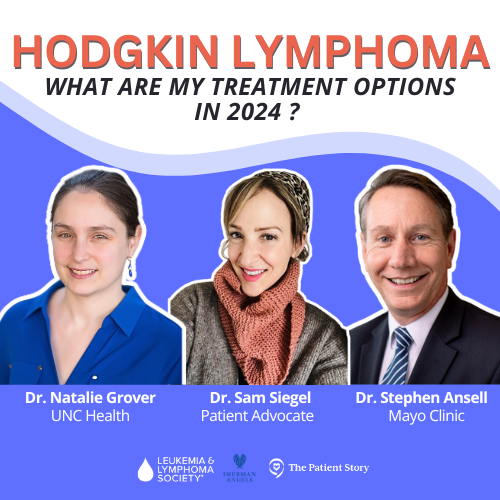
The Latest in Hodgkin Lymphoma
What are My Treatment Options in 2024?
Edited by: Katrina Villareal
Where is Hodgkin lymphoma headed in 2024? Two-time Hodgkin’s lymphoma survivor Dr. Sam Siegel discusses with top lymphoma experts, Dr. Natalie Grover of UNC Health and Dr. Stephen Ansell of Mayo Clinic, as they break down what patients and caregivers need to know!
Key topics include the latest treatment options and clinical trials, reducing toxicity from treatments, advances in post-transplant relapse, and the roles of CAR T-cell therapy and bispecific antibodies in the treatment of Hodgkin lymphoma.
Introduction
Current, Standard Treatments
Latest Advancements in Treatment
SWOG S1826 trial
Bispecific Antibodies
CAR T-Cell Therapy
Stem Cell Transplant
Developments in Salvage Therapy


This program is brought to you by The Patient Story in partnership with The Leukemia & Lymphoma Society and Imerman Angels.
Introduction
Stephanie Chuang, The Patient Story
Stephanie Chuang, The Patient Story: My name is Stephanie Chuang, the founder of The Patient Story. I also got a blood cancer diagnosis a few years ago. Mine was non-Hodgkin lymphoma, but we have so many shared experiences in what we’re looking for and that’s what The Patient Story is all about.
We help both patients and care partners navigate a cancer diagnosis. We do this primarily through in-depth conversations with patients, care partners, and top cancer specialists.
We’re so proud to be partnering with The Leukemia & Lymphoma Society and Imerman Angels for this program.
We want to note that The Patient Story retains full editorial control of this entire program and that this is not meant to be a substitute for medical advice.
Our patient moderator, Dr. Sam Siegel, will be leading the conversation from this point forward.


Sam Siegel, MD, Patient Advocate
Dr. Sam Siegel: Thanks, Stephanie! I’m a two-time Hodgkin’s lymphoma survivor, bone marrow transplant survivor, and primary care physician doing survivorship medicine. I’m here to have this wonderful conversation with Dr. Natalie Grover and Dr. Stephen Ansell about Hodgkin lymphoma updates.
Natalie Grover, MD
Sam: Dr. Natalie Grover is a hematologist-oncologist at the UNC School of Medicine. She’s the clinical director of the cellular therapy program, leads several CAR T-cell therapy clinical trials in lymphoma, and strives to improve treatment options and quality of life for lymphoma patients.
Dr. Grover, can you tell us a little bit about yourself, what drew you to lymphoma, and about your approach to patients and how you care for them?
Dr. Natalie Grover: I was drawn to oncology as a maternal medicine resident. Much of it was based on my relationship with patients whom I saw in the inpatient oncology ward. When I saw those patients, I always wanted to go back and find out more about what happened to them and form connections with them.
There were so many discoveries and new treatments available. Even during residency, the treatment landscape was changing so much and that drove me to oncology.
I like how heterogeneous lymphoma is and how it involves a wide patient population of both young and older patients. It’s truly a systemic disease. There are so many different types of lymphoma so my clinic is a very heterogeneous mix of different patients and I enjoy that.
Sam: That makes a lot of sense. Lymphoma is the umbrella, but it’s a lot of different diseases that can affect multiple parts of the body. I could see how that’s interesting.

Stephen Ansell, MD, PhD
Sam: Dr. Stephen Ansell is a hematologist-oncologist at the Mayo Clinic who studies and specializes in Hodgkin’s lymphoma. His research has led to the use of immune checkpoint therapy in lymphomas, which is a very exciting development. His goal is to translate his research into new treatment approaches.
Dr. Ansell, can you tell us about your path into lymphoma, what drew you to the field, and your approach to patients?

Dr. Stephen Ansell: I trained in South Africa. I was very focused on internal medicine, but they needed someone to do some work temporarily in oncology and assigned me.
When I got there, similar to Dr. Grover, I was excited about the opportunity, the disease, the patients, and how we could make a difference based on the fact that treatments were highly effective and beneficial. Patients benefited substantially even from initial treatments back in the day of more chemotherapy.
What has been exciting for me throughout my career has been to see how we can change treatments by increasing the number of people who benefit and hopefully get cured, and decreasing the side effects and toxicities by being able to find effective therapies that aren’t that hard on patients.
Sam: Your areas of interest and passion are so personally meaningful to me and my lymphoma journey, and I think will resonate with a lot of people.
Even though I had some side effects from the brentuximab at the highest dose that I first started it on, it still felt like a cakewalk compared to my initial drug regimen.
Dr. Sam Siegel
Sam’s Hodgkin Lymphoma Story
Sam: I was diagnosed with stage 2AE Hodgkin’s lymphoma and the reason that 2AE is important is because E means extranodal manifestations. I had some lung involvement and it was confusing whether or not I was a stage 2 with right around the lymph nodes in that lung or stage 4. That was going to impact how many months of chemotherapy I would have.
I started with ABVD chemotherapy. Within two months, the initial cough that I had at the time of diagnosis improved pretty quickly. Towards the end of those two months, I started getting a cough again. My PET scan looked good so the thought was that bleomycin was probably to blame for that cough.
We dropped bleomycin and it felt pretty okay making that decision. I suspected that something else was going on, but because the scan had come back clean, we decided to watch and wait.


About a month or two after that, I developed symptoms that were eerily reminiscent of my initial diagnosis, such as wheezing in the upper left side of my chest, which I knew wasn’t normal, and a pea-sized lump above my collarbone in a very similar location to where the initial lump was.
I suspected that those were Hodgkin lymphoma symptoms and sought care right away. The PET scan showed that I was most likely having a relapse.
It was a process to get the tissue to confirm the relapse. I had to have three biopsies, with the third one involving a thoracic surgery to get a lymph node right near my heart.
By that time, I felt so beaten up by traditional cytotoxic chemotherapy. New information was coming around about salvage therapy, which is the therapy after a person has relapsed from initial therapy. At that time, I didn’t feel that I could go through another few months of multi-drug traditional cytotoxic chemotherapy.
Data was coming out about brentuximab, an antibody-drug conjugate, and using that as a bridge to autologous bone marrow transplant. My oncologist said, “These trials showed that this could be an effective bridge to transplant. What do you think?” I said yes because I wanted to go for the therapy with the least amount of toxicity.
Even though I had some side effects from the brentuximab at the highest dose that I first started it on, it still felt like a cakewalk compared to my initial drug regimen.
That goes to show how important the science is and the clinical trials that inform oncologists how to adjust therapies, especially therapies that were traditionally pretty toxic in terms of long-term and late-term effects.

There are always ways in which we’re trying to make treatment better… we’re trying to replace radiation therapy by utilizing new agents.
Dr. Stephen Ansell
Standard of Care: First-Line Treatments
Sam: Dr. Ansell, can you tell us about the current standard first-line treatments and their efficacy for Hodgkin lymphoma?
Dr. Ansell: In many respects, we think about it in two buckets: people who have more limited-stage disease (only on one side of the diaphragm, either above or below) or advanced-stage disease (both sides of the diaphragm, in the bone marrow, or other tissues).
With limited-stage disease, we again think of two buckets. These are different symptoms and other tests to determine prognostic factors. If you have favorable prognostic factors, we treat you with very minimal chemotherapy. If you have more symptoms and unfavorable factors, we will treat you with a little bit more treatment. If you have advanced disease, we give you more treatment yet again.
There are always ways in which we’re trying to make treatment better, but the most standard way is if you have very limited disease with good favorable factors, we often will give two rounds of chemotherapy treatment and then consider consolidation radiation treatment.
If you have a more advanced disease, still limited to one side of the diaphragm but with more unfavorable factors, we would give more chemotherapy and more radiation treatment. Then for advanced-stage disease, we would give chemotherapy and no radiation treatment.
However, we’re trying to replace radiation therapy by utilizing new agents. We’ve used PET scans to tell us who might need extra treatment or not. I have to hedge a little bit because a lot of it is individualized and that’s the most important thing.
It’s so important to raise awareness about the importance of being involved in clinical trials and knowing that you don’t have to have failed multiple lines of therapy before you consider them.
Dr. Sam Siegel
Sam: Absolutely. How do you decide? There are different prognostic systems so if somebody is unfavorable in one and favorable in others, how do you factor that in?
Dr. Ansell: Pick one system and utilize the data supported by that system. The German Hodgkin Study Group has done a lot of work in this space. In our practice, we tend to use the prognostic system that they use because that helps us standardize treatment.
What we want to do is always push the envelope. We encourage people to participate in clinical trials that are testing new ways compared to the standard ways to see if we can optimize treatment even further.
Sam: I love that. Thank you for bringing up clinical trials. It’s so important to raise awareness about the importance of being involved in clinical trials and knowing that you don’t have to have failed multiple lines of therapy before you consider them.
Clinical trials can be for everyone and there are so many different types of situations where somebody could need a clinical trial. We’re looking at things to de-escalate therapy or alter treatments based on a patient’s situation.
Dr. Ansell: I would say you’re exactly right. The most impressive and important data that has come out on Hodgkin lymphoma is in the front line based on recent clinical trials. Everyone needs to remember that what we do currently is based on people who have participated in clinical trials that have changed how we practice.
Standardly, we utilize new agents, like PD-1 blocking antibodies or brentuximab vedotin plus chemotherapy, rather than chemotherapy alone because that’s improved the outcome of patients. Especially in advanced-stage patients, that’s now the standard of care.
The two biggest drugs that have transformed the care for Hodgkin lymphoma in the past 5 to 10 years are brentuximab vedotin… and checkpoint inhibitors.
Dr. Natalie Grover
Latest Advancements in Treatments
Sam: Dr. Grover, what are some of the newest and hottest treatments for Hodgkin lymphoma?
Dr. Grover: I think the hottest advances in Hodgkin lymphoma are related to incorporating some of these new treatments into earlier lines of therapy to try to both improve outcomes so increase the chance of cure and reduce long-term toxicities.
The two biggest drugs that have transformed the care for Hodgkin lymphoma in the past 5 to 10 years are brentuximab vedotin, which is an antibody-drug conjugate. It delivers chemotherapy specifically to the cancer cells.
The cancer cells in Hodgkin lymphoma have a marker on them—CD30—that’s pretty much universally seen in all the Reed-Sternberg cells, the cancer cells in Hodgkin lymphoma. Brentuximab specifically targets those.
The other drugs are what people may have heard of called checkpoint inhibitors. These immunotherapies help the immune system fight Hodgkin’s lymphoma.
When they incorporated these drugs—nivolumab, pembrolizumab, and brentuximab—they were successful in relapsed/refractory disease. Now they’re being moved to earlier lines of therapy to try to reduce the amount of chemotherapy that we’re giving patients and hopefully to enhance care in these patients.
By limiting chemotherapy and radiation, can you improve patient outcomes?
Dr. Natalie Grover
Sam: How about some recent clinical trials for reducing toxicity? I heard about AHOD2131.
Dr. Grover: There’s a clinical trial for pediatric and adult patients looking at whether we can incorporate these newer treatments, brentuximab and checkpoint inhibitors, in newly diagnosed Hodgkin lymphoma patients.
Everyone gets two cycles of standard chemotherapy then patients get randomized to either getting these new treatments, brentuximab and nivolumab, or continuing to standard chemotherapy.
The question is: by limiting chemotherapy and radiation, can you improve patient outcomes? One thing they want to look at is cure rates and long-term survival from a Hodgkin’s standpoint, but they’re also collecting data looking at quality of life patient-reported outcomes.
The top priority is curing their lymphoma, but we also want to think about the quality of life for patients moving forward and making sure that they live long lives.
Dr. Natalie Grover
Sam: That’s incredible. When you’re talking about late-term effects or reducing toxicities, what are some of the things that we’re trying to reduce long-term?
Dr. Grover: One of the chemotherapy drugs that we give patients can affect their heart function so some of the things that we think about are the risk of heart disease down the line.
One of the drugs that we’re using a lot less often now can affect lung function so we look at issues with lung function past therapy.
With some of these drugs and using more brentuximab, another thing that we’re thinking about is neuropathy. Patients can have some nerve damage and issues with pain, numbness, and tingling or doing different functions, like texting, typing, or writing.
With young patients, another thing we think about is fertility. Even though many of these patients can have children in the future as a lot of these earlier treatments don’t have as big an effect on fertility, it’s still something we think about, especially if we need to escalate people who have a disease that relapses or need more aggressive therapies.
We also think of secondary cancers. Some chemotherapy and radiation may increase the risk of having other cancers.
The positive is that most of these patients live long enough for us to focus on that and think about these effects. The top priority is curing their lymphoma, but we also want to think about the quality of life for patients moving forward and making sure that they live long lives.
Checkpoint inhibitors help the immune system fight the cancer. Some of these patients may stop responding to checkpoint inhibitors so there’s interest in using other types of treatments in combination.
Dr. Natalie Grover
Sam: What about trials to re-sensitize to PD-1 drugs? What does that mean?
Dr. Grover: Checkpoint inhibitors are effective in Hodgkin lymphoma. Right now, we’re moving them to earlier lines of therapy but these are treatments that can also work well for relapsed and refractory patients.
Hodgkin lymphoma is unique because, compared to other lymphomas, there aren’t that many cancer cells in these patients. When pathologists look at cells, there are a lot of immune cells around the cancer cells so there aren’t that many lymphoma cells. A lot of it is your immune reaction to the lymphoma.
Checkpoint inhibitors help the immune system fight the cancer. Some of these patients may stop responding to checkpoint inhibitors so there’s interest in using other types of treatments in combination. If a patient progresses on pembrolizumab or nivolumab, can you combine them with other treatments and re-sensitize your immune system so they can be sensitive again to these treatments? There’s some research looking into that.
We’ve also seen patients get the reverse. These treatments may reset the patients in some way. Patients may get checkpoint inhibitors and then after that may respond better to other treatments. There have been some studies showing that after checkpoint inhibitors, even if they progress on those drugs, patients potentially respond better to chemotherapy or other treatments.
Sam: We’re still learning how these drugs impact the immune system and how they might make you respond better to traditional chemotherapies, even if you didn’t initially. That’s incredible.
Dr. Grover: The current biggest advances are in advanced-stage Hodgkin lymphoma. More recently, brentuximab was incorporated in addition to chemotherapy. Dr. Ansell was part of that study. That improved overall survival in advanced-stage Hodgkin lymphoma patients compared to standard of care.
We can see the progression from old-style chemotherapy to immune checkpoint plus chemotherapy as the front-line treatment.
Dr. Stephen Ansell
Early vs. Advanced Stage Advancements
Sam: Dr. Ansell, can you tell us about the SWOG S1826 trial and what that showed?
Dr. Ansell: Picking up again on the theme of better therapies getting better outcomes and using some of the new drugs that we’ve touched on, as Dr. Grover said, the management of advanced-stage patients has moved over time.
Back in the day, we gave ABVD chemotherapy and tried to leave out bleomycin, which causes lung toxicity, if patients were doing well based on PET scans.
These new drugs, brentuximab vedotin being the first one, were brought into the combination in place of bleomycin. It’s now brentuximab with AVD. When compared head to head, it showed that brentuximab improved the outcome of patients—not only their likelihood of staying in remission but their overall survival.
It was then compared as the standard to nivolumab, the PD-1-directed therapy, plus AVD chemotherapy in place of bleomycin. That then showed progression-free survival at a one-year follow-up. We don’t have mature data yet, but it seemed better already than the brentuximab-AVD chemotherapy and, as Dr. Grover touched on, less in the way of side effects and better tolerated.
That’s likely to become the new standard for advanced-stage patients. We want to see a little bit more mature data. But certainly, in elderly patients where toxicity is a real challenge, this has become a standard for many. We can see the progression from old-style chemotherapy to immune checkpoint plus chemotherapy as the front-line treatment.
Sam: These are exciting times. It’s wild because, for decades and decades, it seemed like we were doing the same thing for Hodgkin patients. Even if I were diagnosed with the same clinical scenario now compared to when I was first diagnosed in 2021, I would be treated differently.
There is still a subset of people where the disease proves to be very challenging and keeps relapsing… We still see patients who have gone through this standard treatment using these new drugs and then the disease comes back yet again.
Dr. Stephen Ansell
Gaps Clinical Trials are Filling
Sam: Can you tell us about these clinical trials and what gaps they fill?
Dr. Ansell: You heard us talk about two new drugs. They came from the relapsed setting but have moved up to front-line treatments. The gaps are for patients, heaven forbid, who have gone through these new therapies.
There is still a subset of people where the disease proves to be very challenging and keeps relapsing. That group’s getting to be smaller and smaller so that’s the good news. The challenging point is that it’s never good enough until there’s nobody in that group. We still see patients who have gone through this standard treatment using these new drugs and then the disease comes back yet again.
Things that are becoming exciting and that we need to do better on is what to do for those patients. Additional treatments that target these other immune checkpoints aside from PD-1 and other ways to make the immune system wake up and do its job are being tested.
The work that Dr. Grover and her team do is taking your immune cells, sending them to “training camp” to get a little docking site on them so they can detect the cancer in a much better way, and then unleashing them on the cancer. That’s proving exciting.
Finally, what we call bispecific antibodies. Those are also being tested and are some of the exciting opportunities in the future.
One arm of the antibody is directed to CD30, but the other arm grabs onto CD3 in the T cells.
Dr. Stephen Ansell
Bispecific Antibodies
Sam: Can you tell us about bispecific antibodies?
Dr. Ansell: This is an area that’s growing fast in Hodgkin lymphoma. Dr. Grover talked about CD30, which is on the cancer cells. One arm of the antibody is directed to CD30, but the other arm grabs onto CD3 in the T cells.
Bispecific antibodies bring those cells into very close proximity to each other. Like your kids in the back of the car who don’t like to sit next to each other and keep poking each other, this causes those cells to be grumpy with each other. The T cells, your immune cells, will then fight the cancer. That’s really what you want to see.
We talked about immune checkpoints that make T cells do a better job. One of the ways we’re doing that is on one arm, PD-1, which is an established immune checkpoint, but on the other, something like TIM-3, which is another immune checkpoint.
Other ways in which T cells are being switched off are now protected so it’s making those cells even more efficient. Those are two of the main ways bispecific antibodies are being tested right now.
With CAR T-cell therapy, we have seen some nice responses in patients whose disease has progressed after many different therapies, but there’s still work to do to improve these therapies.
Dr. Natalie Grover
CAR T-cell Therapy
Sam: Dr. Grover, how about CAR T-cell therapy and post-transplant relapses? Can you tell us about that and where CAR T-cell therapy might play a role?
Dr. Grover: As Dr. Ansell briefly mentioned, CAR T-cell therapy involves taking a patient’s T cells, sending them off, and re-engineering them so they can specifically target the CD30 protein on the cancer cell.
We have a CAR T-cell therapy trial at UNC and at the Baylor College of Medicine. There are two academic trials where we’re studying these CAR T cells in patients with Hodgkin lymphoma. There are also a few international trials. I know there’s a group in Spain and China.
Unfortunately, there isn’t a company-sponsored trial. They’re exciting treatments, but they’re not as easily accessible. Patients do need to travel for these for these treatments.
The big thing is long waiting lists, but we are hoping to get more patients treated more quickly because it still shows that there is an unmet need. Some patients have not responded, progressed after brentuximab, progressed after checkpoint inhibitors, progressed after transplant, and need additional options for treatment.
With CAR T-cell therapy, we have seen some nice responses in patients whose disease has progressed after many different therapies, but there’s still work to do to improve these therapies.
Right now, we have some patients who have been in remission for many years—five-plus years after getting CAR T cells. Many patients get the CAR T cells and have a great response, but their disease relapses afterward. We’re trying to figure out why that’s happening and how we can improve the CAR T cells and improve outcomes for patients.
Patients who relapse can have more aggressive disease as opposed to some other more aggressive types of lymphoma, but with Hodgkin, patients who have relapsed oftentimes can live a long time even with the disease.
Dr. Natalie Grover
Dr. Ansell: There’s one other option that takes both bispecifics and cellular therapies and combines those strategies. That’s taking the natural killer cells from cord blood and using a bispecific antibody that targets CD30 and a protein called CD16 on the NK cell. It sticks this bispecific antibody to the NK cell.
They pre-treat the NK cells before they give them to the patient and then infuse them. You activate the cells outside the body, add the bispecific antibody so that it’s already stuck to the NK cells, and infuse them. Those also have been effective therapies.
Dr. Grover’s right. We’re still learning about how many treatments you need to get. They’re getting high response rates, but the durability is still in question. But I think that’s another exciting strategy of taking cellular therapies and bispecifics and using them together.
Dr. Grover: I think that’s the LuminICE trial, which will be open at several different sites across the country.
Sam: That’s great. That’s an important point. It’s part of the issue of Hodgkin lymphoma compared to non-Hodgkin’s. It’s not nearly as common in terms of the number of people that will qualify for these trials so that may be why there are less commonly offered.
Dr. Grover: Hodgkin lymphoma has higher cure rates and is less common. A lot of times, patients who relapse can have more aggressive disease as opposed to some other more aggressive types of lymphoma, but with Hodgkin, patients who have relapsed oftentimes can live a long time even with the disease.
I’ve seen patients in my trials who have relapsed and have not even been in remission but have been living for many, many years with relapsed disease. A lot of times, these patients may not be as sick, which is a good thing, so they’re able to travel and participate in these trials. Many of these patients may be alive and doing well even though they’re going through treatment or have some disease left.
An allogeneic transplant is still a curative option and something that we would always consider.
Dr. Stephen Ansell
Transplant
Sam: Where is all this in relation to allogeneic transplants for people who are relapsing after transplant? Allogeneic, meaning the donor is somebody else, as opposed to autologous, which is more common in Hodgkin.
Dr. Ansell: To be honest, an allogeneic transplant is still a curative option and something that we would always consider. It’s a little bit high-risk because of the potential for longer-term toxicities.
With a lot of these novel treatments, many of which have been very successful in the past, people delayed allogeneic transplants a little bit. There are some challenges now as patients are having their disease come back after standard treatment so there is a subset of patients for whom that needs to be considered. That’s a very individualized discussion between patients and their doctors to weigh the risks versus the benefits.
One of the key questions to ask is what treatment somebody got as their first line because that impacts what you would do in the second line.
Dr. Stephen Ansell
Developments in Salvage Therapy
Sam: Dr. Ansell, what are some of the developments in salvage therapy, which is given when somebody has their initial relapse?
Dr. Ansell: It’s moving pretty fast right now. Novel drugs are being used in the front line so one of the key questions to ask is what treatment somebody got as their first line because that impacts what you would do in the second line.
However, based on where most patients are right now, not very many have had an immune checkpoint treatment, which is the nivolumab and pembrolizumab that Dr. Grover spoke about. Not too many people have had that as their front-line treatment and using those in combination with standard chemotherapies, like ICE chemotherapy or GVD chemotherapy. In the majority of particularly younger patients, going to more intensive treatment and a stem cell transplant using your own cells is very much the standard management.
Some interesting recent data compared where that was used to standard chemotherapy or the use of brentuximab and chemotherapy then a transplant and then looked at outcomes. The patients with the best outcome got a PD-1 antibody before they got their transplant.
Dr. Grover touched on this, which is an important point. The PD-1 blocking antibody team seems to change the immune system a bit and make patients more sensitive to some of the chemotherapies after the fact so that’s why it seems like it makes a difference. We tend to favor chemotherapy with immune checkpoint therapy as a treatment approach before going to transplant.
We want to see people cured. Heaven forbid that it comes back the first time, but if it does, all the gloves are off. Now we’re going at it as hard as we possibly can.
Dr. Stephen Ansell
Sam: That’s interesting because I know in other cancers, people will save therapies or not want to expose them because the body will learn them. What you’re saying is that the same principle may not apply in Hodgkin. These therapies may sensitize to other therapies or make people respond better so you don’t necessarily need to leave them until later when you’ve burned through other options.
Dr. Ansell: Correct. We want to see people cured. Heaven forbid that it comes back the first time, but if it does, all the gloves are off. Now we’re going at it as hard as we possibly can and we want to utilize all the effective tools that we have so that we can truly beat it into the ground. That’s what I would recommend. Different from other cancers where you might want to string things along in a palliative approach. With Hodgkin, you want to go after it with curative intent.
Sam: It’s wild to think how quickly things evolve and how important it is for patients to seek out providers or treatment at cancer centers who have some connection with the trials and know the latest updates.
How can we advise patients to seek out that kind of care? How can they ask for that from their oncologist if they’re getting treatment in the community?
Dr. Ansell: Be an informed patient. Ask questions and be a strong advocate for yourself. There are excellent resources, like The Leukemia & Lymphoma Society, which have good information related to many of these topics. Being informed about the best way to be managed is useful.
When your doctor sees you and goes through things, asking questions relative to the information that you have helps you feel reassured that you’re on the right track. Most of us are quite okay with patients getting second opinions from other colleagues.
Second opinions help people reinforce the messages you’re already giving. People will be more comfortable doing what needs to be done if they’re hearing the same thing from more than one person. All of that pertains to a good outcome. If you ask questions, make sure you get your questions answered.
Sam: Thanks for empowering patients because it’s so hard to make these decisions even when you have a lot of resources and education. It could be such an emotional time, in addition to not feeling well, and it’s helpful to hear that you expect people to want other opinions and be informed.
Dr. Ansell: To be honest, a lot of patients come in and get so much information that it’s pretty challenging to retain them. I always tell people to bring friends or family. Have other sets of ears that can help reinforce some of the messages so that when your brain is locked down and you can’t think straight, they hear things that you might have missed.
The treatments are getting better all the time so there’s a lot of hope. I’m hoping that in the not-very-distant future, every patient with Hodgkin lymphoma can be cured with front-line treatment.
Dr. Stephen Ansell
Final Messages
Sam: Dr. Grover, can you give us some final points or takeaway messages?
Dr. Grover: I’m excited about improving earlier therapies and moving these newer therapies to the front line both to hopefully enhance cure to prevent patients from relapsing again and reduce long-term toxicities and improve quality of life.
There’s still an unmet need for patients who are refractory to PD-1 inhibitors, brentuximab, and chemotherapy. I’m hoping that over the next few years, we will have more clinical trials and more developments for that patient population.
For patients, ask questions of your provider. Don’t be shy about getting a second opinion. I’m never offended if a patient goes for a second opinion.
Sam: How about you, Dr. Ansell?
Dr. Ansell: If you’re a patient with Hodgkin lymphoma, there are unique and novel treatments that are making a big difference to patient outcomes. The treatments are getting better all the time so there’s a lot of hope. I’m hoping that in the not-very-distant future, every patient with Hodgkin lymphoma can be cured with front-line treatment.
Sam: Thank you so much for that. I remember initially being scared about death and dying. I think that’s what a lot of people think about when they hear the word cancer. Once it began to move away from that and began to become living with cancer or living life after a cancer diagnosis, I thought, I’d like to jog, paint, play guitar, hold my kids, and be able to think as well as possible.
These trials to improve quality of life while simultaneously improving outcomes are so meaningful personally. I know it means a lot to our patient population that you took the time to have this conversation with us. Thank you so much.
Dr. Ansell: My pleasure.
Dr. Grover: Thanks so much for having us.
Stephanie: Thank you so much, Sam, for being our incredible patient advocate and moderator. Also, thank you to Dr. Grover and Dr. Ansell, for the work and research you do to help move the landscape of treatment options in Hodgkin lymphoma.
We hope that you walk away with a better understanding of the latest treatments and clinical trials in Hodgkin lymphoma. They may or may not be right for you, but our goal is to make sure you feel empowered to make a decision for yourself.
Thank you and we hope to see you again at a future program at The Patient Story.