From Doctor to Patient: Shiva Faces a Double Cancer Diagnosis: Rectal and Kidney Cancer
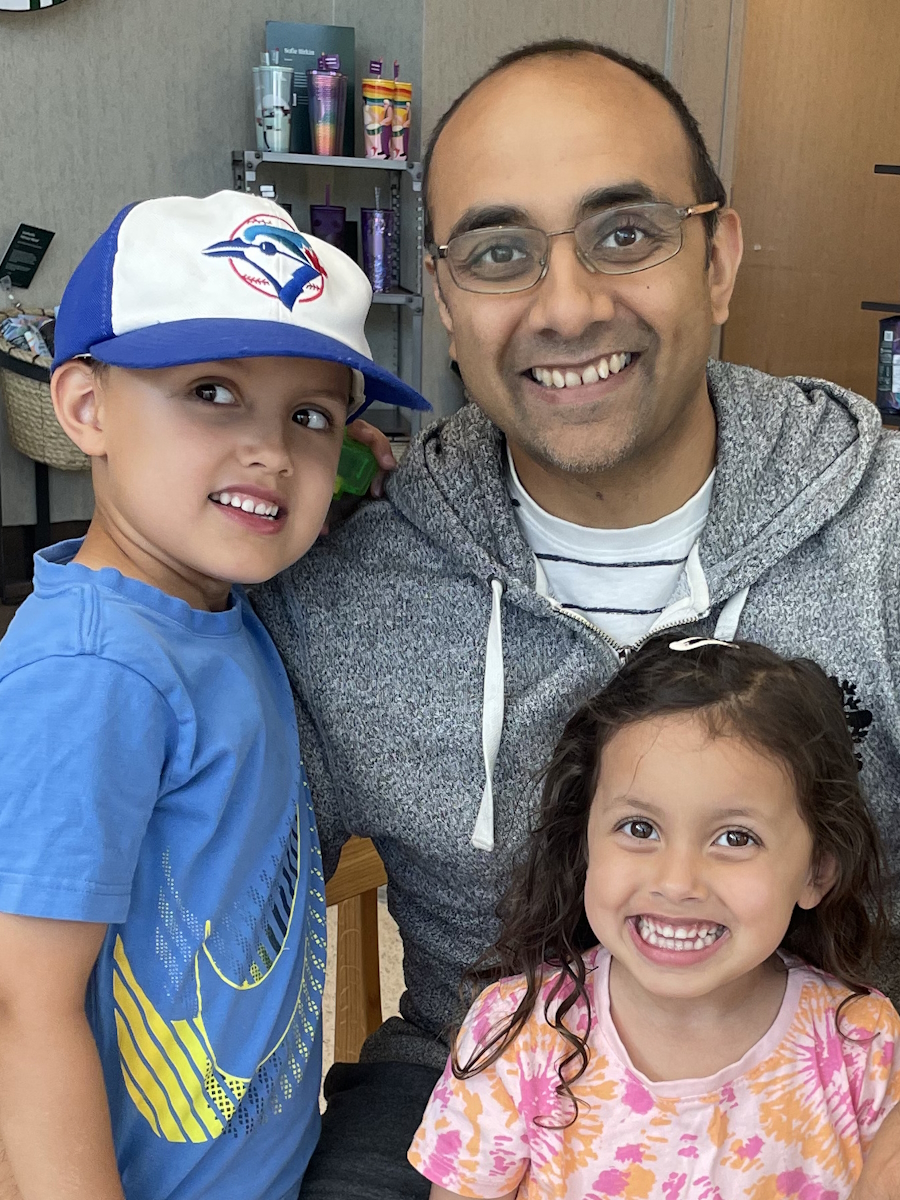
When Shiva, a family doctor from Toronto, first noticed stomach pain, hemorrhoids, and nagging backaches, he chalked it up to stress. After all, he was in the process of moving across continents with his wife and three young kids. But when a friend’s story nudged him to book a colonoscopy at age 40, he found himself waking up to life-changing news: rectal cancer.
Interviewed by: Nikki Murphy
Edited by: Katrina Villareal
As if that wasn’t enough, follow-up scans revealed a separate case of kidney cancer. While the thought of two different cancers could have been overwhelming, Shiva chose to view it as a strange kind of relief that it wasn’t metastasis. His dark humor helped him cope, but what truly carried him through was his family’s love and an incredible care team at North York General Hospital.

Treatment began with chemoradiation: chemotherapy tablets and six weeks of daily radiation. Shiva described the nausea, fatigue, and anxiety of rushing to appointments with a full bladder as more mentally draining than physically. He admitted that “scanxiety” is real, the unease that creeps in before every test or scan. Throughout it all, he leaned on resilience, therapy from psych-oncology, and support from his wife, kids, and community.
Eventually, doctors recommended surgery, which was an eight-hour operation that combined kidney and bowel procedures. Shiva also received an ileostomy, something he adjusted to with surprising grace thanks to excellent stoma nurses and persistence in regaining independence. He continued with immunotherapy for the kidney cancer, grateful to have access to cutting-edge treatment with minimal side effects.
Shiva often reflects on the emotional toll. He speaks candidly about post-traumatic stress, the way everyday aches trigger worry, and how mental health support became as important as physical recovery. Importantly, he emphasizes that health is a privilege and advocates for accessible, inclusive care so no one is left behind.
Now cancer-free, Shiva describes himself as changed. He prioritizes self-care, cherishes time with his children, and embraces life with renewed perspective. He encourages others to trust their care team, seek mental health support, and live fully, whether that means enjoying a simple meal or saying yes to experiences without delay. His story is about resilience, appreciation, and the reminder that life, however uncertain, is meant to be lived wholeheartedly.
Watch Shiva’s video to find out more about his story:
- Discover how a doctor became a patient and found resilience.
- What Shiva learned about life after rectal cancer and kidney cancer
- The hidden mental health side of cancer care you don’t hear about
- Why therapy and humor helped as much as treatment
- How family, faith in care, and small wins kept him grounded
Scroll down to read the transcript of Shiva’s interview.
- Name: Shiva S.
- Age at Diagnosis:
- 41
- Diagnoses:
- Rectal Cancer & Kidney Cancer
- Staging:
- Rectal: T2
- Kidney: T3
- Symptoms:
- Pressure and urgency of bowels
- Back pain
- Treatments:
- Chemoradiation
- Surgery: ileostomy, combined bowel and kidney surgery
- Immunotherapy
This interview has been edited for clarity and length. This is not medical advice. Please consult with your healthcare provider to make informed treatment decisions.
The views and opinions expressed in this interview do not necessarily reflect those of The Patient Story.
Hi, I’m Shiva
I’m Shiva. I’m from Toronto, Canada, and I was diagnosed with T2 rectal and T3 renal cancer in 2024.
When I first noticed something was wrong
In 2023, we moved from England to Canada. I’m a family doctor. We were moving with my family, my wife, and my three kids, so it was obviously a very stressful time. Throughout my life, I’ve always had trouble with my bowels and stress, so I didn’t think too much of it. I couldn’t think of a more stressful time than moving with three small kids.
The symptoms, like hemorrhoids and a vague tummy pain, came up and didn’t go away, and that was the problem in retrospect. I was having back pain, but nothing specific or anything that stood out. I’d like to think, as a physician myself, any big red flags and a little embarrassingly, it turned out to be cancer.
The reason I went for a colonoscopy was because I had a friend whose wife was unfortunately diagnosed very young with a different kind of cancer. I thought to myself, “I’m 40. What would I say to my own patients? I should go for a colonoscopy.” I had my family doctor refer me for one. Luckily, it was very quick, so I didn’t have to wait or argue about getting an investigation. I didn’t have to pay for it because I’m in Canada, which was also great.
The moment everything changed
After I had it done, I woke up to the biggest shock of my life. I worked in family medicine and general surgery, so I’d seen and done colonoscopies on patients and operated on them. As soon as I woke up, I knew something wasn’t right. There weren’t any pamphlets about managing your hemorrhoids. I was thinking to myself, “This is it. This is not going to be a good day.”
Sure enough, I was taken to a very quiet room and waited to get the news. Certain parts of the day are a bit of a haze, but that moment, I remember crystal clear every little bit. As I waited for my wife to pick me up, I knew that she was not going to expect this.
In retrospect, I don’t know what I would have done differently.
I was in shock. I had it in my head that I needed to tell people right away. Shock was a protective mechanism. I didn’t know what to do. I thought, “I’m going to tell my family and whoever I have to tell. I’m going to call up friends who could help me get a plan in place,” all while having a ton of bricks dropped on you and figuring out your position in life. I just turned 40-something and I’m mortal, it turns out.
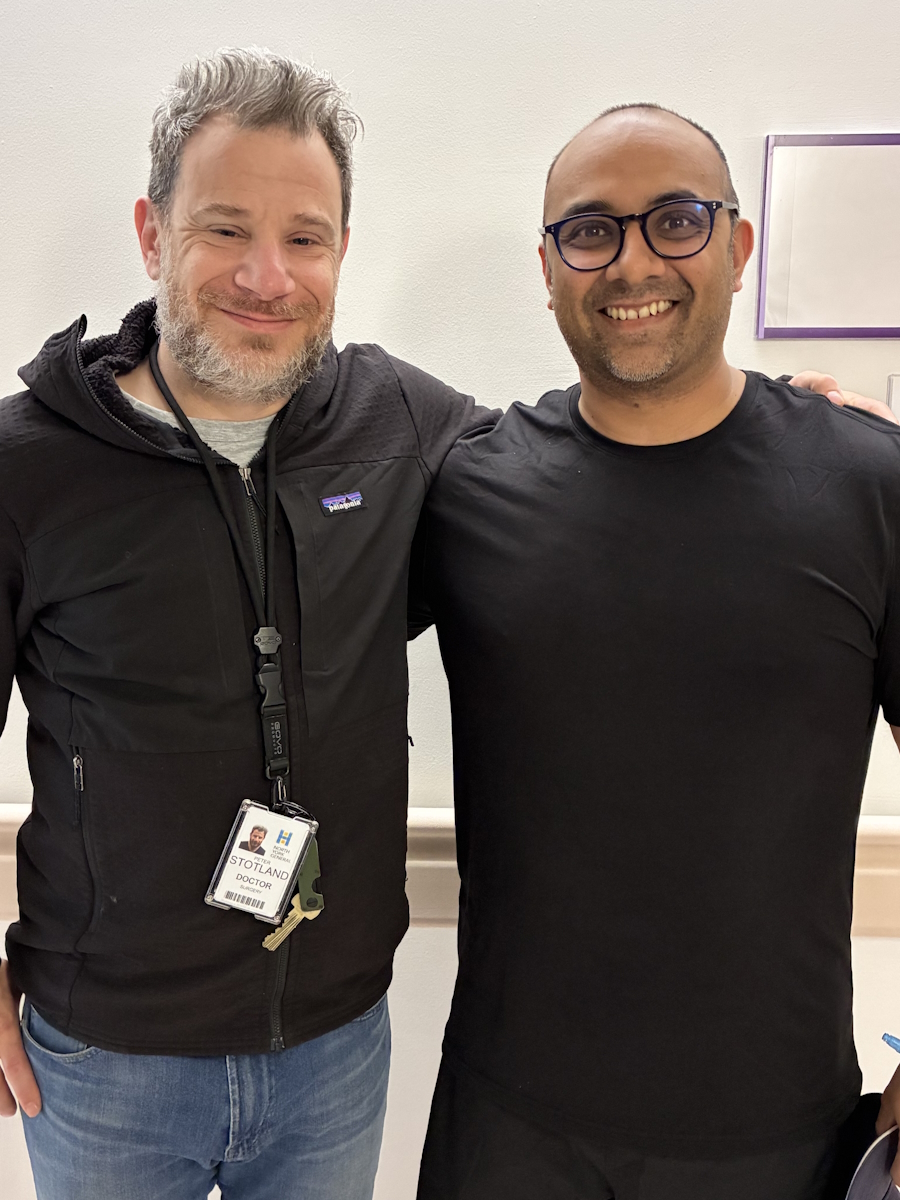
I didn’t want to sit around and ruminate about what’s going on or what’s going to happen too much. The first thing I had to do was to get everything in place and get everyone I needed on board because it was going to be a rough ride. I was lucky enough to have a friend who works in this field. I didn’t hold back in asking whoever I needed to ask and they recommended excellent people at North York General Hospital here, who took everything on from there.
Additional scans revealed the unthinkable
It was a matter of getting a plan in place. I had CT scans and MRIs within a week. I met with the surgeon who put everything together and then met with the oncologist. It was a matter of coordinating everything and trying to stay as normal as I could for the kids. At that time, all my kids were under seven years old, so we had to carry on. We had to pretend everything’s okay, even though I feel like sitting on my bed and not doing anything.
The next step was getting the scans, which showed a lump on my kidney as well. I thought, “Great. This is a metastasis,” but we don’t know yet. They said they’re going to have to do a biopsy. Then they said, “We need to do another scan because there’s another lump on your femur bone.” They said it doesn’t look like anything, but from my perspective, we can’t take anything for granted. At that point, I said, “Can we not scan anything anymore? Because every time you put me through a scanner, you’re finding something. Let’s get these blinkers on and deal with what we got.”
Thankfully, that bony thing turned out to be nothing, but the lump on the kidney turned out to be another cancer on its own that happened to be picked up. I remember thinking it was good news because it’s not a metastasis. Then I remember thinking, “Wow. The bar has gotten so low that it’s better to have two separate cancers than one that’s metastasized.” I laugh at it now. I’ve got a dark sense of humor and that’s how I cope.
I went to see the urologist to make a plan. It was all about timing. What should we do next? Should we operate? Should we do chemotherapy and radiation? Should we do chemotherapy upfront and take a chance? I was told we could do anything. There are options. You have to trust that you’re going to get the best advice.
I have nothing but good things to say about the team at North York General. To be honest, there’s no way I’d get through any of this without my wife and my family. If I were to do this on my own, it’d be too much. I would withdraw at that point. Thank God I had, like all these people around me, but especially my wife, to pull it all together.
My treatment plan
The overall plan after meeting with everyone was to get chemotherapy and radiation. The chemotherapy is going to be in tablet form and six weeks of radiation every day, five days on and two days off. We’ll see how everything goes and then decide if we need to do more chemo or surgery. I met with the radiation oncologist and got everything in place. I got my little tattoos done, which was unbelievably painful even though they’re three little dots.
I remember walking around a hardware store because I had to use the bathroom and having the most nauseating experience. I thought, “Is this going to be six weeks of this?” I didn’t know what was going to happen. I didn’t know what to expect. I said I would never go back to that hardware store again because you start associating places and smells. It’s all vivid. Thankfully, that settled down and didn’t come on with the radiation. They said the chemo tablets would make the radiation work better. The main thing I experienced was unbelievable nausea. I wasn’t vomiting, but I didn’t feel like eating anything.
The other thing was having to drink so much water to get the radiation done every morning. I drive 30 minutes and my bladder has to be absolutely full. You feel nauseous, plus the anxiety of being caught in traffic and not arriving on time. You have all these feelings.
I’m lucky to have these options. I’m lucky to be able to go through this and you don’t want to waste it. At the same time, going to the radiation wing of the hospital, you’re surrounded by people with cancer at various stages. That was a big side effect mentally, seeing people going through the same thing. You are at different stages and you’ve got this big question mark in your head. “Is that going to be me?” That was hard to deal with.
The other side effects were a bit of tingling and numbness in the fingers, but nothing too bad, and a bit of skin irritation.
With general practice, I was working with breast cancer patients. Sometimes, people tolerate radiation well, but some people don’t. When you know these things, you think of the worst-case scenario. You think of the worst person you’ve ever seen.
You start delving into stuff. I came across The Patient Story, which was good therapy for me in a way because I was reading about people my age. You’re trying to take away things and see how people dealt with stuff. But at the same time, you’re hearing about these horrible side effects some people get. When you’re in Canada and you’re not paying for it, you think, “Give me everything as long as I can tolerate it. This is all going to be for the benefit. No pain, no gain.” That was my thinking, but it was tiring.
The big thing was the fatigue. I didn’t realize it until I finished treatment. It’s like, “Wow. I feel like eating better. I feel like drinking more water. I feel like exercising.” This cloud hangs over you for a bit, but you don’t even realize it when you’re in it. It’s a lot of adrenaline, too. You’re exhausted.
When I finished radiation, I had a break. They’re going to redo all the scopes and everything. It’s been six months. This can either be good or bad, and you’re waiting for that, so that was nerve-wracking as well. I was thinking about things a lot more. Everything seemed amplified then. I don’t know if there was a bit of a rebound swelling, but symptoms I didn’t have started coming up, like pressure and pain.
I remember preparing for the colonoscopy and the MRIs, and I thought, “I can’t do this again. I can’t do another enema. I’ve had to do so many enemas for these investigations. It’s so painful.” I thought I was going a little bit crazy with the pain. My pain threshold is not good. Thankfully, I have not had to do that again.
They said, “Let’s go for surgery now. Let’s schedule it for the day after Father’s Day.” You start thinking about these things. Again, you have to keep going. It was a surreal experience, but my surgeon was amazing. The first day he met me, he said, “Look, I know this is a lot for you. You know too much. Your head is going to be all over the place. I’m going to get you to talk to someone from psych-oncology. Talk to them.” It was non-negotiable.
Having never spoken to a therapist, I thought it was good to have that. That was an amazing experience to have someone to talk to. That was the holistic care that we all talk about and aim for. That’s why the whole team at the hospital was absolutely amazing.
The next step was ileostomy surgery
Surgery was interesting. A few weeks before, the surgeon said to me, “You’re going to have to have an ileostomy,” and I was alright with that. I want maximal therapy and I totally trusted him. It’s not ideal. Nobody likes the idea of having a bag, but when you consider the alternative, it’s not bad.
To be honest, you get used to it. We’re at the point where we’re thinking if we’re going to reverse it, but I don’t want to jump out of the pan into the fire. I’m happy if it’ll go, but you don’t know what’s coming next either. I don’t know what that recovery is like either.
Surgery took a lot out of me because they did the kidney surgery and the bowel surgery at the same time, so it was eight hours of operating time. I remember coming back to the ward and being absolutely out of it. It took about a week before I got out of the hospital, which was probably a bit longer than anticipated, but I needed it. It was great to be in a place where they’re not kicking you out and to have that luxury. It was good to get out, but they allowed me to recover. Everyone was amazing about it.
The psychiatrist knew me and she said, “You’re a stoic person. You’re not going to say when you’re in pain. Stay for a couple of days.” It’s amazing to have someone advocating for you in that way because I felt helpless at times and you don’t want to put anyone out. Am I blocking the bed for somebody else? I don’t want to be a burden. If someone else needs surgery, what if I’m in their bed? No, you need to get better, too. You need to be in a better spot.
Health is a luxury. Having someone to advocate for you is a luxury. My wife and my mother-in-law were helping look after the kids while I was gone. It was hard to be away and keep it all under wraps, but the kids were amazing. Everyone was amazing.
Adjusting to life with an ostomy
Post-op, it was time to get better, physically, mentally, and emotionally. You’re trying to recover. You’re waiting on test results. Is everything going to be fine with my lymph nodes? Is anything unexpected coming up? You’re waiting and trying to get back physically to where you were.
I was eating the blandest food now with the ostomy. I love my food and I can’t eat anything I want to eat. All I could eat was rice pudding. I never want to see rice pudding again. It’s delicious, but when you eat it 20 days in a row, no thanks. I had to change my diet. I also did a lot of pacing around in my backyard and walking around the neighborhood as my exercise. I didn’t want to push myself too far.
Getting used to the ostomy partly involved getting used to eating again. It was surprisingly easy to manage. When you’re at home, it’s different. The stoma nurse was amazing in teaching me how to manage it. People gave me a lot of leeway because I’m a doctor, but you’re doing it in front of a mirror. It’s different as a doctor and as a patient. She was good and gave me the confidence that I needed to know that I can do this. Sure enough, I did. When you’re figuring things out, you figure them out pretty quickly because you only make that mistake once or it becomes the new normal for you.
Here, you get a grant that helps pay for some of the medical equipment, but these are expensive. I don’t know what people do who can’t afford it. The big fear for me was being out in public and having to change my bag. In the beginning, I was going to regular bathrooms and I wondered if I could use the disabled one. Does this count? I’m trying to rationalize. You don’t want to get harassed by someone and be told you shouldn’t be in there. Sometimes I do and sometimes I don’t. It’s these silly things that go through your head.
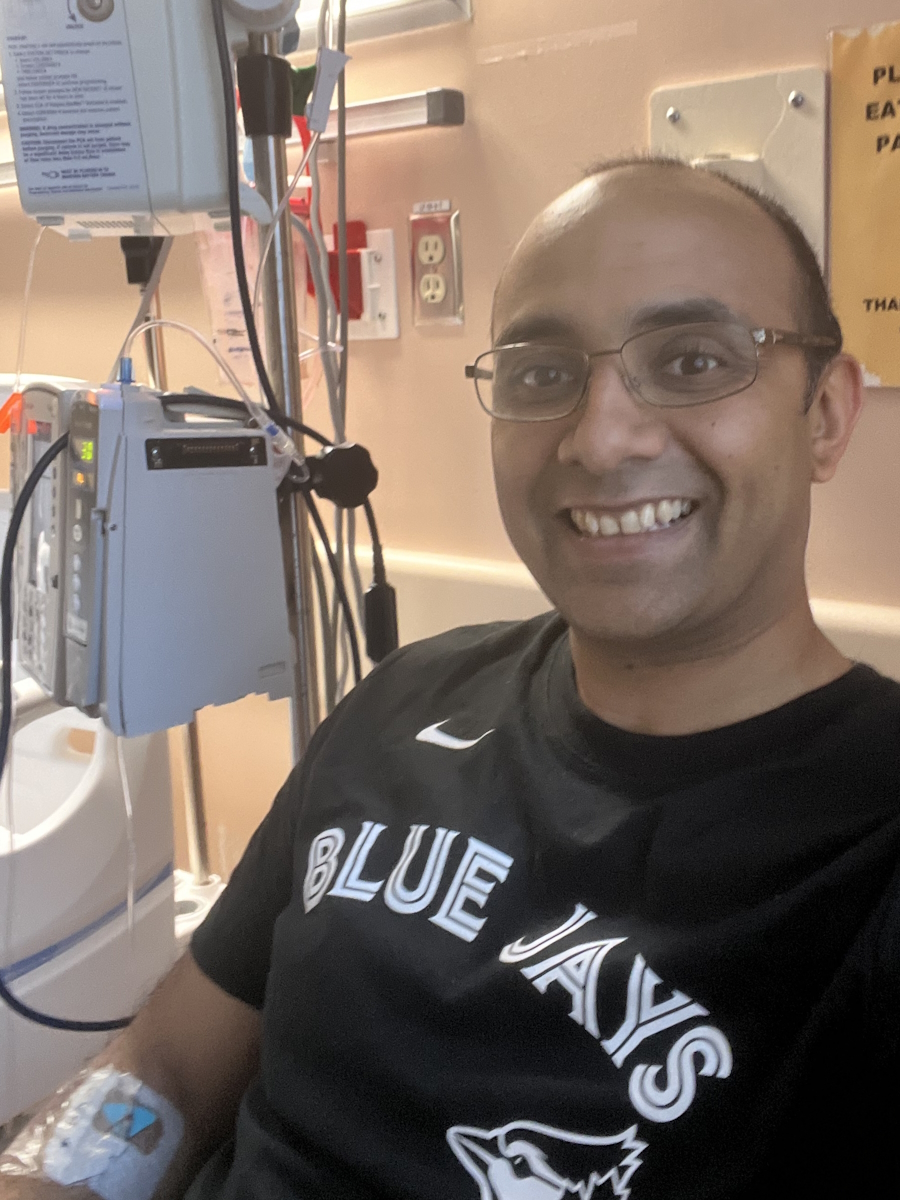
I had to take some more chemotherapy tablets after the surgery. I experienced the same thing with the tiredness. The nausea wasn’t as bad. I got immunotherapy at the same time. A year of that and that was more for the renal cancer. After all the testing, they said I was eligible for it.
For the immunotherapy, I had to go to the chemo ward for it, but it’s not like chemo. I didn’t have any side effects, but I hear people who have them and have to stop treatment because of the side effects. I feel lucky that I’ve been able to get it with relatively few, if any, side effects. Thank God for it. If it does everything it says, like improve survival and this and that, great. Keep it coming.
Now we’re at a point where we’re thinking about whether we can reverse the stoma. Soon, hopefully.
I have scanxiety
The small things that people say can make such a big difference mentally. I was still in the hospital and the oncologist came by to say hi and see how I was doing. He said, “Congratulations, you’re cancer-free now.” I know it meant so much for my wife to hear that and it meant a lot for me to hear that. I was in a little bit of a daze post-operatively, but it stuck with me. This is it. We’re starting fresh again.
I get scans every six months. Regular colonoscopies will be the new way forward. You can’t predict the future. You don’t know how things are going to be. But if you ask me, I can say I’m cancer-free. My oncologist told me and as far as I know, he’s right.
Do I get anxious when there’s a scan? Yes, every time it seems. Maybe it’s just in my head, but I feel it every time I’m going through something else or another symptom comes up. The scanxiety that everybody talks about is real. You think about every pain that you get now. I don’t think about it until there’s a scan coming up. I try and rationalize the symptom by saying everyone else experiences it, but I can’t take it for granted because I didn’t think that this would be anything when I said I should get a colonoscopy.
Unfortunately, these things happen. I’m more aware now of what I put into my body. I’m at a stage now, thankfully, where I’ve got so much more energy and the fog’s been lifted. Before, it was more of I can do things, but it’s like doing them underwater, so you’re doing them slowly. You’ve got the motions down. But now, the fog’s been lifted and I find I can do things now. I can be healthier. I can make healthier choices and get myself in better shape.
I want to get back to normal. That was in the past. This is the present and the future. You have to enjoy your life and everything about it now. It took a lot to get to that mental stage. There are good days and bad days, mentally more than anything.
I’m a changed person now
You don’t think about your mortality. There’s an innocence that I feel like you lose. It’s hard to listen to things or see things, and have it not go back to cancer. They trigger you. Your mind goes to, “Will I ever be 90 years old? Will I ever get to that stage in life?” Maybe. Not many people get to 90 anyway. But that innocence about things. Watching a movie trailer and seeing it’s about a person with cancer. It’s like, “Great. Do I want to watch this? Is this going to be a downer?” In the past, I would have watched it with no issues.
I did a lot of research on myself — self-audit is how I think about it. Cancer is so traumatic. Post-traumatic stress is how it was explained to me. There are different things you can do for that, like journaling and writing. I never did that and I never thought about doing that, but you have to do it. In the same way you trust your surgeon, you have to trust that inner monologue in your head. You have to trust the therapist or oncologist or whoever tells you that you need to work on these things because it’s going to help with your recovery and reestablish yourself. You can either totally withdraw or embrace it and channel it into something good.
I’m not at a stage where I feel like my kids are not going to understand this. There’s going to be a day when I want them to understand it and they’ll have to. I hope they would see this and help them understand that weird summer we had when we couldn’t jump on daddy’s tummy.
You lose that bit, but you gain so much. I’ve gained this appreciation for things. Do the things that you want. Don’t put them off. Live in the moment. I wasn’t doing that before. I wasn’t looking after myself the same way. I was the type of doctor who you do as I said, not as I did. Now I take the time to look after my body and do the things that mentally help me feel better, and I prioritize those for my overall health. That’s a legacy that I want to leave for my kids, the habits that they should do, so that they’re never in this position.
My advice to others
Positivity is definitely a luxury in life. That’s what we have to prioritize in life. You can do everything right and still get cancer. But at the same time, you’re going to get through it. You’re going to see the other side of it. You’re here now, so you might as well enjoy it. There’s so much to be worried about in this world. The world’s going to keep turning. It doesn’t revolve around me.
I’ve got so much to be thankful for, like my wife, my kids, my family, and my friends. It’s been a crappy time, but everyone has been amazing and if nothing else, it made me appreciate life so much better.
Go and enjoy life. Whether you live to be 90 or not, you have a limited time on earth. Use 100% of that time. Don’t shut yourself out of this world because you’ve been diagnosed with something. Thank God for socialized medicine. The most important thing that we have as a society is to look after our own health.
I’m glad that I had such an amazing team of people at North York General Hospital. I’m sure there are great teams everywhere. Trust your doctors. Trust your nurses. Trust everybody looking out for you. Trust the cancer researchers. It can happen to anyone, unfortunately, but it’s not a death sentence by any means. It’s not a fun ride, but the ride ends and you go on living.

Inspired by Shiva's story?
Share your story, too!
More Rectal Cancer Stories
Kalei M., Rectal Cancer, Stage 4 (Metastatic)
Symptoms: Presence of mucus and tissue-like substance and blood in stool, stomach cramping
Treatment: Radiation therapy, chemotherapy, surgeries (two lung resections)
Jessica A., Rectal Cancer, Stage 4 (Metastatic)
Symptoms: Changes in bowel movements, blood in stool, abdominal pain, back pain, difficulty sitting comfortably, constipation, feeling of incomplete evacuation (as if some stool remained after bowel movements), mucus-like stool consistency, bloating
Treatment: Immunotherapy under a clinical trial
Shiva S., Rectal Cancer, T2, and Renal Cancer, T3
Symptoms: Pressure and urgency of bowels, back pain
Treatments: Chemoradiation (for rectal cancer), surgery (ileostomy, combined bowel and kidney surgery), immunotherapy (for kidney cancer)
Jeanine B., Rectal Cancer, Stage 3 (T3bN0M0)
Symptoms: Long history of bleeding that was blamed on hemorrhoids, pain in the tailbone, urgent need to use the restroom, unusually narrow stools, presence of mucus in stools, fatigue
Treatments: Chemotherapy, radiation therapy
Devon B., Rectal Cancer, Stage 4
Symptoms: Pain when trying to move bowels, increased frequency of bowel movements alternating with periods of constipation, passing mucus instead of feces, narrow stools
Treatments: Surgery (ostomy surgery), radiation therapy, chemotherapy
James K., Rectal Cancer, Stage 3C/4
Symptoms: Occasional rectal bleeding, increasing fatigue
Treatments: Chemoradiation, surgeries (coloanal pull-through, temporary ileostomy, ileostomy reversal, permanent colostomy), adjuvant chemotherapy
More Kidney Cancer Stories
Mia H., Kidney Cancer (SMARCB1-Deficient Renal Cell Carcinoma, Non-Sickle Cell Trait), Stage 4
Symptoms: Bad cough, fatigue, nausea
Treatments: Chemotherapy, radiation, immunotherapy
...
Alexa D., Kidney Cancer, Stage 1B
Symptoms: Blood in the urine; lower abdominal pain, cramping, back pain on the right side
Treatment: Surgery (radical right nephrectomy)
...
Bill P., Papillary Renal Cell Carcinoma, Stage 3, Type 1
Symptoms: Kidney stone, lower back pain, sore/stiff leg, deep vein thrombosis (DVT) blood clot
Treatment: Nephrectomy (surgical removal of kidney and ureter)
...
Burt R., Pancreatic Neuroendocrine Tumor (pNET) & Kidney Cancer
Symptom: None; found the cancers during CAT scans for internal bleeding due to ulcers
Treatments: Chemotherapy (capecitabine + temozolomide), surgery (distal pancreatectomy, to be scheduled)
...
Sonia B., Kidney Cancer, Stage 1
Symptoms: Fatigue, abdominal discomfort, flank pain, constantly abnormal bloodwork
Treatment: Surgery (partial nephrectomy, ileostomy)
...
Bill P., Papillary Renal Cell Carcinoma, Stage 3, Type 1
Symptoms: Kidney stone, lower back pain, sore/stiff leg, deep vein thrombosis (DVT) blood clot
Treatment: Nephrectomy (surgical removal of kidney and ureter)
...
Laura E., Type 2 Kidney Cancer (Papillary Renal Cell Carcinoma), Stage 4
Symptoms: Profound fatigue, hypertension, high red blood cell count, severe back pain, badly swollen legs
Treatment: Chemotherapy (Cabometyx (cabozantinib) assigned under S1500 PAPMET clinical trial)
...
Nina N., Chromophome Renal Cell Carcinoma, Stage 2
Symptoms: Blood in urine, blood clots, intense abdominal pain
Treatment: Partial nephrectomy (surgical removal of right kidney)
...