Laurent Gemenick’s Bladder Cancer: A Story of Second Opinions and Self Advocacy
Laurent’s story is a reminder that, as overwhelming as it is, living with bladder cancer can be filled with hope and learning to advocate for yourself can lead to opportunities to help others. This inspired the birth of a national organization to help bladder cancer patients across all of Spain.
Laurent was relatively young and didn’t fit the usual profile of a bladder cancer patient. So when he first noticed blood in his urine, urologists assumed an infection, but the blood in his urine continued. He then had an ultrasound which came back negative, but the blood in his urine continued. So he had a cystoscopy, which allowed them to look at the bladder from the inside and this procedure was what led to a bladder cancer diagnosis in October 2022.
Getting the right diagnosis had proven tricky, but his need to advocate for himself was just beginning as an even bigger turning point was just around the corner. After a difficult surgery to remove the bladder tumor, Laurent received a rushed recommendation for bladder removal. He and his partner, David, decided to seek second opinions. Five second opinions. Visiting five specialists gave them clarity and hope, as four of the five encouraged bladder preservation, proving how vital self-advocacy can be.

Throughout this experience, Laurent realised how isolating bladder cancer can feel. He struggled to find patient-friendly information and supportive communities. That’s why he joined a French support group and eventually co-founded CANVES, Spain’s first bladder cancer patient group, to help ensure that no one faces bladder cancer alone. By sharing experiences, hosting events like Spain’s first National Bladder Cancer Patients’ Day, and advocating for early detection, he empowers patients to ask questions, connect with others, and make informed decisions.
Laurent wants every patient to know that life doesn’t stop with a diagnosis, and that reaching out for support and timely access to reliable resources can make all the difference. Watch his video and read his interview below for more on:
- How second opinions changed one bladder cancer patient’s life
- Why Laurent believes no patient should ever feel alone
- A candid look at life after a harrowing bladder cancer diagnosis
- The inspiring birth of CANVES
- Practical tips for self-advocacy and early detection
- Name: Laurent Gemenick
- Diagnosis:
- Bladder Cancer
- Symptom:
- Presence of blood in urine
- Treatment:
- Surgery: transurethral resection of bladder tumor (TURBT)

Thank you to Johnson & Johnson for supporting our patient education program. The Patient Story retains full editorial control over all content.
This interview has been edited for clarity and length. This is not medical advice. Please consult with your healthcare provider for treatment decisions.
Interviewed by: Taylor Scheib
Edited by: Chris Sanchez and Jeff Forslund
There is no need to be afraid. When you get this news [that you have bladder cancer], you just have to keep going and keep living.
Laurent Gemenick – Bladder Cancer Patient Advocate
About Me
I’m Laurent. I’m from Belgium. I was diagnosed with bladder cancer.
I’m a happy-go-lucky person, always smiling. My friends and family describe me as talkative and positive. I love to garden.
When I was diagnosed with cancer, my world, my life, fell apart.


My First Symptom Was Blood in My Urine
The first symptom I had was blood in my urine. In my case, it was different, because it only became obvious at the end of urination. It wasn’t easy to see with my naked eye.
That’s what first made me go to the doctor.
Trying to Get My Diagnosis
At the appointment with the urologist, I discovered that I didn’t fit the age for having bladder cancer.
This kind of cancer usually affects older men or people with a family history of cancer. Neither was true in my case. So my doctor said that the blood in my urine could’ve been caused by a strain instead. He told me to come back another time.
But then I produced bloody urine again. I went back to the doctor and got an ultrasound. They suggested that I get an ultrasound because it can reveal if there is a tumor in the bladder.
Still, nothing came out, but I continued to have blood in my urine. This time, they did a cystoscopy. This procedure places a camera into the bladder and lets doctors confirm the patient’s diagnosis for sure.
That’s how they ended up diagnosing me with bladder cancer at the end of October 2022.
My relationship with the doctor wasn’t great. I was in the ICU for three days because of a procedure called transurethral resection of bladder tumor (TURBT). It didn’t go well, which is why it took three days.
Then the doctor took a sheet of paper out and said they would have to remove my bladder. He told me to “sign here” on the paper, and they’d do the surgery in 10 days.
I didn’t even know at the start that you could get bladder cancer, and I went from that to the point that this doctor was telling me, “I’m going to need to take out your bladder.”
Luckily, I had David by my side. He was always by my side.
We started looking for second opinions. We went to five specialists and got five opinions.
Four of those five specialists presented the same thing. They agreed that for treatment, they recommended preserving the bladder because of my young age, and that you don’t remove the bladder from a young patient.
They actually didn’t even use the word “cancer.” They kept saying “polyps.” The doctor I’m seeing now, who’s treating me, even took a long time to say the word “cancer.”

I didn’t even know at the start that you could get bladder cancer, and I went from that to the point that this doctor was telling me, “I’m going to need to take out your bladder.”
Laurent Gemenick – Bladder Cancer Patient Advocate

It’s So Important to Get a Second Opinion
The issue of second opinions is very important.
The patient may forget to get one because they go into shock after hearing the diagnosis or because of the mindset that the doctors are always right, and “what the doctors say is what we should do.”
But this is life-changing surgery. If they take out this organ, it’ll change your life because you’ll need to have a colostomy bag put in.
It requires seeing more than one doctor and getting more than one opinion so you can make an informed decision. If they are on the same path or not, if they have the same ideas.
My Treatment and Follow-up
I get follow-up appointments every six months. I get a urinalysis and cystoscopies.
The first resection surgery during the ICU stay in the beginning removed most of the bladder cancer. Since my biopsy results have been good, I have the check-ups every six months.
I Found it Hard to Find Information For Patients
We tried looking for information on the internet. You will find everything online — including the worst-case scenarios. David was my filter because he kept me from searching online.
On Facebook, I found a group of bladder cancer patients, but they were from France. Luckily, my first language is French. They welcomed me to the group and supported me. I joined at the same time as four other patients. Three had their bladders removed. One has passed away.
It’s a support group — they live what I live with bladder cancer. We discuss treatments. We experience anxiety at every appointment. We know the shared pain.
We were introduced to the World Bladder Cancer Association in Madrid, and that’s how we started CANVES.
Why I Decided to Start a Patient Organization
I don’t think what happened to me happens to all patients — being told that they would need to have their bladders removed, and “sign the paper here.” I think it has to be nuanced, and it depends on the experience and empathy of the doctor who’s taking care of you.
In Spain, there are two healthcare systems. You have the public healthcare system and the private healthcare system.
The private healthcare system works well. The public system does, too, but it takes more time to get things done there. You can’t get an appointment as quickly or often. Doctors usually don’t have more than five or ten minutes to talk to each patient. That’s actually a Europe-wide problem. In Belgium, the same thing happens.
That’s why we created CANVES. We understand that doctors don’t have a lot of time to dedicate to their patients, to give them the explanations or support they need. So we want to give the patients the information they need.
That’s our motivation. To make sure no one has to be alone with this.

That’s our motivation. To make sure no one has to be alone with this.
Laurent Gemenick – Bladder Cancer Patient Advocate

Fighting the Stigma in Bladder Cancer
There are 22,000 cases of bladder cancer each year in Spain, which makes it one of the most frequently diagnosed cancers here. There was no patient association here. Nothing. Resources? Nothing. Support? Nothing.
Most patients who have bladder cancer are indeed men, and those who are older. But we have to consider that more and more young people are getting diagnosed with bladder cancer. Patients used to be 70 or 80 years old, but they’re getting younger, 60 or maybe even younger.
And men don’t talk; they don’t go to the doctor.
It seems different for women. Starting when they are little, we tell them to go to a gynecologist as soon as puberty starts, to get tested. We don’t have similar conversations with boys to see a urologist for testing until they are typically 40 or 50 years old.
A milestone — this year, we organized the first National Bladder Cancer Patients’ Day. This was so important because we had the support of the Spanish scientific societies. This was huge because it happened in a short time, and united all these professionals to help people in one room.
That’s the most important thing for us: helping people. We get emails, and we talk and speak to people every day. This is the best thing we can do. This is why we exist.
We hope to have better information and build a faster line of detection, so if a patient goes to the emergency room with blood in the urine, we can help implement a protocol of tests to see whether it’s bladder cancer. Most of the time, if it’s caught early enough, bladder cancer is curable.
My Message of Hope for You
There is no need to be afraid. When you get this news, you just have to keep going and keep living. That’s the most important thing.
Many people think, “Why me?” Cancer diagnoses are becoming increasingly common.
You have to keep on living because life is short.

You have to keep on living because life is short.
Laurent Gemenick – Bladder Cancer Patient Advocate
Special thanks again to Johnson & Johnson for supporting our patient education program. The Patient Story retains full editorial control over all content.

Inspired by Laurent's story?
Share your story, too!
More Bladder Cancer Stories
Laurent Gemenick, Bladder Cancer
Symptom: Presence of blood in urine
Treatment: Surgery: transurethral resection of bladder tumor or TURBT
Jon T., Locally Advanced Muscle-Invasive Bladder Cancer
Symptom: Darkening urine, blood in urine, dull right flank pain
Treatments: Surgery(transurethral resection of bladder tumor or TURBT), antibody-drug conjugate, chemotherapy
Michael V., Bladder Cancer (Non-Invasive High-Grade Papillary Urothelial Carcinoma), Stage 1
Symptoms: Frequent urination, burning sensation when urinating
Treatments: Surgery (transurethral resection of bladder tumor or TURBT), immunotherapy (Bacillus Calmette-Guérin or BCG treatment)
Dorinda G., Bladder Cancer
Symptom: A significant amount of blood in the urine
Treatments: Surgery (transurethral resection of bladder tumor/TURBT, surgery for papillary lesion), immunotherapy (BCG), chemotherapy
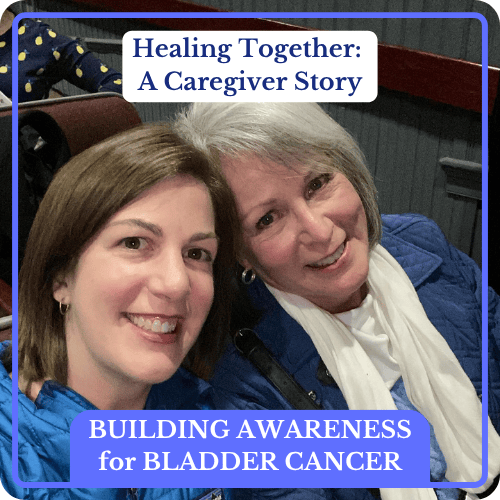
Healing Together: A Mother and Daughter Navigate High-Grade Bladder Cancer
Mary Beth’s story about caregiving starts with an important awareness message about female bladder cancer symptoms.
Danny G., Non-Muscle Invasive Bladder Cancer
Symptoms: Fatigue, back pain, erectile dysfunction, nausea
Treatments: Surgery (transurethral resection of bladder tumor or TURBT), chemotherapy, immunotherapy