DLBCL: The Latest in Treatment and Research
What Patients and Caregivers Need to Know

3x DLBCL Survivor
City of Hope
Mount Sinai
Robyn, a three-time DLBCL survivor, and two top lymphoma specialists, Dr. Tycel Phillips from the City of Hope and Dr. Joshua Brody from Mount Sinai, discuss the latest DLBCL treatments and developments happening in the most common subtype of non-Hodgkin lymphoma: diffuse large B-cell lymphoma (DLBCL).
Brought to you in partnership with The Leukemia & Lymphoma Society and its Clinical Trial Support Center.
This interview has been edited for clarity. This is not medical advice. Please consult with your healthcare provider for treatment decisions.
- Introduction
- What is DLBCL? What is the standard care for first-line treatment?
- Bringing up different treatment options with your hematologist-oncologist
- What is CAR T-cell therapy?
- Benefits and challenges of CAR T-cell therapy
- CAR T-cell therapy for refractory patients?
- What are bispecific antibodies?
- What is the comparison between epcoritamab and glofitamab?
- Side effects from bispecific antibodies
- CAR T or bispecifics for relapsed/refractory patients?
- Clinical trials
- DLBCL Patient Stories
DLBCL, diffuse large B-cell lymphoma, is the highest incident lymphoma in America. Every year, about 90,000 people [are] diagnosed with lymphoma [and] about 25,000 of those are diffuse large B-cell lymphoma.
Dr. Josh Brody
Introduction
Stephanie Chuang, The Patient Story: I went through non-Hodgkin lymphoma treatment back in 2017 so this is a topic that’s very near and dear to me. My own experience as a cancer patient is what motivated me to start something to really help humanize the cancer experience for those of us who don’t have a science background. That was the genesis of The Patient Story.
We reach cancer patients, care partners, [and] caregivers with content; mostly in-depth stories. We also highlight conversations with specialists in the field.
The goal is to humanize cancer. What does that mean? It means you’re not alone and here’s some information we hope will be helpful.
Our partner, The Leukemia and Lymphoma Society (LLS), has done incredible work in terms of research and community. The LLS also has a clinical trial support center. It’s a free service where patients can get one-on-one support with a LLS Clinical Trial Nurse Navigator, who will personally assist you throughout the entire clinical trial process.
The focus in this webinar, is the latest in DLBCL treatments and research. We have three doctors: two lymphoma specialists and one who is a three-time DLBCL survivor.
Dr. Joshua Brody is from Mount Sinai and Dr. Tycel Phillips is from [the] City of Hope. Robyn spent years on the medical side, started off [as a] radiologist seeing patients, and then became a patient [herself].


What is DLBCL? What is the standard care for first-line treatment?
Stephanie, TPS: Let’s set the stage. We hear about DLBCL a lot. Dr. Brody, what is DLBCL and what is the standard care for first-line treatment?
Dr. Josh Brody: DLBCL, diffuse large B-cell lymphoma, is the highest incident lymphoma in America. Every year, about 90,000 people [are] diagnosed with lymphoma [and] about 25,000 of those are diffuse large B-cell lymphoma.
We have about 84 types of lymphoma. People say, “Wait, do I have the good one or not?” It’s not just two types. It’s not the good one and the bad one. We divide these lymphomas into many ways so we don’t have to memorize a list of 84 things.
The first way we divide them is Hodgkin’s and non-Hodgkin’s. We are talking about non-Hodgkin’s lymphoma. We divide non-Hodgkin’s lymphoma into B-cell and T-cell lymphomas. We’re talking about B-cell lymphoma. Then we sometimes divide B-cell lymphomas into low-grade versus aggressive. Low grade, these grow very slowly: follicular lymphoma, marginal zone lymphoma, [and] some others. The aggressive lymphomas, diffuse large B-cell [is] the most common of them. Maybe you’ve heard of Burkitt lymphoma, mantle cell lymphoma, [and] some of these other things that can grow more quickly.
We’re so lucky because the treatments for lymphoma have evolved more rapidly than for any other cancer in the world. Even though we are the fifth most common cancer, we have more FDA-approved medicines than any other cancer. The reason is [that], thankfully, the progress has been very rapid. We don’t get FDA-approved medicines without progress to prove that those therapies can be pretty good.
Over the past 20 years, the standard therapies for diffuse large B-cell lymphoma [are] these alphabet recipes. R-CHOP sounds a little aggressive and it is, as Robyn can tell you. People that are working full-time before R-CHOP are frequently working part-time during R-CHOP so it’s aggressive enough that it affects your life in a real way. It affects your hair.
R-CHOP is not the most aggressive stuff we have. It is standard therapy. Today, it may not be the only standard front-line therapy. There are a couple of slightly new versions of R-CHOP that are options now. I will say that five years from now, I don’t think R-CHOP will be the standard. I think we’ll even have some better things.
The R [is] rituximab. It is immunotherapy — targeting lymphoma using your immune system to kill those lymphoma cells, but not powerful enough by itself. The P is prednisone. The CHO is chemotherapy.
All the side effects you’ve heard about with chemotherapy — hair falling out, a little bit of nausea — not so bad, but it’s a real thing and some of these other side effects you heard about.
R-CHOP, thankfully, cures about 60% of people with DLBCL — not every type of DLBCL, but overall. That’s pretty good. We’re lucky to be able to cure 60%. Not that lucky if you’re in the other 40, though, as Robyn or lots of our patients could tell you.
We actually have a lot of progress and probably still some curative things. A lot of progress, more so than probably any other cancer, and yet a lot of room for improvement still.
The treatments for lymphoma have evolved more rapidly than for any other cancer in the world. Even though we are the fifth most common cancer, we have more FDA-approved medicines than any other cancer.
Dr. Brody
Stephanie, TPS: I do want to ask Dr. Phillips to lay out the options. If somebody relapses in the first six [or] 12 months, how different is that prognosis or treatment?
Dr. Tycel Phillips: For patients who do not respond to R-CHOP and immediately relapse — what we consider primary refractory patients and that likely extends out at least into the first six months — those patients have done very poorly historically with a lot of the standard options that we have, like RICE, which are just various combinations of chemotherapy drugs. Hopefully, not cross-resistant to each other [and] provide a different mechanism of action compared to the drugs using CHOP with rituximab as well, with the goal of getting them to autologous stem cell transplantation.
Again, historically, that group has done fairly poorly because they are probably chemo-resistant. They’re not going to respond to any sort of chemotherapy drug. The whole design of chemotherapy is to prevent DNA replication or cause DNA damage at some point during the replication cycle. If a cancer drug has figured out a way to get past one, it’s likely to figure out a way to get past most of the rest.
An auto transplant really should be named an autologous stem cell rescue because it’s still just more chemo. It’s not anything fancy about the stem cells that you’re getting back there, just your own stem cells to rescue your body.
For the most part, a lot of the clinical trials that help these relapsed/refractory regimens are probably heavily dependent on these relapse patients, which are generally the patients who relapse a year or so after chemotherapy.
These are the reasons why we get the response rates for most of these regimens, such as RICE, DHAP, and the big CORAL study, which was a big regimen looking at these relapsed/refractory regimens to see which one was better. They’re really probably driven by refractory patients again because these are relapse patients. These refractory patients are not the ones that are going to drive these studies.
A lot of big emphasis recently has been on other ways to treat these patients, especially these early refractory patients or patients who relapse within six months to a year with other regimens besides chemotherapy, which brings into the CAR T discussion.
For patients who can’t get to CAR T or who are ineligible for CAR T, in the second-line setting beyond chemotherapy, there is lenalidomide and tafasitamab, which are for patients who are ineligible for autologous stem cell transplantation. That regimen itself, at least from the clinical trial, seems to be more effective in those who have only received one line of therapy versus those who are heavily pre-treated, meaning they have two or more prior lines of therapy before [receiving] this drug.
In that second-line setting, there aren’t a ton of other agents approved, even though we have options such as polatuzumab-bendamustine-rituximab. We are a bit hesitant to use that regimen in some sense because the bendamustine does cause quite a bit of depletion of your immune system, specifically T cells. The T-cell depletion can be quite profound and prolonged, which can hamper things that depend on T cells to be effective, like CAR T, etc.
There also is a new agent recently, which is a CD19 drug antibody conjugate called loncastuximab, which has a very different drug attached to it, which is a little bit different from MMAE, our usual antibody drug target. That is also another option.
Then there is selinexor, which is [an] export one inhibitor [that] was approved [for] this patient population, but probably has very little uptake because of the toxicity of the agent.
If we’re looking at currently approved agents, the chemo or the regimens I just mentioned are the currently only approved ones outside of CAR T at this point.
A lot of big emphasis recently has been on other ways to treat these patients, especially these early refractory patients or patients who relapse within six months to a year with other regimens besides chemotherapy, which brings into the CAR T discussion.
Dr. Tycel Phillips
Bringing up different treatment options with your hematologist-oncologist
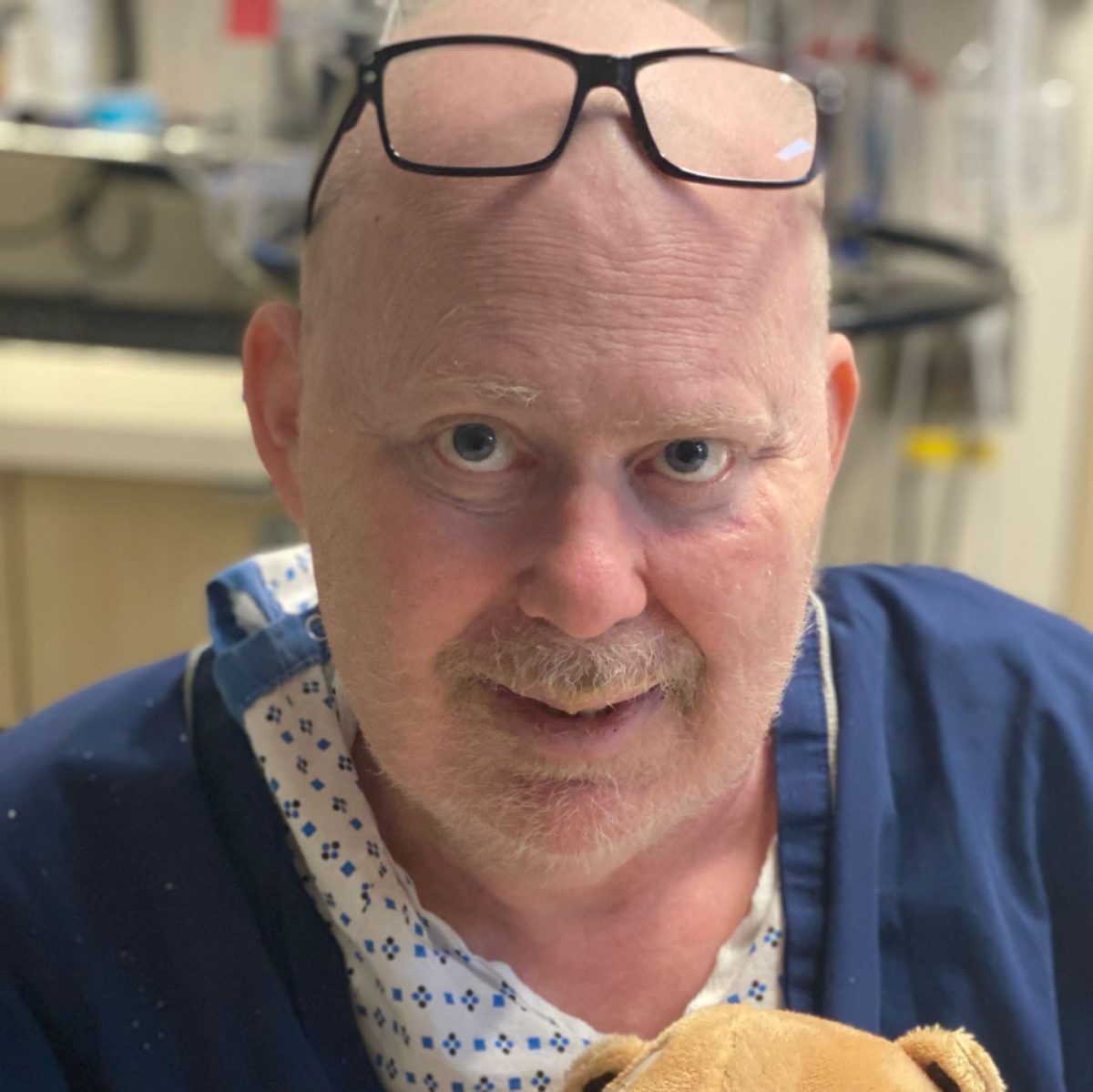
Stephanie, TPS: Robyn, you’ve been through a lot: different kinds of chemo, chemoimmunotherapy regimens, auto stem cell transplant, and eventually CAR T. It sounds like you were the one who researched CAR T. How did you bring up the discussion of CAR T with your hematologist-oncologist? What were the differences for you in terms of going through the stem cell transplant and then going through CAR T?

Robyn: Overall, I did extremely well. The auto stem cell transplant was extremely difficult for me. I was very, very sick. [It was a] terrible experience. I did survive. I’m here, but I didn’t want to go through that again.
When the auto stem cell transplant failed, I did not want to go through an allo (allogeneic) transplant.
I’d gone online. There’s a site called www.clinicaltrials.gov. Anybody can get online. I really had no advantage being a doctor except that I had heard about the site so I had started looking at different trials. My husband, who’s an engineer, and I both looked at all these different trials and emailed investigators when I relapsed. We just tried to find a space and a trial.
I just thought that was the right decision for me. It was not recommended by my oncologist. [As] a matter of fact, my oncologist thought that I should go ahead and have an allo transplant using my son as a donor, as a haplo (haploidentical) and I didn’t want to do that.
I looked at it on my own. Nowadays, things are very different. In 2016, there was only one phase 1 clinical trial for Kymriah, which is what I had. I based my decision on 26 patients and 12 went into remission, which is not a big number. My oncologists were not comfortable with that, but somehow, I felt that was the right decision for me. Everyone is unique.
I did get different opinions from other oncologists. I was a very complex case. I was a younger patient who was healthy. But I was so sick during the stem cell transplant with septic shock and that helped determine what I decided to do.
Everyone is unique and it’s a big decision, but I wanted to live my life and not have the risk of graft versus host disease, which could actually limit the enjoyment of life and so that was also within my decision.
I just thought that [CAR T] was the right decision for me. It was not recommended by my oncologist. [As] a matter of fact, my oncologist thought that I should go ahead and have an allo transplant using my son as a donor, as a haplo (haploidentical) and I didn’t want to do that.
Robyn S.
Stephanie, TPS: It’s a great example of this equation. For everybody, it’s a different equation in terms of what you weigh more heavily. Is it how long you think you can get more out of life in terms of survival or is it quality of life?
Drs. Brody and Phillips, I know that this happened back in 2016 so it’s a very different landscape than now. But anything you want to add in terms of the decision-making or talking about this with a patient?
Dr. Phillips: She highlighted a very important dilemma we have. The decision for an allo transplant is probably very controversial amongst lymphoma doctors. You have some people who are very beholden to it and others who probably would never send a patient for an allo transplant based on what Robyn has already mentioned. The simple fact of the risk of graft versus host disease, finding an appropriate donor, and, with lymphoma, actually making sure the cancer is in remission before you get to an allo.
I wish we had a better system to illustrate clinical trials throughout the US. I don’t think we still have a great system, even in 2023. A lot of us depend on clinicaltrials.gov or word of mouth versus having a good system where any patient can just plug in their disease and we pop up all these studies and trials that are actually active and open.
That’s the thing about clinicaltrials.gov. Just because they list sites doesn’t necessarily mean those sites are actually up and active, which I think a lot of people don’t realize.
Dr. Brody: I agree with everything Tycel said. Robyn was either lucky or prescient or maybe a combination because in retrospect, if it was me, CAR T versus allo transplant, it would be a no-brainer.
We now have randomized trials comparing CAR T to autologous transplants for those that relapse quickly, 12 months after front-line therapy. CAR T is probably both more effective and kinder with less of those toxicities. CAR T can be toxic, but overall, head to head, I would probably rather get a CAR T-cell therapy than an autologous transplant. I think most people would probably agree.
It’s tricky. If you’re a specialist, you think that’s the way to go. A transplant doctor will say, “Yeah, we could do [a] transplant.” It’s the same with clinical trials. If you’re a doctor that doesn’t focus on clinical trials, you won’t think of that. It won’t come to mind.
Robyn is one of these rare people that can advocate very well for herself. You do need doctors sometimes to be able to help advocate for you.
The last time we looked, 25 to 30% of patients that are eligible are getting CAR T. That means the vast majority of patients are not getting CAR T.
Dr. Brody
What is CAR T-cell therapy?
Stephanie, TPS: I love that, Dr. Brody, thank you.
Let’s talk about CAR T more in depth. What exactly is CAR T-cell therapy and what does it entail in terms of how people actually go through it?
Dr. Brody: We take a little bit of a person’s immune system, some immune cells from their blood. They literally do gene therapy on your immune cells. They put a new gene into your immune cells and when we put [them] back into you, that gene allows those immune cells to go find lymphoma and then kill lymphoma.
Humans have about 20,000 genes. This gene that they stick into those immune cells is not one of those 20,000. It’s amalgamated from five other genes put together into one gene. That gene is called CAR, a chimeric antigen receptor. You get FluCy (fludarabine and cyclophosphamide) chemo and then we re-infuse the CAR T cells.
A few years ago, we would say folks with multiple-relapsed DLBCL didn’t have curative options just like patients with metastatic breast cancer. In those patients, we would say the CAR T-cells might cure 35 to 40% of patients. Going from what we call 0% to 40% sounds like it’s miraculous. Not 100% so still a lot of room for improvement. The efficacy is very impressive, miraculously impressive, but it’s not benign therapy.
There is this risk of side effects and probably 20% of people get some of these high-grade side effects. The most commonly discussed one [is] cytokine release syndrome, CRS. It’s like having a terrible infection, but there’s actually no bacteria [or] virus infecting you and people can land in the intensive care unit because of that.
Another one [is] neurotoxicity [or] ICANS (immune effector cell-associated neurotoxicity syndrome). It can literally be a type of encephalopathy. People can start hallucinating [or] become unconscious. It can be dangerous.
These high-grade toxicities might happen in up to one in five patients. Even if it doesn’t happen in the other four out of five, we don’t know which one in five is it going to happen [to] because we have to monitor all of those patients very closely, usually in the hospital.
The last time we looked, 25 to 30% of patients that are eligible are getting CAR T. That means the vast majority of patients are not getting CAR T.
Dr. Phillips
Benefits and challenges of CAR T-cell therapy
Stephanie, TPS: With that being said, Dr. Phillips, if you could just touch on the benefits and the challenges?
Dr. Phillips: The biggest excitement is that we’ve been all talking about immunotherapy for decades and here we are with a true immunotherapy with a much better and manageable safety profile than what we typically would see with an allogeneic stem cell transplantation.
The uptake of CAR T is not what it should be. The last time we looked, 25 to 30% of patients that are eligible are getting CAR T. That means the vast majority of patients are not getting CAR T due to access issues, meaning they can’t get to a CAR T center, or they don’t have anybody that needs to be there with them or relocate to a center for a month to get CAR T.
These are all logistical challenges that we are trying to fix and overcome along the way, but it’s not been necessarily the easiest thing to get over because these patients will need caregivers, especially as we’re trying to move CAR T to an outpatient setting. They have to have somebody that can take care of them.
Financially, I don’t think CAR T is going to be feasible moving forward where, originally, patients are hospitalized for 30 days. Unfortunately, payers aren’t going to pay for that and hospitals can’t [foot] the bill for that any longer.
They do need some support to help take care of them, which is not unfortunately dissimilar to what we see with transplant patients. The hope is that requirement may ease for some patients who aren’t necessarily going through complications. But right now, unfortunately, it is a requirement in most centers that they have somebody to take care of them.
CAR T-cell therapy for refractory patients?
Stephanie, TPS: [With] refractory patients, [they undergo] different treatments [and] there’s no response. It’s not [that] you were in remission and then you relapsed. It just didn’t respond. When would you consider CAR T for someone in that position?
Dr. Phillips: Thankfully, now, in second-line. That generally would be the immediate treatment at this point, unless there’s some reason that they can’t get CAR T.
Those patients should be the patients we get to CAR T because we already have two studies that have demonstrated that CAR T was superior to autologous stem cell transplantation with both axi-cel and liso-cel in this patient population. This is the ideal patient population for CAR T.
The key thing with bispecifics, at least from what we can see from the early stages, is that they appear to be effective in patients with relapsed/refractory diffuse large B-cell lymphoma.
Dr. Phillips
What are bispecific antibodies?
Stephanie, TPS: Wonderful. Now let’s get into bispecific antibodies. Dr. Phillips, what are bispecifics?
Dr. Phillips: The easiest way to think about bispecifics is like [an] off-the-shelf CAR T product. It still works to utilize your own T cells to fight off cancer, but instead of the manufacturing process, it basically administers an antibody that will bind to some marker in your cancer, bind to your T cell, which will force an interaction between the two, [and] lead to T-cell activation and [hopefully] some sort of T-cell expansion, growth, etc.
These antibodies, at least the CD20/CD3s and some of the newer CD19/CD3s, are a bit better than what we have with blinatumomab, which was given as a continuous infusion, by allowing those Fc portions and just muting them to be still intact to the antibodies. They have a much longer half-life so these things can be administered more conveniently.
If we look at the agents that we have that will likely get approval, we have mosunetuzumab, which is approved for follicular lymphoma. [This] is given as a step-up dosing once a week until you get to [a] full dose and then once you reach full dose, given every three weeks for either eight or 17 cycles.
We have epcoritamab, which will likely get approval for diffuse large B-cell lymphoma. Again, given in a step-up dosing every three weeks, but will continue weekly through the first three cycles and biweekly from cycles four through nine, and then once a month indefinitely.
Then glofitamab, which is another CD20/CD3 bispecific antibody given in step-up dosing. This one is given with a pre-medication obinutuzumab to help reduce the risk of CRS, which is still prevalent because it’s a T cell-directed therapy, and then given once every three weeks thereafter. This one is also given for a fixed dose of just 12 cycles.
Then we have odronextamab [and] plamotamab in the pipeline of other bispecific antibodies and there are many more coming down the line.
The key thing with bispecifics, at least from what we can see from the early stages, is that they appear to be effective in patients with relapsed/refractory diffuse large B-cell lymphoma. Some studies have shown that they are effective in patients post-CAR T. The question that we’ll get into later is: which post-CAR T patient is actually a patient that’s going to respond to a bispecific?
The same side effects exist. CRS occurs, probably not to the severity and intensity [that] we see with CAR T and the management strategy will probably end up being a bit different. There is ICANS or neurological toxicity. Again, not to the degree of severity that we see with CAR T but still present.
A lot of community physicians and patients will get first-hand experience, good or bad, with these bispecifics and, hopefully, more guidance will get out there for how to best manage some of these events because a lot of these physicians haven’t dealt with this.
In a couple of years, hopefully, as more and more physicians get comfortable with these drugs, they’ll get more access to patients and they’ll be more comfortable managing the side effects. This will probably have a bigger catchment area just because of [fewer] restrictions on these drugs than what we see with really CAR T at this point.
We don’t want to confuse complete remission with cure. Just because we can’t see any cancer doesn’t mean there might not be a little bit left.
Dr. Brody
What is the comparison between epcoritamab and glofitamab?
Stephanie, TPS: Dr. Philips does a great summary of a huge space so [I] appreciate that. It sounds like, for DLBCL in particular, there are two that are a little bit more advanced in the studies than the rest although there are many that we should be watching out for. Dr. Brody, between epcoritamab and glofitamab, anything you see with the response so far [in] the clinical trials?
Dr. Brody: Overall, these two are much more similar than different.
They’ve been in many hundreds of patients. They focused on a trial of about 150 patients each and both had complete remission rates of about 39%, 39.4% for both of them so that’s pretty similar. Again, just under 40% of people. The tumor melts and disappears so that we cannot even see it on a PET scan or a CT scan.
We don’t want to confuse complete remission with cure. Just because we can’t see any cancer doesn’t mean there might not be a little bit left. But it does seem like a lot of these complete remissions are very durable [and] very long-lasting.
We definitely have patients in complete remission from these therapies for more than two years. We don’t have five years yet because these medicines haven’t been around for five years. But if a person stays in complete remission for two years, the chance of being cured seems to get pretty good. That’s true for many therapies, certainly for CAR T and for other therapies.
One little difference between them is the way they are administered. Epcoritamab is given as a subcutaneous shot, just a shot under the skin, so pretty quick. Glofitamab is given as an infusion. The first infusion is eight hours. Later on, it becomes four hours and two hours. A little bit more time intensive there, but not too bad. Maybe that’s a point in favor of epcoritamab.
I’ll give a point in favor of glofitamab, to be fair. The glofitamab studies are mostly designed to be time-limited. You get 12 cycles, about nine months of glofitamab, and then you just stop the therapy and you’re in complete remission. We just keep an eye on you. If you were to relapse, you could get more of it, but if you’re in complete remission, we just stop giving the therapy. That’s just how they were designed so we don’t have to give it forever.
The epcoritamab studies have been designed to just keep going. As long as the person is in remission and doing well, just keep giving it.
It’s hard to say which one is better [or] worse. I find half of my patients like the idea of, “Yeah, give me a break. I’ve been through a lot,” and [the other] half say, “I don’t know. I kind of want to keep getting this therapy.” We don’t know which one is right or wrong. Some people see the benefit of time-limited therapies. They don’t have to keep coming to the doctor as frequently.
Maybe a little bit of benefit of one over the other in both directions but, overall, more similar than different, [with] remarkable efficacy, and much easier to use than CAR T cells.
If I do not have a caregiver and someone’s recommending CAR T, what kind of options come up there? [The] one-word answer is bispecifics.
Conceptually, it’s the same possible side effects, but, thankfully, we’ve mostly just seen much less of them and lower-grade versions of them.
Dr. Brody
Side effects from bispecific antibodies
Stephanie, TPS: Assuming bispecifics are approved and it’s not being used as a clinical trial for somebody, what about the side effects, Dr. Brody? Dr. Phillips did [mention] CRS seems to be [a] lower grade in bispecifics as opposed to CAR T. Anything else?
Dr. Brody: As Tycel said, conceptually, it’s the same possible side effects, but, thankfully, we’ve mostly just seen much less of them and lower-grade versions of them.
The average CAR T-cell patient today is sometimes still spending 11 days in the hospital just for observation, whereas the average bispecific antibody patient usually spends one day in the hospital. Even though the vast majority of them don’t get any of those side effects, at the moment, we have to still observe them all just to make sure that we don’t miss the one out of ten that gets the bad side effect.
For DLBCL, the plan with most bispecifics still is at least one day of observation. Probably about 5% can get the high-grade version of CRS and much less than 5% get neurotoxicity. Rare, but it can happen and, therefore, requires a bit of monitoring.
If I have access to both, if I can’t get CAR T, then ideally, a bispecific is good in that situation.
Dr. Phillips
Statistically, you would want to get both.
Dr. Brody
CAR T or bispecifics for relapsed/refractory patients?
Stephanie, TPS: How do you consider which one to go to first for relapsed/refractory patients? What are the considerations?
Dr. Phillips: CAR T has the more definitive data so if you have access to both, you’re hard-pressed to put a bispecific before CAR T at this current date. I would say CAR T then bispecific thereafter, pending the response to the patient with CAR T.
If the patient has no response to CAR T, I have very little faith that they will have a response to a bispecific. We’d feel much, much [more] comfortable if a patient had some sort of response to CAR T [and] then lost it to try to resurrect that response with the bispecific.
But if I have access to both, if I can’t get CAR T, then ideally, a bispecific is good in that situation.
Dr. Brody: It’s actually less of a question of which is better, CAR T [or] bispecifics, because, frustratingly, for all the advances that we’re bragging about, the numbers are that the majority of patients are not cured by either.
Statistically, you would want to get both. You’d want to have the option to get both. As Tycel just said, if you get CAR T today and they fail 30 days from now, quite honestly, you probably won’t be able to get bispecifics because there [are] no trials that allow rapid failing CAR T patients to get access to bispecifics.
We’ve done the opposite in our patients quite a bit where they’ve got bispecific [and] if they stayed in complete remission, they kept going. But we had a few where they progressed eventually and we gave them CAR T-cells.
In a lot of cases, clinical trials are some of the best medical care that you’re going to receive.
Robyn S.
Clinical trials
Stephanie, TPS: I like that we’re comprehensive about this. We could talk about clinical trials really quickly because I think there’s a lot of misunderstanding. Robyn, you went through a clinical trial. Anything you want to say from the patient’s perspective? I think people think there’s a placebo or I’m going to be in an experiment and there’s a lot of fear. What would you like to tell people about your actual experience with a clinical trial?
Robyn: As a patient and also as a physician, it’s important that people realize that in a lot of cases, clinical trials are some of the best medical care that you’re going to receive. They’re cutting-edge. It is often the way to go in unusual cancers or some other diseases that can’t be controlled by anything else.
Dr. Phillips: That’s the thing people need to remember. It’s not guinea pigs. This is how we advance the field, especially in diseases without [a] standard of care. This is really your chance to get something that could potentially be life-saving. More people should be offered clinical trials.
Robyn: Keep your options open. Keep your mind open. Do some research. Read.
In this case, this is a blood cancer group. Talk to LLS if you’ve relapsed. See what their opinions are and get several opinions.
Be your own advocate. Physicians don’t agree on things, [which] doesn’t make somebody wrong or right. It’s a process. Science is not exact. It’s not black and white so you need to figure out what’s right for you. Do your research and don’t be afraid because a clinical trial might be the solution for you.
Stephanie, TPS: Thank you, Dr. Tycel Phillips, Dr. Joshua Brody, and Robyn. Thank you so much for making this such an enjoyable conversation about what could be very overwhelming.

Be your own advocate. Physicians don’t agree on things, [which] doesn’t make somebody wrong or right… You need to figure out what’s right for you.
Robyn S.
For FREE 1:1 support to enroll in and stay in a clinical trial, check our The Patient Story’s partner organization in the program, The Leukemia & Lymphoma Society, and its Clinical Trial Support Center!
Here is a direct link to a form to fill out – and someone from The LLS will reach out after.
DLBCL Patient Stories
Jonathan S., Diffuse Large B-Cell Lymphoma (DLBCL), Stage 4
Symptom: Severe shoulder pain
Treatments: R-CHOP chemotherapy, methotrexate, focal radiation, autologous stem cell transplant
Leanne T., Follicular Lymphoma Transformed to DLBCL, Stage 3B
Symptoms: Fatigue, persistent cough
Treatment: R-CHOP chemotherapy, 6 rounds
Paige C., Diffuse Large B-Cell Lymphoma (DLBCL), Stage 4
Symptoms: Weight loss, extreme fatigue, swollen lymph nodes in the neck
Treatment: R-EPOCH chemotherapy



One reply on “DLBCL: The Latest in Treatment and Research”
I am 74 years. I was diagnosed first with endometrial cancer in 2004that whole pelvic and overuse removed. No lymph nods were involved and the oncologist said I was cancer free. But on 2007 I had a swollen lymph nods on my eyelid that it was Defuse large B cell lymphoma. I did R-chop treatment 6 rounds. Oncologist said I was cancer free.but again came back after 3.5 years only one swollen lymph nod in my left neck. I had Stem cell Transplant after 3 times in hospital for chemotherapy and then stay a month in hospital that was so tough. But it came back 3 months later that I had scan. Oncologist wanted to to T cell that I did all the check up tests that I passed. The day before cell collection one social worker that on stem cell transplant I asked to be change because she was making miserable I asked to be changed she said I can’t handle the T cell treatment and my oncologist cancelled it. And after a month started Mor-208 treatment with immune therapy ever week. After 2 weeks my neutrophil went so low that he stoped the Revilmid 25. Then after Zorvix shot he changed to 15mg Rivilmid pill that after 10 days my neutrophil went to 0.01 he stoped the med for a month I receive 2 shots a week until my cells were up now he said I start the 10 mg to see what happens.the interesting thing is my 1-12-23 pet scan showed no more cancer but he says we continue in case you have a microscope lymphoma cell in my body. Please some one that know about this treatment tell me about it. I don’t see anyone to mention that.I am thankful for your services and sorry for long history. I have to say that I am doing fine and walk 10,000 to 15000 steps a day. And almost never had care giver and took care of myself.