Building Bonds Episode 2: How to Find and Partner with a Doctor for Better Waldenström Care
Finding a doctor is important in your Waldenström macroglobulinemia care. A strong partnership leads to more informed decisions, personalized care, and a greater sense of control. Patient advocate Pete DeNardis, hematologist-oncologist Dr. Jonas Paludo from Mayo Clinic, and patient advocate Lisa Ramirez discuss how her decisions led to being treated by Dr. Paludo and forming a trusted patient-doctor relationship.
Edited by: Katrina Villareal
Discover the importance of second opinions and how even top specialists recommend them. Understand how a Waldenström macroglobulinemia specialist can provide a unique perspective having seen more cases. Learn about shared decision-making in Waldenström treatment. Hear first-hand experiences of navigating a chronic cancer with your doctor by your side. Get practical tips for advocating for yourself or a loved one in the treatment process.

We would also like to thank The Leukemia & Lymphoma Society and the International Waldenstrom’s Macroglobulinemia Foundation for their partnership.
This interview has been edited for clarity and length. This is not medical advice. Please consult with your healthcare provider for treatment decisions.
- Introduction
- Proactively Participating in Your Care
- Signs and Symptoms
- Insurance Concerns
- WM at a Glance
- Common WM Questions
- Getting a Second Opinion
- Knowing Your Options
- Finding a WM Specialist
- Treatment Approaches to WM
- I’m Newly Diagnosed. What Now?
- Deciding to Stay Local or Travel for Your Care
- How Often Do You See WM Patients?
- Approaches to Personalized Care
- Managing Your Life with WM
- WM Treatment Options
- The Emotional Impact of a WM Diagnosis
- Important Takeaways from Initial Consultation
- Lifestyle Changes in the Face of a WM Diagnosis
- Maximizing Your Quality of Life
- Patient Advocacy
- The Role of Care Partners
- Living with WM
- Waldenström: The Patient-Physician Relationship
- Key Takeaways
- Conclusion

Introduction
Tiffany Drummond, Patient Advocate
Tiffany Drummond: I’m a patient advocate with over 20 years of experience in cancer research. My journey as a care partner began when my mother was diagnosed with endometrial cancer in 2014. I quickly realized the challenges of finding reliable information to support her care, so I am committed to helping others avoid similar difficulties.
At The Patient Story, we create programs to help you figure out what’s next. Think of us as your go-to guide for navigating the cancer journey. From diagnosis to treatment, we’ve got you covered with real-life patient stories and educational programs with subject matter experts. I’m your personal cheerleader, here to help you and your loved ones best communicate with your healthcare team as you go from diagnosis through treatment and survivorship.

We want to give a big thank you to The Leukemia & Lymphoma Society for its partnership. The LLS offers incredible free resources, like their Information Specialists who help you communicate with members of your healthcare team and provide information about treatment options.
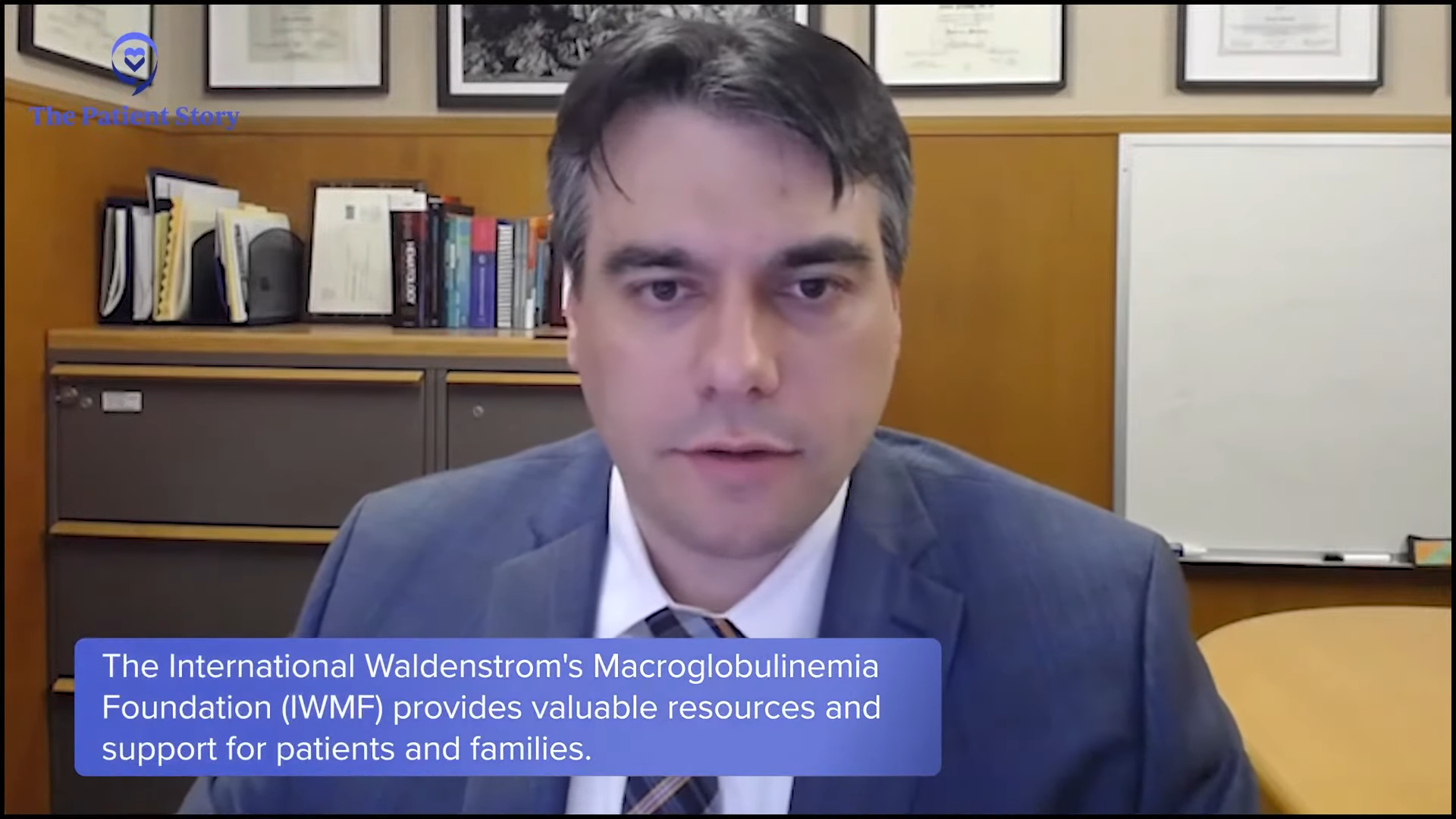
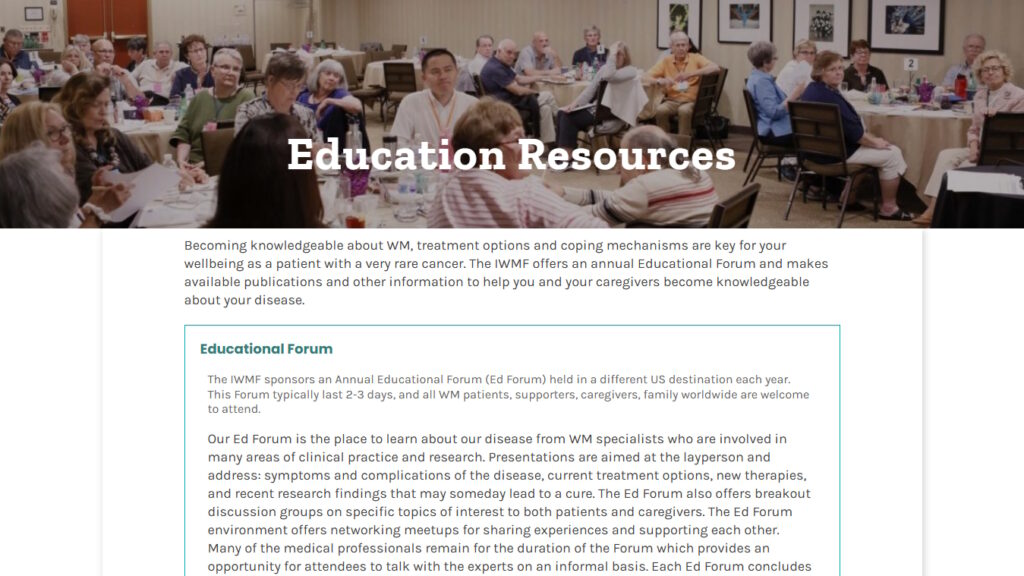
We also thank IWMF (International Waldenstrom’s Macroglobulinemia Foundation), an organization specifically dedicated to Waldenström’s patients and care partners. They also offer free resources, including over 60 in-person support groups worldwide.
The Patient Story retains full editorial control over all content. While we hope you find this helpful, please keep in mind that the information provided in this program is not a substitute for medical advice. Pete, a patient advocate and Waldenström’s survivor, will lead the conversation.

Peter DeNardis, IWMF Chair Emeritus
Peter DeNardis: I’m currently the chair emeritus of the International Waldenström’s Macroglobulinemia Foundation. I have been a long-time volunteer for the organization and a patient myself. I was diagnosed 20 years ago and I’m well aware of the importance of a strong patient-doctor relationship. I look forward to learning from our esteemed panelists about how best to build and maintain that relationship.
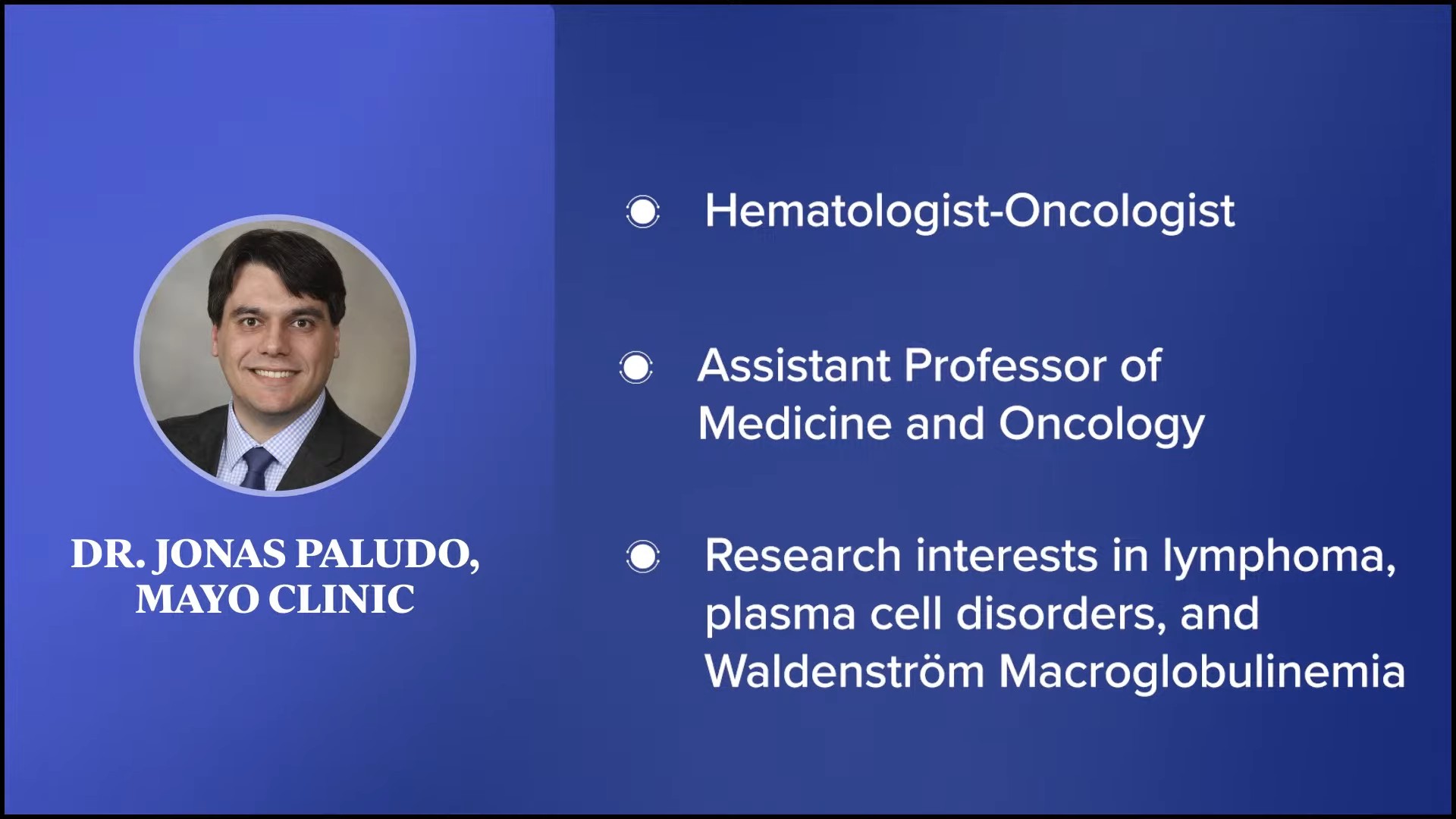
With us is Dr. Jonas Paludo, a hematologist-oncologist and assistant professor of medicine and oncology at Mayo Clinic in Rochester, Minnesota. His research interests include studies to understand the biology, genetics, and therapy of lymphoma and plasma cell disorders, and he is also a noted researcher in Waldenström’s.
Lisa Ramirez, Patient Advocate
Lisa Ramirez: I was diagnosed in 2021. I was getting into a doctoral program and had to do some routine testing and physical exams, and in the process, I was diagnosed with Waldenström’s macroglobulinemia. The diagnosing oncologist was retiring, so he passed me on to another doctor in his practice.
I did a lot of research on Waldenström’s immediately and read Dr. Gertz’s recommendation on getting a second opinion, which I appreciated. I looked for the doctor who I thought would be best in getting a second opinion from and that was Dr. Paludo since he specialized in Waldenström’s in young people. I got another opinion from a physician at a major cancer center in the state in which I live as well.
I had a great rapport with Dr. Paludo immediately, but I initially thought I would only see him for a second opinion since I lived in Texas and he was at Mayo Clinic. I made it work and secured Dr. Paludo as my primary oncologist. I was very pleased about that.


Proactively Participating in Your Care
Peter: It’s good that you immediately did research and also went for a second opinion. Is it appropriate to say that you were an involved patient from the start?
Lisa: Yes. I work in public health. I’m a natural researcher and a very curious person. I wanted to learn as much as I possibly could and as quickly as I could about Waldenström’s to plan out my course of treatment and to be a well-informed patient.
I listened to all the lectures I could get my hands on and tried to understand the philosophies of the different cancer institutes. They seem to have differing philosophies about treatment and I tried to find one that fit with my personal philosophy and how I wanted to approach treatment.
I wanted to learn as much as I possibly could and as quickly as I could about Waldenström’s to plan out my course of treatment and to be a well-informed patient.
Lisa Ramirez
Signs and Symptoms
Peter: Looking back, do you think you had any symptoms that you weren’t paying attention to at the time?
Lisa: I was having night sweats, but I didn’t I thought I was experiencing early pre-menopause symptoms. Now I know the difference between hot flashes and night sweats. There’s a big difference.
I had some testing done because of other reasons and there was a note to rule out lymphoma and to check in six months after. Right at the six-month mark, my primary physician had me see a hematologist because of those test results. I had zero symptoms then. I felt great.
Looking back, I had some input from other oncologists that perhaps I had the disease for so long that I thought I felt good. That small incremental change in a negative way can go unnoticed, but I thought, “Does it matter? If I believe I feel good, then I feel good.”

Insurance Concerns
Lisa: The average time between diagnosis and treatment is about two and a half years and that’s about how long it took for me, so I was right on pace with the average.
Peter: You got a second opinion in a different state. You live in Texas while Mayo Clinic is in Minnesota. Did you have any financial or insurance issues trying to see Dr. Paludo?
Lisa: Surprisingly not. I received some treatment in another city in Texas. When you break down the costs, that treatment was more expensive.
Different institutions have different priorities in terms of testing and the amount of testing at checkups. In my case, the cost of the additional testing outweighed the cost of travel to Minnesota. It ended up being more cost-effective and worth it to travel to receive treatment at Mayo Clinic.
Peter: You’re very fortunate in that regard. I’m glad that worked out for you. You’re under great care and it appears that right from the start, you’re a very involved, proactive patient, so I applaud you for that and hope that other patients can take your lead.
WM at a Glance
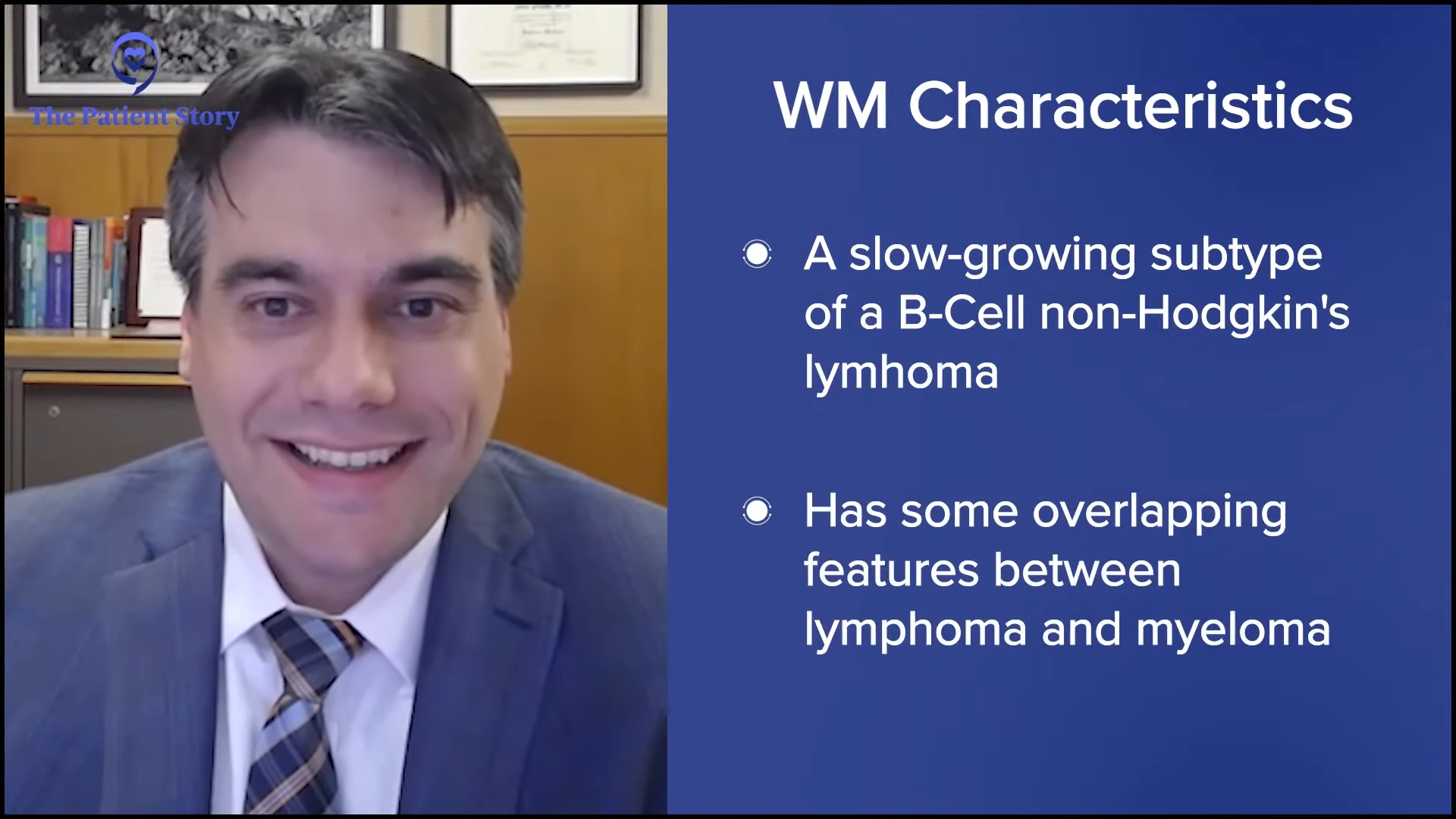
Peter: Dr. Paludo, many of us patients have a general idea of what Waldenström’s macroglobulinemia is, but can you give a 30,000-foot view explanation of what the disease is?
Dr. Jonas Paludo: Waldenström’s is a rare type of blood cancer. It’s a form of an indolent or slow-growing subtype of a B-cell non-Hodgkin’s lymphoma. It’s a disease that has some overlapping features between lymphoma and myeloma, but it’s a type of blood cancer.
Common WM Questions
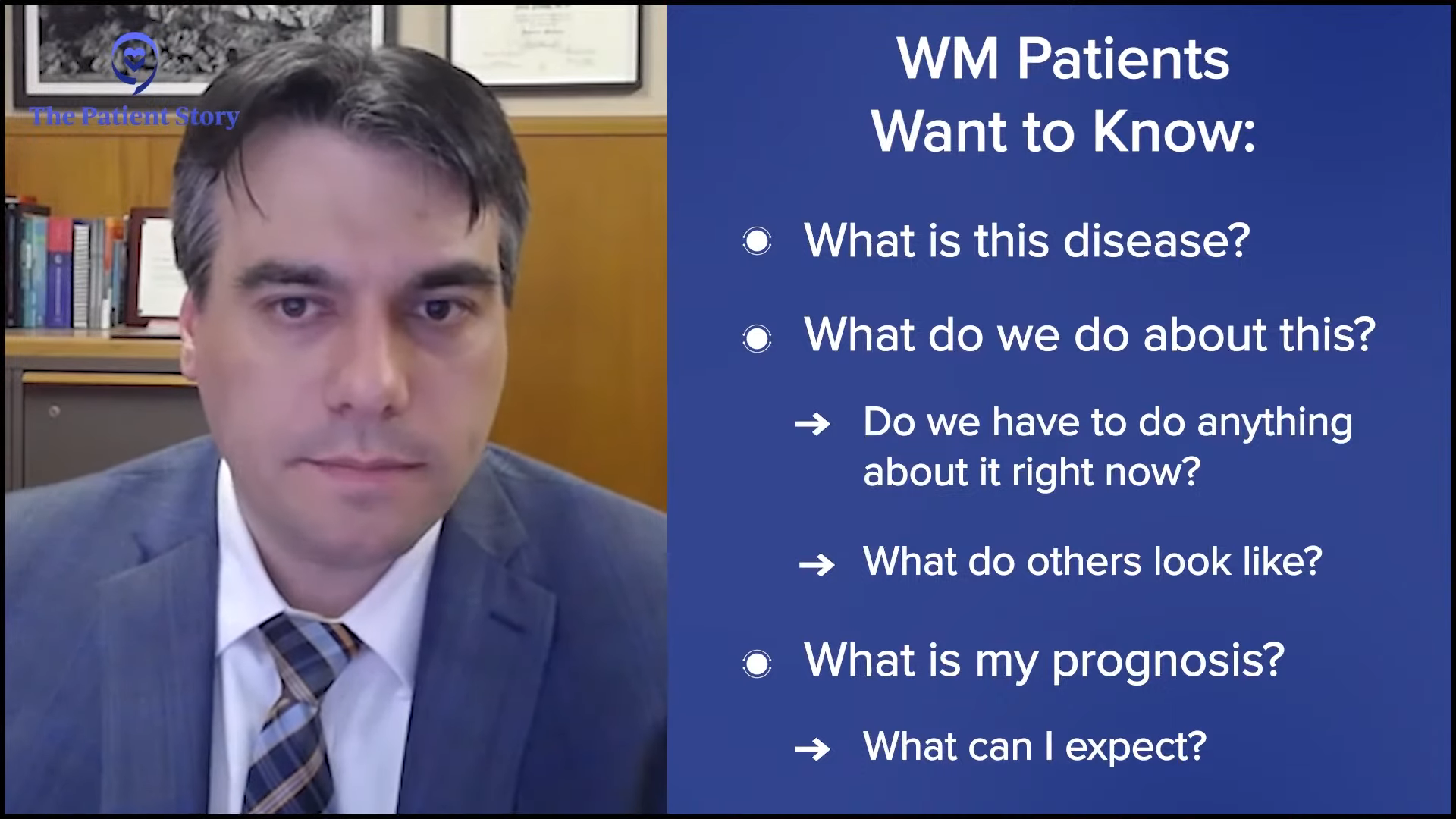
Peter: You see patients either coming initially to see you or for a second opinion. They probably have similar questions, but in your experience, what are the more common questions that patients ask?
Dr. Paludo: I can group the most common questions into three specific categories. In one shape or another, they’re trying to understand: What is Waldenström’s? What is this disease? Then the next one is: what do we do about this? Do we have to do anything about it right now? What it will look like? And then the third one is: what is my prognosis? What can I expect out of this disease?
Peter: Those questions are pretty common for Lisa and me when we were first diagnosed, so it’s good to see those questions are still being asked.
Diagnostic parameters, treatment options, follow-up testing, and surveillance are not as well-established in rare diseases as they are in more common diseases.
Dr. Jonas Paludo
Getting a Second Opinion
Peter: Many in the medical community and even the IWMF itself encourage patients to get a second opinion in certain circumstances. Dr. Paludo, as a healthcare provider, what are your thoughts on patients getting second opinions?
Dr. Paludo: Waldenström’s is a rare disease and like any rare disease, a second opinion should always be considered. Diagnostic parameters, treatment options, follow-up testing, and surveillance are not as well-established in rare diseases as they are in more common diseases or more common forms of cancer, like breast cancer or colon cancer, for example. That’s where a second opinion can help.
In addition, the familiarity of physicians with the disease or the current evidence and data of the disease can be quite variable. It’s part of reality. We can’t keep up with all the information generated daily for all diseases. Getting a second opinion from someone who has more experience or more interest in that specific type of rare disease is very important and adds a lot to the treatment and management.
I always encourage second opinions. To be honest, with most patients I see with Waldenström’s, I’m the one giving the second opinion. But for the patients who we see that are local, I encourage asking for another opinion elsewhere to have different points of view. I don’t think a second opinion would ever hurt a patient. It can only add information and help with the treatment and plan.


Peter: That’s a good point and hopefully they’re not trying to juggle three different opinions. In Lisa’s case, it was the one that she felt more comfortable with, which is appropriate.
Dr. Paludo: That’s a potential downside, but the benefits of a second opinion outweigh that downside.
Lisa: Waldenström’s is so different in terms of it being a cancer because you want to time treatment perfectly and take into account your quality of life. With a lot of other cancers, there’s a rush to treat and there are very specific treatment regimens. With Waldenström’s, you’re playing a very long game of chess.
You want your partner to be someone who you trust and who understands your quality of life and your age as you’re moving along the course of treatment. You’re going to want someone who understands you well enough, to keep pace, and who has a similar philosophy and approach to treatment. With Waldenström’s in particular compared to other cancers or other diseases, it’s important when selecting an oncologist that there’s a good fit.
Different cancer centers can appeal to different types of people. Mayo Clinic and Dr. Paludo were the perfect fit for me.
Dr. Jonas Paludo
Knowing Your Options
Peter: How did you know where to go for a second opinion? You mentioned Dr. Gertz’s presentation, but how did you figure out what your options were?
Lisa: The resources from the IWMF immediately pointing to Dr. Gertz and understanding Mayo Clinic’s philosophy led me there and looking into physicians there. I found Dr. Paludo in relation to Waldenström’s and other aspects of Waldenström’s that were of particular interest to me. I immediately sought him out for a second opinion.
I seem to resonate more with the philosophy of Mayo Clinic. They seem to have an approach that is slower to overreact. Their approach feels more strength-based rather than fear-based and I respond to that. When I need to embark on an intimidating treatment like chemotherapy, I want my partner to be able to reassure me that I’m strong enough, that I’ve prepared enough, and that it is the right time.
I understand that people have different motivations for starting treatment and some people can be more motivated by fear-based approaches. I don’t respond well to that. I respond better to a strength-based approach and the reassurance that all my questions are answered and that there’s enough time spent understanding the procedure or what’s happening with the progress of the disease. I find direct information very reassuring.
I have had oncologists who took a different approach where they feel nervous about my condition and then I start to feel very nervous and anxious. I know that it’s best to time treatments correctly and wait a little bit longer. It’s a fine line. Different cancer centers can appeal to different types of people. Mayo Clinic and Dr. Paludo were the perfect fit for me.
Finding a WM Specialist
Peter: Dr. Paludo, you mentioned that some patients come to you initially while others come for second opinions. If you’re telling a patient to get a second opinion, where do you direct them to? And for the patients who come to you initially, how did they find out about you in the first place?
Dr. Paludo: I also rely a lot on the IWMF resources to help patients decide on where to go next. There are so many factors, like insurance coverage and cost of travel, that are so particular to each patient, so I try not to be very specific. I point them to resources that they can look at to see which one makes more sense based on insurance, cost, travel, timing, family members, where they are, and things like that.
As with most rare diseases, you find more experience in bigger centers because they tend to see more patients with their rare diseases. It doesn’t necessarily mean that’s the only place you can find experience and expertise. It’s just the more common place where you can find expertise for rare diseases. The IWMF helps with pinpointing areas with more expertise or experience with Waldenström’s than other sites.
Peter: Because of my involvement with the IWMF, I’m well aware of the services they provide. On their website, they have a list of top doctors to go to for a second opinion regardless of what part of the world you’re in. The IWMF also has online discussion groups and Facebook groups where you can ask other patients who they go to. Granted, that’s word of mouth from one patient to another, but you can form an idea of who are the more noted doctors and who you could see if you want a second opinion.
The biggest challenge that I see is often related to indications to start treatment… sometimes it’s better if we don’t jump into treatment and instead sit tight and watch very closely.
Dr. Jonas Paludo
Treatment Approaches to WM
Peter: Dr. Paludo, what do you see that some healthcare professionals don’t get right about a WM patient?
Dr. Paludo: Waldenström is such a unique disease that the biggest challenge that I see is often related to indications to start treatment. Because of the uniqueness of this disease with overlapping features with other indolent lymphomas, sometimes I see more of a generalization of what we do for similar diseases applied to Waldenström’s. I understand where they’re coming from, but it doesn’t always fit with our best practices for Waldenström’s.
They haven’t seen a lot of cases and sometimes it can be difficult for a provider to sit tight on a patient who has a very high IgM level and hold off on doing something. It’s often easier to do something, but sometimes it’s better if we don’t jump into treatment and instead sit tight and watch very closely when patients are asymptomatic or not having significant symptoms.
Peter: I hesitate to say this, but back when I was first diagnosed, there was something called the 10,000 IgM Club. There were a handful of patients who felt that they were okay and feel fine. Their IgM level is 10,000, but their symptoms are fine. In hindsight, that may have not been, but every patient is different. You’re exactly right. It depends on a patient’s symptoms and how they’re feeling along with the blood values. It’s critical to go to a specialist if you can.


I’m Newly Diagnosed. What Now?
Peter: Let’s turn to the important role of the doctor-patient relationship in managing your disease course, both short- and long-term, especially about WM. It’s considered incurable, but with the more novel agents that have come around in the last 5 or 10 years, it’s much more treatable.
Lisa, you mentioned your path to getting a second opinion. What advice would you give to a newly-diagnosed patient who’s looking for care and what do you think is most important?
Lisa: What we’re talking about here is building rapport. You have to be able to trust your oncologist 100%. There are some scary moments and you question yourself. You want to have the reassurance of an oncologist who has expertise in this area, understands you, and has a sense of how uniquely your disease is manifesting.
Every WM patient is a little bit different, so find a physician who you can trust and sees you. Sometimes that’s not something tangible. It’s what occurs during a conversation and a sense that you feel shared insights or philosophies. During my visits with Dr. Paludo, he would ask, “And what else?” I loved that he always left room for all of my questions and he was always very direct with me.
You want to have the reassurance of an oncologist who has expertise in this area, understands you, and has a sense of how uniquely your disease is manifesting.
Lisa Ramirez
Do your research. Understand what it is that you want in terms of your quality of life and what’s important to you. For example, I was going to start treatment under the care of a different oncologist, which would have put at risk my ability to dance ballet on my toes because there was a higher risk of peripheral neuropathy with that particular treatment. At my age, I thought the first treatment I should do perhaps shouldn’t be that one. I was able to have that conversation with Dr. Paludo and talk about things that are important to me.
Oncologists see a lot of different patients and their priority is to save your life and get you treated, which is understandable, but it’s a little bit different with WM. My quality of life includes being able to dance on my toes, so losing feeling in my toes was a big deal. It would have negatively impacted my quality of life had I started with that particular treatment if I had the unfortunate side effect of being unable to feel my toes.
Find an oncologist who understands who you are as an individual, what your quality of life is based upon, what’s important to you, who you feel comfortable sticking with throughout your life, and who will map out a course of treatment that’s going to work for you. One time, Dr. Paludo said, “You’re probably going to have to do all the treatments. We just have to figure out what works for you when.” Everyone’s different, so that’s important.


Deciding to Stay Local or Travel for Your Care
Peter: You have a good rapport with Dr. Paludo. Do you still see a local oncologist in Texas?
Lisa: No, I see Dr. Paludo exclusively. I was already scheduled for treatment somewhere else, but I got cold feet at the last second. The first step in treatment is so critical. It impacts the next move and the next move and the next move. Even though those moves are spaced out—hopefully many years apart—it still sends off a ripple effect.
You want to feel very comfortable with your provider and the institution you’re receiving care from is critical. I had to advocate for myself and say, “I know it doesn’t make sense to seek treatment in a different state and to get my primary care from an oncologist so far away, but we’re going to Minnesota.”
How Often Do You See WM Patients?
Peter: Dr. Paludo, Mayo Clinic is a world-renowned medical institution, but, hopefully, many people with Waldenström’s also understand that it’s world-renowned for Waldenström’s macroglobulinemia. Out of curiosity, can you say how many patients you maybe see a day or in a week that have Waldenström’s?
Dr. Paludo: It’s variable these days, but I estimate about two to three patients a week with Waldenström’s and sometimes as many as five patients a day. We looked at this a few years back and to give some context, if you were to consider all practicing doctors in the US and all newly-diagnosed Waldenström’s patients in a year, each doctor will see a new case of Waldenström’s once every eight years. This gives you a sense of how rare diseases are very, very difficult to come across.
I want the patient to feel empowered that they can ask any question, no matter what it is, and bring up any concerns or fears that are important to them.
Dr. Jonas Paludo
Approaches to Personalized Care
Peter: You and Lisa have a very good doctor-patient relationship. In your experience, does each patient approach you differently? Do you have a different approach depending on what kind of interaction you have or what works best for that patient?
Dr. Paludo: My approach is different for each patient. The things that we always try to discuss and focus on are the main concerns that each patient brings to the visit, which can be different. If someone was recently diagnosed with Waldenström’s versus someone who’s reviewing, studying, researching, and now we’re talking about treatment, there would be some differences in how I approach each patient.
Managing Your Life with WM
Peter: Given that Waldenström’s is becoming more of a manageable disease, what is your guidance to patients when they first come to you as far as dealing with having a disease like ours? You have periods of requiring active treatment and periods of watching and waiting for the next shoe to drop, in a sense.
Dr. Paludo: It depends on the situation, but I’m always trying to discuss the key concepts related to Waldenström’s. We talk about follow-ups and treatment indications. I like to address that because they’re important for the patient, especially if they’re not coming to Mayo for their care.
At the end of the day, we always try to establish trust and an open space. I want the patient to feel empowered that they can ask any question, no matter what it is, and bring up any concerns or fears that are important to them. It’s difficult to do everything in one visit, although we do try, but sometimes we need several visits to discuss all of these.
Peter: That’s very commendable. That should be the model for all clinicians. Unfortunately, a lot of them are pressed for time or dealing with a large patient load, so they don’t make the extra effort, and you should be applauded for doing that.


WM Treatment Options
Peter: Lisa, you had some choices to make concerning treatment. Were you aware of the treatment options before you spoke to Dr. Paludo?
Lisa: Yes. The second oncologist I saw was supposed to be my first treatment opinion. When I started talking to her about the treatments, she said, “Gosh, you sure do know a lot about this. What do you think?” I didn’t get the first opinion that I was hoping for because I had done so much research that the oncologist felt that maybe I had a better sense of what treatment I should start with, which ultimately led me to a second opinion with Dr. Paludo.
I have done a lot of research, which I enjoy doing. It’s not a situation you want to be in, but I work in public health and public health strategy, so I enjoy strategy and research. I wanted to find out as much as I could about the treatment options. From the scientific papers, it’s not always clear. Actual patient experiences are something that’s missed in very scientific journal articles, which can only be shared through patient-to-patient experiences.
With Waldenström’s, that can be additionally challenging because we are each so unique. It’s a full-body disease that manifests differently. The symptoms are different from person to person. There are also fewer females with the disease and fewer people my age, so it can become more difficult to know exactly what to expect even though you do a lot of research.
What reduced my anxiety was talking to Dr. Paludo about being vulnerable about parts of the treatment that I thought were most concerning.
Lisa Ramirez
The Emotional Impact of a WM Diagnosis
Peter: You did a lot of research, but how were you dealing with it emotionally? How did it affect you when you were first diagnosed and how did you deal with the enormity of it?
Lisa: When I was first diagnosed, I was shocked. I knew I couldn’t have the conversation with my daughter that day, so she had a sleepover that night.
After that, I felt somewhat calm about it, even though I do have a history of anxiety disorder. I knew going into treatment that my outcomes would be better if my anxiety was reduced. Stress plays a huge role in your physical health in general, but especially as you undergo something as stressful as chemotherapy where you have a lot on the line.


I made sure to take care of my mental health through exercise and seeing a therapist weekly. What reduced my anxiety was talking to Dr. Paludo about being vulnerable about parts of the treatment that I thought were most concerning. I was able to talk in-depth about how I was concerned about a recurrence of my anxiety and eating disorders in the course of treatment.
Dr. Paludo was able to reassure me that, at any point in time, if I was having concerning symptoms, we could talk about it, but most of all, we could always stop treatment and take a different course of action. That option was never presented to me before by any of the oncologists I had seen. Having that way out and knowing that I had that autonomy was so reassuring and helped me get through a lot of rough times throughout treatment.
I had a pretty good treatment experience. It wasn’t always easy, but it was a lot easier knowing that I had the support of my oncologist to pivot, redirect, and find a different course of treatment that worked better for me. My quality of life was most important to both of us.
Peter: That focus on quality of life is critical. Every patient’s different, both physically and mentally, and it’s important to treat both aspects of how a patient approaches their disease.
Important Takeaways from Initial Consultation
Peter: Dr. Paludo, when you see a patient, what do you want patients and care partners to take away from that initial visit with you? What do you want them to understand?
Dr. Paludo: One of my priorities is to have patients understand that treatment for Waldenström’s is not a sprint but a marathon. It’s a long-term process that involves long-term planning, and we have to consider all short- and long-term strategies for treatment.
I usually say that when you’re getting treatment, you’re not in a long-term commitment. You can always stop and find a different option. I also like to discuss, usually in broad terms, that what we have today for treatment options has an overall similar efficacy. They are different in potential side effects, logistics, duration, and frequency. That often allows patients to focus on the implications of the treatment on their quality of life and their goals.
Once we remove the efficacy piece from the discussion, we can talk more about side effects and logistics. We can focus on how the treatment can help patients achieve what they want at the end of the day, which is improved quality of life, and accomplish what’s important to them. Those are things that I always like patients to take away from those initial discussions about treatment options before even we decide on which treatment to go next.
Lifestyle Changes in the Face of a WM Diagnosis
Peter: Lisa, you wanted to make sure you had a good quality of life. After you were diagnosed and started treatment, did you do anything different? Did you make lifestyle changes to help you emotionally and physically?
Lisa: Absolutely. Dr. Gertz said that frailty is the enemy, so I immediately got a personal trainer and hit the gym. People train for marathons. This is the rest of my life. I don’t want chemotherapy to knock me down. I need to be as fit as possible.
I also participated in an educational session on nutrition through The Leukemia & Lymphoma Society and met with a nutritionist. I changed my diet to reflect some of the recommendations based on those talks. I’m eating more of a plant-based diet and building up my strength as I approached treatment knowing that treatment was inevitable.
I saw a therapist weekly, which ultimately helped. During chemotherapy, I didn’t miss any work. I remained very active. I was still able to dance. I wasn’t allowed to skateboard anymore, but I was still exercising as much as I could to fight the fatigue and it paid off. That makes a big difference in terms of how one feels during the course of treatment and your ability to be resilient and make good progress in treatment.
Peter: I agree completely. It’s important to move. A lot of patients say that their treatment has debilitated them, but I tell them to try to move a couple of feet and take a couple of steps a day and build on it. It does make a difference.

Maximizing Your Quality of Life
Peter: Dr. Paludo, do you have any follow-up advice for Waldenström’s patients on how to deal with quality of life issues? Can they continue to live like they did before they had WM?
Dr. Paludo: Absolutely. It’s always difficult to cope with a new diagnosis of any cancer, including Waldenström’s. Every patient is a little different on how they try to cope. I try to understand what’s important for each patient and focus on what we can do to control what we can.
With Lisa, dancing was very important. We couldn’t control when treatment was needed, but we could control that she could continue to dance. It would be a form of exercise that helps her cope and keep some form of normalcy. Life can be disrupted with diagnosis and treatment, so trying to keep as much of a normal life as possible after diagnosis or when you’re going into treatment is very important. As you go through the watch and wait period with Waldenström’s before treatment or in between treatments, it’s very possible to live life like before as much as possible.
I’m not a mental health expert, so I also look for help. I refer my patients to cancer therapists and psychologists. The team we have at Mayo Clinic helps. I play within my limitations and always look for help from others who know more than I do about topics that are very important for every patient.
Patient Advocacy
Peter: Lisa, you’ve advocated for yourself right from the start. What would your advice be to newly-diagnosed patients or even those who are even in remission?
Lisa: For newly-diagnosed patients, get connected with IWMF. I was so impressed with the resources available for such a rare disease. It’s honestly very impressive how well IWMF is organized.
If you’re a young person or under 50, it can be more challenging because it’s almost a different disease. When you have young kids at home, there are a lot of different things to consider. Getting connected with the IWMF support group for young people was helpful. Find support with people in your community.
Watch lectures and read all the resources available sooner rather than later. You have some time to figure everything out. If you’re newly diagnosed and you don’t have symptoms that require immediate treatment, you have time to research.
It’s necessary, I would say also, to look at the different cancer institutes that have different philosophies. When you’re listening to lectures from different experts, find who resonates with you and what makes sense to you. Who do you seem to align with in terms of what feels right for you and what you value?
Take time to consider all that’s important to you so that you can locate the physician and your team that you’re hopefully going to be with for the rest of your life, working on achieving a good quality of life while living with this disease. Take in all the information, talk to your support network, and connect.
At first, I thought that having Dr. Paludo as my primary oncologist was not possible, but you may be surprised at what is possible so have hope and advocate for yourself.
It’s great to have an external brain to help process the information and to reflect back to you.
Lisa Ramirez
The Role of Care Partners
Peter: You approach each appointment with knowledge beforehand, you do your research, and you advocate for yourself. Do you go to your appointments on your own or do you take a care partner with you? You read that someone should always have someone else with them because they can mishear something. How do you manage that?
Lisa: I have a great partner and support. You’re absolutely right. Sometimes it can be overwhelming. When I would go to appointments with a different provider, I’d walk out sweating and notice I was so nervous during the appointment. Having someone there can be helpful. When I went to treatment, my partner would go with me. One time, my sister went with me.
Sometimes, you get disappointing news. I oddly got disappointed that I couldn’t do chemo a couple of times and I got upset and emotional, so to have someone to provide emotional support is helpful. It’s much better to not have to do it alone.
But if you are alone, there are people who are there to support you. At Mayo Clinic, there’s a whole team. Everybody there is supportive, so you can do it alone. It’s great to have an external brain to help process the information and to reflect back to you. Maybe you didn’t even notice that you weren’t feeling comfortable with a certain provider. It’s helpful to have someone to bounce off, so it’s important to have someone with you.

Peter: Dr. Paludo, what’s your advice in that regard? Do most patients come with someone to the appointment? And do you suggest it to patients if they don’t?
Dr. Paludo: Most patients come to their appointments with someone else. That’s very helpful and very important, if possible, of course. It’s difficult to take people away from their normal day-to-day lives, but it helps to have someone else also listening. We usually don’t remember everything that is discussed. Each person may remember different parts of the discussion. It helps, so I encourage that if possible.

Living with WM
Peter: Lisa, you’ve been living with Waldenström’s for a few years now. How do you not let Waldenström’s consume your everyday life? What’s your approach to living with it?
Lisa: In the beginning, it was difficult to not let it consume my life. For me, planning out a theoretical course of treatment to last my whole life was helpful. What helped was having that plan in place and also having a plan when I didn’t have symptoms or symptoms that I thought were bothersome to me.
Having those things mapped out in advance allows me to trust the plan and not have to think about it in my daily life. Once those decisions are made for the future, I can always change my mind at any point, but to have that mapped out for myself allows me to forget that I have Waldenström’s and live my life. It might take a minute to get there.
At first, it’s consuming. You’re consumed with the research. Don’t overreact. Take your time. Talk with your oncologist about a plan, put a plan in place, and then put it aside and live your life. Ultimately, treatment is all about having a good quality of life and living your life normally. You want to be able to do that and not add any additional stress to yourself. Putting a plan in place, putting it aside, and referring back to it when you need to is important.
Talk with your oncologist about a plan, put a plan in place, and then put it aside and live your life. Ultimately, treatment is all about having a good quality of life and living your life normally.
Lisa Ramirez
Waldenström: The Patient-Physician Relationship
Peter: Right from the start, you had a good relationship with Dr. Paludo. How has that evolved over the past few years? Is it different now than it was initially?
Lisa: Dr. Paludo has been very consistent. Initially, I met with him before I even met with who I thought was going to be my primary oncologist. I walked away from that conversation saying, “Gosh, I met the right oncologist for me. Too bad. I can’t possibly get treatment in Minnesota.”
It felt like a good fit from the beginning and we’ve built upon that trust. I instantly felt comfortable and felt trust. He engaged with me in a way that was strength-based and not over reactive. He’s very steady. Our relationship hasn’t changed much other than we’ve been through this treatment together and there’s a deepening of trust.
I’ve talked about my next treatment episode with my partner and when I have to do the weekly treatment, we’re going to live in Minnesota for six months. There’s no question about that. I know Dr. Paludo’s there for me and he’s my oncologist until the end, so I feel very comfortable with that.

Key Takeaways
Peter: Dr. Paludo, do you have any key takeaways for patients or healthcare providers in building and sustaining a strong relationship through the cancer journey?
Dr. Paludo: Advocate for yourself. Go after what you think is important for you. Lisa and I are on the same page. For the healthcare providers, what’s very important is to actively listen to each patient’s priorities. Listen and not just hear. Pay attention and focus on what’s important for each patient, like their main concerns and fears.
As providers, we have to be frank and honest with the limitations of what we know and what we don’t know about Waldenström’s. There are a lot of things that we know now that we didn’t know before, but there are a lot of questions that we can’t answer yet. Being honest with our limitations, paying attention, and focusing on what is important to the patient help build that trust, which is important in a relationship. We’re all going together through good and not-so-good moments in this long journey of Waldenström’s.
Being honest with our limitations, paying attention, and focusing on what is important to the patient help build that trust, which is important in a relationship.
Dr. Jonas Paludo

Peter: It’s good to see you’re both in agreement. You’re both following the proper path and I applaud both of you, especially for taking the time to share your experience with healthcare providers and patients.
Lisa mentioned that she first did a good bit of research through the IWMF website. I did that myself 20 years ago. I was a youngster back then and the services and support they provided meant so much to me that I started volunteering for the organization and I’ve been with them since then.
Waldenström’s is a rare disease, so you don’t encounter many people who have it, so finding an online community was of great benefit. Sharing stories with them, joining support groups, taking part in discussions, viewing webinars, and going to their annual educational forum are key components of becoming a more knowledgeable patient.
Before we had the technology, I would have my own chart that I would give to my doctor and say, “Here are my trends.” He would laugh at me, but he would look at it. We had a great relationship and that’s important to have. Be educated about your disease, know your options, what your preferred lifestyle, and what you want in quality of life, and pick a doctor who fits well.
Lisa: My therapist thinks Dr. Paludo is great. She’s convinced he took some classes in psychotherapy. She’s got great admiration for him. I’m also trained as a therapist and I would say Dr. Paludo has those skills, but please don’t leave the work you’re doing to be a therapist, although you’d be a great one.
Mayo Clinic is huge and yet after every visit, I would think, “How is it possible that each person on my care team was able to spend that much time with me?” I’ve never encountered that anywhere else. How is it that nurses remember me? People remember me. We had little inside jokes. Those things matter so much.
Our healthcare environment is changing. There’s limited time with patients. We’re speaking to healthcare institutions and I don’t know how providers get reimbursed and what expectations are in general.
Physicians want to have these kinds of relationships with their patients and perhaps there’s a larger pressure that prevents them from doing so. I hope that we can get back to that. Institutions like Mayo Clinic and physicians like Dr. Paludo give me the hope that it’s possible to have those kinds of relationships with patients in the current healthcare environment somehow.
Dr. Paludo: I don’t think I can say it better. It’s important to keep in mind what the priority is, which is the patient and what matters to that patient. Always keeping that in mind is the goal at the end of the day.


Conclusion
Peter: I enjoyed this discussion. It’s always good to meet with a fellow WMer and a noted, world-renowned Waldenström’s clinician and researcher. I’m very grateful for both of you for sharing your time. I hope others find this information very useful and beneficial as much as I did. Thank you both and thanks to The Patient Story.
Tiffany: Thank you, Pete, Lisa, and Dr. Paludo for an engaging discussion. It is so crucial to be empowered so that you and your caregivers can make informed decisions about your care.
Thank you to our partner, The Leukemia & Lymphoma Society (LLS). Make sure to visit their website, particularly their Information Resource Center, which provides free one-on-one support. Thank you to the International Waldenstrom’s Macroglobulinemia Foundation (IWMF), which has over 60 peer support groups worldwide where they share experiences, discuss concerns, and exchange information.

Special thanks to The Leukemia & Lymphoma Society and the International Waldenstrom’s Macroglobulinemia Foundation for their partnership.
Waldenstrom’s Macroglobulinemia Patient Stories
...
Pete D., Waldenstrom Macroglobulinemia
Symptom: Irregular blood test results during a regular workup for Crohn’s
Treatments: Chemotherapy, surgery, radiation, monthly IVIG
...
Sheree N., Waldenstrom Macroglobulinemia
Symptom: Feeling anemic
Treatment: Chemotherapy (bendamustine & rituximab)
...





