During these visits, we focus on clinical assessments and laboratory monitoring. We look at hemoglobin levels to monitor for anemia. We monitor IgM levels to track monoclonal protein. We check serum viscosity if there are any symptoms suggestive of hyperviscosity.
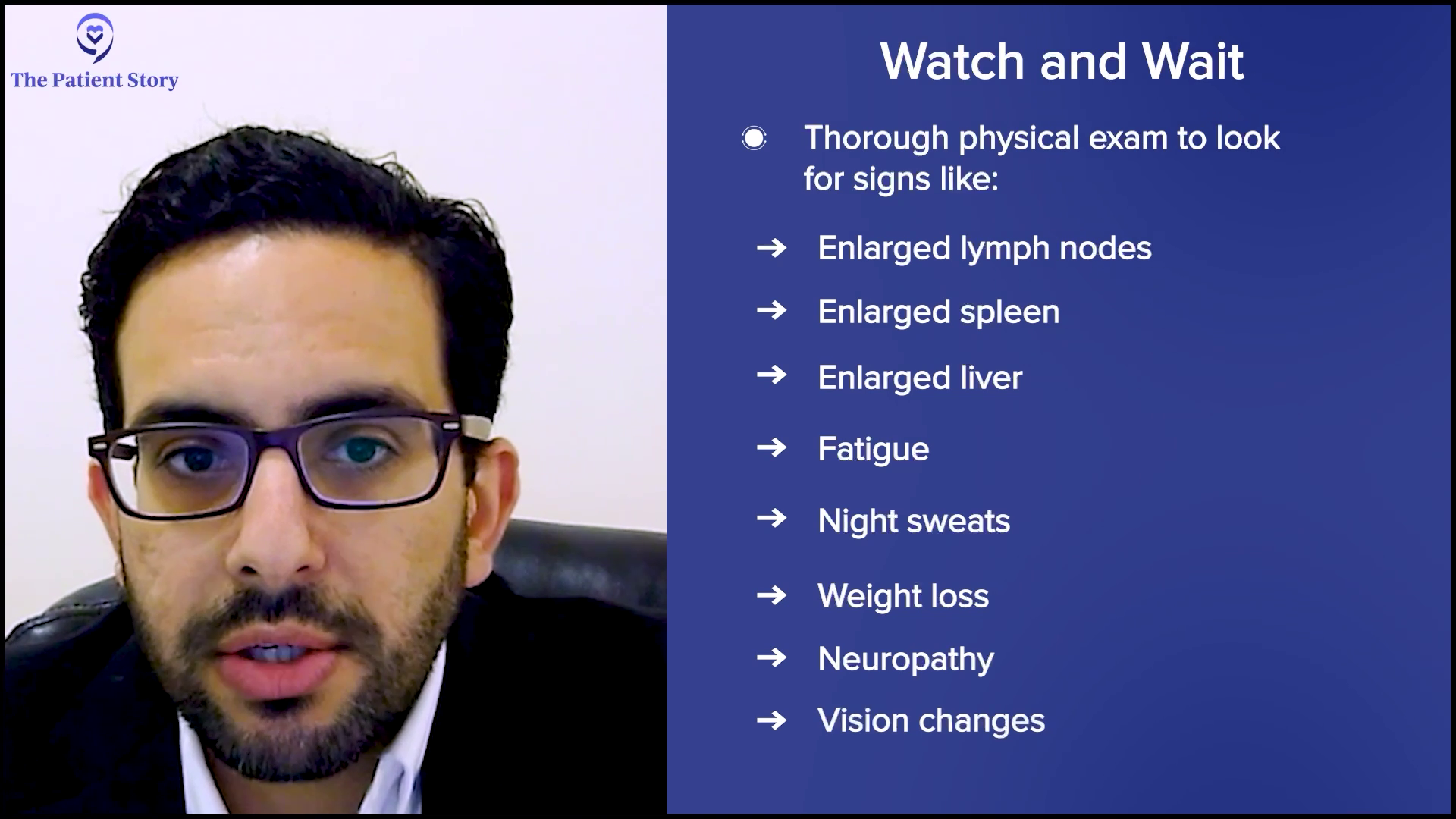
We also check kidney function, calcium levels, and assess for any signs of organ involvement. A thorough physical exam is equally important. I look for signs like enlarged lymph nodes, enlarged spleen, enlarged liver, and ask about any new or worsening symptoms, like fatigue, night sweats, weight loss, neuropathy, or changes in vision that could signal disease progression.
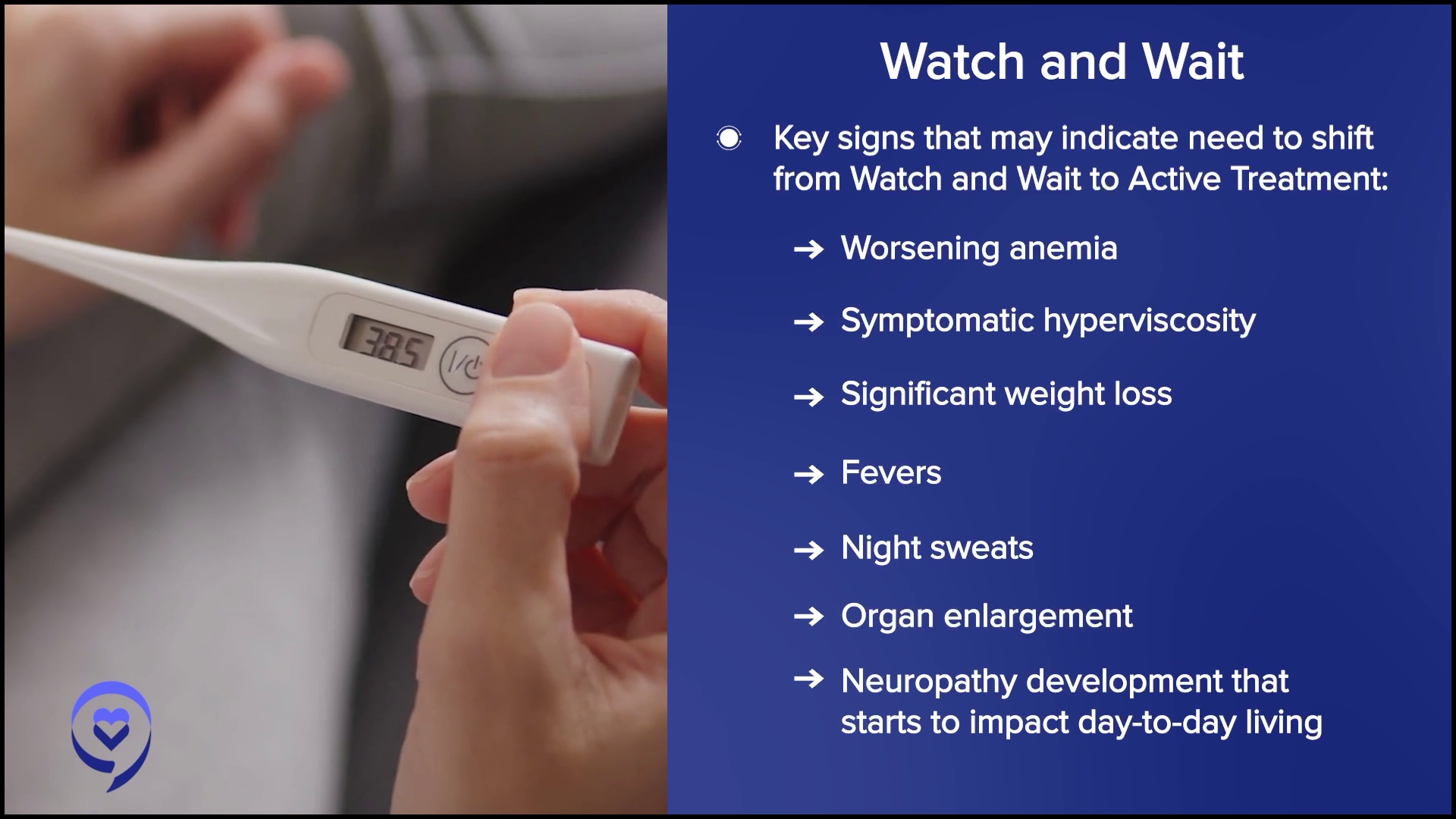
Key signs that might indicate a need to move from watchful waiting to active treatment usually include worsening anemia, symptomatic hyperviscosity, significant weight loss, fevers, night sweats, organ enlargement, or the development of any kind of neuropathy that would affect your daily life. If any of these arise, we reassess and discuss the treatment options.

In addition to monitoring, I always like to emphasize the importance of maintaining a healthy lifestyle. Staying active, eating a balanced, healthy, and whole foods diet, and managing other health conditions, like high blood pressure or diabetes, can improve overall well-being and help patients feel more in control of their health.
Emotional support is also very important as living with chronic conditions like Waldenström’s, even in a watch-and-wait phase, can be stressful. Regular follow-ups not only track disease activity but also provide reassurance and a structured plan for managing the condition over time.
The watch-and-wait approach is not about doing nothing. It’s more of a proactive strategy based on solid data and extensive clinical experience.
Dr. Hussam Eltoukhy
Pete: Could you talk a little bit more about the emotional and psychological challenges in that aspect? How do you help a patient navigate through that part of having the disease?
Dr. Eltoukhy: Living with a chronic condition like Waldenström’s, especially under our watch-and-wait approach, can be emotionally challenging for many patients. There’s this uncertainty of knowing you have a cancer diagnosis but not needing immediate treatment. Many patients will relay that it creates a lot of anxiety and stress. It’s completely natural to feel this way, but there are several strategies that we try to do to help patients cope with this.
I try to emphasize that it’s important to remember that the watch-and-wait approach is not about doing nothing. It’s more of a proactive strategy based on solid data and extensive clinical experience. If we recommend monitoring rather than immediate treatment, it’s because we know from research and patient outcomes that this is the safest and most effective approach for certain cases. Sometimes, if you explain it to them this way, it can help alleviate some of this uncertainty and fear.
That said, managing the emotional side of this journey is as important. Stress management techniques like mindfulness meditation and deep breathing exercises can help reduce day-to-day anxiety. Regular physical activity is also excellent, even doing something as simple as walking, which I always advocate for my patients. If you ask any of my patients, I tell them, “Do you track your steps daily? If not, you should start tracking and start increasing.”
Start with small goals and try to work your way up. If you can get that to 10,000 steps, great, but start somewhere, even if it’s at a lower number. Increasing physical activity can have a profound impact on mental health by improving mood and reducing stress. I’ve seen it with my patients. I’ve had patients who have done this and say their energy level has increased.
By focusing on physical health and emotional well-being, patients can live full, active lives while feeling confident that their condition is being closely monitored.
Dr. Hussam Eltoukhy
Support groups are also important. They can be very valuable whether they’re in person or online. Connecting with others who are going through the same experience can provide a sense of community and shared understanding. It helps to know that you’re not alone in navigating these emotional ups and downs. Counseling or speaking with a mental health professional can also be very helpful. They can provide tools to manage anxiety and cope with uncertainty.
It’s very important to emphasize to patients the importance of staying connected with their loved ones. Family and friends can be an essential support system, offering emotional comfort and practical help when needed. Maintaining a positive outlook doesn’t mean ignoring the challenges but trying to focus on what’s in your control. Staying active, attending regular follow-ups, and trying to lead a fulfilling life despite having a diagnosis.
Ultimately, while the watch-and-wait approach can feel uncertain, it’s grounded in strong evidence and a deep understanding of the way Waldenström’s progresses and acts. By focusing on physical health and emotional well-being, patients can live full, active lives while feeling confident that their condition is being closely monitored. At RWJBarnabas, we offer many support groups and have a regular monthly calendar that we offer to patients.
Maria: As the supportive team to the provider and the patient, we do our best so that the patient doesn’t have to worry about anything as far as authorizations or appointments. We educate them on all of that because those can be also very stressful for them. We try to take all of that away from them so they can focus on their health.
However, we also use the resources that are on campus. There are plenty of groups, like Dr. Eltoukhy said. We also have resources that include dietary and social work that we can refer these patients to and support them.
The staff here is kind and empathetic and treats patients like family. They know that they can call us if they’re scared and we don’t rush them. They know if something happens or they’re having a little symptom in between, they can call, they will receive a callback, and we will take the time to listen and report it to Dr. Eltoukhy, who will then follow up. They know that even though there is a bit of a wait, they can reach out to us at any time.
We do our best so that the patient doesn’t have to worry about anything… so they can focus on their health.
Maria Lamantia
Pete: That’s great. Thank you to both of you. You touched on many aspects, much more than I even anticipated. Your advice is very sound and your practice is amazing and commendable. I know from personal experience that a lot of the things that you mentioned are important in helping a patient navigate through not only the physical health aspects but also the mental health aspects of dealing with the disease and living with a chronic illness.
I go to my local hospital. I take notice of what services they provide and if they have any special programs coming up, I take advantage of them. I’m deeply involved in volunteering for the IWMF, but they help me immensely. It’s always important whatever cancer you have to try and get together with patients who have similar cancers to learn from each other and share stories. There’s a healing aspect in sharing and understanding what someone else has gone through and the IWMF provides that capability.
The IWMF has support groups and affiliates all around the world that help patients. We have a weekly newsletter, online discussion groups, webinars, and an annual education forum. We answer any questions patients, their caregivers, or their family members may have at any point in time.
I encourage people to visit IWMF.com and check out their services. It’s an extra level of care that you can get besides what you’re getting from a very caring hematologist-oncologist and a very caring staff who works with them. I can’t speak highly enough of the very qualified medical community and medical staff and the IWMF. When you put those two together, you’re in very good hands.
How Waldenström’s Patients Should Talk to Their Healthcare Team About Their Symptoms
Pete: Another thing that comes up, especially when you’re dealing with a disease that is chronic and you’re in a watch-and-wait period, is odd manifestations that you think is the disease. How should a patient communicate those symptoms? Should they say something or not say something? What’s your advice for communicating any symptoms to their healthcare team?
Dr. Eltoukhy: Effective communication with your healthcare team is crucial when managing a condition like Waldenström’s, especially if you’re on a watch-and-wait approach. One of the most important things patients can do is to promptly report any new or worsening symptoms. You don’t have to wait for your next scheduled appointment, whether it’s in three or six months. I end every single visit with my patients by telling them that if anything comes up before the next appointment, they should call and come in. I don’t say that to fill in the gaps. I tell the patients over and over again, “Do not wait. Come in.”
Effective communication with your healthcare team is crucial when managing a condition like Waldenström’s.
Dr. Hussam Eltoukhy
It’s important for patients to understand that and to know that they can reach out to their doctor. You don’t have to wait. You’re not bothering anyone. We want you to do that. We want you to come in. I want to know if anything is going on because we want to catch some of these symptoms like hyperviscosity very early. Don’t wait. Call your team. If you can’t see the doctor, see one of their colleagues or their nurse practitioner. If something feels different or concerning, reach out right away. That’s what we’re here for.
Keeping a symptom diary can be a very helpful tool. By tracking how you feel on a daily or weekly basis, you can start to identify patterns or changes over time that might not be obvious at the moment. Note things like fatigue levels, changes in weight, night sweats, any new pains anywhere, or any new neurological symptoms like numbness or tingling. Detailed information can give your doctor and the rest of your team a clearer picture of what’s happening and can help guide decisions about whether it’s time to adjust your plan.
Listening to your body and trusting your instincts is also key. No one knows your body better than you. If your gut is telling you that something isn’t right, whether it’s a new symptom or a shift in how you’re feeling overall, it’s important to speak up. You’re not bothering anybody. No one’s going to think otherwise.
Your healthcare team is your partner on this journey. Open and ongoing communication ensures that we can address concerns early and adjust care as needed.
Dr. Hussam Eltoukhy
What’s the worst-case scenario? It wasn’t caused by Waldenström’s. As a patient, don’t think anything of it. We want you to tell us all the new symptoms. We want to know what’s going on because we’re here to help the patient.
Sometimes, subtle changes can signal that it’s time to reassess and take a different plan. If you were on the cusp of considering treatment, maybe it’s time to consider it or not consider it. Remember that your healthcare team is your partner on this journey. Open and ongoing communication ensures that we can address concerns early and adjust care as needed. Once again, don’t hesitate to reach out. This is why we’re here. We’re here to support you every step of the way.
Clinical Trials for Waldenström’s Patients
Pete: You mentioned that even in the community hospital setting, you participate in clinical trials. Are clinical trials being conducted in your setting? What kind of trials do you have your patients participating in?
Dr. Eltoukhy: Across all cancers, we currently have over 60 clinical trials available at our community cancer center, including many for hematologic malignancies. We offer phase 2 and phase 3 clinical trials. We’re not able to offer phase 1 clinical trials at this time.
Offering clinical trials in a community setting is a great way to provide patients with access to cutting-edge treatment without requiring them to travel to larger academic centers. When determining the feasibility of conducting trials in our center, one of the biggest considerations that we look at is resources. It’s not just about having the physical space or the equipment. We need to ensure that we have the right personnel and infrastructure in place to manage trials safely and effectively. This includes dedicated research coordinators, nurses, pharmacists, and regulatory staff who are trained in clinical trial protocols and patient safety.
Our goal is to offer trials that are not only scientifically valuable but also feasible and safe to administer in the community setting.
Dr. Hussam Eltoukhy
Clinical trials in the US are very heavily regulated and rightfully so. There are strict guidelines and oversight to ensure that every trial is conducted ethically, that patient safety is the top priority, and that data is collected accurately. We have to assess whether we can meet all those requirements from patient monitoring to data reporting while maintaining the highest standard of care.
Ultimately, our goal is to offer trials that are not only scientifically valuable but also feasible and safe to administer in the community setting. We want to make sure patients have access to innovative treatments while receiving the same level of care and oversight that they would expect from one of these larger academic centers.
Different Phases of Clinical Trials
Pete: For those who aren’t as knowledgeable about clinical trials, can you do a quick overview of the different phases of clinical trials?
Dr. Eltoukhy: Phase 1 is when a new drug starts to be administered. Once you move on to phase 2, you have already determined the safety of the drug and you’re starting to look at efficacy and how it could work. Once you move on to phase 3, you have a better understanding of how well it works and how safe it is, and you’re looking at a broader approach and getting the real data on efficacy and how well it works.
A phase 4 clinical trial is always ongoing. Any drug that’s out there is always being monitored to make sure that it continues to be safe because safety doesn’t end after phase 1 or phase 2. Safety is ongoing. In phase 1, they’re new drugs that need very close monitoring and you could have unexpected side effects. We don’t quite partake in phase 1 trials right now, but we have many phase 2 and phase 3 trials.
Busting Clinical Trial Myths
Pete: In a community clinical team, what can you do to ensure patients will learn about clinical trial options and whether they should be concerned about the potential side effects of being in a clinical trial? Am I going to be worse off by doing that or not? How do you educate them? How do they find out about the clinical trials?
Dr. Eltoukhy: That’s a very common concern. Ensuring patients learn about and understand clinical trial options starts with the clinical team, especially the physician. Physicians should take an active role in discussing these opportunities directly with the patients.
When I open a clinical trial at our community center, it’s because I believe it has the potential to benefit the patients. But offering a trial isn’t enough. We have to make sure that patients understand, are fully informed, and are comfortable with their options. For me, that means sitting down with each patient and having an open, honest conversation.
The right choice for one patient isn’t necessarily the best for another patient. It’s essential to personalize the discussion based on the patient’s health status, personal preferences, and lifestyle.
Dr. Hussam Eltoukhy
I explain what we can offer under the standard of care, what treatments are currently approved and routinely used, and lay out what the clinical trials could provide. I go through the potential benefits, the goals of the study, and also any limitations or uncertainties. Patients must understand not just the possibilities but also the risks and the level of commitment involved.
One of the most critical aspects of these conversations is avoiding bias. My role isn’t to push a patient toward one option or another but to provide them with all the necessary information to make an educated, confident decision. What might be the right choice for one patient isn’t necessarily the best for another patient. It’s essential to personalize the discussion based on the patient’s health status, personal preferences, and lifestyle.
Ultimately, patients should feel empowered to choose the path that’s best for them, whether that’s enrolling in a clinical trial or sticking with the standard of care. By fostering clear, transparent communication, we try to help patients navigate their options and ensure that they’re making decisions that align with their goals and values.
Our goal is to offer as many trial opportunities as we can in our setting but also to recognize when a referral is necessary for something more specialized.
Dr. Hussam Eltoukhy
Bringing Waldenström’s Clinical Trials to the Community Cancer Care Site
Pete: From a perspective of trying to make sure that your patients are aware of these clinical trials and wanting them to take advantage of them if it’s in their best interest, how do you ensure that they have access to the latest trials? How does it work for your hospital system to get involved in a clinical trial, especially for Waldenström’s patients? Do you seek them out yourself or are you approached by the people who are running the trial? How does the process work?
Dr. Eltoukhy: We recognize the importance of staying connected with larger academic centers that may offer these opportunities. A lot of times, we will open trials collaboratively with the Rutgers Cancer Institute. One of the key roles of community medical centers is to understand where we fit within the broader healthcare system. It’s not a one-size-fits-all approach. We need to be very clear about what we can effectively manage in our setting and when it’s in the patient’s best interest to refer them to an academic center for a clinical trial or more specialized treatment.
Once again, it’s not about limitations in expertise. It’s about ensuring patients receive the best possible care whether that’s locally or through a specialized trial at an academic center. Of course, whenever possible, we want to provide that care closer to home. It’s more comfortable, more cost-effective, and less burdensome. Traveling long distances to participate in a clinical trial can be incredibly challenging, especially when dealing with the physical and emotional toll of cancer care.
High-quality cancer care isn’t limited to large academic centers. Community hospitals like ours play a vital role in delivering comprehensive, patient-centered care that’s accessible, effective, and personalized.
Dr. Hussam Eltoukhy
Our goal is to offer as many trial opportunities as we can in our setting but also to recognize when a referral is necessary for something more specialized. Effective collaboration means maintaining strong communication with the academic center, letting them know what trials we have open, what we can manage, and as importantly, what we can’t. By advocating for our patients and fostering these partnerships, we’ve been able to create a seamless system where patients benefit from the convenience of local care and innovations of cutting-edge research when needed. It’s about working together to make sure patients have access to the best options, wherever they may be.
Pete: The IWMF, through the efforts of Dr. Jorge Castillo at Dana-Farber, has established the WM-NET, which is designed to become a network of hospitals across the United States that will participate collectively in clinical trials and have them at their sites. Not all of the participating organizations are going to do all of the trials, but they will try and distribute it more broadly to make it easier for patients to get access to these trials locally rather than having to travel to a major cancer center.

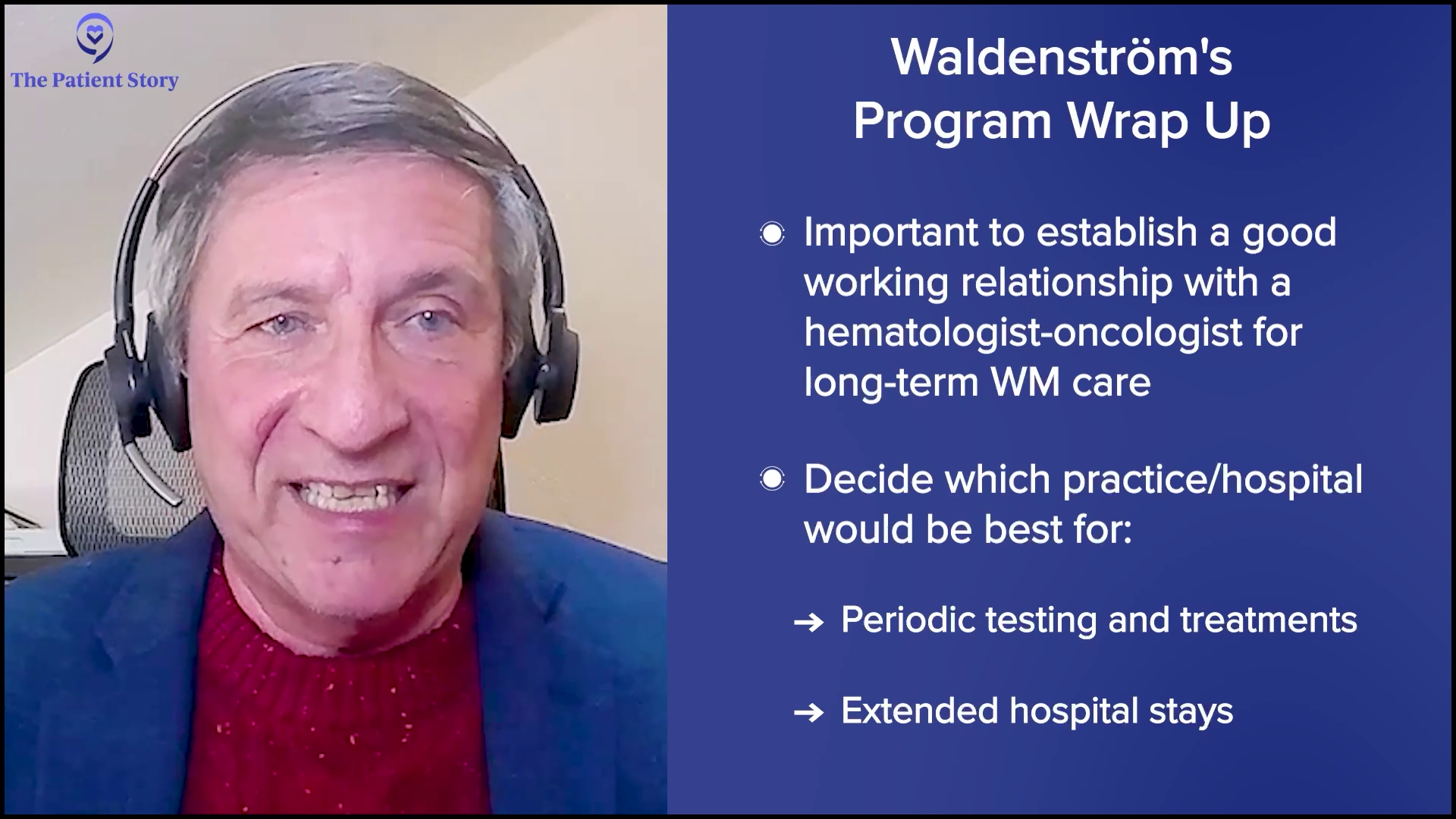
Final Takeaways
Pete: Thank you, Dr. Eltoukhy and Maria, for your time and perspective on providing care to Waldenström’s patients in your hospital setting and community-based hospitals. Do you have any final remarks you want to pass along to Waldenström’s patients?
Maria: It would be an honor to treat you and take care of you. Consider our establishment if you don’t want to go to the bigger facilities. It’s a more boutique-like atmosphere. If you come to see Dr. Eltoukhy, you will be in very good hands. It’s an honor to work alongside him.
At the end of the day, cancer care is a partnership between doctors and patients, between community hospitals and academic centers, and between healthcare teams and families.
Dr. Hussam Eltoukhy
Dr. Eltoukhy: Thank you so much for having me. It’s been a privilege to share my perspective on improving outcomes for patients with Waldenström’s, particularly within the community setting.
I hope it’s clear that high-quality cancer care isn’t limited to large academic centers. Community hospitals like ours play a vital role in delivering comprehensive, patient-centered care that’s accessible, effective, and personalized. Whether it’s through offering clinical trials, collaborating with larger academic centers, or simply being there for patients in their communities, the goal is always the same: to provide the best possible care tailored to each individual’s needs. It’s about open communication, staying informed, and making sure patients feel empowered and supported throughout their journey.
At the end of the day, cancer care is a partnership between doctors and patients, between community hospitals and academic centers, and between healthcare teams and families. By working together, we can ensure that every patient has access to the best treatments, latest research, and compassionate care that they deserve, no matter where they are. Thank you again for the opportunity to be part of this important conversation.
Pete: It’s been a pleasure speaking to both of you. I learned a lot and got a better appreciation, other than what I already have, of community care practitioners and the dedication and care they have, making sure that Waldenström’s patients are on the path to living healthier and fuller lives. You are instrumental in making sure that happens, so I commend both of you.
For Waldenström’s patients, caregivers, and families, it’s very important at the beginning to establish a good working relationship with a hematologist-oncologist who’s going to be managing your journey with Waldenström’s. It’s important to decide what practice or hospital setting you prefer to go to for periodic testing and treatments, or extended hospital stays if you should ever need them when you have some significant issues. All the doctors, nurses, physician assistants, medical staff, and clinical staff are to be commended for their commitment on a day-to-day basis to help all of us live fuller, healthier lives.
Establish a good working relationship with a hematologist-oncologist who’s going to be managing your journey with Waldenström’s.
Pete DeNardis
I want to encourage anyone around the world who’s affected by the disease to take advantage of opportunities that are out there to find the best local hospital systems that can cater to their needs but also to be involved with an organization devoted specifically to their disease, like the International Waldenström’s Macroglobulinemia Foundation. The IWMF is the only global organization dedicated specifically to the support, education, and research of Waldenström’s.
By becoming a part of the IWMF community, you would have access to weekly newsletters, quarterly publications, webinars, in-person patient forums, and support groups, all devoted specifically to Waldenström’s. The IWMF also has online discussion groups and social media support groups, so no matter where you are in the world, the IWMF will be there to help you. Visit IWMF.com.

Stephanie: Thank you so much to Pete, Dr. Eltoukhy, and Maria for providing such incredible context. Self-advocacy is vital, especially for Waldenström’s where having long-term care and long-term doctor-patient relationships are so important. Don’t be afraid to speak up for yourself and ask any questions that are coming up for you, whether you’re a patient or a care partner. The keyword that Dr. Eltoukhy kept talking about was partnership. It doesn’t have to be one place or the other, as long as the medical team is working in partnership with you.
We also want to thank again our sponsor, Pharmacyclics, an AbbVie company, for its support of our independent patient program. We would be remiss to forget shouting out our partners, The Leukemia & Lymphoma Society (LLS) and the International Waldenström’s Macroglobulinemia Foundation (IWMF). Visit their websites for more on these wonderful organizations and what they provide in terms of quality services for patients and care partners in Waldenström’s.
Thank you so much for joining our program. We hope that this was helpful for you and that you walk away with more knowledge and understanding and more questions. We hope to see you at another discussion. Take good care.

Thanks to The Leukemia & Lymphoma Society and International Waldenström’s Macroglobulinemia Foundation for their partnership.

Thank you to Pharmacyclics, an AbbVie company, for supporting our independent patient education content. The Patient Story retains full editorial control.
Waldenström’s Macroglobulinemia Programs
Waldenström’s Macroglobulinemia Patient Stories
...
Pete D., Waldenstrom Macroglobulinemia
Symptom: Irregular blood test results during a regular workup for Crohn’s
Treatments: Chemotherapy, surgery, radiation, monthly IVIG
...
Sheree N., Waldenstrom Macroglobulinemia
Symptom: Feeling anemic
Treatment: Chemotherapy (bendamustine & rituximab)
...