CLL Treatment Side Effects
Patient Discussion ft. Dr. Matthew Davids, Dana-Farber Cancer Institute
Our CLL and SLL patients join to power a discussion about common treatment side effects, sharing their personal experiences, and getting some guidance from our featured CLL/SLL expert, Dr. Matthew Davids of Dana-Farber Cancer Institute.
- Introduction
- BTK Inhibitors
- BTK Inhibitors Side Effects
- Ibrutinib (Imbruvica) Patient Experiences
- Acalabrutinib (Calquence) Patient Experiences
- Michele N., CLL Patient on Acalabrutinib
- Headaches
- Coughing
- Less likely side effects vs. other BTK inhibitors
- Similar side effects to other BTK inhibitors
- Leesa P., CLL Patient on Ibrutinib, Switched to Zanubrutinib
- Gastrointestinal side effects
- Jane D., CLL Patient on Zanubrutinib
- Atrial fibrillation (A-fib)
- BCL2 Inhibitors (Venetoclax or Venclexta)
- CD20 antibodies (rituximab, obinutuzumab)
- Doublets (2-targeted drug regimens)
- Triplets
- CAR T-cell therapy
- Support for CLL/SLL side effects
- CLL Patient Stories
Thank you to Pharmacyclics & Janssen for its support of our patient and care partner program! The Patient Story has full editorial control over the content.
Introduction
Welcome
Michele Nadeem-Baker: Welcome to our CLL Patient Roundtable. Today, we’re going to be talking (about CLL) treatment side effects and across the range of all available therapies. I’m your host and also one of you, a CLL patient. I’m really excited about today’s program because it’s not only for patients, but it’s with patients here.
We’re going to be putting a CLL specialist to the test and telling him about different side effects that we’ve been having, and trying to get some answers and some relief. Which ones are the most common? Their impact on our quality of life and yours and learning how to get through them.
Audience Poll: Whom do you go to for your CLL/SLL care?
We’re just going to jump right into this program, right into our first poll. That is just to get an idea of some things. Whom do you go for your CLL or SLL care? Is it a CLL or SLL specialist? A general hematologist- oncologist and general oncologist? Or you’re not sure? So whom do you go to for your CLL, SLL care?
The majority of you see a hematologist oncologist, 56% and the rest of you, 44% see a CLL or SLL specialist. This is good. That is really good to know.
I’m going to first introduce you to our panelists and I’m going to tell you where they’re from, when they were diagnosed, and if they’re on treatment.
Patients in Discussion

Michele N., CLL Patient on Acalabrutinib
- 2012: Diagnosed with CLL
- 2012-2015: Watch and wait
- 2015-2019: Ibrutinib (Imbruvica) + FCR [Clinical Trial]
- 2019-2021: Watch and wait
- 2021-Present: Acalabrutinib (Calquence)
Michele Nadeem-Baker: First, there’s me. I am not only a medical journalist, but I am also a patient. As I had said before, I was diagnosed in 2012 when I was living between Boston and South Florida, and then I moved back permanently to Boston and I started treatment at Dana-Farber Cancer Institute in 2015. That was the iFCR trial. I was on that until 2019. Then I went back on treatment this past fall and I’m now on ibrutinib.
Brad A., CLL Patient on AVO Clinical Trial
- 2010: Diagnosed with CLL
- 2010-2014: Watch and wait
- 2014: FCR chemo
- 2014-2020: Watch and wait
- 2020-Present: AVO trial (acalabrutinib + venetoclax + obinutuzumab)
We have Brad from Texas. He was diagnosed in 2010. Watch and wait until 2014. He was on FCR five months. He was off treatment until September of 2020. Then he started and he remains on a clinical trial some of you probably heard of and that is the AVO, otherwise known as the acalabrutinib, venetoclax, obinutuzumab trial. He’s still on that.
Hannah D., CLL Patient on Ibrutinib
- 2013: Diagnosed with CLL, put on FCR chemotherapy
- 2013-2016: Watch and wait
- 2016-Present: Ibrutinib
Next we have Hannah, the lovely Hannah from Indiana. She was diagnosed in 2013 and she went immediately on treatment, as some of you do, and she was on it for four months. She’s been off treatment Back in 2016, she started on ibrutinib and continues on it today.

Jane D., CLL Patient on Zanubrutinib Break
- 2014: Diagnosed with CLL
- 2014-2021: Watch and wait
- 2021-2022: Zanubrutinib, presently on break
We also have more patients with us. Jane from New Jersey, diagnosed in 2014. She had a nice watch and wait time until last year. She started zanubrutinib. She’s currently on a break from that treatment.
Leesa P., CLL Patient on Zanubrutinib
- 2008: Diagnosed with CLL
- 2008-2018: Watch and wait
- 2018-2021: Ibrutinib (Imbruvica)
- 2021-Present: Zanubrutinib (Brukinsa, not FDA-approved for CLL/SLL)
Next, we have Leesa from California. She was diagnosed in 2008, and in watch and wait until she started ibrutinib back in 2018. Then after over three-and-a-half years on that, she was switched directly to zanubrutinib. That was about eight months ago.
Lynn B., SLL Patient on Ibrutinib
- 2013: Diagnosed with SLL (small lymphocytic leukemia)
- 2014:
- Lenalidomide (Revlimid) + rituximab (Rituxan)
- Ibrutinib (Imbruvica) + rituximab (Rituxan)
- 2014-Present: Ibrutinib (Imbruvica)
Last but not least Lynn from Texas diagnosed in 2013 on treatment nearly immediately on REVLIMID and Rituxan. Lynn has SLL and he was on that combination for three months and then ibrutinib for the last eight years and remains on it.

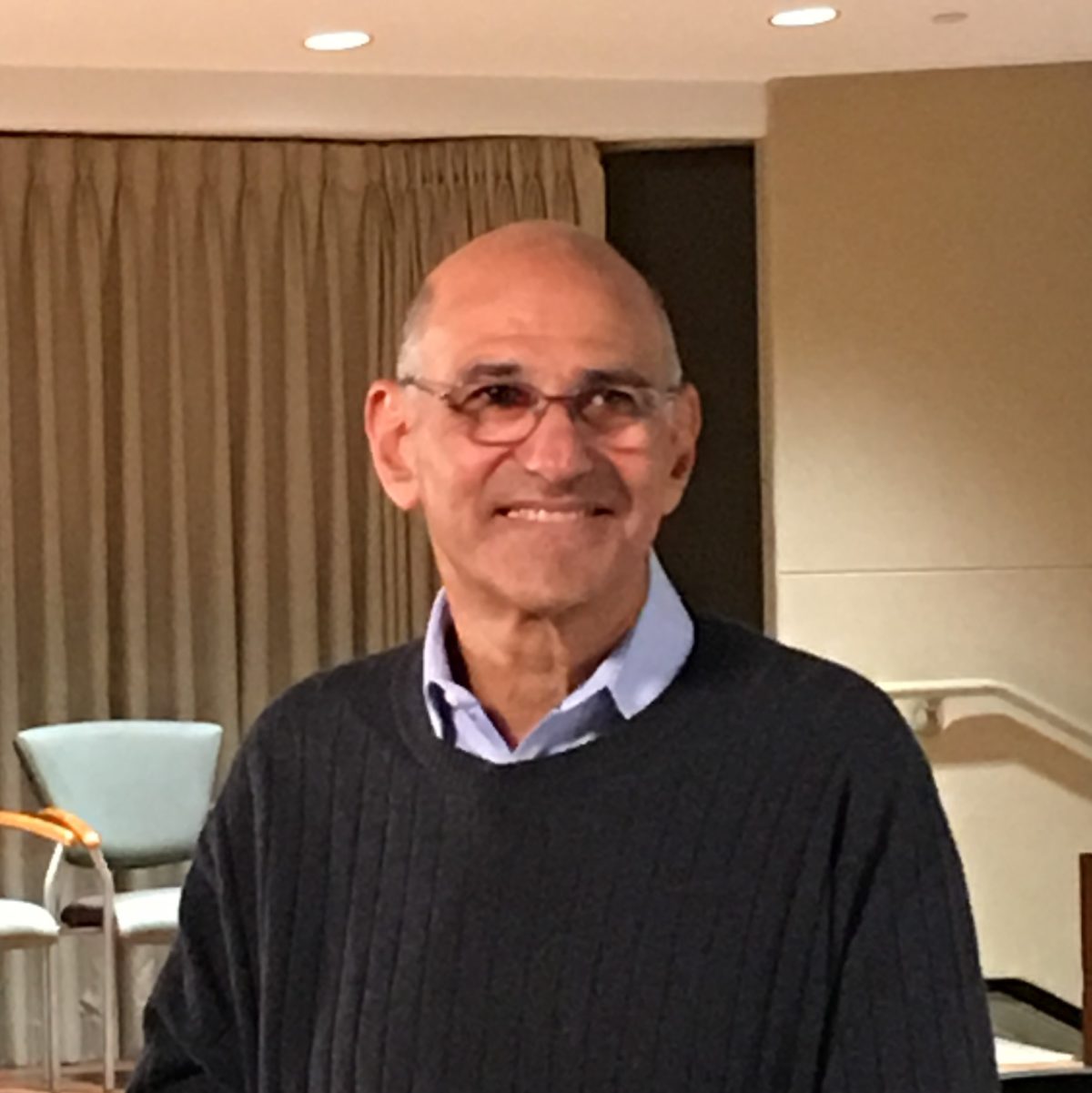
Dr. Matthew Davids, CLL Specialist
Thank you to our patient panel for being with us. With us, to give us the facts and answers today on our panel, we have Dr. Matthew Davids of Dana-Farber Cancer Institute. He is the director of clinical research for the Division of Lymphoma, is an associate director of the CLL Center and an Associate Professor of Medicine of Harvard University Medical School.
I am so excited to have him with us as I do go to Dana-Farber and he is so loved there, and he’s really renowned around the world for all of what he’s done in CLL. Thank you for being here, Doctor.
Dr. Matthew Davids: Thanks, Michele.
BTK Inhibitors
Michele Nadeem-Baker: We’re going to start today, Dr. Davids, by talking about BTK inhibitors that are currently used, their side effects, and how you administer them. My first question for you is is the majority of patients on, whether it be singularly or in combination, on BTK inhibitors these days?
Dr. Matthew Davids: Let me take a quick step back and just tell you that I’ve seen how the field has evolved. I started seeing patients in around 2009, and at that time, all we had available was chemo-immunotherapy. It was right around that time also that the first BTK inhibitors came into clinical trials, and we treated some of the very early patients on single agent BTK inhibitors, including ibrutinib.
It’s really amazing to see how far the field has come in about a decade. And we’ll talk, I’m sure, about all these different mechanisms, different combinations, etc.
Now I think the most common way that the BTK inhibitor drugs is given is as a single agent given continuously. And the estimates that I’ve seen is about a third of CLL patients who are on treatment are on just a single BTK inhibitor therapy.
Michele Nadeem-Baker: What are the ones just to review that are being used?
Dr. Matthew Davids: Ibrutinib was the original one. It’s definitely being used the most widely across the world in CLL. The other one that’s approved now for patients with CLL is acalabrutinib, which has been approved for a few years now and is also increasingly being used.
It’s interesting that I think at least a couple of you are on zanubrutinib since zanubrutinib is not yet approved for CLL, but it is approved for related conditions like mantle cell lymphoma, for example. We have a lot of robust clinical trial data supporting the activity and safety of zanubrutinib in CLL. So we expect it to get a formal label very soon. Some of you guys are on the cutting edge because you’re already on it before it’s even approved for CLL.
BTK Inhibitors Side Effects
Michele Nadeem-Baker: Regarding side effects, why don’t we go one by one into these different drugs and ibrutinib? I was curious what the most common side effects are and then we’ll go to some of our panel today to tell you about theirs, and ask you some questions.
Dr. Matthew Davids: One just kind of general statement I would say about the BTK inhibitor class of drugs is that they have some common side effects between them. Even though I think a lot is made out of differences between the drugs, I’d say there’s a lot more in common between the three drugs we’ve been talking about, ibrutinib, acalabrutinib, zanubrutinib than there is in terms of differences.
Most of the side effects that we see can occur with any of these three drugs. Starting with ibrutinib, but this really would apply to the other drugs as well, when patients first start on it, it causes a lot of changes in the body.
Fatigue
There’s a lot of CLL cells that are dying off. So a lot of patients describe fatigue when they’re first getting started. It can take some time to get through that, sometimes weeks or even months.
Rising lymphocyte counts
The other thing that’s very common with all of these drugs is that we see the lymphocyte count rising in the first few weeks that patients start out on treatment. This is something I always find very helpful to counsel the patients about ahead of time, because in the past, when I’ve made the mistake of forgetting to do that, I see patients kind of freaking out that their white blood cell count is going up and when really we’re trying to get it to come down eventually.
But we learned over time that that’s okay. There’s nothing bad about the white count going up. It actually reflects the cells moving out of the lymph nodes and then they die off in the blood. So it’s actually a good thing when we see that happening.
Gastrointestinal issues (diarrhea)
Patients also describe diarrhea sometimes when they first start ibrutinib or the other drugs. It’s quite common.
Less common side effects
- joint aches
- rash
- cardiovascular- atrial fibrillation
- high blood pressure
- bleeding
- brusing
You can see other things a little bit less commonly, like joint aches or rash, and then the cardiovascular side effects, which can crop up at any time, things like atrial fibrillation or high blood pressure and then the bleeding and bruising.
That’s another thing a lot of patients will notice early on is bruising. It’s less common to have more serious bleeding issues, but we definitely see bruising more commonly.
Ibrutinib (Imbruvica) Patient Experiences
Michele Nadeem-Baker: That was a great overview and a great way to launch into this section. Thank you, Dr. Davids. I would love to jump to our panel to describe some of the things that they have experienced. I’m going to start with Lynn in Texas with SLL.
Lynn B., SLL Patient on Ibrutinib
Lynn. you’re on ibrutinib, do you still have some of the side effects or are you more like what Dr. Davids was speaking about? Like you had them more in the beginning?

Summary of side effects:
- Fatigue
- Joint pain/muscle cramps
- Brittle nails
- Frizzy hair
- Neutropenia at 3 months
- Neupogen injections resolved the problem
- Neuropathy at 1.5 years (numbness not pain)
- Bruising
Lynn B.: Yes, because I was switching from lenalidomide with Rituxan to ibrutinib with Rituxan. So the fatigue was already there, as I began and went on ibrutinib.
Then I had the joint (pain). That was the most prominent thing that first week or two is that the joint and muscle pain that was there, and muscle cramps, those things were just a little bit overwhelming, but they diminished with time.
Following that, I had the brittle nails that came along and frizzy hair. Neutropenia at three months, my neutrophils were low and I had a doctor at MD Anderson gave me, prescribed the Neupogen.
I had three injections of that and the neutrophils rebounded. That’s the only problem I really had with blood counts. Remember I’m SLL, so they’re looking at my lymph node size and they were all internal and at three months they were significantly reduced.
But I had neuropathy, came along at about a year-and-a-half and I continue to have (it). It’s not a pain, but it’s a kind of a numbness in the feet and a tingling in the hand sort of thing. You mentioned hemorrhaging earlier. I do have some, just if I bump anything like most folks on these kinds of drugs, I do have some bruising that will occur. If I take a hard lick, I’ll put pressure on it or even get ice to be sure that it doesn’t get carried away. So just some things to think about. Dr. Davids, I’m sure you’ve heard all of them.
Causes of neuropathy
Michele Nadeem-Baker: Dr. Davids, when you have patients that come in and again with this, we’re trying to help all who are watching us to get ideas of how to have these conversations with their doctors. Your being a great doctor (who) answers his patients’ questions, we would love for you to be able to answer some of the things that Lynn was just talking about.
Is there anything that can be done for neuropathy since his started a little later on? Is that something that can happen once you’re taking the drug for a while or does it usually present itself early on?
Dr. Matthew Davids: Neuropathy can happen on BTK inhibitors, but I have to say it’s quite rare. It’s not one of the common side effects we see. Generally, I start looking for other causes if I see neuropathy. I think more common things like diabetes or blood pressure issues, these sorts of things.
But there definitely have been some patients I’ve had who’ve had neuropathy and I have not been able to identify another cause. So I’ve tried things like reducing the dose of ibrutinib, for example, to see if that helps, maybe with some success.
If it’s a painful neuropathy, there are drugs you can take to help manage the pain. Gabapentin, for example, can be very helpful for that type of pain.
Help for joint and muscle pain/cramps
Lynn B.: Since the joint and muscle pain and cramps is something almost everybody has, is it just weather the storm or is there any help for the patients (who) are suffering with that?
Dr. Matthew Davids: I do think the joint and muscle pain is more directly related to the BTK inhibitor drug. I think that’s more clear than the neuropathy, where it’s often a different cause. So with that one, in addition to obviously taking medicine to manage the pain, you can try reducing the dose.
The other trick that I’ve used sometimes, especially if it’s happening early on, is to actually add a low dose of prednisone, which is an anti-inflammatory drug, and that can sometimes take those aches away.
Then as your body adapts to the BTK inhibitor, sometimes you can stop the prednisone and not have the pains as much. But I’ve had patients where the aches and pains are so difficult to deal with on one BTK inhibitor that we actually just try switching to a different BTK inhibitor. Sometimes that’s been successful, as well.
Hannah D., CLL Patient on Ibrutinib
Infection (Urinary tract infections)
Hannah D.: I, like Lynn, I started out with the terrible joint pain and aches, but I persevered and they did diminish almost completely, eventually.
What I’m experiencing right now is widespread infection throughout my body. No one has really pinpointed the source of it all, but my body is reacting to it where all of my joints from my shoulders down to my toes are inflamed and just some other side effects that are not pleasant.
I’m being treated with multiple antibiotics and antiviral, and my doctor’s appointments are ongoing. But what I wanted to ask you, I know that infections are not uncommon when on ibrutinib, which I’ve been on, like Michele said, for six years.
Not related to joint pains, but yeah, I’m having UTIs. I had a couple of UTIs in the beginning and they did say nothing to worry about. That is pretty common with IMBRUVICA. I took antibiotics and it was resolved. It wasn’t that problematic, but it seems to be now.
This late in the game having been on it, would it be common for that to be an effect from IMBRUVICA?

Dr. Matthew Davids: There’s a couple of different factors here. One of which is that, I think as you all realize, just by virtue of having CLL, it does increase the risk of infection generally and that’s whether you’re on treatment or not.
Even when you’re on different types of treatment, in a way, it actually doesn’t matter too much. No matter which treatment you’re on, it does cause some additional suppression of the immune system that can increase the risk of infection.
Now, with the newer drugs like ibrutinib and the BTK inhibitors, we think those risks are generally less than what we saw with chemotherapy-based treatments like FCR than some of you have had. But that being said, infections can still crop up at any time.
What BTK inhibitors are doing is they’re shutting down B cells, that’s the type of cell that CLL cells come from. But it’s also shutting down a lot of your normal B cells, which are there to help you make antibodies and fight off infections. So as long as you’re on a drug like a BTK inhibitor, you’ll have some suppression of your immunity.
Possible solutions
Dr. Matthew Davids: One thing that hopefully they’re doing is following your IGG levels, immunoglobulin G. If those are low and you’re having frequent infections, IVIG, intravenous immunoglobulin can be helpful to reduce infections.
If you’re already doing that, the other thing I’ve had some luck with is a certain antibiotic called Bactrim or trimethoprim sulfamethoxazole. Being on that at a low dose chronically could sometimes help reduce infections.
Hannah D.: Good to know. Thank you.
Nail changes
- Brittle nails
- Nail loss
Michele Nadeem-Baker: Dr. Davids, one last thing on. This could be a common one between all BTK inhibitors and maybe you can let us know. And that is the nail infection part or the thinning of nails or breaking of nails or I’m not even sure exactly. I just know everyone talks about their nails. Should people be going to a specialist for that? Or is that something that their hematologist-oncologist or specialist can address?
Possible solutions
Dr. Matthew Davids: I think if it’s mild, that’s maybe something the hematologist-oncologist can start with. There’s been some anecdotal success I think with biotin supplementation, vitamin can help with that a bit.
Also for a lot of patients, that’s fairly seasonal. They find in the summer and then in the winter when it gets dry and their hands get cracked, at least in this part of the country the nail issues get worse.
I’ve had patients who’ve had some luck, wearing moisturizing gloves at night, for example, to keep their fingers nice, moist, so aquaphor and these sorts of things.
But if you’ve tried some of those basic things that are still having issues, it is helpful to see a specialist and sometimes it’s actually the dermatologist. If you can find a good dermatologist, they have expertise in skin and nails and they can have some other helpful suggestions.
Michele Nadeem-Baker: I know for an example, at Dana-Farber, we’re lucky enough to have a dermatology department which specializes in being able to identify what all these things are and just look at things in a nanosecond and say, I know exactly what that is and this is what you need.
That’s just been a fabulous resource, I know for me. If anyone else has that, where they go to or ask their doctor, their oncologist, (whom) they should see, because I know my team is who had suggested it. They have been a fabulous resource.
Acalabrutinib (Calquence) Patient Experiences
Michele Nadeem-Baker: Let’s switch to acalabrutinib. Some of these are going to be extremely similar. On acalabrutinib, I believe Brad is on it and I am on it, but Brad’s on it along with venetoclax and (he) was on obinutuzumab, so I’ll share with you.

Michele N., CLL Patient on Acalabrutinib
Summary of side effects:
- Headaches
- Neuropathy (worsening)
- Fatigue
Michele Nadeem-Baker: For me, in the beginning, and I hear that this is pretty common, you had mentioned it – headaches. I had it for maybe the first five weeks and it improved.
The first month I started my (treatment), I don’t know if I had neuropathy to begin with, but if I didn’t, neuropathy worsened. I think I had a minor part to begin with and it worsened, and sometimes fatigue, but certainly not as fatigued as I had been in the past on other treatments.
So Dr. Davids, what are you seeing with acalabrutinib, it being the second drug out in BTK inhibitors. Are these more common for acalabrutinib or are you seeing some other side effects that are more prevalent?
Headaches
Dr. Matthew Davids: We’re fortunate now that we have a couple of large studies that have compared ibrutinib to the other drugs. One study compared ibrutinib directly to acalabrutinib and then another study compared ibrutinib to zanubrutinib.
So specifically with acalabrutinib in that randomized study, the things that were a little bit more common with acalabrutinib were headache, exactly as you described.
Possible solutions
Dr. Matthew Davids: That’s one that, for whatever reason, seems to be particularly responsive to caffeine. So I usually tell patients, drink a little extra coffee in the morning, maybe a Tylenol, and most cases like for you, it passes within a few weeks of starting the drug.
Coughing
The other thing that came out in the randomized study was the cough was a little bit more common in patients on acalabrutinib, not really clear why. That also tended to be very transient and went away on its own.
Less likely side effects vs. other BTK inhibitors
- Atrial fibrillation (A-fib)
- Raise blood pressure
- Bleeding issues
And then most other things were actually less with acalabrutinib. So there was a less likely chance of developing atrial fibrillation, less likely acalabrutinib will raise the blood pressure, and less likely that you’d have the bleeding issues that we were talking about.
Similar side effects to other BTK inhibitors
- Infection rates
- Significant bleeding rates
- Developing other forms of cancer
But certain other things were similar. So infection rates were similar, rates of more significant bleeding were similar, rates of developing other forms of cancer, which can happen in any patient with CLL were also similar between acalabrutinib and ibrutinib, so that’s why I kind of emphasized, even though there are some differences in general, these these drugs are quite similar.
Michele Nadeem-Baker: Wonderful. And zanubrutinib because we’re starting we’re going to need to jump to our next section after this. But zanubrutinib is, as you know, we have a couple of panelists that have been on it or are on it.
You had mentioned, Dr. Davids, about joint pains and all with ibrutinib. Leesa was on ibrutinib. Leesa, would you like to explain to Dr. Davids with ibrutinib and then your switch to ibrutinib as it pertained to you?
I am able to go out. It’s nerve wracking. It messes with your mind because you’re constantly worried, because there really isn’t much of a warning.
Leesa P., CLL Patient
I just don’t know how my body is doing any particular time. And yes, it’s a life-altering side effect.
Leesa P., CLL Patient on Ibrutinib, Switched to Zanubrutinib
Summary of side effects:
- Ibrutinib: Joint pain
- Zanubrutinib: GI problems
Leesa P.: Thanks, Michele. I was on ibrutinib for a little over three years, and that entire time I had horrific joint pain. There were several times to the point that I could not even walk, and it was constant.
The things that did help me were prednisone, although I had to take it in extreme moderation, because that created a whole nother problem for me. And hot water. If it was my hands, I could soak my hand in hot water with Epsom salts. So that was my only relief. But the joint pain was there the entire time.
Once I switched to zanubrutinib, in two days, all the joint pain went away. I’m like, Miracle Drug, this is wonderful. Everything was going very smoothly for about five months. Then I started experiencing GI issues to the extreme that were difficult to control.
Maybe part of that was my fault for not taking enough Pepto or then switching to Imodium and really stepping up how much I would take of that. So I have been taking two Imodium a day to control the GI issues and I’m still in the early stages of trying to get that under control, but I think I’m doing a lot better so far.
Michele Nadeem-Baker: Leesa, is it keeping you home more?
Leesa P.: I am able to go out. It’s nerve wracking. It messes with your mind because you’re constantly worried, because there really isn’t much of a warning.
I just don’t know how my body is doing any particular time. And yes, it’s a life-altering side effect.
…it might be okay to take a break for a period of time and see if things get better. That can actually be helpful in terms of understanding how much the drug is contributing…
Dr. Matthew Davids
Gastrointestinal side effects
Michele Nadeem-Baker: Thank you so much for being brave to share that side effect. Dr. Davids, are you seeing much of that with patients on zanubrutinib or other BTKi’s?
Dr. Matthew Davids: Not commonly, but I definitely have seen it. I mean, these drugs definitely can irritate the GI tract in various ways. It is a little strange that it kind of popped up after several months of being on it, so hopefully you’re having an evaluation to look for other causes. But even if there is another stimulus that caused this to start, zanubrutinib could be contributing.
Possible solutions
The other thing that I encourage patients to think about, if these side effects are really challenging, is especially if they’ve been on treatment already for a few years, that it might be okay to take a break for a period of time and see if things get better. That can actually be helpful in terms of understanding how much the drug is contributing, because if you stop the drug and a month later, you’re still having the same symptoms, it suggests it’s probably not the drug.
Whereas if you stop it and two days later, everything gets better, it gives you your answer there, too. Although these drugs were developed as continuous treatments, as long as you’re in remission and you’ve been on them for a while, you can take some breaks and that can be okay.
Jane D., CLL Patient on Zanubrutinib
Michele Nadeem-Baker: Jane, who was also on ibrutinib, could you share? I know that right now you’re on a break from treatment and that goes along with what Dr. Davids was just saying. Could you let us know about how you were doing on ibrutinib?
Summary of side effects:
- Mucositis (mouth sores)
- High white blood count
- Atrial fibrillation (A-fib)
Jane D.: I started on zanubrutinib last July. I went in for my two week check to my CLL specialist and I had a mask on and he said, let me see you in your mouth. He took a look and he said, oh, you have mucositis. And that’s an inflammation of the mucous membranes of the body. I wouldn’t have even mentioned it to him because I had had copious amounts of dental work done. That’s been one of my CLL issues.
He said, no, we don’t want you to suffer at all. So he decreased the dose for a month. So I went down to 80 milligrams twice a day and it got better. But he kept me at the lower dose then for the rest of the time I was on it, which wasn’t that long.
My white count did go through the roof as was described, and I was so glad I was prepared for that. Then on February 1st, I went for a routine physical and my doctor called me that night. He said, Jane, you’re in AFib, and you need to call your doctor immediately. I did. I started on something called Eliquis that probably everybody has seen for blood clots.
Then I began what feels like, even though it hasn’t been, an endless, few months of trying to get this thing under control.It is unclear to both my electrophysiologist, who is a cardiologist who deals with heart rhythms, if I had afib prior or not, I don’t know. But I was never very aware of it, as I have been since February 1st.
I’m on three medications and I had a cardiac ablation on May 2nd at Weill Cornell, where I go. I’m still improving. I had a loop put in my chest that gives my electrophysiologist daily feedback as to what my EKGs are doing.
I’m coming along and I plan to go back to the drawing board this week with my CLL specialist and figure out because I’m already feeling the symptoms return from the CLL. So that’s it. Dr. Davids, have you seen a lot of patients with Afib in your practice?
Atrial fibrillation (A-fib)
Dr. Matthew Davids: I certainly have. That is one that we think is less common with zanubrutinib compared to ibrutinib based on the head to head study. But that being said, even in the head to head study, about 4 to 5% of the patients on zanubrutinib developed new atrial fibrillation.
So all of these drugs have that risk associated with them. I’m sure we’ll also talk about some other classes of drugs now available in CLL that don’t carry that risk and can be great alternatives to consider when you need treatment for CLL.
Jane D.: Do you find the majority of your patients respond to Afib treatment and then are they able to go back on the BTK inhibitors or do you avoid them?
Possible solutions
Dr. Matthew Davids: It really depends on a case by case basis. If the atrial fibrillation is well controlled, you don’t necessarily need to be out of it as long as you’re on the blood thinning medicine and the rate is relatively slow.
I think the challenge there is that when you’re then on a blood thinning medicine like Eliquis and you’re on a BTK inhibitor, your risk of bleeding definitely goes up quite a bit. That’s where thinking about switching to a different CLL therapy, I think is a good idea.
Jane D.: Okay, thank you.
BCL2 Inhibitors (Venetoclax or Venclexta)
Michele Nadeem-Baker: Thank you, Jane, for sharing that. Dr. Davids, that brings us to the other types of treatments that we have, such as BCL2 inhibitors and venetoclax. Can you tell us a bit about about venetoclax? And would that be one that you’re talking about that could be an option potentially?
Dr. Matthew Davids: You read my mind, Michele. That’s exactly what I was thinking of, was Venetoclax. This is a drug that has really become the backbone of a lot of different combination regimens that we’re developing now in CLL.
It was actually originally developed as a single drug like the BTK inhibitor drugs. We actually treated some of the first patients in the US with venetoclax back in 2011 at Dana-Farber.
What we learned very early on with the development of the drug is that it’s so potent at killing CLL cells that we actually have to start it at a very low dose and gradually ramp up week by week over five weeks.
Key side effect concern: Tumor lysis syndrome (TLS)
Patients need to be monitored very closely for something called tumor lysis syndrome, which is where the CLL cells can burst open and release toxins into the blood. That was a bit of a learning experience early on with that drug. But we’ve got it down now and we know how to safely administer it.
No known side effects of:
- Cardiovascular risks
- Bleeding
Some known side effects of:
- Gastrointestinal issues: diarrhea, nausea
- Lower neutrophil count (into neutropenia)
The nice thing about venetoclax is that it has no cardiovascular risks that we know of. It has no bleeding risks. It does still have some risks of gastrointestinal side effects like diarrhea or nausea. It can lower the neutrophil count, you heard earlier about neutropenia, so we need to monitor for that. But most patients tolerate venetoclax very well.
Because it’s so powerful, it’s actually being developed in regimens that are time limited. So giving it for one year or two years, maybe with an antibody drug like rituximab or obinutuzumab, and then stopping treatment.
Many patients now have been in remission from their CLL for several years after receiving just one or two years of venetoclax so it’s a great drug. It’s been very helpful. It’s now being combined with the BTK inhibitors, like in Brad’s case, the AVO experience. That’s also very exciting.
Monitoring for tumor lysis syndrome (TLS)
Michele Nadeem-Baker: Brad, you and I were talking about the venetoclax portion of your trial and the fear of tumor lysis syndrome with venetoclax. Can you tell us what your fears may have been and how those were mitigated?
Brad A.: Sure. As Dr. Davids said, there is this concern about TLS when you start venetoclax and the way that they monitor you, and Dr. Davids can speak to this more, is based on your profile, the size of your lymph nodes, your white cell count and so forth.
In my case, I had a high white cell count and my lymph nodes were large. So my doctor at MD Anderson put me in the hospital for the first couple of days of Week One. Remember, Dr. Davids says this is a five-week ramp up. I was in the hospital for a couple of days, Week One for venetoclax, so that they could keep me on IV fluids.
They could check my blood every 4 hours and keep me hydrated. And if TLS started, then they could respond. They also did that for Week Two. The dose doubles when you start Week Two. So there (were) a couple of nights, a couple of days that I was in the hospital at MD Anderson to be monitored, as well.
I had tolerated Weeks One and Two well, although my potassium spiked a couple of times, but nothing serious. I never went into TLS, but by Week Three then I just had IV fluids for a few hours on that first day that I started the third dose and didn’t have to be in the hospital.
Then by Weeks Four and Five, I wasn’t in the hospital or even IV fluids at all. So it’s definitely something that you have to consider. Again, it’s based on your unique profile of your CLL in terms of lymph nodes and white cells and your spleen and so forth, as to how closely they have to monitor you during this ramp up.
Michele Nadeem-Baker: We’ll be talking to Brad more when we get to our section on AVO and in some of the trials that are out there. Dr. Davids, we have a question from the audience asking, ‘Will the muscle aches and pains that are caused by venetoclax go away once treatment is over?’
Question: Will muscle aches/mains caused by venetoclax go away when treatment ends?
Dr. Matthew Davids: Yeah, muscle aches and pains are less common with venetoclax than they are with the BTK inhibitors, although I have seen it. If it really is being driven by the venetoclax, it should stop very soon after the drug is stopped.
That’s, again, an advantage of a time limited therapy, is that if you’re having a nagging side effect like that, at least if you know that you’re only on the drug for a year, you sort of have a finish line in sight and just kind of get through that year and be done with it.
I think that is a challenge psychologically with the BTK inhibitors, since they have been developed as continuous treatments. There’s no sort of endpoint, really. If you’re having side effects, you don’t want to live with them forever. You want to be proactive and try to switch around the dose or switch to a different drug. You have to be a little bit more proactive about managing.
Michele Nadeem-Baker: Thank you. So it seems that there are various mitigation strategies for a lot of these different side effects that people are having and that most of them are not forever.
Dr. Matthew Davids: Generally, that’s right. Yes.
CD20 antibodies (rituximab, obinutuzumab)
Michele Nadeem-Baker: That’s great. We spent a lot of time now on BTK inhibitors and BCL2’s. So on CD20 antibodies, Dr. Davids, can you summarize really quickly when they would be used and the benefits of using them? Examples of these would be rituximab and obinutuzumab,
Dr. Matthew Davids: Those are the two right now that are approved in CLL that we’re using. Rituximab has been around for 25 years at this point and it was a mainstay of combination treatments like FCR with chemo. We obviously have a lot of experience with it.
Obinutuzumab came around in around 2013, when it was approved in CLL and right from the start, we had a sense that it was a little bit more potent than rituximab.
Rituximab vs. obinutuzumab
Dr. Matthew Davids: We’ve now seen across a couple of different studies, head to head comparisons where patients got either a drug with rituximab or the same drug with obinutuzumab. Those patients tended to do better when they got obinituzumab and in some cases even live longer, what we call an overall survival benefit. So we do think in most cases, if you’re going to use the CD20 antibody, obinutuzumab is probably the better one to use.
One of the challenges is that some of the big clinical trials have been done with rituximab, especially for patients who have had prior treatments. So if your doctor has offered you rituximab, for example with venetoclax, there’s nothing wrong with that, that’s the standard of care. But I think as we kind of move toward the future, we’ll have more and more combination approaches with obinutuzumab, since it does seem to be a more potent antibody.
CD20 antibody + BTK inhibitor update (June 2022)
I’ll add also that until this point, we haven’t had really convincing evidence that adding a CD20 antibody to a BTK inhibitor is helpful. Although I will say at this meeting I was just at last week in Europe, there was an update of a study comparing acalabrutinib with obinutuzumab to acalabrutinib alone for previously untreated patients. The patients treated with the two drugs, the combination, have been in remission for significantly longer.
It’s edging ever so close to an overall survival benefit also that they may be actually living longer. So it’s getting a little hard to ignore the data from that study. We think in the future we may consider adding obinutuzumab to acalabrutinib at least in untreated patients.
Doublets (2-targeted drug regimens)
Michele Nadeem-Baker: That’s really great information and great to hear that there was news happening at EHA (European Hematology Association).
We’re going to go forward to doublets, which I’m sure patients hear about. What are doublets and can you give us some examples of some of them?
Dr. Matthew Davids: Yes. I would consider doublets to be combinations of two of the different targeted drugs. So it could be venetoclax with the CD20 antibody like we were just talking about, or it could be venetoclax with a BTK inhibitor.
Venetoclax + ibrutinib – expected approval soon
That’s one to be aware of, especially if you’re a patient who’s not yet on treatment, because we’re going to have a new regimen coming along very soon, which is ibrutinib plus venetoclax.
We anticipate that the FDA is likely to approve that combination by the end of this year, and that will be another option, and it’s time limited, like the venetoclax obinutuzumab that I was mentioning before.
But what’s nice about it is that it’s all oral, it’s two pills, and you take them together for about a year of combination, plus another three months of the BTK inhibitor, and then you stop. We think that that’s going to have a very durable response.
MAJIC clinical trial (venetoclax + acalabrutinib)
Then the other exciting development is additional data that’s accumulating with acalabrutinib with venetoclax. We’re going to be opening a global study very soon that we call MAJIC that’s comparing acalabrutinib with venetoclax as a doublet to venetoclax with obinutuzumab as a doublet. So sort of what’s the best doublet for that first therapy for CLL.
Michele Nadeem-Baker: Absolutely. So if someone is already on something like acalabrutinib, can they then add in obinutuzumab and get on one of the future trials like venetoclax and obinutuzumab?
Dr. Matthew Davids: Yes.. There’s various clinical trials out there. For example, there’s trials that accept patients who are on BTK inhibitors and then add a second drug to it to try to, what we call, deepen the response.
For example, we haven’t talked yet about MRD, minimal residual disease, but that’s basically a way to look for even tiny molecular evidence of CLL in the blood and the bone marrow. We find that if patients can get into an MRD undetectable state, it allows them to actually stop therapy and hopefully have remission for a period of time.
So a lot of these add on studies take patients already on BTK inhibitors, add the second drug, and if they get to undetectable MRD, they can stop both drugs and then be observed.
I’m aware of an ongoing study at MD Anderson that’s looked at adding venetoclax to the BTK inhibitor. We have a study of Dana-Farber adding in copanlisib, which is a kind of similar drug.That could be an option to consider. There’s a lot of interest in that approach.
Triplets
AVO Clinical Trial
Michele Nadeem-Baker: Now we’re going to talk about triplets. Brad (is on) the AVO trial as said before. That’s three different drugs. It’s acalabrutinib, which we’ve talked about, venetoclax, which we’ve talked about, and obinutuzumab, which we just spoke of. Brad, how did you decide to go on this? Did you have other choices or were you looking for a trial?
Brad A., CLL Patient in AVO Clinical Trial
Deciding whether to join a clinical trial
Brad A.: The answer is I was not looking for a trial at the time when my doctor, Dr. William Wierda at MD Anderson, sat down with me and we started talking about the need to start treatment and what Dr. Davids and we’ve talked about this during this webinar, the fact that we’ve made such tremendous advances in the treatment of CLL over the past decade.
When I sat down with Dr. Wierda and we had that conversation, I was a beneficiary of that because he gave me three options. He gave me a BTKi option, he gave me a BCL2 option, and then he gave me the trial option.
The trial option, he certainly felt like that was the right option for me, but it was also appealing in the sense that acalabrutinib, obinutuzumab, venetoclax are all FDA approved, so it’s not like we’re in the Wild West here on the frontier experimenting with new drugs. These were proven drugs that were being combined to get deeper remissions.
In the end, it was easy for me to agree to go the AVO trial route. But again, I want to emphasize to the audience that it’s a tremendous time – well, if you can say tremendous time to be in treatment – but to have options, to actually have options for treatment.
Michele Nadeem-Baker: Dr. Davids, regarding what Brad is on and the AVO trial, what is, I don’t know if it’s too early to show this, but when Brad gets off this trial, (and) he’s already uMRD, what is the average length of remission that’s being seen so far (after the trial)?
Dr. Matthew Davids: I believe Brad’s on a trial for patients who’ve had prior treatments, which was a study that was started a little bit later. We actually started the first study of the AVO triplet, which is for patients who’ve never had any prior treatment. We started our study back in 2018 and we have reported we recently published the results for the initial 37 patients on the study.
For those patients we saw that 86% of the patients got to this uMRD state, undetectable MRD in the bone marrow, which was pretty amazing to us. I mean, that’s even similar to what we saw with the iFCR regimen, which needed chemotherapy. So without the need for chemotherapy, we were able to achieve similar rates of uMRD.
We’ve been following the patients on the study at the time of the report for a little over two years. At that point in 37 patients, not a single patient had progression of the CLL despite the fact that most of them were already off treatment for a while. So obviously, the follow up is short, as we would say, because obviously we want to do much better than 2 to 3 years, but so far certainly looks very, very good in this in this population.
Michele Nadeem-Baker: So the trial that Brad’s on then obviously it’s too early because I don’t know if there are other cohorts that had finished prior to Brad, what would be being seen.
Dr. Matthew Davids: Yeah, our cohort is a is the first one. We added a second cohort to the study actually that’s specifically for patients who have what we call high risk CLL with TP53 mutation or deletion 17p, and we’re continuing to actually put patients on that portion of the study. So if there’s any patients out there who unfortunately have higher risk CLL and have not been treated, definitely consider the study.
Michele Nadeem-Baker: This is all exciting for patients out there. And what we’ve been talking about, we haven’t even talked about every type of treatment out there that it just shows that thankfully there are more and more choices and more research being done by combining different drugs, which is just very hopeful for all of us. So we have some other questions from our audience.
But first of all, Brad, I wanted to ask you if you had any particular questions for Dr. Davids before we leave the section.
Muscle/joint stiffness
Brad A.: I’d probably say the one question I might have is I’m having some muscle and joint, I might call it stiffness, Dr. Davids rather than pain. I assume that’s a cumulative effect of being on acalabrutinib and venetoclax now for about almost 18 months. I’m assuming that those side effects will diminish fairly quickly when I finish at the end of August. Can you comment on that?
Dr. Matthew Davids: Yeah, I think that’s very likely, particularly with the acalabrutinib, we can see those types of aches, so I’m hopeful that they’ll get better very quickly once you stop.
Brad A.: Michele, I might go off topic for just one second to go back to just how fabulous these drugs are and point out that I’m in a two year trial. I finished it in August. I’ve been in remission, MRD negative since September of last year. But that gives you a sense of how powerful these combinations can be.
Dr. Matthew Davids: It’s great.
CAR T-cell therapy
Michele Nadeem-Baker: Exciting. And Dr. Davids, could you share with us a bit about on CAR T? A lot of people ask about it. A lot of people think it’s curative, which I I’ve learned it is not. What are the major side effects about CAR T that maybe patients should think about first? And when is it used?
Dr. Matthew Davids: Just for anyone out there who doesn’t know what CAR T is so chimeric antigen receptor T cells. This is a way to actually use your T cells from your own blood to get them sent off to a lab where they can be engineered to recognize CLL cells and then re-infused back into yourself.
The originator of this calls them the serial killers of cells because they can go around killing CLL cells potentially for years at a time.
There was a week a few months ago where every patient who came in was asking me about this report that was published in Nature. I think a couple of patients treated originally at UPenn were still in remission ten years later and still had evidence of the CAR T cells.
If that’s not a cure, I don’t know what is. I actually do think these have curative potential for patients with CLL. So you may be wondering, well, why don’t we just give everyone CAR T cells then?
CAR T-cell therapy major side effects
- Cytokine release syndrome (CRS)
- Neurologic side effects
- Mild: Headaches
- Serious: Confusion, difficulty finding words
- Severe: Coma (rare)
Dr. Matthew Davids: The reason is because of some of the risks and side effects with the current versions of CAR T that we have. There are two broad categories. One is something called cytokine release syndrome or CRS. This is an effect that can happen within a few days of receiving the cells back. It can be quite scary because your body reacts in a way as if it’s having a major infection.
You may have heard of sepsis, for example, where the blood pressure can drop and you can get very high fevers You might need to go to the intensive care unit in the hospital. There’s things you can do, but it can be unsettling, obviously, to go through that.
Secondly, there can actually be some neurologic side effects. Neurologic side effects can range from headaches to more serious things like confusion or even difficulty finding words, and rarely, rarely even more severe things like coma. These are obviously very serious things, and not something that you would want to have if you could go on acalabrutinib or ibrutinib or venetoclax or any these other drugs which are so well-tolerated.
We are reserving CAR T cells for patients who have been through all these other treatments and don’t have other great options.
Dr. Matthew Davids
Not yet FDA-approved for CLL
Right now CAR T cells, although they’re approved in other very aggressive types of lymphoma, they’re not approved yet in CLL. I think for a large part because we have so many effective and very safe therapies for patients with CLL. We are reserving CAR T cells for patients who have been through all these other treatments and don’t have other great options.
The risk of the T-cells is worth taking. But I’m hopeful as we continue to develop CAR T cells further that we’ll actually be able to develop safer products that have less likely risks like this. I think if we can make them safer and better tolerated, we could actually really extend the CAR T technology to a larger group of CLL patients and extend that curative potential.
But we’re not quite there yet. It’s been a challenging thing to do that, and a lot of people are working really hard to do that right now.
Support for CLL/SLL side effects
If you’re in a smaller practice, it’s helpful if your oncologist has a relationship, even if it’s with a general cardiologist or a general dermatologist, to be able to get access to them fairly quickly and have that dialogue and communication.
Dr. Matthew Davids
When to seek out specialists
Michele Nadeem-Baker: Thank you. We’ve all been talking about different side effects that happen whether due to CLL, due to treatment, and different things. With patients we do realize that our oncologists, our CLL specialists are fantastic, but that is your specialty.
Do you suggest when someone when patients like in Jane’s case with AFib that they should be seeking out specialists for the particular side effects that they have.
Dr. Matthew Davids: I think that’s to some degree kind of side effect specific. But I think Jane’s example is a great one where getting a cardiologist involved early, I think is very helpful. Some of the larger centers like here, and I’m sure Cornell, as well, there’s particular cardiologists who have certain expertise in some of the complications from cancer therapies, so-called cardio-oncologists.
I think we’re starting to see that more and more at bigger centers for other diseases, as well, like kidney disease. We have some onco-nephrologists and we have gastroenterologists now who are interested in oncology. So if you’re at a big center, I think it’s great to have that, but I don’t think that’s completely necessary either.
If you’re in a smaller practice, it’s helpful if your oncologist has a relationship, even if it’s with a general cardiologist or a general dermatologist, to be able to get access to them fairly quickly and have that dialogue and communication.
Sometimes these subspecialists, especially if they’re not onco-cardiologists, they may not know a lot about BTK inhibitors because that’s not part of their practice, but if you have good communication between the oncologist and the cardiologist, I think that’s really key to optimize the management of the side effects.
Final word: Where do our patients seek support through side effects?
Michele Nadeem-Baker: I’m going to turn it back to the patients. I’m going to ask each of you to answer if you’re having something happen or you’re trying to figure out what’s going on with the side effect, what you do, what your advice would be to other patients, and how to first try to talk it through or find some help. Hannah, how do you do that?
Hannah D.: I try to keep a good open line of communication. I have a local oncologist and then I also travel three states away to see a specialist. And they work very well together. They keep communication. I keep communication with them, as well.
The other thing I do is I belong to a fantastic support group that’s online, which is how I met you. What I find in that is that there are so many common side effects and everybody has these ways that they’ve learned to deal with them, And having that kind of support is so helpful. I’ve gotten fantastic ideas that I’ve tried and that have worked.
I’ve gotten comfort from others who have had the same side effects. It’s comforting to know that other people, that’s pretty normal. You don’t want to call your oncologist every time your nail hurts. But when you have a group of people who’ve been through it, it’s just a fantastic type of support that I think everyone should have.
Michele Nadeem-Baker: I find that’s both online, as well as the virtual meetings, thanks to technology that we all have. Thank you, Hannah. Lynn, how about you when you’ve had some of these things?
Lynn B.: The comment came up about atrial fibrillation and certainly, that’s a side effect that may or may not be apparent to the patient. If we thought we had something going on, we probably would be contacting a doctor or going to emergency room or something like that. But I will agree with what Hannah has said, that there is a lot of support among groups, Facebook groups, and Patient Power, and CLL Society and so forth.
When you’re dealing with these side effects, to me, the best thing to do is just get an email off to the to the nurse and get some feedback from the doctor because sometimes the opinions we get from other patients may be valid or may not be. It may vary from patient to patient what might be causing this? Sometimes I wonder, is this just old age or is this the aging process that’s causing some of the side effects? But I do say that a pill a day keeps the cancer away. So I’m happy with what I’ve got.
Michele Nadeem-Baker: Lynn, in my case, two pills a day keep the cancer away on acalabrutinib. But that’s a great point, you want to make sure that your sources are credible. That’s why, for instance, on this program here with The Patient Story, we have Dr. Davids, so that we can find out the ways to go about it. It is great to have the support from other patients, but to know who the patients out there, I guess also who are credible and base things on medical advice or those who perhaps are finding it in other ways.
In thinking of ourselves as dealing with doctors and helping patients become more better at self advocating, Brad, what do you suggest for patients? What you have found to be really, really helpful so that you’re great because you are a great self advocate and you help others in advocating. What are great sources for you to share with them?
Brad A.: The Leukemia and Lymphoma Society is a great resource and also Facebook groups. There’s a very active Facebook group that Michele, you’re the administrator of that I’m often on and try to help people.
Michele Nadeem-Baker: Leesa, when you were looking for help, I know that you were great in asking our support group and sharing it with us, but was that your doctor, your primary care doctor, or your oncologist that you sought help from?
Leesa P.: My oncologist is who I normally go to and we have a portal and I can email him directly and he’s really amazing at getting back to me the same day and within two hours, almost all of the time. So he’s my main source, of course.
I always look at the information on support groups and just the little things, like soaking in hot water and Epsom salts or things like that or, you know, it’s not harmful and it couldn’t hurt.
Michele Nadeem-Baker: Thank you. And Jane, do you have any words that can give people a great outlook moving forward for CLL patients?
Dr. Matthew Davids: I think we have a new resource, The Patient Story that can be helpful as all the other resources we all use. I’ve met some great new friends in CLL. That’s been a bright spot and I’m very lucky that I have…
There’s just no worry. If you’re worried, feel free to contact your doctor. I can email my doctor directly and he gets right back to me. I’m very fortunate for that. I’ve kept him abreast of every single thing going on with the cardiologist and you know, that’s the way to go. I think some of us are just very stoic and it’s okay to get some help sometimes.
Michele Nadeem-Baker: Any last words for our patients watching and those who are here on our panel. about CLL and the future of treatment?
Dr. Matthew Davids: We’re again, sort of in a very exciting time right now for patients with CLL. We’ve had so much progress in the last decade, but there’s so many other exciting things going on right now.
I mean, one other thing we didn’t get to was the development of a whole new generation of BTK inhibitor drugs called non covalent BTK inhibitors. So, for example, one called pirtobrutinib, which seems to be working very well even for patients with CLL whose progressed on the earlier drugs like acalabrutinib and zanubrutinib and ibrutinib.
So the longer you live, the longer you’ll live, because we continue to have more and more treatments for patients.
Michele Nadeem-Baker: It’s just all so hopeful and helpful. Thank you for being with us to all of our patients here on our panel. Dr. Davids, thank you so much. And for all of you who have joined us. I am Michele Nadeem-Baker for The Patient Story. Please stay tuned for the survey at the end. Take care and have a great day.
Thanks to our supporters for our informational program for patients and care partners! The Patient Story retains full editorial control of all content.

CLL Patient Stories
Symptoms of CLL
Learn about how some of the common CLL symptoms first present themselves from patients who have been diagnosed with CLL.
Susan K., Chronic Lymphocytic Leukemia
Symptoms: Swollen lymph nodes on the neck, high white blood count
Treatments: Venetoclax & obinutuzumab
Hannah D., Chronic Lymphocytic Leukemia
Symptoms: Fatigue, high WBC
Treatments: Imbruvica, venetoclax