Seeing Beyond the Fear: Steven’s Fight Against Rare Eye (Lacrimal Gland) Cancer
When a small dark spot appeared in Steven’s vision in June 2024, it seemed like a minor eye issue. He saw an ophthalmologist, and went through the normal process to uncover what was going on in his eye. What he didn’t know was that the source lay in one of the smallest yet most vital structures of the eye—the lacrimal gland, responsible for producing tears. Further testing revealed something far more serious: a rare cancer called adenoid cystic carcinoma, originating from that tiny gland tucked above the outer corner of his eye.
Interviewed by: Nikki Murphy
Edited by: Chris Sanchez
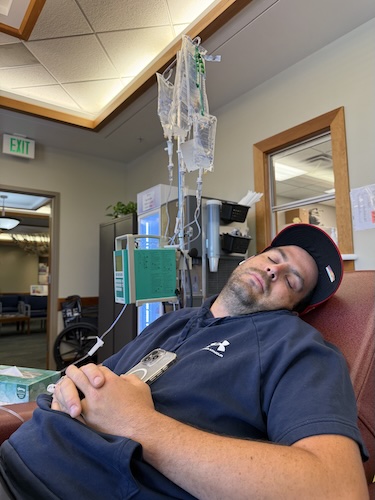
Steven’s lacrimal gland cancer diagnosis unfolded gradually and culminated in surgery that revealed cancer rather than the expected benign cyst. While his initial shock was compounded by the rare and poorly documented nature of adenoid cystic carcinoma, Steven credits his support team, including his wife, children, and a neighbor oncologist, for helping him make sense of his treatment options. After consultations at MD Anderson and Mayo Clinic, he began an intensive six-week regimen of radiation and chemotherapy, chosen specifically for the cancer’s tendency to spread along nerves and resist standard treatments.

Throughout his treatment, Steven remained firmly committed to family life and self-advocacy. He emphasizes how critical his support team was in managing daily realities like side effects, exhaustion, and the ongoing fear associated with “scanxiety.” His story is marked by personal and professional transformation. When he completed treatment, he was relieved and proud and celebrated by ringing the clinic gong.
Steven now looks ahead to regular monitoring and a new chapter in oncology nursing, hoping his personal insight into adenoid cystic carcinoma will empower him to advocate more authentically for future patients. Ultimately, his lacrimal gland cancer experience highlights the power of hope, the importance of purposeful action, and the value of forming strong support networks.
Watch Steven’s video and read through the transcript of his interview further down to delve into:
- How early self-advocacy can make a critical difference in rare cancer diagnosis and treatment
- The importance of a strong support system in coping with both treatment and uncertainty
- Steven’s transformation from patient to future oncology nurse, inspired by his own experience with lacrimal gland cancer
- The distinct challenges of parenting during treatment, and how maintaining involvement and honesty with children fosters connection and healing
- How being proactive and insisting on a thorough investigation led to timely and effective treatment for Steven
- Name: Steven S.
- Diagnosis:
- Lacrimal Gland Cancer (Adenoid Cystic Carcinoma of the Lacrimal Gland)
- Age at Diagnosis:
- 36
- Symptoms:
- Appearance of black spot in vision
- Drooping of affected eye
- Treatments:
- Surgery: tumor excision
- Chemotherapy
- Radiation therapy
This interview has been edited for clarity and length. This is not medical advice. Please consult with your healthcare provider to make informed treatment decisions.
The views and opinions expressed in this interview do not necessarily reflect those of The Patient Story.
My name is Steven
I was diagnosed this past June 2025 with adenoid cystic carcinoma, coming from the lacrimal gland in the orbit of my eye.
When I first noticed something was wrong
It was June of 2024 when I started to notice a black spot in my peripheral vision. It was kind of like if you press on your eye, you can see a black spot on the opposite side. I thought, “That’s weird,” so I called an ophthalmologist.
I had never seen one before, so I just googled and found the closest one and went, and they ran tests in the office. They just said, “We don’t see anything.” I had actually, I don’t know, 10 or 12 years before, had had a tear duct surgery for a clogged tear duct, so they had to unclog that. I thought it was related to that.
I thought, “There’s got to be something in my eye,” because it wasn’t like black spots or floaters or anything like that. So I thought, “There’s got to be something in my eye,” and I just ignored it for the next year. The doctor just said, “We don’t see anything.” They told me that if it kept coming back, they would send me to a retinal specialist, but I just ignored it for the next year.
Then I had just graduated from nursing school. When I was in nursing school, they did this thing called your capstone, where you do ten shifts with the same nurse. I was in the operating room, and I sent a selfie to my wife. I noticed that my eye was lower, which scared me.
After I graduated, I put my symptoms into ChatGPT, and it said I should go in. So that day, it was a Sunday, I just went into the ER, and they did a CT scan and an MRI, and they found the tumor. They originally told me it would be just a benign cyst, and they referred me to an oculoplastic surgeon. He told me the same thing: “Yeah, it’s probably just a cyst.” But looking at the original MRI results, it actually said they couldn’t rule out ACC, but it’s less than 1% of cases that have that.
The day of surgery
When I had surgery, I was just expecting it to be simple. All the doctors said it was no big deal. My doctor said, “I’ve done this surgery hundreds of times. It’s usually a cyst filled with, like, hair and bone and stuff, and it’s really nasty.” He even told me he would give me a picture. So when I went in for surgery, I thought, “Yeah, this is no big deal, and I’ll be fine.”
But then I woke up, and the nurse practitioner who assisted in the surgery said, “We did find cancer. We’ll let you know more later.” They sent it for biopsy. That day, that was really all I knew. I didn’t know anything. I didn’t know what kind of cancer it was. I didn’t know anything.
In the days following, I read the surgical notes that are on the app, where I have access to all my medical records. They said it was invading bone, but they didn’t say what kind of cancer. I guess they couldn’t really until it came back from the biopsy, but until the doctor called me with those results, it was just a guessing game. I didn’t know anything about it.
The moment everything changed
When I first heard the diagnosis, I had never heard of this type of cancer, which is a very rare form of cancer. I’d never heard of it. I did as much research as I could. I’ve done a lot more since then, but that day I researched it and mostly found out that the most important thing for different survival rates is the growth pattern of the tumor. There are three different types. I found out later that mine is the middle one, which is the most common. There’s solid, which is the most invasive. Then there’s cribriform, which is what mine is, and then there’s tubular, which is the least invasive and has the best prognosis. But mine is the middle one.
Once I found out those results, after researching it, you scare yourself. You really do. They tell you there’s not much data on it, and you see all the life expectancies, and you just don’t know what to think. I didn’t know what to think, really.
Sharing with my wife, she has taken it harder than anyone, which I expected. She was at work, and I had to call her with the results. I didn’t want to wait, and she wouldn’t have wanted me to wait, so I just told her over the phone. She said, “I’m not looking up anything until I get home.”
Since then, we told our kids, they don’t really understand, so we just told them, “Dad has cancer,” and that’s about the extent of it. They’ve seen me do the treatments. My wife has shared videos that she’s taken and pictures of radiation and chemo and stuff like that.
Why I wanted to get multiple opinions
When I first found out, I actually had a neighbor who’s a medical oncologist, and I called him. He said, “I’ll look into this for you.”
My eye doctor, the surgeon who did the surgery, when he gave me the results, said, “I’m setting you up with radiation oncology and to get a PET scan done to see if it’s spread anywhere else.” My oncologist neighbor said there wasn’t much he could do because he works with chemo, and chemo doesn’t usually work with this kind of cancer. He said I would want to see a radiation oncologist, which I had already set up.
I saw the radiation oncologist first, and they said it would be 30 treatments, five days a week. They put this mask over your face so you’re in the same position every time, and they’re really accurate with where the radiation goes. Then my neighbor called me back and said he had talked to some colleagues at places like MD Anderson and the Mayo Clinic, and they said there is a type of chemo that you can try that has been shown to help in conjunction with radiation. So I opted to do that as well with him.
I also joined a Facebook page of people who have the same type of cancer. It was pretty straightforward. Everyone does the same kind of treatment. Surgery is the best first thing you do, and then radiation. It’s hard for them in surgery to get it all because it follows nerves. It’s in the lacrimal gland, the tear gland, and that’s right by your optic nerve and everything. So you have to do radiation to try to kill the rest. From there, we just have to do scans to see how successful it was.
How I handled treatment
With treatment, they say that kind of chemo I was on is one of the worst as far as nausea goes. I had nausea, but I never had any vomiting or anything like that. It was more like I’d feel it in my stomach, then I’d eat something, and the next day I’d think, “I can never eat that again.”
With radiation, there was severe exhaustion. I put Aquaphor around my eye because it started to get really red. They said you can have skin breakdown if you’re not on top of that. This chemo doesn’t really cause hair loss, but with the radiation, my eyebrows started falling out, and I had these weird patches of hair loss from the radiation as well. Other than that, I was able to stay pretty active, which for me is important.
I continued to work through most of the treatment. I took about two weeks off at the end because it got hard with how tired I was from the radiation and everything.
My wife was the real hero there because she also works, and she really took care of basically everything. The kids were just starting school, which, after they started school, was nice for me because they were gone and I could rest or whatever. Still, I wanted to be a part of their lives. I didn’t want to just check out, so I’d still do as much as I could.
Even doctors told me, “You can ignore that exhaustion as much as you want. You can do as much as you want as far as being active or being with your kids.” So we would still take them to the park or to the pool and all that stuff, just trying to keep it as normal as possible. But it was hard because I had all my appointments, and then my kids have appointments too, and balancing all of that is pretty tough. Our daughter with Down syndrome has a bunch of appointments. This year, she got diagnosed with sleep apnea, so we’ve had to see a cardiologist for her and then the sleep doctor as well. Balancing everything is pretty tough.
What the plan looks like moving forward
I finished treatment at the beginning of September. It felt good to be done. They have this big gong that you ring when you’re finished, and they let me keep my radiation mask.
It was just nice not to have to go in there every day and not feel that same level of exhaustion, even though that exhaustion is part of it, and treatment is important. Knowing that I’m done and that I can keep going with my life and everything I like to do feels really good. I can’t think of many words to describe it besides saying I was just glad to be done with it.
They said to wait about three months for the inflammation to go down, and then I’ll have scans. I’ll have another MRI and everything in November, at the end of November. With this kind of cancer, the tumors are slow-growing, but it’s very persistent, which is what they told me. So every three months, I’ll have scans for at least a year. After that, they go every six months or whatever the plan ends up being. If they find tumors elsewhere, hopefully they can surgically remove them. It’s very common for it to spread to the lungs, or it can spread to the liver and a bunch of different places, so they have to monitor everything really closely. Catching it early is the most important thing.
Everyone says there’s “scan fear,” and for sure that’s real. You want to see that they don’t see any signs, especially locally, but also that it hasn’t spread. They say keeping the cancer local is the most important thing. But if it’s still there, then treatment options are kind of limited. Some people have their whole eye removed or different things like that. There’s not much else they can do for that, unfortunately.
The most challenging part of my diagnosis
The biggest challenge is probably just seeing how everyone reacts to it. I know I can do the treatment. I feel like it’s scarier for everyone else, especially for my wife. Luckily, my kids don’t understand as well, so they haven’t had that fear.
For me, it’s hard to explain. I know what I have to do, but seeing how everyone else responds to it, even extended family — every time I see them now, that’s what they ask me about because everyone is worried. The only thing I can think of is that I want to do everything I can. That’s kind of why I opted in to do the chemo. I wanted to do everything I could, the most I could, so that I don’t have regrets later, wondering if maybe something could have worked and I didn’t do it.
What hope means to me
Hope is just knowing or believing that good things can happen. If I didn’t have hope, I would just give up. Why go through the treatment? It’s difficult. Why do it if you don’t have any hope of it working?
I would tell anyone to know that I believe everyone has a purpose, and with that purpose, you can help other people. My message is that if you’re going through a hard time, just keep going. Hopefully you have a strong support team. That’s been what has helped me the most. If you don’t, then find one, because other people can help you a lot.
I’ve had a ton of help from family. My sisters did bake sales to help raise funds, and obviously, my family here at home. I know that they love me and I love them, and that hope, the hope of continuing to be with them, is what has gotten me through most everything.
My biggest advice to others
In nursing school, one of the biggest things they tell you is to be an advocate for your patients. Be an advocate for your patients as a nurse. I would also say: be an advocate for yourself. If you feel like something’s not right, make sure that you are being heard.
There’s a chance that when I went to the ER, they wouldn’t have done an MRI and would have sent me home or told me to go see an ophthalmologist again. Make sure that you are getting the treatment and help you need, and that you’re not being ignored. Make sure the doctor you see isn’t just going through the motions, that the doctor hears you.
Just be an advocate for yourself and make sure that you’re heard when you’re going through something like this.

Inspired by Steven's story?
Share your story, too!
More Head and Neck Cancer Stories
Vikki F., Head and Neck Cancer (Nasal Squamous Cell Carcinoma)
Symptoms: Nosebleeds that persisted for years, nose changed in shape, nasal pain, migraines
Treatments: Surgeries (subtotal rhinectomy, reconstruction surgery including radial forearm free flap, bone grafts, and cartilage), chemoradiation
...
Red S., Tongue Cancer (Squamous Cell Carcinoma of the Tongue), Stage 3
Symptom: Persistent tongue ulcer that increased in size
Treatments: Surgeries (partial glossectomy, flap surgery), radiation therapy
...
Alyssa N., Adenoid Cystic Carcinoma
Symptoms: Persistent jaw pain, lightning-like facial pain during the first bite of meals
Treatments: Surgery (tumor removal), radiation
...
Eva G., Oral Cancer, Stage 4
Symptoms: Sore on the tongue, which caused pain during eating and speaking; changes in the color and texture of the tissue where the sore was located
Treatments: Surgery (partial glossectomy, radical neck dissection, reconstruction), radiation
...
Teresa B., Recurrent Breast Cancer (Hormone-Positive), Oral Cancer (Lip Cancer), and Skin Cancer (Melanoma)
Symptoms: Lip cancer: chapped lips & a pimple-like growth on lip, breast cancer: enlarged left breast with lump, melanoma: none
Treatments: Surgeries (bilateral mastectomy with reconstruction, lumpectomy, craniotomy, Mohs, surgery, wide local excision), hormone therapy, radiation therapy
...