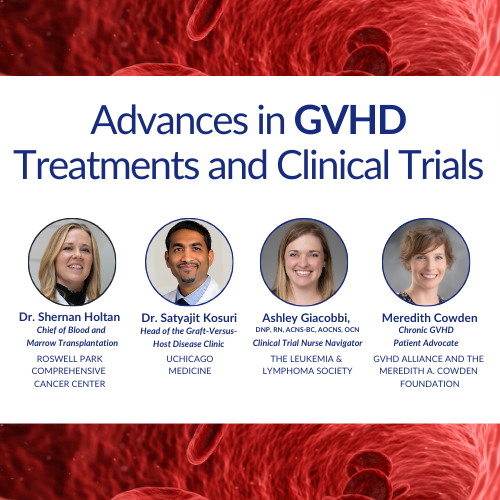
Advances in GVHD Treatments and Clinical Trials
Edited by:
Katrina Villareal
Graft-versus-host disease is a potentially life-threatening condition affecting an estimated 50% of blood cancer patients who receive stem cell transplants from a donor. Transplant experts explain GVHD risks, how to watch for symptoms, the current treatments available, and new clinical trials aimed at prevention and treatment.
Watch the Full Webinar
In addition to our summary from this empowering webinar, watch the full video replay and catch every word from the experts and patient advocate!
Patient advocate and GVHD Alliance co-founder Meredith Cowden shares her experiences with GVHD. Experts from UChicago Medicine, Roswell Park Comprehensive Cancer Center, and The Leukemia & Lymphoma Society who are on the front lines of GVHD research and treatment discuss the role clinical trials play in advancing the treatment landscape and what it could mean for you. Discover how to take steps to learn more about clinical trials from a clinical trial nurse navigator.

This program is brought to you by The Patient Story in partnership with The Leukemia & Lymphoma Society.
- Introduction
- Understanding Graft-Versus-Host Disease (GVHD)
- Current GVHD Treatments
- Challenges of Existing Options for Managing GVHD
- Clinical Trials for GVHD
- Enrolling in GVHD Clinical Trials
- Nutrition & Exercise When You Have GVHD
- Areas Requiring More Research & Gaps in Transplants & GVHD
- GVHD Treatments Final Takeaways
- Conclusion
Introduction
Stephanie Chuang, The Patient Story
Stephanie Chuang: I’m a blood cancer survivor myself and started The Patient Story out of my own experience. I felt so alone. I wanted to know what it meant after diagnosis and how we could get through it. As we know, a diagnosis is just the beginning of figuring things out. Our goal at The Patient Story is to help patients and care partners navigate life after a cancer diagnosis, primarily through in-depth conversations with patients, care partners, and top cancer specialists.
We are so proud to partner with The Leukemia & Lymphoma Society, the largest nonprofit dedicated to creating a world without blood cancers. For decades, they have invested almost $2 billion in groundbreaking research and pioneering so many approaches. On top of that, they also support patients and families with programs like the Clinical Trial Support Center, which provides free one-on-one support with nurse navigators.
This program is not meant to be a substitute for medical advice, although we hope that you walk away feeling like you have more to ask your own medical team.


Satyajit Kosuri, MD
Stephanie: Dr. Satyajit Kosuri is a hematologist-oncologist with the University of Chicago Medicine. He is an expert in stem cell transplantation and leads the Graft-Versus-Host-Disease Clinic and the research in trying to improve patient access to transplants. Dr. Kosuri, what drew you to this field of medicine and specifically GVHD?
Dr. Satyajit Kosuri: When I started my oncology fellowship, I was going to be a genitourinary oncologist and I was very much set. When I did my transplant rotation, what drew me was that it spanned all fields of medicine, so you had to continue to have a pretty good breadth of knowledge. The immunology was very, very intriguing. We’re dealing with very complex diseases as well as the transplant itself, which is basically an immune system transplant.
When I tell patients, family members, fellows, and trainees about the field of transplant, I tell them, number one, I’m an immunologist, number two, I become an infectious disease doctor, and then, number three, oncology comes in as part of the triad. That’s what drew me to the field and what I find very interesting. Graft-versus-host disease is part of the entire picture that we’re trying to improve upon within the context of transplant.
Shernan Holtan, MD
Stephanie: Dr. Shernan Holtan is a hematologist-oncologist with Roswell Park Comprehensive Cancer Center in Buffalo, New York. She is the chief of the Blood and Marrow Transplantation and has led so many clinical trials in GVHD. Her research has led to the discovery of the amphiregulin (AREG) biomarker for monitoring graft-versus-host-disease. Dr. Holtan, what drew you to medicine and specifically focus on graft-versus-host disease?
Dr. Shernan Holtan: My story is a lot like Dr. Kosuri’s. In medical school, I was most interested in rheumatology, infectious disease, cancer medicine, critical care medicine, dermatology, and plastic surgery. I thought, How am I ever going to pick between these different specialties? I loved cancer reconstruction and the connection with patients going through cancer and giving them hope after a devastating diagnosis.
On a whim, I took a rotation on the BMT service, in part because it sounded cool. The other part of it is you didn’t have to work weekends and as a very tired fourth year med student, I was excited about that. I was stunned. It was every great aspect of medicine rolled in one specialty, so I was sold and never looked back.


Meredith Cowden, Patient Advocate
Stephanie: Meredith Cowden is a chronic GVHD patient advocate and co-founder of the GVHD Alliance. Why did you decide to dedicate your life to advocating for so many other people with GVHD?
Meredith Cowden: I had acute myelogenous leukemia (AML) at 19. Chemotherapy wouldn’t completely work, so I needed a bone marrow transplant. Shortly after, I developed acute graft-versus-host disease and then I developed chronic graft-versus-host disease, which I’ve had since April 2002.
Graft-versus-host disease is rare and we’re spread out all over the place, so it’s isolating and hard to find resources, information, and even the appropriate treatment team.
I originally wasn’t into the patient advocacy world. I didn’t want to deal with it anymore, but I didn’t want anyone else to have to deal with it. I got angry and frustrated, and frustration is one of the greatest motivators for me. When I would talk to other patients, there was a sense of relief and comfort they felt in talking with somebody who could understand their experience. From that point, I thought that this is where I need to be.
Ashley Giacobbi, Clinical Trial Nurse Navigator
Stephanie: Ashley Giacobbi is a clinical trial nurse navigator with The Leukemia & Lymphoma Society. Can you describe the work that you do with the Clinical Trial Support Center?
Ashley Giacobbi: I am a nurse navigator with The Leukemia & Lymphoma Society’s Clinical Trial Support Center. We provide individualized clinical trial searches and clinical trial resources to patients with blood cancers or patients who have had blood cancer in the past but may be managing long-term effects of their disease or treatment.
We provide one-on-one connection with patients, caregivers, and their healthcare providers. We take the time to learn about a patient’s diagnosis, past treatment, and other medical conditions that could play a role in their eligibility for clinical trials. Most importantly, we take the time to learn about patient and caregiver preferences and any unique obstacles that may hinder or support their participation in a clinical trial, so that we can target the support that we’re able to offer and give personalized resources.

When immune systems grow suspicious, they’re programmed to do one thing and that is to attack. This new immune system can attack the recipient from the inside.
Dr. Satyajit Kosuri
Understanding Graft-Versus-Host Disease (GVHD)
Stephanie: Dr. Kosuri, what is GVHD?
Dr. Kosuri: When we’re doing a stem cell transplant or bone marrow transplant, we’re doing an immune system transplant. When we’re healthy, the immune system protects us, whether it’s getting rid of bad cells or protecting us from various infections. It considers the body that it’s growing up in as its neighborhood, so it has an inherent desire to protect its neighborhood and recognizes the body that it’s in as being part of itself. When there are things that are not supposed to be there, it recognizes them and gets rid of them.
We’re taking the stem cells from a person with a healthy immune system and putting them into the transplant recipient, so this immune system is growing inside of a new neighborhood. For the most part — and this is where matching comes into play — it recognizes its new neighborhood as its own and leaves it alone. It takes up the mantle of, “I’m going to protect this body and eradicate any leukemia cells,” and that’s the graft-versus-leukemia effect.
But sometimes, there are parts of the new neighborhood that are not what it’s used to, so it starts to grow a little bit suspicious. When immune systems grow suspicious, they’re programmed to do one thing and that is to attack. This new immune system can attack the recipient from the inside, which can lead to some inflammatory physical damage to the patient or the recipient of the stem cell transplant.
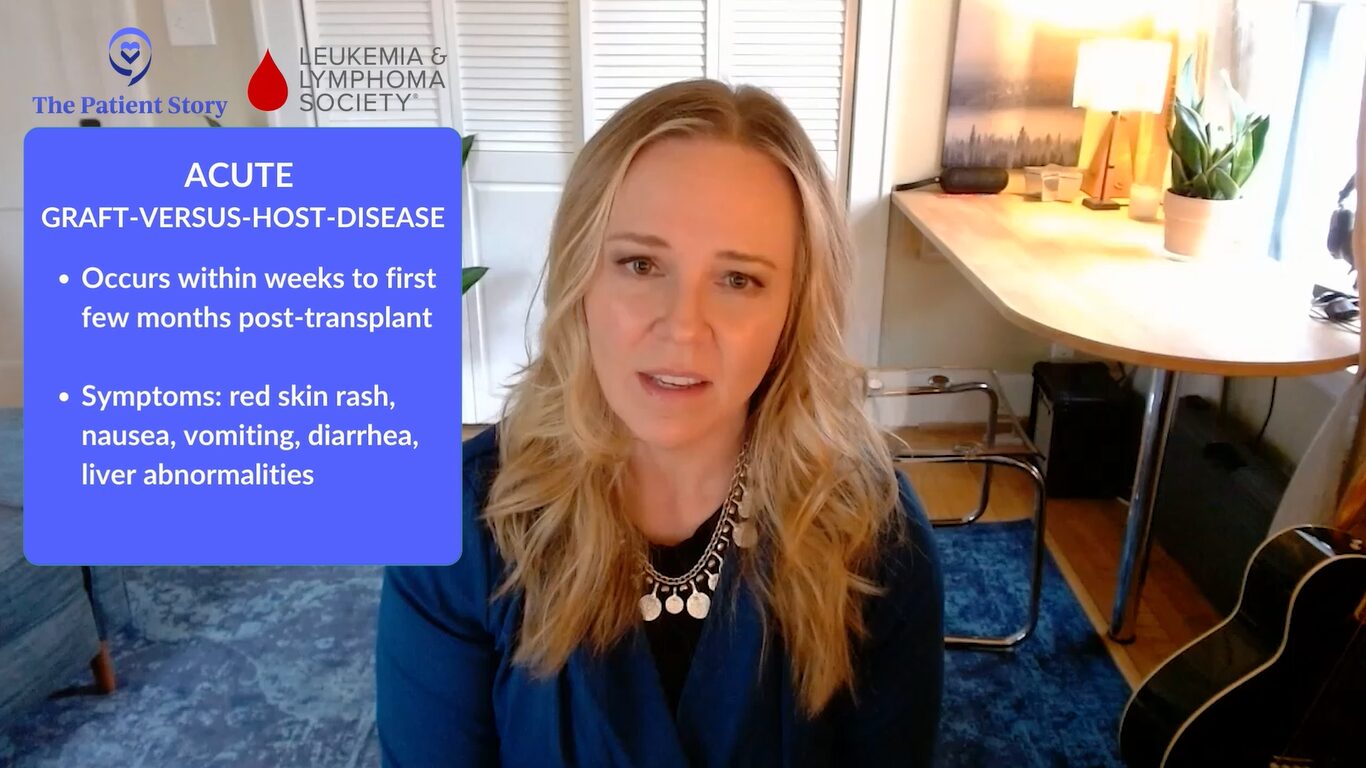
Types of GVHD
Stephanie: Dr. Holtan, what are the main types of GVHD? How do they differ and what are some of the common symptoms?
Dr. Holtan: We mainly think of graft-versus-host disease in two phase although there can be some overlap between the two.
Acute graft-versus-host disease happens within weeks to the first few months post-transplant and that has a particular pattern. Most of the time, it’s a red skin rash, but sometimes it can also lead to nausea, vomiting, diarrhea, and liver abnormalities that we might see on blood tests. There’s a very clear time during which this develops and a pretty clear clinical presentation, so it’s pretty easy to determine what it is.
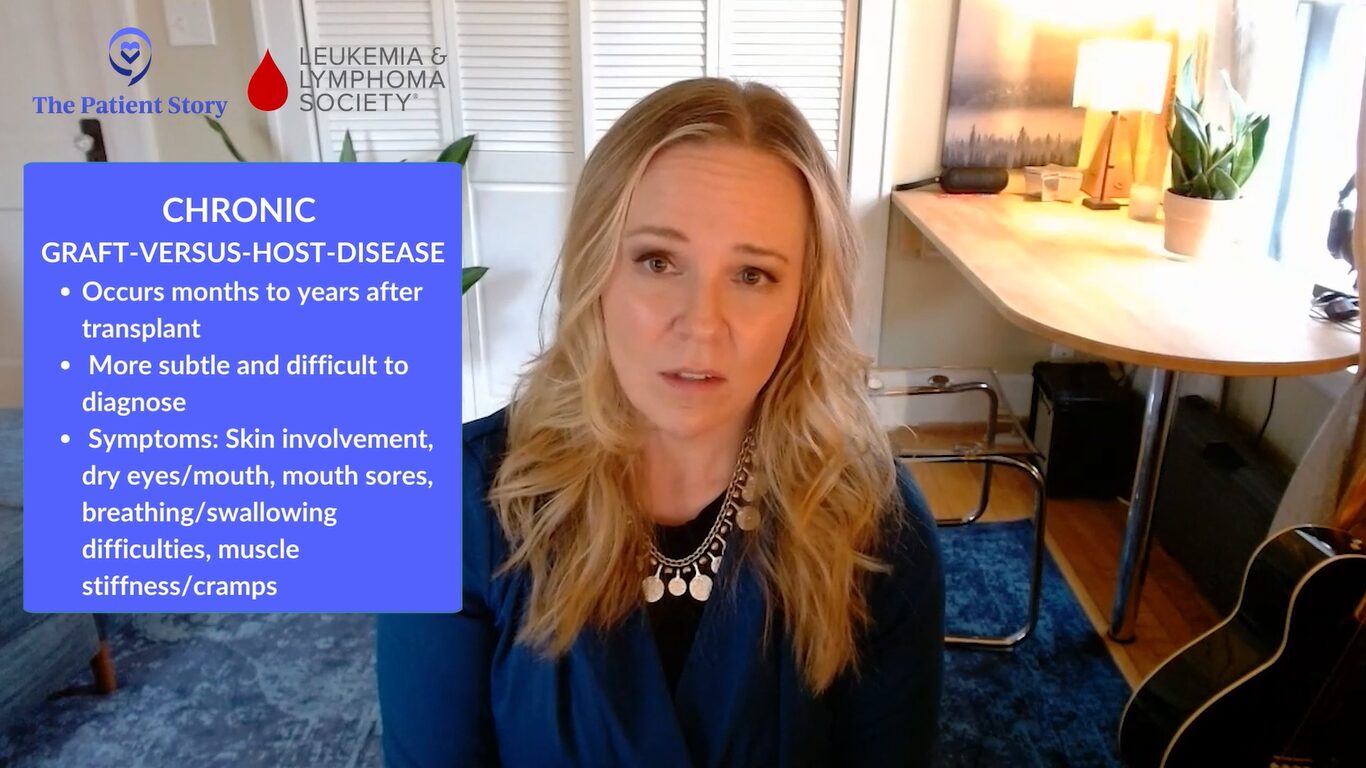
Chronic graft-versus-host disease typically happens later in the months to years after transplant. It can be more subtle and difficult to diagnose. As Dr. Kosuri was saying, this is primarily an inflammatory reaction at the beginning, which ultimately will gradually lead to scar tissue.
Think of a wound that is having some difficulty healing. There’s a lot of inflammation and the body tries to stop that inflammation by putting a scar on top of it. This can happen in almost any organ in the body. Usually, the skin is involved, but it can also cause dry eyes, dry mouth, mouth sores, difficulty breathing, difficulty swallowing, changes with the muscle tissue fascia, and making people feel stiff and have muscle cramps. Any organ can be involved with chronic graft-versus-host disease.
Even though we think about chronic manifestations as a later problem after transplant, we can see some of those changes even within the first few weeks.
Dr. Shernan Holtan
Stephanie: Dr. Holtan, when does it technically turn from acute to chronic? Is there an official time where now we know it’s chronic? Is there a general time frame?
Dr. Holtan: There isn’t an official rule. When Dr. Kosuri and I were in training, we were taught that acute graft-versus-host disease happens before Day 100 and chronic GVHD happens after Day 100, but that’s not really true. The biologic processes can happen at any time post-transplant. Acute GVHD usually happens in the first few weeks to months, but we have even seen acute manifestations of GVHD happen much later.
Even though we think about chronic manifestations as a later problem after transplant, we can see some of those changes even within the first few weeks. The lines are blurred now, so we describe graft-versus-host disease based on its symptoms and appearance rather than time frame post-transplant.
It took a while before my doctors said I had GVHD because they were thinking it was something else. Over the years, I’ve had a variety of different manifestations of chronic GVHD.
Meredith Cowden
Meredith’s GVHD Story
Stephanie: Meredith, what was it for you in terms of those first symptoms? At what point did you realize that this was not going away?
Meredith: In the beginning, I noticed that I had a couple of different things going on at the same time. My stomach started to bother me a lot and I got very nauseous. It was hard to find food that I could tolerate and that was appetizing. I had some gastrointestinal issues going on. I also developed a rash. I’m naturally a pasty pink person, but my skin got red and burned, so it was hard to wear clothing.
When I received treatment, the issues started to get resolved, but then it started to transition. The GI issues didn’t necessarily go away but they changed and my skin got a little bit different.
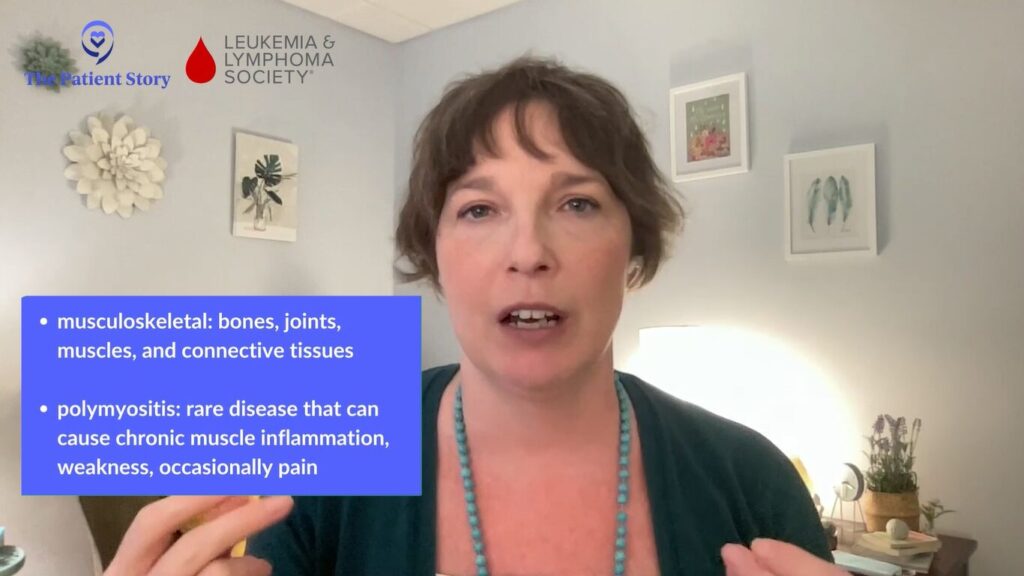
I had musculoskeletal involvement. I developed polymyositis, so there was a lot of pain. I was very weak and couldn’t move around a lot. I lost muscle mass. It took a while before my doctors said I had GVHD because they were thinking it was something else. Over the years, I’ve had a variety of different manifestations of chronic GVHD.
Dr. Kosuri: Chronic graft-versus-host disease can affect multiple sites in a way that may be difficult to initially pick up. I’ve gotten feedback from patients that what they’ve found helpful is when I describe chronic GVHD prior to the transplant.
I ask them to imagine taking all the autoimmune conditions and rolling them into one and putting them inside a human body. Those are ways that chronic GVHD can manifest, whether it’s dry eyes, a scleroderma type presentation, or pulmonary fibrosis. It’s a great mimicker.
Stephanie: It sounds like it might be hard to identify quickly if people aren’t speaking up too and share the different things that you’re experiencing and communicating openly with your doctor.
There are many different types of complications, but infection comes to the forefront.
Dr. Satyajit Kosuri
Severe Complications in GVHD
Stephanie: I don’t know if there’s difficulty in noticing what the severe complications are, but, Dr. Kosuri, are there any that you’d like to highlight?
Dr. Kosuri: There are complications of the entity itself and then there are complications that will arise from the treatment or the way we try to treat the disease. GVHD in and of itself is an immune dysregulation. The immune system that’s supposed to behave in a certain way is misbehaving or it might be turned on and can’t really control itself. What happens in this state?
There are many different types of complications, but infection comes to the forefront. We prioritize monitoring patients who have graft-versus-host disease not only from the GVHD itself but also from the medications that we use to try to quell the inflammation and calm things down. Both can lead down the pathway of bringing down the level of protection that the human body has as it’s starting or trying to recover from the stem cell transplant.
One of the things that we emphasize for patients is if they’re feeling unwell in any way, shape, or form, they have to let their transplant providers know very quickly. That way, whatever suspicion we may have, we can diagnose and take care of it very quickly. If it’s a small infection, we can treat it and it doesn’t become a big infection.
Be very proactive and very compliant with the medications. Patients take 20 different medications after a transplant and sometimes it’s hard to take all of them, especially when the pills are big. We hear that as one of the main complaints. We make sure that patients are on antiviral medications, antifungal medications, and a medication to protect them from PJP (pneumocystis jiroveci) pneumonia. These help protect and almost substitute in a way because the immune system is not online early on and when you have graft-versus-host disease, it’s not behaving the way that it’s supposed to.
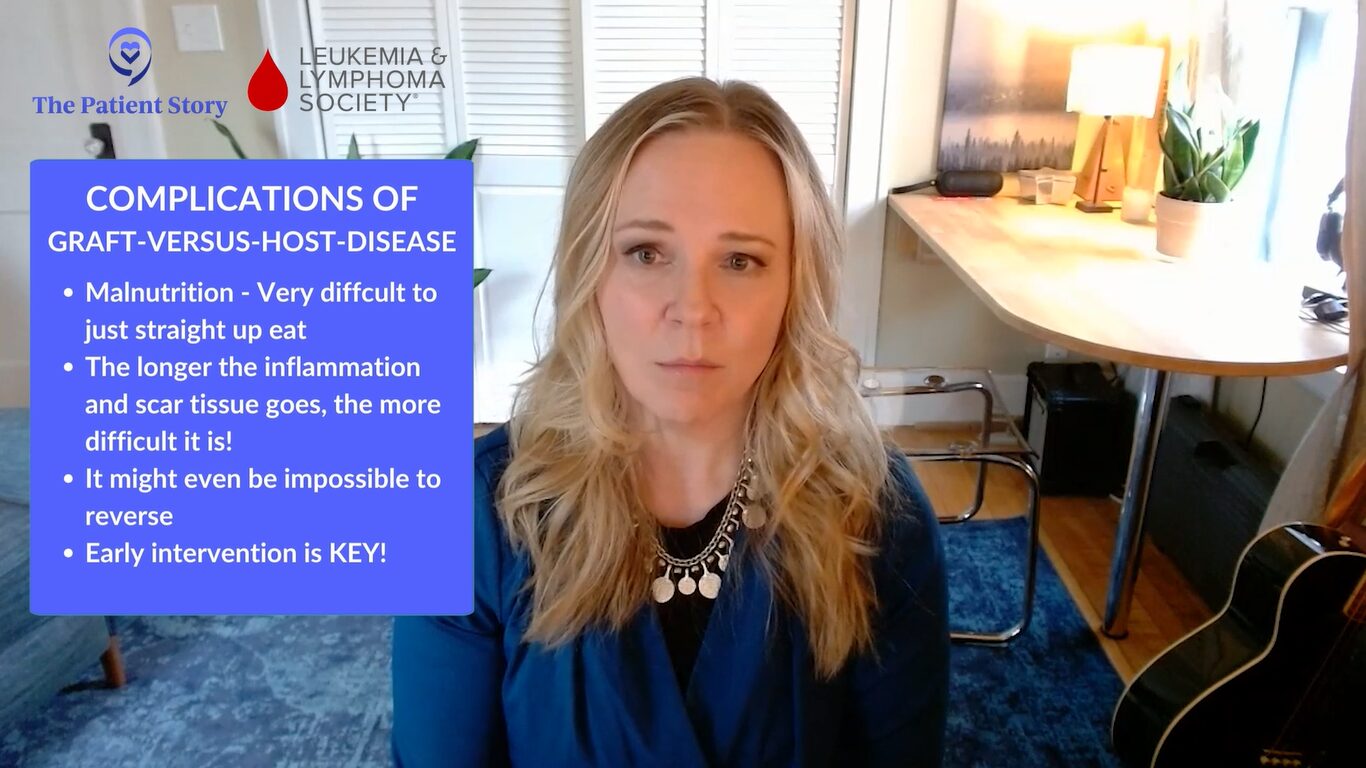
Dr. Holtan: We certainly know that graft-versus-host disease can affect different organs and tissues, and that the treatment can have just as many toxicities as GVHD itself. Some of the most challenging issues we run into are malnutrition, straight-up difficulty eating, all the way to impaired organ function.
What Dr. Kosuri mentioned is key about notifying for changes in symptoms with chronic graft-versus-host disease. You want to intervene before there’s permanent damage. The longer the inflammation and scar tissue goes, the more difficult it is or it might even become impossible to reverse. Early intervention is necessary to try to avoid permanent damage.
If there’s anything that seems even a little bit wacky, ask. There’s no harm in asking. It’s one of the best ways to take care of yourself.
Meredith Cowden
Stephanie: From your own patient experience, did you know that you could bring these up to your doctor? Do you feel that patients you talk to know that they can do that? What do we need to do to make sure that this is happening?
Meredith: I was diagnosed at 19. I was young and there were things I learned over the years. This might sound naive and silly, but there were things that I thought were completely normal but were actually symptoms of GVHD.
Over time, I’ve developed strong relationships with each member of my care team, so I’m very comfortable saying, “This feels weird. I don’t know about this. Can you look at that? Check me out please.” To have that kind of conversation, you have to build that relationship so that everyone is comfortable and can have a discussion with one another even when they have differing opinions. You can get more out of that conversation than if a typical patient-doctor exchange. Oftentimes, things get missed that way.
For patients, treat your doctors like people. Be friends with them. You’re going to be with them for a long time. They want to help you. If there’s anything that seems even a little bit wacky, ask. There’s no harm in asking. It’s one of the best ways to take care of yourself. For the providers, it’s a good idea to ask patients to do a quick scan of their body to get the whole picture because it’s easy to forget stuff. Is there anything that’s going on that we haven’t touched on that you noticed?
The backbone of therapy for both acute and chronic GVHD is corticosteroids.
Dr. Satyajit Kosuri
Current GVHD Treatments
Stephanie: Dr. Kosuri, what are the current standard treatments for GVHD?
Dr. Kosuri: The keyword is current because this is something that’s changing and we hope will continue to change as we go through the years.
The backbone of therapy for both acute and chronic GVHD is corticosteroids. Many patients and their family members will have heard of the medication called prednisone or various types of the steroid.
The degree of the GVHD matters. If you have a mild, acute graft-versus-host disease, this could be potentially managed with topical corticosteroid. As it becomes more severe or involves more organ systems or more of the skin, we start graduating from topical steroids to systemic steroids.
Depending on where we are in the transplant process, our patients will already have been on another immunosuppressive agent, like tacrolimus, sirolimus, or cyclosporine. The goal is to treat with steroids plus or minus this other agent and then taper them off once we have a response.
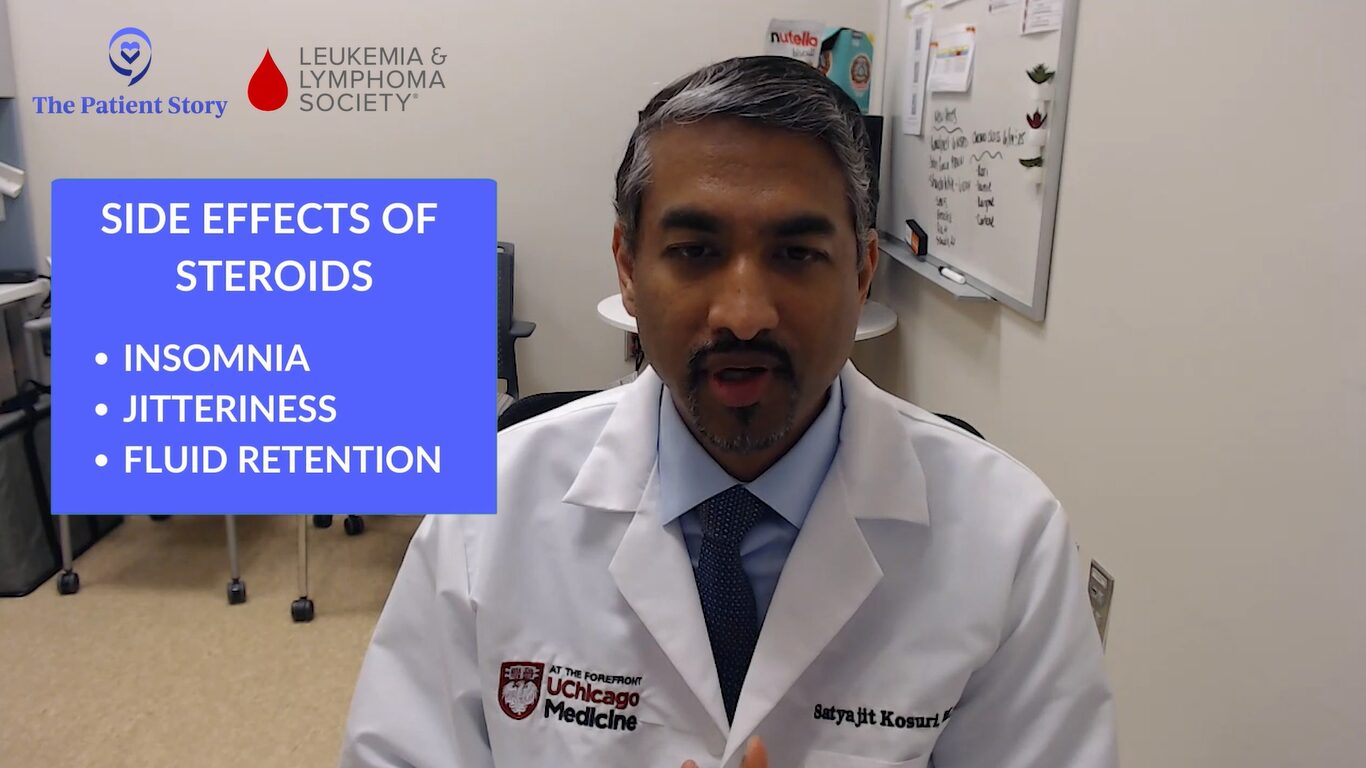
With steroids, over a period of time, you can accumulate some of those side effects that we don’t like to see in patients, like insomnia, jitteriness, and fluid retention. Those are for people who are in the category of steroid-responsive.
Another category of patients are those who are steroid-refractory, which is where the graft-versus-host disease may be a little bit more sticky and not respond to steroids, or steroid-dependent, where patients are unable to get off steroids. In those cases, we go further down on immune suppression choices. There are other medications available. One that’s FDA-approved and works for both is ruxolitinib. There are also other various options. That becomes more of a longer term treatment.
There isn’t a blood test that can diagnose graft-versus-host disease right now, but we can use biomarkers to help us understand the severity of the immunologic reaction and how much damage has been done.
Dr. Shernan Holtan
Challenges of Existing Options for Managing GVHD
Stephanie: Dr. Holtan, what are some of the key limitations or challenges with the existing options for managing GVHD?
Dr. Holtan: The greatest challenge is understanding how much therapy to give for graft-versus-host disease. We base our treatment upon the severity of symptoms, but that isn’t adequate. There are still some patients that we are over-treating and some patients we are under-treating.
This is where the role of biomarkers can come in. There isn’t a blood test that can diagnose graft-versus-host disease right now, but we can use biomarkers to help us understand the severity of the immunologic reaction and how much damage has been done internally that we can’t detect clinically. This is a huge challenge because even though we examine patients fully and they reveal all their symptoms, we still can’t know how bad things are, so biomarkers can support us in helping to guide that therapy.
This is particularly under investigation right now using biomarkers such as ST2 (suppressor of tumorigenesis 2), REG3α (regenerating islet-derived 3-alpha) known as the MAGIC (Mount Sinai Acute GVHD International Consortium) biomarkers, and then the one that we developed at the University of Minnesota, amphiregulin or AREG. Both of these biomarkers can be used to understand how severe the graft-versus-host disease is.
I have patients who have had severe infections of the GI tract, like C. difficile colitis or viral gastroenteritis such as adenovirus gastroenteritis. An allogeneic transplant recipient might have these infections and we’ll treat the infections, but they’ll have persistent severe diarrhea so you won’t know if you’re still dealing with the infectious process and the healing that has to occur or if graft-versus-host disease developed as a result of the immune system trying to target the infections. Even a biopsy can’t always tell you this, but we can use biomarkers, especially amphiregulin, to help sort this out.
When we’re treating patients with these symptoms, it’s almost like it’s graft-versus-host disease until proven otherwise.
Dr. Satyajit Kosuri
I had a gentleman who had severe adenovirus gastroenteritis and was having 15 to 20 bowel movements a day. We used an amphiregulin test to know if this could be graft-versus-host disease. The result was normal. It was not elevated. I continued to check every week because his gastroenteritis went on for a long time, even though we treated it.
Clinically, he had weeks of diarrhea, but we followed that test every week and the number was always low, so we never gave him prednisone. If I didn’t have this reassurance, someone might say it’s GVHD. It took some time, but he made a full recovery. This is how we can use these biomarkers to help support our clinical decision-making. We need more trials along these lines because the real world is messy.
Dr. Kosuri: I can’t emphasize how important what Dr. Halton is mentioning because oftentimes in transplant medicine, we’re operating in the gray and we have to make guesses. Sometimes when we’re treating patients with these symptoms, it’s almost like it’s graft-versus-host disease until proven otherwise. When you have that type of thought process, it can be difficult and we can actually hurt the patient with the GVHD management in and of itself.
The example that Dr. Holtan mentioned, most transplant physicians would say, “This has to be GVHD and we have to give them prednisone,” and that could lead to other infections or it can worsen the infection the patient already has. We get into these situations that are difficult to manage and if we have something like these biomarkers, it can make our lives as well as the patient’s life much easier and with less toxicity than what we would say is the normal kind of approach.
We had no human data to support how we manage steroid-refractory GVHD. Out of decades worth of work, there were no studies.
Dr. Shernan Holtan
Stephanie: A lot of this is addressing the symptoms that come with GVHD. This may be a rookie question, but I’m trying to understand. Is there research going into how to address the drivers of what’s happening with GVHD?
Dr. Holtan: We know what causes graft-versus-host disease. The donor T cells are attacking tissues and organs. However, we can’t always tell when that attack is over. The whole field of steroid-refractory graft-versus-host disease has developed out of an assumption that the T cell-mediated attack is still happening, so all trials for steroid-refractory GVHD involve intensification of immunosuppression without actual knowledge that there are T cells still causing damage.
This was something that bothered me. These are things that drive you crazy about the field and want to change it. I realized that we had no human data to support how we manage steroid-refractory GVHD. Out of decades worth of work, there were no studies that justified that this is the right path.
I performed a study where we had rectal biopsies of patients with grades 3 to 4 gastrointestinal GVHD. They were steroid-refractory and received other therapy. I wanted to look at the biopsies for a sign that it was the donor immune system still doing the damage to prove what we’re doing is right and I found absolutely no evidence to support our practices. There was no increase in T cell infiltration. There was no immune signature at all that suggested that it was out of control T cell-mediated damage in the steroid-refractory patients. All we saw were signs of tissue damage.
I’m hoping that the field will evolve. Instead of intensifying immunosuppression, give something more immunomodulatory, support immune tolerance, and give something to help heal the damaged organ. Change the paradigm. That was a huge frustration that I had as a fellow and I hope more people read that paper now.
Clinical Trials for GVHD
Stephanie: We’ve talked about the current landscape of GVHD and treatments, and some gaps of need. Before we go into them, what are clinical trials?
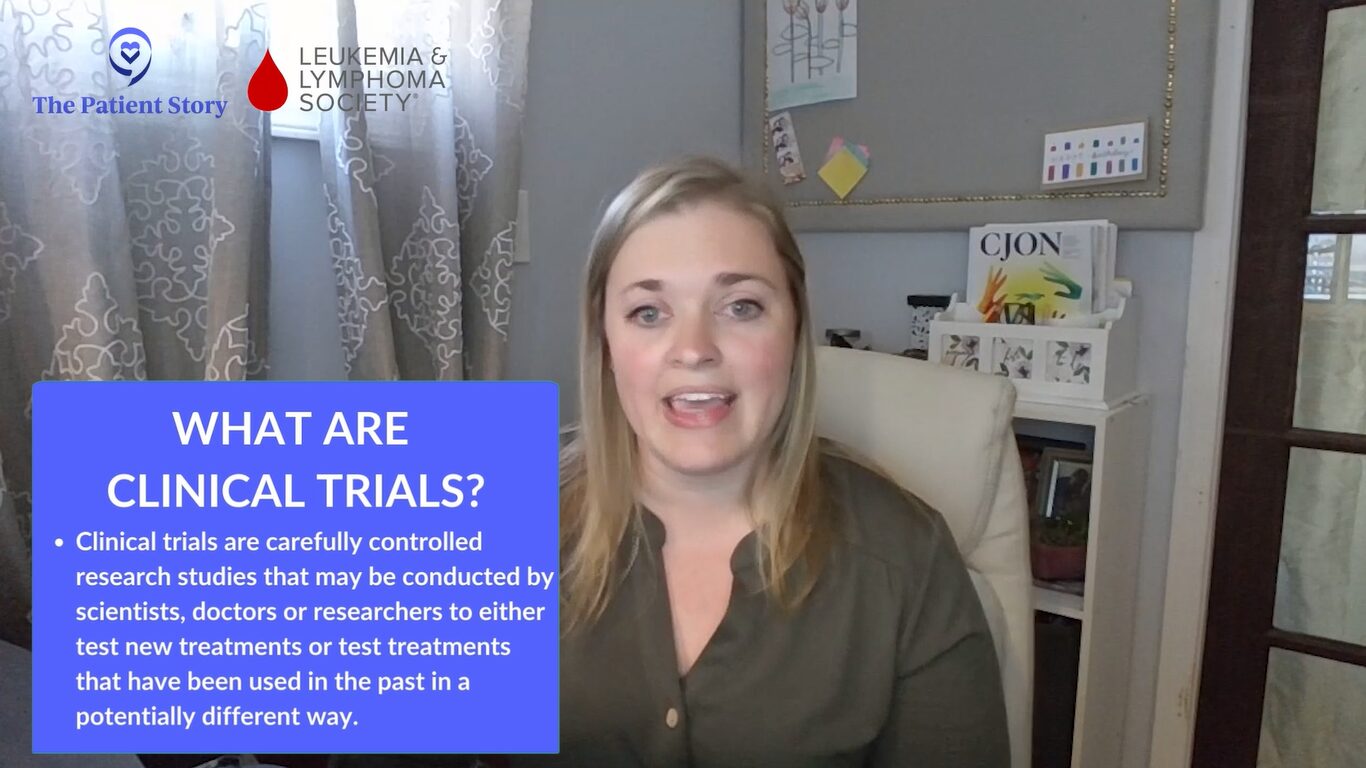
Ashley: Clinical trials are carefully controlled research studies that may be conducted by scientists, doctors, or researchers to either test new treatments or test treatments that have been used in the past in a potentially different way. Trials can also compare new treatments to existing treatments or to various combinations of treatments to find out which treatment might work best or which would be better tolerated, all with the goal of improving care and treatment for patients.
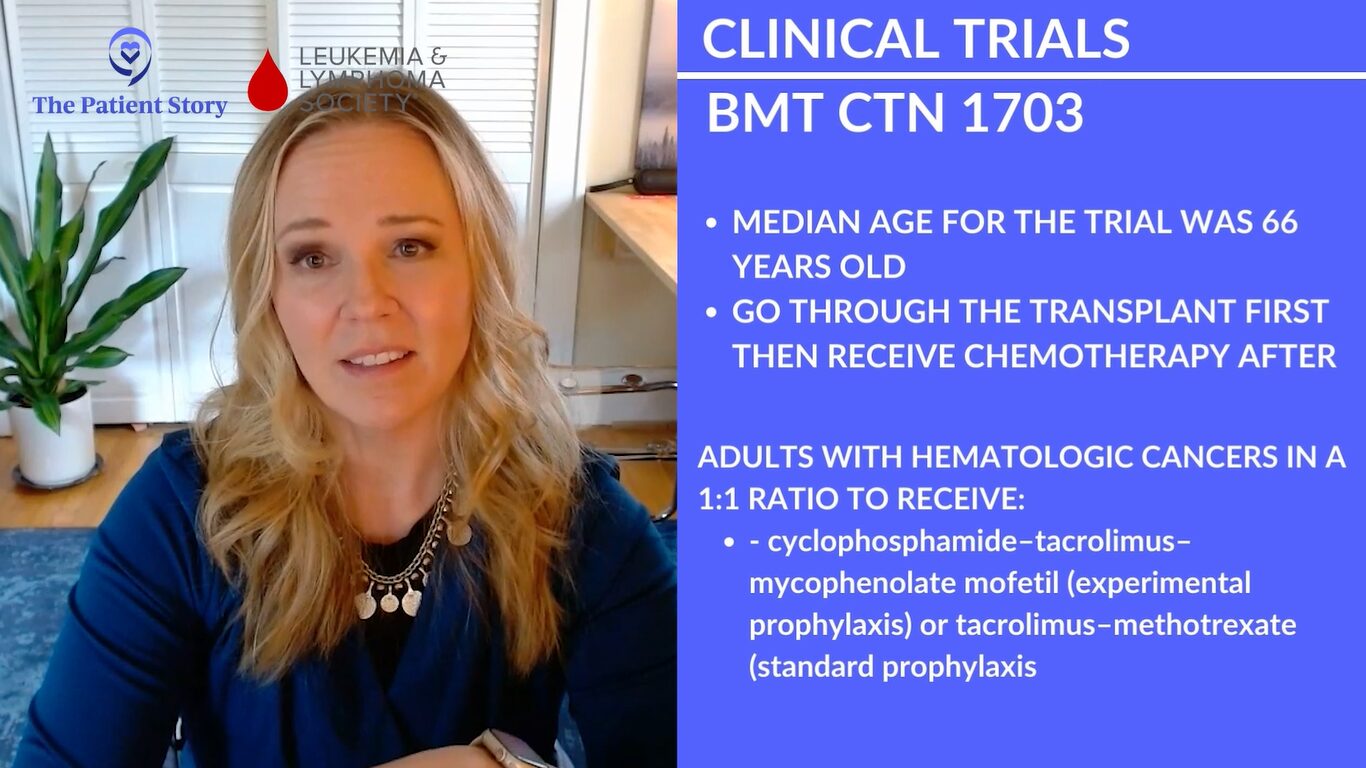
BMT CTN 1703 Clinical Trial
Stephanie: Dr. Holtan, can we talk about one of the trials that you helped lead? What’s the potential and the excitement about that?
Dr. Holtan: An ounce of prevention is worth a pound of cure. The theme in these studies is prevention of graft-versus-host disease. Our field is in the midst of an important era. We have very effective prevention for acute and chronic graft-versus-host disease with multiple modalities that we have not had in the past.
The BMT CTN 1703 study was repurposing a chemotherapy agent called cyclophosphamide to prevent acute and chronic graft-versus-host disease by giving it after transplant in the setting of reduced-intensity transplants, so patients who are typically older. The median age of the trial was 66, going through transplant, and would receive this chemotherapy after the transplant. That initially sounds crazy to do. Why would you give chemo after the transplant?
We’re learning how this works, but it helps to deplete allo-reactive T cells. The good cells that we want to persist are completely immune to cyclophosphamide, so regulatory T cells, which are T cell peace mediators, and stem cells themselves are resistant to this chemotherapy. It eliminates the cells we don’t want and preserves the cells we do.
This modality was compared against the standard, which was a calcineurin inhibitor (CNI) plus methotrexate (MTX), and that’s been the standard since 1986. Our field hasn’t undergone a major change where we saw that the new treatment arm was superior. We haven’t had this kind of change since the mid-80s.
We did a similar study in Minnesota looking at post-transplant cyclophosphamide in the myeloablative setting. We saw remarkably low rates of acute and chronic GVHD using this platform. The rates of grade 3 to 4 acute GVHD were 5%. The rates of chronic GVHD requiring immunosuppression were also about 5%. It’s not a randomized nor a phase 3 study, so we haven’t done that comparison. I have a lot of conflicts of interest, so I don’t want to do that study because the results of phase 2 are so good. I wonder what Dr. Kosuri thinks about that.

Dr. Kosuri: Dr. Holtan’s work with 1703 is one of the more important studies that we’ve had recently in the field of stem cell transplant. When we look at our field and the studies that we conduct, having a randomized study in such a large manner is very, very rare, so this was a big deal. It’s not just the findings, but the way that the study was conducted.
The study went through other randomized trials and the two best options went into 1703. As Dr. Holtan mentioned, the results are very, very important and being adapted in a widespread manner amongst many of the transplant centers not only in the United States but even abroad, so it’s a very, very impactful piece of work.
The important thing, as she highlighted, is that these are for older patients who have had multiple lines of therapy and may be coming into transplant in a more frail physiologic manner than someone who is in their 20s, 30s, or 40s. The reduced-intensity aspect is very, very important.
I agree that the post-transplant side has had such an impact on the incidence of acute and chronic GVHD. The other thing that I’ve noticed is the nature of the graft-versus-host disease that could develop. Even if someone were to receive post-transplant cyclophosphamide as a GVHD prevention strategy or what we call T cell-depleting methods, there are other ones also.
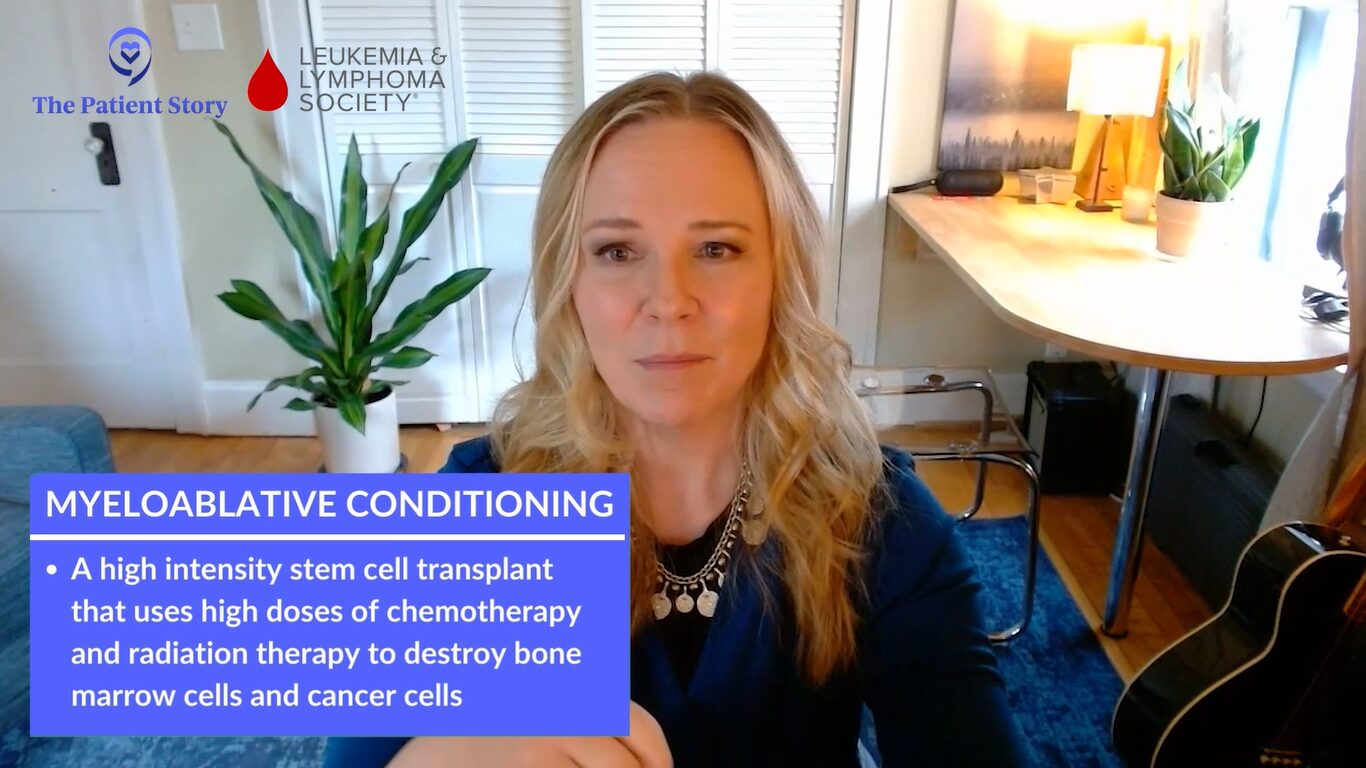
When we’re giving higher-intensity conditioning, the amount of initial damage and inflammation that occurs is higher and the risk of developing both acute and eventually chronic GVHD can also be higher.
Dr. Satyajit Kosuri
When we compare it to the standard of care, if they were to develop graft-versus-host disease, there is the potential that it may be more responsive to current treatment modalities. You can treat it and it can potentially go away versus you trying to treat it and patients may become more steroid-refractory or steroid-dependent. Incidence is important and the incidence is much lower. My opinion is that the nature of the GVHD that may happen is also different.
As far as myeloablative conditioning, if we think it works in one setting with a group of patients who may be a little bit more sensitive to the toxicities of transplant, as a transplant physician, we want to try to apply it to the younger, fitter patient population who are receiving myeloablative transplants or the higher-intensity transplant.
The important point there also is when we’re giving higher-intensity conditioning, the amount of initial damage and inflammation that occurs is higher and the risk of developing both acute and eventually chronic GVHD can also be higher.
If we can take this modality, use it in the myeloablative setting, and decrease the incidence of both acute and chronic GVHD, that’s something I think that we’re all very supportive of. As transplant centers are changing their standard approaches, we ourselves at the University of Chicago are figuring out a way to standardize our myeloablative transplants using PTCy (post-transplantation cyclophosphamide), even though we don’t have a randomized, large randomized study.
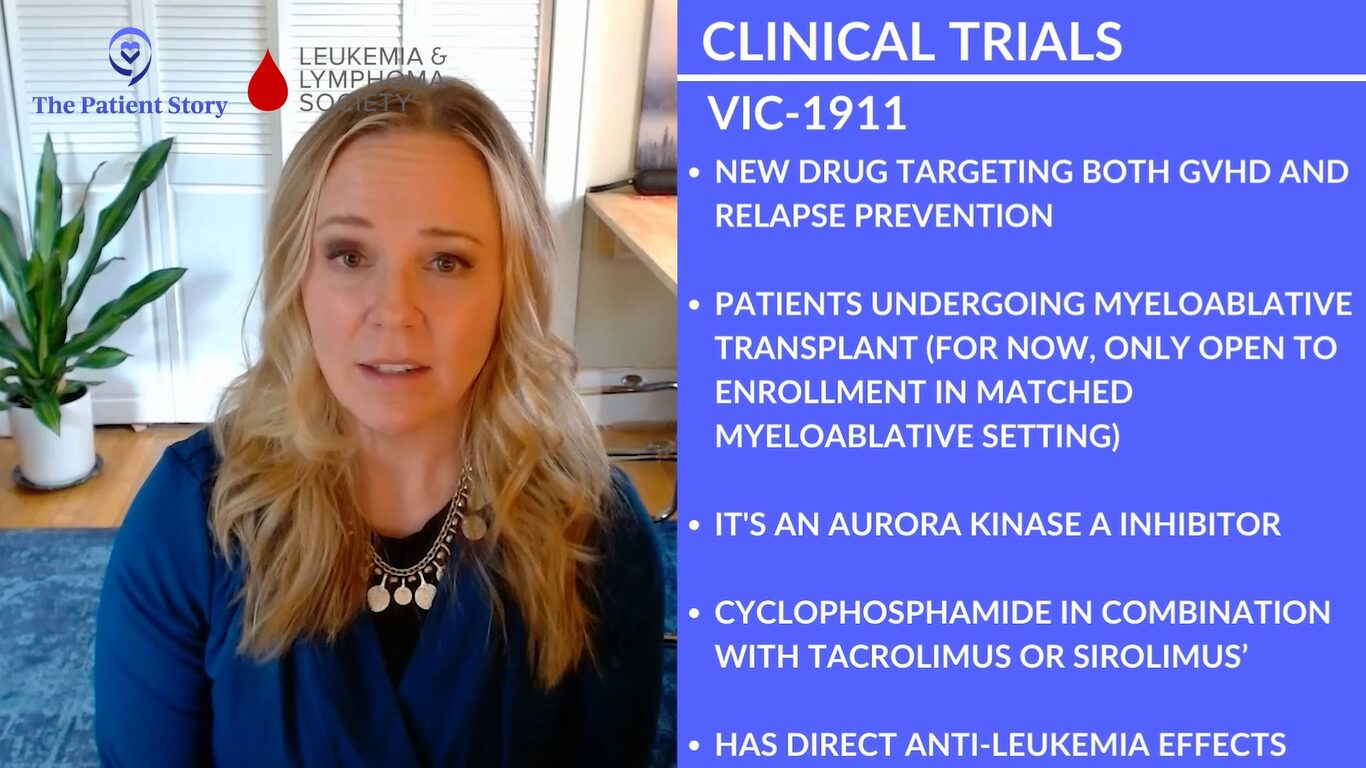
VIC-1911 Clinical Trial
Stephanie: Speaking of higher-intensity transplant groups, that’s also for VIC-1911, right, Dr. Holtan? What’s exciting about that and who’s going to benefit from that potentially?
Dr. Holtan: This is a new clinical trial looking to improve on the post-transplant cyclophosphamide platform. Now that we’ve nearly eliminated severe acute and chronic graft-versus-host disease, our unmet need is addressing relapse.
We’re looking to see if we could do something different within the GVHD prophylaxis platform that not only keeps GVHD rates low but also directly reduces the risk of relapse. We took away one of the drugs in the platform called mycophenolate mofetil (MMF). We don’t think that MMF probably does very much to be honest. The heavy lifting is done by cyclophosphamide in combination with whatever we partner it with, tacrolimus or sirolimus.
We took MMF out and put in a drug called VIC-1911, an Aurora kinase A inhibitor (AURKA). That drug is known in preclinical testing to keep GVHD rates low, but it also has direct anti-leukemia effects. It helped to kill leukemia cells in the test tube and in mice. Mice who received this combination had better survival overall due to less graft-versus-host disease and less relapse.
We’re testing a platform to see: does it protect people from graft-versus-host disease and can it also protect from relapse? We have two primary endpoints in this study: GVHD and relapse. If we can move the needle with relapse, we will have evolved the platform even further.
This trial is ongoing right now only for the myeloablative or high-intensity conditioning regimen, but we hope to complete the study, learn the results, and, if successful, expand it to other platforms. It’s currently in phase 1. We have just found the dose that we want to test going forward.
Stephanie: That’s great context. Some trials are further along. People are always wondering, “Oh, that sounds so promising! But when are we actually going to see that in the real-world setting?” It’s great to know that the research is happening, but we’ve got a ways to go with that one.
Dr. Kosuri, you talked about PTCy and this trial is about lowering the dose. Can you talk more about that and who will benefit?
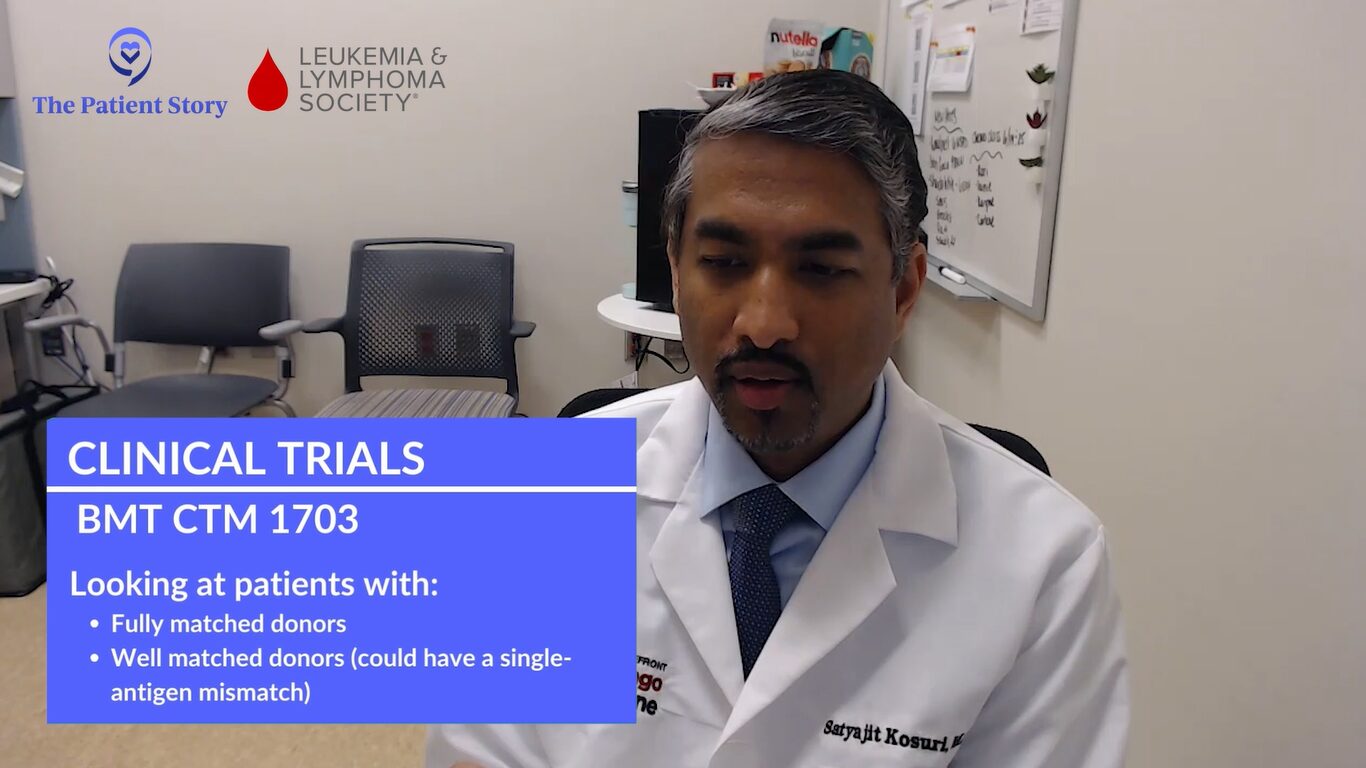
Dr. Kosuri: In Dr. Holtan’s 1703 study, we were looking at patients who have fully matched donors or what we call well-matched donors. Well-matched donors could also mean having a single-antigen mismatch. This is coming off post-transplant cyclophosphamide.
For patients who have haploidentical donors or half-matched donors, we’ve been able to successfully use that platform with very comparable and good rates of graft-versus-host disease reduction. The idea is if you can use it in a half-matched or half-mismatch, you can also use it in well-matched patients. We call that 7/8.
There are two studies. OPTIMIZE is coming after another study called ACCESS, which is looking at the same dose of post-transplant cyclophosphamide that we used in haploidentical transplants and reducing the dose a little bit.
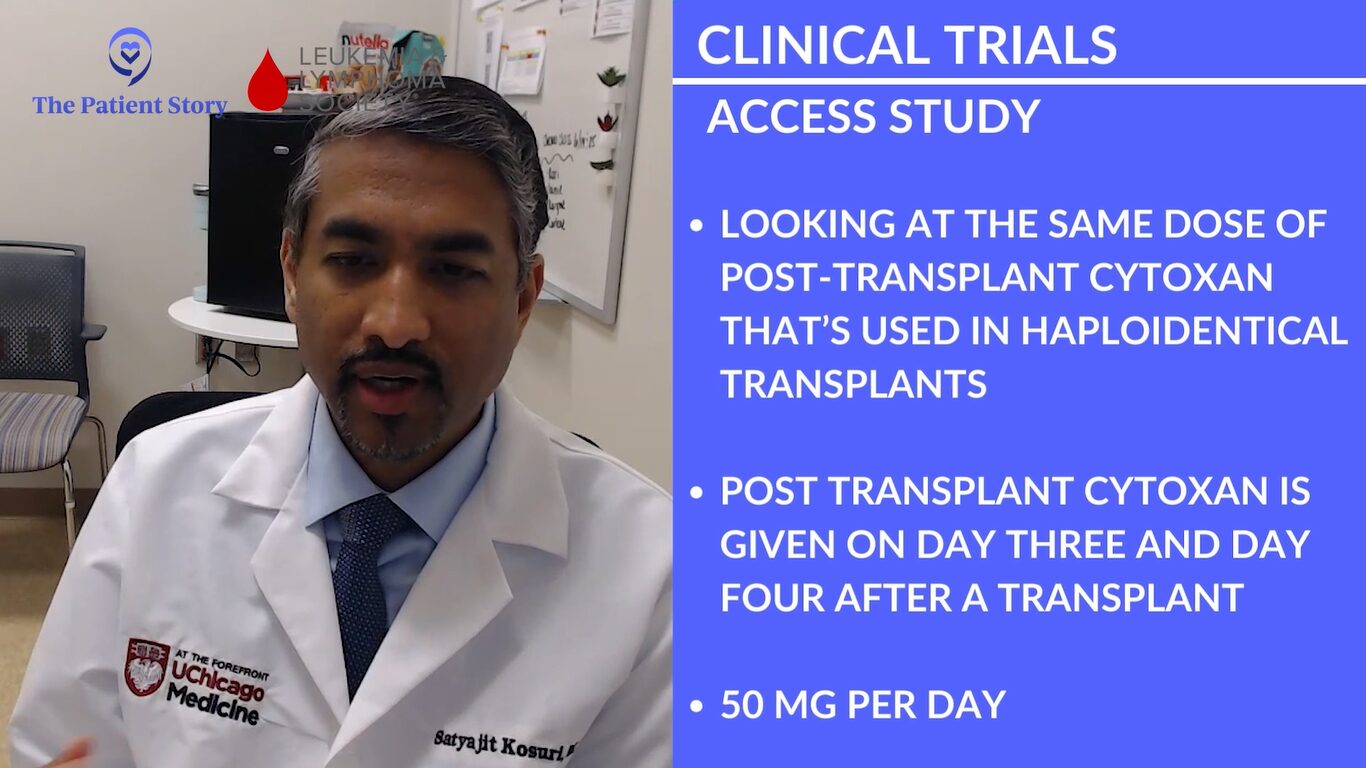
Post-transplant cyclophosphamide is given on days 3 and 4 after a transplant at 50 mg each day. Data in the haploidentical transplant setting suggests that if we’re able to reduce the dose a little bit, a couple of things can happen along the lines of toxicity. One of the things that interests us is how quickly someone may engraft after a transplant, meaning how quickly their white blood cells come back and how quickly their hemoglobin and platelets recover.
If we reduce the dose a little bit, are we able to maintain graft-versus-host disease prevention, efficacy, or advantage? Maybe we’re able to improve a little bit with regard to the time it takes for the graft to come in. It’s a phase 2 study looking at patients who are 18 and older, who have a 7/8 donor, and both reduced-intensity as well as the myeloablative condition transplants.
We can find a list of clinical trials that will be open for consideration for a particular patient based on prior treatments and any conditions they may have.
Ashley Giacobbi
Enrolling in GVHD Clinical Trials
Finding a Clinical Trial
Stephanie: Finding clinical trials and enrolling in them is very difficult. We know ClinicalTrials.gov is available but may not be the most user-friendly. Can you walk us through the steps of how a patient could find a clinical trial that’s right for them?
Ashley: ClinicalTrials.gov is an amazing resource. It’s a database of all active and ongoing clinical trials, but it can be very challenging to use. This database contains all clinical trials for all conditions. It’s not exclusive to cancer clinical trials. Although cancer clinical trials make up a large portion of the clinical trials conducted in the United States, there are so many other clinical trials that are ongoing that it can be challenging to find one that’s right for you.
As a representative of the LLS and the Clinical Trial Support Center, we always encourage people to reach out. We hone in and find clinical trials that are most appropriate for the individual in whatever situation they are in. As opposed to having to filter through ClinicalTrials.gov, we can find a list of clinical trials that will be open for consideration for a particular patient based on prior treatments and any conditions they may have.
Types of Clinical Trials
Stephanie: We also understand that there are different kinds of trials available, like prevention, treatment, quality of life, and observational. Can you take us through what they mean in the context of GVHD?
Ashley: There are a lot of ongoing clinical trials for GVHD as this is an area of need. There’s a lot of ongoing research and that falls into different buckets.
Prevention clinical trials may look at altering the regimen prior to transplant or the medications taken after the transplant in an effort to prevent the development of acute or chronic GVHD.
Another type is treatment trials and these may include specific medications or investigational therapies that would manage acute or chronic GVHD if it’s already present.
Quality of life clinical trials are so important. There are a lot of clinical trials investigating symptoms that people with GVHD may experience. There may be behavioral interventions being investigated, such as exercise or even the use of an app to provide support. Some clinical trials offer social support or dietary recommendations in an effort to reduce symptom burden and really improve quality of life.
Finally, there are observational or natural history trials. These would be less involved as patients wouldn’t have to participate as much. These trials collect information either from the patient’s medical record or prior testing that’s been done to learn more about GVHD, who might develop GVHD, or how they might respond to specific treatments. These are important in the information gathering phase, but they might not require as much involvement from the patient perspective.
Eligibility criteria help determine the group of patients who will potentially receive the most benefit from the therapy being investigated.
Ashley Giacobbi
Qualifying for a Clinical Trial
Stephanie: You may find a trial that seems great, but there are eligibility criteria and screening processes that you may have to go through. What does that typically look like for patients?
Ashley: History, previous treatment received, and other factors play a role in the eligibility criteria, but those help determine the group of patients who will potentially receive the most benefit from the therapy being investigated. These criteria are also there to help reduce any unnecessary risk by preventing those who have underlying conditions that could be made worse by the treatment from participating in that clinical trial.
Those criteria may include things like the type of GVHD, acute versus chronic, which body systems are being affected, as well as any prior treatment received for the management of GVHD. Very often, steroids are used and some of these clinical trials will require that people have already attempted the use of steroids. Those eligibility criteria help us to find appropriate clinical trials for the individual.
Stephanie: You have touched on what you at the Clinical Trial Support Center in terms of helping people with a personalized trial list, going off of ClinicalTrials.gov and making sure it’s more tailored to them. Is there anything else you’d like to share about what they could expect?
Ashley: Patients can be referred to the Clinical Trial Support Center either by a healthcare provider or they can get in touch directly themselves. Very often, we connect with caregivers of patients.
Initially, we take the time to learn about the patient, what’s important to them, and their history. Those details are so important when looking for clinical trials and that’s usually via phone call.
Beyond that, we take the time to go through and review clinical trials. We’re very fortunate to have a unique database that looks at clinical trials in ClinicalTrials.gov but also stores information that we receive from investigators and sponsors of clinical trials so that we’re able to provide the most up-to-date information to patients when they’re considering clinical trial options.
Once we’ve generated a list, we’re able to send that to the patient, caregiver, or healthcare provider and share the clinical trials that we’ve found for that particular person. They can then take back that list to review with their healthcare team and see if any of those trials is a potential option for them to explore.
A lot of emerging data suggests that preservation of muscle mass actually helps reduce the risk of relapse, so this is not just cosmetic. It is about quality of life, but it’s also about the efficacy of the therapy itself.
Dr. Shernan Holtan
Nutrition & Exercise When You Have GVHD
Stephanie: Dr. Holtan, what specific nutritional and exercise interventions are being investigated to support muscle health during and after transplant?
Dr. Holtan: This is a substantial topic. I always tell my patients that if I could give a pill that could keep their muscles strong, I’d be the richest woman in the world. Having the ability to maintain muscle mass throughout chemotherapy of any kind is important. We need to do more in this area not just for transplant but for all cancer therapy.
There are multiple studies going on around the world that are looking at different types of nutritional supplements to maintain muscle mass and help promote intestinal healing. There’s some interesting research going on out of Italy using a nutritional supplement that has a growth factor that can help the gut heal itself.
There might be different nutritional approaches based on infection profiles. For example, we want to avoid a certain type of bacteria growing in the intestinal tract and avoid something in the diet that might help prevent that from growing. Those types of studies are important and we need to be able to expand them so that more patients can participate because, in reality, we don’t know what the best diet really is. We want people to get calories and protein in.
The same thing goes for exercise. We need to do more to facilitate exercise, especially resistance training. A lot of emerging data suggests that preservation of muscle mass actually helps reduce the risk of relapse, so this is not just cosmetic. It is about quality of life, but it’s also about the efficacy of the therapy itself. There’s a lot of work we need to keep doing in this space, so stay tuned. Obviously, this is the most important thing that we can work on besides improving the toxicities of the treatment itself. Supportive care is so important. We have a lot more work to do.
It’s on us to educate both referring providers as well as patients to understand that things have improved over time both from an access standpoint as well as supportive care standpoint.
Dr. Satyajit Kosuri
Areas Requiring More Research & Gaps in Transplants & GVHD
Stephanie: Dr. Holtan, you did mention that only a fraction of potential transplant candidates even get referred. What is contributing to this under-utilization? How can we address those barriers?
Dr. Holtan: We have an educational gap. The transplant field is vastly different in 2024 than it was even in 2021 and certainly way different than it was in the ‘80s or ‘90s, so we have to do a better job of communicating. What have been the advancements in care? How have we improved on the availability of donors? We no longer need a perfect match. How have we reduced graft-versus-host disease and improved other toxicities so that more patients are able to be reached?
There’s a lack of referral and also fear from the patient’s side as well. We have a lot of education to do to share that it is different today, much safer, and hopefully we can be able to take care of a lot more patients in the future.
Dr. Kosuri: Many of the old thoughts that we have about transplant are that you have to be a certain age or how scary it is and things of that nature. It’s on us to educate both referring providers as well as patients to understand that things have improved over time both from an access standpoint as well as supportive care standpoint.
The supportive care has changed over the last decade significantly and that’s why we’re able to take patients who previously the field would not consider, even if they were in good shape.
There can be a patient who is 50-some-odd years old but has been beaten up because of the disease or the treatment, so transplant would be very difficult for them, whereas we can have a 70-year-old who is running a half marathon. It’s not just numerical age; it’s the physiology of what the patient’s body is at the time that we’re considering transplant.
I totally echo what Dr. Holtan’s saying. It’s about education and casting our net very wide with regard to patients and patient advocacy groups as well as physicians or the referring providers.
We’re seeing so much change because of our understanding of the biology of the diseases that we’re dealing with coming into transplant, the technical aspects of the transplant, and GVHD prevention.
Dr. Satyajit Kosuri
GVHD Treatments Final Takeaways
Ashley: There are resources and support available. It’s never too early or too late to explore clinical trials when you’re talking about GVHD and clinical trial options during the transplant process.
Dr. Kosuri: Over the last decade, I have had more hope as a clinician in the field of transplant. Even though it’s trying to move, the field has been set in its ways for a very long period of time. But within the last 5 to 7 years, we’re seeing so much change because of our understanding of the biology of the diseases that we’re dealing with coming into transplant, the technical aspects of the transplant, and GVHD prevention, like the 1703 study.
There are many trials looking at the initial treatment of graft-versus-host disease and how to get patients off of steroids quicker. With chronic graft-versus-host disease that is far off, more severe, and more fibrotic, there are ways to manage that.
I want to emphasize Dr. Holton’s work regarding biomarkers. For a long period of time, our approach when it comes to GVHD was if we try something and it fails, we try another agent and provide more immune suppression. We’re hoping to minimize that approach where you throw something at a wall and see what sticks. It may be different for each patient. Do we need GVHD treatment in patients who have certain symptoms? If it is graft-versus-host disease, how do we know when to come off therapy or how to add therapy? That’s where the biomarker becomes very, very important.
I can’t emphasize enough how nutrition, exercise, and sleep are key to help recovery and resilience. I want people to know that they have more control than they think.
Dr. Shernan Holtan
Dr. Holtan: I want patients and their families to know that they have a lot of control in these processes. I believe very much in the principle of self-efficacy. Yes, this is a medical treatment that we are delivering, but there’s a lot a person can do for themselves and that their family can do together to help make the process easier.
I can’t emphasize enough how nutrition, exercise, and sleep are key to help recovery and resilience. I want people to know that they have more control than they think and look for ways that they can help build up their strength and resilience, lean on their network, and use these tools and resources to help build up the spirit and body to be able to withstand the trials and tribulations that certainly lie ahead. The medical advancements are real, but people also have a lot of control and they should know that.
Meredith: Hope is incredibly important. Recognition that you do have control is imperative. Be selfish and put yourself first. Don’t try to take care of all the people around you to the detriment of yourself. If you don’t want to do something or can’t meet with somebody, don’t do it.
Continue to find meaningful and fulfilling activities so that the illness doesn’t become your identity. You have an illness, but you’re not defined by that illness.

Conclusion
Stephanie: I want to thank Dr. Kosuri of University of Chicago, Dr. Holtan of Roswell Park, Meredith of the Meredith Cowden Foundation and co-founder of the GVHD Alliance, and Ashley of the LSS’s Clinical Trial Support Center.
The LLS, being a partner of ours on this program, is such a great resource. The CTSC provides amazing one-on-one support in terms of understanding clinical trials, finding, enrolling, and even staying on them.
We hope that this program was empowering and that you’re able to take away not just from this program but from the many stories that we have.