Testicular Cancer: A Medical Oncologist Shares Everything You Need to Know
A conversation with Alok Tewari, MD, PhD

An estimated 9,910 new cases of testicular cancer cases were diagnosed in 2022 according to the National Cancer Institute. When thinking about prevention or a diagnosis, you likely have questions about causes, treatment, fertility, sex, and survival.
Dr. Alok Tewari is a medical oncologist at Dana-Farber Cancer Institute who specializes in cancers arising from the genitourinary tract like testicular cancer.
In this conversation, Dr. Tewari discusses the signs and symptoms of testicular cancer, how to do self-exams, diagnosis and treatment for testicular cancer, and potential risk factors. He shares candid insight into what it’s like to undergo surgery and how you can spot testicular cancer early.
This interview has been edited for clarity. This is not medical advice. Please consult with your healthcare provider for treatment decisions.
The key point is as you’re cleaning yourself [and] notice any abnormalities anywhere on your body, you should always feel free to ask your doctor about it. It’s much safer just to ask them than not.
Dr. Alok Tewari
Introduction
I’m a medical oncologist and I’ve been working at Dana-Farber since I started [my] fellowship in 2016. I gravitated towards GU (genitourinary) medical oncology because of [the] experiences I had during my training.
Signs & symptoms of testicular cancer
How is testicular cancer typically detected?
A minority of patients develop testicular discomfort and are found to have cancer. There [are] a lot of reasons you can have testicular pain and most of them are not related to testicular cancer, but every so often, that does happen.
There [are] a lot of different ways that patients get diagnosed with testicular cancer.
There [are] patients who are just doing a self-exam, even though that’s not clearly recommended as part of screening guidelines. Patients will be examining themselves in the shower and feel something abnormal or notice a change in size. That’ll get evaluated and the diagnosis will come about.
There are patients who notice something abnormal but think it’ll go away. Oftentimes, you can have inflammation in the area and that can definitely go away. But because of some taboo about talking about your genitals, [people] may not be so motivated to talk about it in general.
We do see some patients who present later when they have larger masses or have developed metastatic disease.
It does run the gamut. The key point is as you’re cleaning yourself [and] notice any abnormalities anywhere on your body, you should always feel free to ask your doctor about it. It’s much safer just to ask them than not.
A lot of times, there [aren’t] any clear symptoms. The minority of patients will present with some testicular pain; that’s actually not the most common way. The most common way that patients are diagnosed is that they notice something abnormal in size, a lump, or something like that.

If you start to feel abnormal — losing weight, developing pain, your GI or urinary function is not the same [as] it always was — then you get evaluated and it leads to a diagnosis of testicular cancer. There are a lot of other things that can cause those problems, but that’s another way.
It’s not always symptomatic. It’s okay to monitor and check yourself. It’s not the most sensitive or specific, but it can be helpful. If you notice anything abnormal, ask.
There’s no real relationship between having testicular pain, for example, and the presence of metastatic disease. If this is diagnosed because you’re having back pain or troubles related to your abdomen and it turns out to be testicular cancer, that probably is related to metastatic disease. But just testicular pain itself doesn’t mean anything.
Self-exam
How do you do a self-exam for testicular cancer?
There is not a clear recommendation from any organization, but if one were to be doing self-checks in the shower, which is the easiest time to do it, it’s not just washing the area.
It’s more of palpating your scrotum, actually feeling your testicles specifically — not too firmly to cause pain, but just making sure that there [are] no bumps or lumps, [and] that the size is similar to what you experienced before.
Testicles can often be different sizes; that’s not necessarily something. It’s more the change that you might wonder about.
Diagnosis & treatment
How is testicular cancer diagnosed?
The most common way it’s diagnosed is when you feel an abnormality, then an ultrasound is typically done. The ultrasound is a pretty good test for noticing some sort of abnormality that’s not typically there.
How is testicular cancer treated?
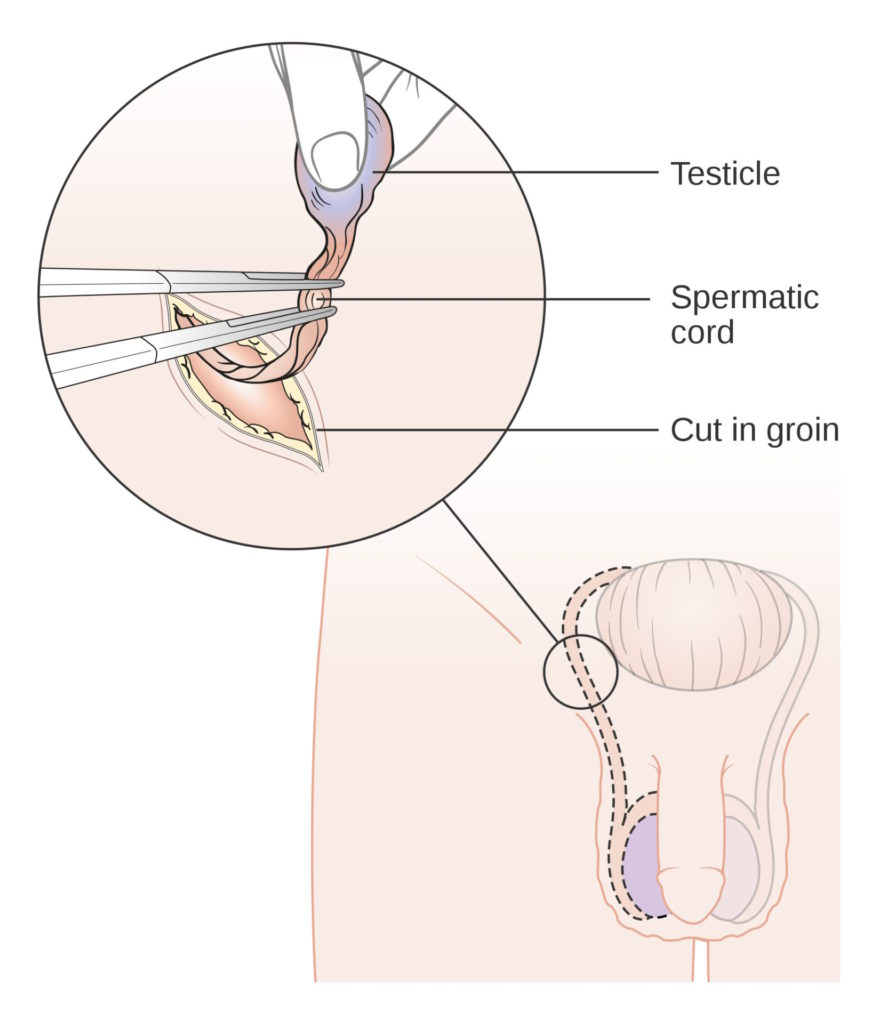
What will typically happen is you’ll have surgery where a urologic surgeon will make an incision in your groin area, roughly up near your inguinal canal, and will remove the testicle that way.
It’s a pretty well-tolerated surgery. You usually don’t stay in the hospital. You can have some soreness or numbness based on random factors, but most folks recover pretty well and pretty quickly. Oftentimes, that’s it.
You’ll have some scans [and] some labs done to make sure that there [are] no signs of spread. If there [are] no signs of spread, then you’ll be done. You’ll just have to have regular surveillance to make sure it doesn’t come back. Usually, after two years, the risk of it coming back is very small.
Sometimes, though, you either develop symptoms in your back or somewhere else that lead to this diagnosis. Unless things are a little bit unstable where you’re not feeling really well and there’s a need to start therapy, you’ll still have surgery and your testicle will still [be] removed; that helps us understand what we’re dealing with.
Depending on what you have at diagnosis and how much the spread has been, there [are] different therapies that could potentially be undertaken.
Age group at risk for testicular cancer
It definitely is a cancer that can affect patients of all ages. It’s just most common in the early teenage years to late 30s. It’s the most common cancer in young men, essentially.
However, there are patients much younger than their teenage years who get it. There are patients in their 70s who get it. It’s very uncommon at that age, but it does happen.
Hereditary risk factors for testicular cancer
If you have a family history of testicular cancer, that does slightly increase your risk above the average population so that’s the sort of thing that you should know about.
When you’re getting your health care, that should be something your doctor should know so they can tailor their physical exam appropriately. It’s something you can just be a little more aware of than you might otherwise be.

Other factors for testicular cancer
Geographical location
Nothing definitive. There was an increased incidence in northern countries, like Scandinavia especially, over the last several years for unclear reasons. That seems to have tapered off a little bit, but unexplained.
It’s not as common in places like Australia, for example, so something about the northern climate seems to be associated with it. There’s probably an environmental exposure component to it that we don’t understand.
Once you start to see enough patients, you’ll meet people [whose] friends have had testicular cancer. These are groups of patients that you can’t pinpoint anything, but it’s just something that we see sometimes.
Just because you have a friend who had testicular cancer doesn’t mean you’re going to have it, but there are these one-off associations that I don’t have enough data to draw a conclusive link on.
Can cell phones cause testicular cancer?
Those associations are hard, but there’s nothing that’s been shown.
I wouldn’t say that the incidence has increased drastically since people have been having cell phones over the last 10 to 15 years. Nothing clear in that respect.
I think there is a certain bias. You recall what you remember. If a friend had testicular cancer, all of a sudden you remember it because that’s a significant event and so we have a recall bias in that respect.
From a statistical perspective, there’s nothing clear, but we’re always trying to learn more.


Does testicular cancer affect sex and fertility?
The process that leads to the development of testicular cancer certainly seems to be related [to] decreased fertility relative to the average population. We know that patients who are diagnosed with testicular cancer can have more trouble than average with conception and fertility.
The usual thing to do is to discuss sperm banking even before having surgery. There [is] a very small set of patients who won’t have normal sperm production and so trying to sperm bank even before surgery is something that can be considered. We definitely recommend sperm banking prior to any chemotherapy or any surgery because those can impact sperm health for sure.
After you get through that and you’ve recovered from chemotherapy or from surgery to remove your testicle, the normal process is if you’re interested in trying to have children, you try the usual way. If you’re having difficulty after six months, then you can either rely on banked sperm or enter into the fertility health process.
Challenges of testicular cancer
One of the challenges in this disease is that people do so well and that’s an interesting way of putting it. What makes it a challenge is that it’s hard to understand when patients don’t do well. There’s a small, small subset of patients who don’t do well with this disease. Understanding that and how to better treat them is a real challenge.
I encourage folks to think about how to donate tissue. We have programs at Dana-Farber. We keep everything private. We’re looking for folks who are interested in learning more and helping us learn more. There are folks such as myself, Dr. Van Allen, or other people at Dana-Farber who would be very interested in helping to learn more.
Testicular cancer awareness
Testicular cancer is the most common cancer that affects young men [between] the age of 15 to about 40. The best thing to know about is that it’s very curable.
The most common way that it’s found is that you are doing a self-exam and you feel something abnormal relative to prior examinations, it gets evaluated and is found to be cancer. It’s pretty uncommon for it to be found in an advanced setting, but that does happen.
Regardless of how it’s found, the goal is cure and that happens most of the time. If you’re diagnosed with testicular cancer, you’ll have some labs checked.
The most common thing that happens, after you get an ultrasound to confirm that something is abnormal, is that you’ll have surgery. The surgery is a day surgery. It’s pretty well-tolerated and people recover pretty well.

The question is: has it spread or not? If it hasn’t spread, you’ll have surveillance and that’s just to make sure that it doesn’t come back. If it does, then it’s treated properly early. If it has spread, then depending on kind of how it’s spread and so on, you’ll have to have different therapies.
But again, the overall chance of cure is really good. Despite getting diagnosed with this cancer, there [are] a lot of reasons to be optimistic.
We’re still trying to learn a lot more and research in this field is pretty new because we thought that it’s been cured and so it hasn’t necessarily been a priority. But we’re focusing on trying to learn why sometimes it behaves the way it does and we hope to know more as time goes on.




