Clinical Trials Update
What to Know in Myelofibrosis Care
Edited by:
Katrina Villareal
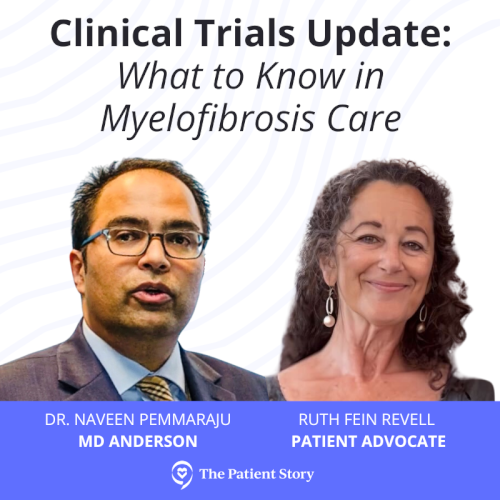
Following the American Society of Hematology Annual Meeting (ASH), Dr. Naveen Pemmaraju of MD Anderson and patient advocate Ruth Fein Revell discuss the latest myelofibrosis treatment options.
This interview has been edited for clarity and length. This is not medical advice. Please consult with your healthcare provider to make informed treatment decisions.
The views and opinions expressed in this interview do not necessarily reflect those of The Patient Story.
Introduction
Ruth Fein Revell, Patient Advocate
Ruth Fein Revell: Hi and welcome to our program, Clinical Trials Update: What to Know in Myelofibrosis Care. My name is Ruth Fein Revell and I’ve lived with a myeloproliferative neoplasm (MPN) for nearly 30 years.
I was diagnosed with essential thrombocythemia in 1995, polycythemia vera about 20 years later, and myelofibrosis in 2018. I’ve also lived with a number of complications from dangerous blood clots and hemorrhages that put me in the ICU to debilitating headaches, bone pain, and extreme fatigue.
I’m a health and science writer and very fortunate to be in a clinical trial for the last four years with amazing results, eliminating my symptoms, and significantly reducing my bone marrow.


We want to note that The Patient Story retains full editorial control of this entire program. This is not meant to be a substitute for medical advice.
Joining us is Dr. Naveen Pemmaraju, a top expert in MPNs and myelofibrosis from MD Anderson. Dr. Pemmaraju, it’s so nice to see you. Thanks for joining us and for being a part of this program. Can you tell us more about yourself and what drew you to MPNs?
Naveen Pemmaraju, MD
Dr. Naveen Pemmaraju: Thanks for having me. I’m a professor of leukemia at MD Anderson in Houston, Texas. I serve as the executive director for cancer medicine and as the director for our rare disease program, including blastic plasmacytoid dendritic cell neoplasm (BPDCN).
I am an expert in both clinical trial research and patient care for patients with MPNs, including myelofibrosis, polycythemia vera, essential thrombocythemia, and mastocytosis.
Ruth: It’s always great to see you and to speak to you. You offer so much to the MPN community and we really thank you.
JAK inhibitors are not JAK2 mutant-specific inhibitors, so that’s why they work in patients whether they’re JAK, MPL, CALR, triple-negative, or have no mutations.
Dr. Naveen Pemmaraju
Standard of Care: JAK Inhibitors
Ruth: We now have four JAK inhibitors and one one of them was just approved. Walk us through this. First of all, how does a JAK inhibitor work?
Dr. Pemmaraju: The basic premise is that MPN cells signal through a specific pathway called the JAK/STAT pathway.
A regular cell uses the JAK/STAT pathway for normal blood cell growth, differentiation, and lifespan. Now take an MPN cell and that pathway is hijacked and used in a malignant way, so those cells keep growing and dividing. It’s like a light switch that’s turned on that doesn’t go off.
Interestingly, the JAK inhibitors are not JAK2 mutant-specific inhibitors, so that’s why they work in patients whether they’re JAK, MPL, CALR, triple-negative, or have no mutations.
JAK inhibitors are based on the principle that the JAK/STAT pathway and the cells are overactive and not working properly. JAK inhibitors aim to block that malignant activity and restore normal growth.
Ruxolitinib was the first-ever approved JAK inhibitor. Since 2011, three JAK inhibitors have been US FDA-approved: fedratinib in 2019, pacritinib in 2022, and momelotinib in 2023. The four currently approved JAK inhibitors have some interesting similarities and differences.
[Ruxolitinib] works very quickly in relieving the symptom burden for our patients with MPNs.
Dr. Naveen Pemmaraju
Ruxolitinib
Dr. Pemmaraju: Ruxolitinib, the first and longest in class, is a JAK1/JAK2 inhibitor. This drug was simply amazing in the original clinical trials, which were COMFORT-I and COMFORT-II, led by Serge Verstovsek and Professor Claire Harrison.
In those studies, we learned a few things about ruxolitinib. One is that it works very quickly in relieving the symptom burden for our patients with MPNs. It can shrink the spleen rather quickly as well, so quickly that the hallmark ended up being at week 24 by six months.
Some side effects to look out for over time in this otherwise well-tolerated drug have been the development in some patients of opportunistic infections, such as herpes zoster or shingles, weight gain, and non-melanoma skin cancers.
Basal cell and squamous cell cancers of the skin are already common in our patient population, so a lot of our patients end up seeing a dermatologist. Most of our patients don’t necessarily discontinue for those side effects, but we need to watch out for them.
All patients who are going to get treated with fedratinib should have their thiamine level checked.
Dr. Naveen Pemmaraju
Fedratinib
Dr. Pemmaraju: Fedratinib improves symptoms and decreases spleen size, but it has a very notable toxicity or side effect, which garnered an FDA black box warning. It’s a very serious potential side effect called encephalopathy. Some have seen it to be Wernicke’s encephalopathy, but on later analysis, not exactly.
Wernicke’s encephalopathy is a name for a syndrome that can cause problems with thinking and even balance and can result from severe nutritional deficiencies. For fedratinib, it appears that it displaces vitamin B1 (thiamine) so what we see is the linking of those. All patients who are going to get treated with fedratinib should have their thiamine level checked because the encephalopathy can be related to that.
Patients can have GI side effects with fedratinib, like nausea, vomiting, and diarrhea, so we have to watch out for that, particularly in our older and more frail patients.
The unique thing with pacritinib is for several years, it was being watched for the development of cardiac and/or bleeding signals.
Dr. Naveen Pemmaraju
Pacritinib
Dr. Pemmaraju: Pacritinib is an interesting agent. Again, all these are trying to hit the JAK/STAT pathway, but this hits other pathways outside of that and that may be part of its benefits and toxicities.
It helps to shrink down the spleen and improve the symptom burden of patients, but the unique thing with pacritinib is for several years, it was being watched for the development of cardiac and/or bleeding signals.
I and others have done a lot of evaluation and analysis, including post-approval. We’re not seeing a high signal for that, but that’s something you have to be aware of if the patient is on a blood thinner, having chest pain, or having heart surgery.
Not only did [momelotinib] show improvement in the spleen size and symptoms, but what’s interesting — and pacritinib is showing this as well — is having an improvement in anemia.
Dr. Naveen Pemmaraju
Momelotinib
Dr. Pemmaraju: Momelotinib is the most recently approved JAK inhibitor. Again, not only did it show improvement in the spleen size and symptoms, but what’s interesting — and pacritinib is showing this as well — is having an improvement in anemia. Now that’s important.
Ruxolitinib and fedratinib don’t necessarily do that and, in some cases, it can make it transiently worse. Momelotinib has ACVR1 inhibition. Pacritinib also showing that as well unleashes a new era for our patients of JAK inhibitors having beneficial side effects, such as improvement of anemia and potentially, thrombocytopenia.
You have to watch out for GI side effects with fedratinib, pacritinib, and even momelotinib. In the earlier studies of momelotinib, there was a signal for peripheral neuropathy. I want to put those forward as an overview. There are some subtleties and differences, if one reads further.
Ruth: Thanks for that explanation. I’ve heard a lot of people say that they have a different mutation, so a JAK inhibitor isn’t going to help them, but we know that that’s not the case, so thanks for your explanation of how they work.
There isn’t a single molecular test. The decision is based on clinical factors and the art of medical decision-making.
Dr. Naveen Pemmaraju
Switching JAK Inhibitors
Ruth: How do you know which JAK inhibitor might or might not work and which one to try first? How is that decision made?
Dr. Pemmaraju: The decision to switch JAK inhibitors is not scientific. We’re not there yet. At some point, I envision that we’ll have a decision tree, like our colleagues in CML. But right now, there’s no molecular test, so it is the art of medicine. It is clinical decision-making.
There are some factors, if one looks up in the NCCN and other guidelines. One is platelet count. Ruxolitinib and fedratinib should be given to patients who have a certain amount of platelets and that’s where pacritinib was able to get its approval.
Pacritinib is specifically approved in the front-line setting for patients whose platelet count is less than 50, for example. The NCCN guidelines and other groups say that once you use pacritinib in later lines, maybe you don’t have to pay attention to the platelet as much, but that’s obviously for debate.
Another factor is the GI signal. If you have someone who has a known encephalopathy syndrome or thiamine deficiency, then fedratinib is not going to be one that you would choose.
Finally, you have to look at some of these subtle side effects that we mentioned earlier, such as GI and neuropathy, to help you choose.
The bottom line is there isn’t a single molecular test. The decision is based on clinical factors and the art of medical decision-making.
Switching can have financial cost repercussions, new toxicities when a patient was otherwise doing ‘okay,’ problems with access to the drug, and could uncover idiosyncratic side effects that may be specific to that patient and weren’t seen in the studies.
Dr. Naveen Pemmaraju
Ruth: So it’s possible that somebody could start on one JAK inhibitor and at some point switch to another. Is that an issue if you change?
Dr. Pemmaraju: This is a great important point about switching JAK inhibitors and what are the indications. There are several buckets here.
First is clear disease progression in terms of the spleen. If you have a patient who’s been on a certain JAK inhibitor for a sufficient amount of time and you have a spleen that previously shrunk but now starting to rise again, that could be considered disease progression and an indication to switch.
Second is worsening MPN symptom burden to the point where the patient’s quality of life is affected.
Third is blast count, peripheral blasts or bone marrow blasts, going up.
Fourth is the progression of the disease to an outright higher level of disease, what we call an accelerated blast phase.
The development of these clinical factors, such as the platelet count, may matter if you have a patient who’s on ruxolitinib, for example, and you consistently have platelets below 50, then that’s an indication to switch, for example, to pacritinib. If you have a patient who has anemia, you may think about momelotinib.
These are some of the reasons to think about switching. But again, there isn’t a molecular test or a definitive moment to switch. Switching can have financial cost repercussions, new toxicities when a patient was otherwise doing “okay,” problems with access to the drug, and could uncover idiosyncratic side effects that may be specific to that patient and weren’t seen in the studies.
Finally, you have a question about withdrawal and overlap, so these are things I think we’ll all work out together over the coming years as we have these JAK inhibitors in the clinic.
The story of JAK inhibitors is an evolving story and it’s evolving at three levels.
First is the science of it alone. In 2005, I was at Johns Hopkins with Alison Moliterno and Jerry Spivak, and I remember the day that the JAK2 mutation V617F was elucidated. From that time to now, we have JAK inhibitors that are amazing, so science is still evolving.
Second is the clinical part, as we’ve discussed. When to switch, how to switch, what are the factors, etc.
Third is the future. How do we combine these drugs with a second agent and potentially a third agent? What are those cross-reactivities? How does that benefit the patient to start those upfront rather than later on? You have this evolving area that’s quite exciting but also quite daunting not only for the patients and the clinic but for researchers.
This is preliminary data, but it was so encouraging that they are now moving on to a phase 3 randomized global study.
Dr. Naveen Pemmaraju
Clinical Trials: Combination Therapy
Selinexor & Ruxolitinib
Ruth: We’re seeing some really exciting updates as far as combination therapy. Let’s talk about clinical trials, starting with selinexor plus a JAK inhibitor and then move on to other combinations.
Dr. Pemmaraju: At ASH 2023, Dr. Sri Tantravahi from Utah presented the first public data of front-line combination, updated I should say, of selinexor with ruxolitinib. This is untreated patients with myelofibrosis, intermediate to high risk, who were given the combination rather than ruxolitinib, which would be considered the standard or JAK inhibitor.
Although it was early on and only a few patients, very surprisingly and amazingly, the group showed that there’s a high rate of activity in spleens being reduced as well as symptom burden being increased.
Now, this is preliminary data, but it was so encouraging that they are now moving on to a phase 3 randomized global study. The combination selinexor-ruxolitinib, so the XPO1 inhibitor plus JAK inhibitor, versus JAK inhibitor alone. Those data will be eagerly awaited.
This is also, if I may say, a fascinating study.
Dr. Naveen Pemmaraju
Navitoclax & Ruxolitinib
Ruth: What about the BCL inhibitor navitoclax?
Dr. Pemmaraju: A second combination is that of the BCL-XL inhibitor navitoclax with ruxolitinib, which I presented as an oral presentation at ASH on behalf of my colleagues. This is also, if I may say, a fascinating study.
We globally enrolled 252 patients into a randomized, double-blind, placebo-controlled study of ruxolitinib plus navitoclax, which is not yet approved for any indication, versus ruxolitinib alone. Again, we had intermediate to high-risk patients, around 80-plus percent of intermediate-2 patients.
What we found is a very outstanding rate of 60-plus percent of patients in the combination arm having an SVR35 at week 24, so spleen volume reduction of 35% or more, versus only 30-plus percent in the control arm, which was ruxolitinib alone. The waterfall plot showed that almost all patients benefited from the combination.
In terms of statistical analysis, the primary endpoint of spleen reduction was met with a high statistical significance, but the symptom burden difference was not yet found to be statistically significant. Both groups had reductions, so there was a numerical reduction of the symptoms in both the combination and the ruxolitinib alone, but there was no statistical difference.
The study is ongoing for collecting for maturity and overall survival duration, so this was a preliminary presentation at 15 months follow-up. We’ll stay tuned to see how it gets updated over the next congresses.
Great safety, but you have to watch out for thrombocytopenia, which is low platelets, and watch for that signal very closely.
Luspatercept & Ruxolitinib
Ruth: Another combination being investigated is the use of a shot called luspatercept to boost hemoglobin or fight anemia, and that also is being used with ruxolitinib. Can you tell us more about that one?
Dr. Pemmaraju: Luspatercept is a fascinating molecule. It’s already FDA-approved in the myelodysplastic syndrome setting. In the MPN setting, we think it has a similar activity to improve hemoglobin and anemia, which is an urgent, unmet medical need.
The initial studies have shown positive data, which is either luspatercept by itself, usually given every three weeks, or in combination with the JAK inhibitor ruxolitinib. Those studies are ongoing and we eagerly await those results in the coming year or two.
When the group looked back at certain subsets, including the intermediate-1 patients and others, it appeared that there was a benefit in both spleen size and symptoms.
Dr. Naveen Pemmaraju
Pelabresib & Ruxolitinib
Ruth: We’ve also had the MANIFEST trial, which is the trial that I happen to have been on for the last four years, and that’s a different drug, s pelabresib. Could you talk about that combination and what you think the potential is?
Dr. Pemmaraju: Another exciting combination presented at ASH 2023 was that of the MANIFEST-2, which is ruxolitinib plus a new agent pelabresib, a bromodomain or BET inhibitor, which is not yet FDA-approved for any indication.
This encouraging data set was presented by Dr. Raajit Rampal from Memorial Sloan Kettering. It’s the second-largest study ever conducted in the myelofibrosis front-line space, which included 430 patients. They also randomized ruxolitinib-pelabresib versus ruxolitinib alone in the control, mostly intermediate-1 to intermediate-2 patients, so a slightly different population.
They showed a very similar profile. A highly statistically significant primary endpoint was met, which is SVR35 at week 24. The symptoms in all comers, although showing a numerical decrease in both groups, did not quite meet statistical significance.
When the group looked back at certain subsets, including the intermediate-1 patients and others, it appeared that there was a benefit in both spleen size and symptoms.
The supposition is the same as navitoclax. These two are the first ever in our field, resulting in phase 3 global, double-blind, placebo-controlled, front-line, untreated myelofibrosis patients with a novel combination of pelabresib and navitoclax, neither of which are FDA-approved for any indication.
I would say my editorial comment is super exciting for the field that we even did it. Both were international studies largely conducted during the pandemic and involved lots of patients and investigators.
The primary endpoint was met for both of them. The symptoms were not quite met in either study in terms of statistical significance so the question asked is three-fold.
What is the utility of following the symptom burden scale in combination studies, something that was designed 15 years ago for a single-agent JAK inhibitor?
Do we expect a combination to improve symptoms over ruxolitinib alone, or because you’re introducing a second drug, you’re going to introduce new toxicity?
On behalf of my colleagues, maybe it’s time to reevaluate: what are the endpoints for our patients with myelofibrosis? Perhaps in addition to reducing spleen size and improving symptoms, we should be factoring in overall survival, progression-free survival, and bridging to stem cell transplant. This is the time to talk about it because these combination studies are difficult, if not impossible, to judge based on the COMFORT-I and COMFORT-II studies.
Imetelstat is in an ongoing phase 3 trial, which is in the second-line setting and beyond, against the best available therapy (BAT).
Dr. Naveen Pemmaraju
Telomerase Inhibitors
Ruth: Let’s go beyond JAK inhibitors. There are other drugs being studied. Can you help us understand other approaches?
Dr. Pemmaraju: There’s an exciting alphabet soup of clinical trials and drug molecules out there. It’s exciting for our patients to know that there are people around the world who care about MPNs, so it’s good to know that despite COVID, we have a lot of innovation.
We’re adding a new trial once a week, so it’s almost impossible to keep up, but I do want to give some sampling of what’s going on.
Imetelstat is very important for everyone to know. It’s a first-in-class telomerase inhibitor. Some people have heard of telomeres. They are the little ends on the ends of chromosomes that help to determine aging and possibly even cancer biology.
Imetelstat is in an ongoing phase 3 trial, which is in the second-line setting and beyond, against the best available therapy (BAT). I praised this trial because it’s the first and, to my knowledge, only phase 3 trial that has overall survival as its primary endpoint. Hopefully, it will give us a readout in the next year or two.
MDM2 Inhibitors
Dr. Pemmaraju: MDM2 inhibitors have gotten a lot of press in all MPNs. This is a key pathway that has to do with guarding the cell TP53. It’s an oral drug that has been studied before. As a class of drugs, there may be some GI side effects to watch out for, but in the later trials we’ve seen, the groups have figured out a way to address that by either adjusting the dosing schedule or dosing frequency.
I’m excited to see where that area goes. Right now, the lead trials are MDM2 inhibitors with ruxolitinib as an add-on approach or a suboptimal approach. You’re already on a JAK inhibitor. You have an okay response, not a great one, but not quite ready to come off of it, and then you add the MDM2 inhibitor. Those studies are actively ongoing and I think we’ll be excited to see those results.
The good thing about myelofibrosis is whether you’re JAK, CALR, MPL, or triple negative, you respond to JAK inhibitors and novel agents alike.
Dr. Naveen Pemmaraju
Genetic Mutations in Myelofibrosis
Ruth: What if someone’s myelofibrosis isn’t driven by a JAK mutation but a different mutation, is there a different approach? We’ve also been hearing about a cancer vaccine related to CALR, so could you walk us through both?
Dr. Pemmaraju: There’s a two-part answer to the question of molecular mutation targeting in MPNs. Historically and in the clinic right now, there is no difference at the moment.
The good thing about myelofibrosis is whether you’re JAK, CALR, MPL, or triple negative, you respond to JAK inhibitors and novel agents alike. That’s an interesting thing that suggests that there’s a common pathway.
But for the future, yes. Already in the clinic in 2024, we expect a new era to begin, which is, for the first time, to have mutant-specific approaches for both JAK2 and CALR. I expect that we’ll see multiple different drugs targeting mutant JAK2 specifically. The hypothesis is: could that be better and more specific than targeting the whole pathway? Let’s see. You’ll see phase 1 trials there.
CALR turns out to be a really good target, especially for immune therapy targeting. That’s only new science in the last five years. There are vaccine approaches either by themselves or with other immune drugs, such as ipilimumab. There’s an exciting bispecific molecule, which is a mutant CALR x CD3 bispecific antibody that I and others will be working on.
There are also going to be other ways to target CALR. You have multiple different ways of targeting mutant-specific approaches, but let me highlight these are phase 1 clinical trials. They’re backed by animal preclinical data. Now we need to see how they do in the initial trials.
For the first time, I’m seeing sustained improvement in the anemia of MPN, specifically myelofibrosis. We have three different categories trying to address this for our patients.
Dr. Naveen Pemmaraju
Anemia in Myelofibrosis
Ruth: Dr. Pemmaraju, you mentioned that many people suffer from anemia when hemoglobin is low. We know they can feel extremely fatigued so much that it interferes with their quality of life, which I know from personal experience, unfortunately. With what you’ve described, do you feel like we’re getting better tools to fight anemia and hopefully avoid people needing more frequent transfusions?
Dr. Pemmaraju: Yes. For the first time, I’m seeing sustained improvement in the anemia of MPN, specifically myelofibrosis. We have three different categories trying to address this for our patients and it’s simply exciting.
First is the JAK inhibitors themselves. As we mentioned earlier, the first initial ones did not improve and may have worsened the anemia transiently in some patients. Now these second- and third-generation JAK inhibitors are improving the anemia and possibly through the inhibition of ACVRL1, so that’s exciting.
Second is the additional agents, such as luspatercept. You can add on an agent that works outside of the JAK inhibitor that aims to stimulate the hemoglobin and improve the anemia.
Third is these novel agents. When you look closely at the navitoclax and pelabresib data sets, in those two particular instances, you have some people who get anemia as toxicity, but you also have patients who have anemia improvement with the combination, maybe better than with ruxolitinib alone. These three approaches, we’re already seeing in the clinic in phase 1, 2, and 3 clinical trials.
Out of all of these theoretical things, a lot of times what our patients are suffering from is anemia. When the hemoglobin gets below 7, 6, 5, or 4, it’s not even compatible with life, much less quality of life. Anything we can do to reduce the burden of getting transfusions, missing appointments, and missing life events is going to be a big breakthrough, and I’m starting to see that.
If a transplant is available and indicated, it is the only curative approach for myelofibrosis.
Dr. Naveen Pemmaraju
Role of Stem Cell Transplant in the Treatment of Myelofibrosis
Ruth: Typically, a doctor will tell a patient that the only cure for myelofibrosis is having a stem cell transplant. With these new medical therapies, my question is always the same: do you see a changing role for transplants?
Dr. Pemmaraju: The role of stem cell transplant in myelofibrosis is one of great importance still. While I’m personally excited about all of these drugs in development, two things are important.
First, none of these have been shown to create a long-term cure in and of themselves for myelofibrosis. Second, if a transplant is available and indicated, it is the only curative approach for myelofibrosis.
Having said that, the realistic problem with allogeneic transplants is that it’s not available for everyone because of their comorbidities, how frail versus how fit they are, matching, the infection rate, and the mortality rate. As patients get older, it may be tougher at some centers and for some folks to do it. There are some real limitations.
The other problem is that out of all of our patients, the vast majority are not going to transplant. Improvements are being made with transplants every day. Haploidentical transplant, which is a half match, is becoming more of a standard, so that gives the donor pool exponentially more options.
Trying to reduce graft versus host disease, which are complications after the transplant, with medicines are revolutionizing the field.
As I’ve traveled all over the world, people can do stem cell transplants in economically diverse situations. The transplant procedure itself can be highly expensive. Interestingly, even though cost-effectiveness is an issue, in some locales, if you can do a transplant and potentially cure the disease, it can lead to an improvement in socioeconomic status overall.
There are some cool, important things happening. But it’s an important point that even with all the excitement of these medicines and medicine combos, we’re still not at the point where we’re talking about a cure, so if you have the availability and indication for transplant, you have to pursue that consideration.
We have brand new approaches that we didn’t have a few years ago. There is a lot of data and science, so there’s hope.
Dr. Naveen Pemmaraju
Final Takeaways
Ruth: Let’s put all of this together. For those of us living with myelofibrosis or others who are concerned about progressing to myelofibrosis, what do you want to leave them with? When you total up everything we’ve talked about, how do you want to leave the conversation?
Dr. Pemmaraju: This discussion was very exciting because it left me with even more hope than when I started the day. I would leave our patients, caregivers, family members, advocates, and stakeholders with a message of hope and positivity. It’s not blind hope and positivity. It’s not based on hunches or ideas. It’s based on data.
The last three years in particular, I would call it — and I do not use this phrase lightly — a golden era for research for the MPN, specifically including myelofibrosis.
There are four areas to highlight and to be very excited about for our patients and families. First is the development of new JAK inhibitors. We mentioned the four that are already approved in the US, so let’s get them available all over the world. There are several more in clinical development.
Second is the JAK inhibitor combinations. Very exciting data from ASH. Let’s see the new combinations. Maturing data for navitoclax, pelabresib, and selinexor.
A third area of excitement and hope is that of anemia-improving agents.
Finally, the delineation, description, and demonstration of brand-new molecular pathways inside the cells that were never known before. New insights and ways of approaching. We mentioned potential immune therapy approaches, like the CALR mutation. It’s exciting that we have brand new approaches that we didn’t have a few years ago. There is a lot of data and science, so there’s hope.
Ruth: Dr. Pemmaraju, thanks so much for being with us today. You’re always a pleasure to talk to and so informative to our guests. We really appreciate your time.
Dr. Pemmaraju: Thank you so much for having me. This was a very thought-provoking and stimulating discussion.