Ciara’s Acute Lymphoblastic Leukemia Story
Ciara was diagnosed with acute lymphoblastic leukemia (ALL) at 24 years old after experiencing symptoms like fatigue and night sweats. She describes undergoing chemo, taking monoclonal antibody drug blinatumomab, and experiencing side effects.
Ciara shares how she navigated life with cancer, including what got her through the hardest times, managing the issue of fertility preservation, and how the leukemia diagnosis changed her life perspective (for the better!). Thank you for sharing your story, Ciara!

- Name: Ciara T.
- Diagnosis:
- Acute lymphoblastic leukemia (ALL)
- 24 years old
- Staging: N/A
- 1st Symptoms:
- Fatigue
- Shortness of breath
- Night sweats
- Petechiae
- Treatment:
- Chemotherapy
- Intrathecal rituximab, 8 treatments
- Vincristine, dexamethasone, & pegaspargase for ~3 months
- Monoclonal antibody drug
- Blincyto (blinatumomab)
- 5 rounds
- 4 weeks on, 2 weeks off
- 24/7 infusions
- Chemotherapy
- Diagnosis
- Chemotherapy Treatment
- Reflections and Quality of Life
- What was the hardest part of treatment for you?
- What helped you through the most stressful times?
- What were some practical ways that people supported you?
- Dealing with long commutes to treatment
- Was there a talk about fertility preservation?
- How do you handle the anxiety of potential relapse?
- How has cancer changed your life perspective?
- Advice for someone who has just been diagnosed
This interview has been edited for clarity. This is not medical advice. Please consult with your healthcare provider for treatment decisions.

It may take some time to get past the initial shock and grief, but once you get your footing, do things you enjoy again and just keep going.
Don’t let anyone tell you how to have cancer or how you should feel. It’s your journey, so be as open or closed as feels right, stand up for yourself in being your own advocate, and be bald, wear a wig or no wig.
It’s all up to you. Fight this disease and carry on in your journey on your own terms.
Ciara T.
Diagnosis
What were your first symptoms?
Hindsight is 20/20, I guess, because for about a month I was having all kinds of weird side effects. I didn’t realize it was all connected until I got the diagnosis.
I was very fatigued. I could sleep for 8 hours, wake up, and feel like I could sleep for 8 more. At the time, my husband and I were on the third floor of our apartment complex.
I was short of breath walking up to our apartment, and I was like, “Okay, I need to go back to the gym. I should not be this winded.”
I was a nanny, and I couldn’t finish a story without being short of breath. The fatigue and shortness of breath were definitely the biggest.
I was having some night sweats and really bad headaches for about a week before the diagnosis. I had a few nose bleeds. I had spots, which I came to find out was petechiae on my legs. Come to find out, it was all related.
How did you get diagnosed?
I had been feeling off for about a month, and then for about 5 days, I thought I had the flu or something. Friday, after work, I went to a MinuteClinic around the corner, figuring they would do a strep test or flu test to see what was going on.
Because I was complaining of chest problems like shortness of breath, they did an EKG and a chest X-ray.
They also did a bunch of blood work. They said it might take a couple of days to get the results, but they would call me when they knew something.
At 7:30 p.m. or so, I went home after getting the tests. I got a call at 10 a.m. the next morning from a different doctor.

He said, ‘You don’t know me, but as soon as you left last night, your doctor called me to consult.
After preliminary results came back, we think you have leukemia. You need to get to an emergency room.’
Processing a cancer diagnosis
I was just standing there doing dishes when he called. I was like, “Uh, what?” You never expect that you’re going to hear “cancer.”
We’d been living in Austin for about 9 months. I had so many questions because I didn’t know what hospital to go to, I didn’t know what to say when I got there, and I didn’t know if he was going to tell them I was coming.
He impressed upon me the seriousness of the situation. He said, ‘I need you to know this is serious. I don’t want to wait a few days. I need you to go right now.’
That freaked me out a bit, but it was good that he let me know it was serious.
»MORE: Patients share how they processed a cancer diagnosis

Did you go to the ER right away?
My husband took me to the hospital immediately. I grabbed electronics like phones, my laptop, and chargers. I didn’t pack a bag, though. I didn’t know. I didn’t know that I wouldn’t be back at my apartment for 2.5 months, but I wasn’t.
I went to Seton’s emergency room in Austin that day, and on that Monday, they transferred me down to MD Anderson in Houston.
Describe the bone marrow biopsy
They give you 2 different options. Before all of this, you could give me a Benadryl, and I would be knocked out. I don’t like to take more medicine than I need, so for the biopsies, I typically just get the local anesthetics.
I don’t like taking the anxiety medicine. I hate the feeling of not being in control of my body.
I like to have control, and I’m a very scheduled person. When I went to get the biopsy, I asked them, “Can you show me the tool you’re going to use?” I’m so glad I asked because it feels like a corkscrew is going into your bone. The tool is really pretty small, though.
They drill into your hip bone, stick a needle in, and they pull the marrow out. That doesn’t feel good. That’s a deep ache inside your bone. There’s nothing really for that, but it’s over in 15 minutes.
Chemotherapy Treatment
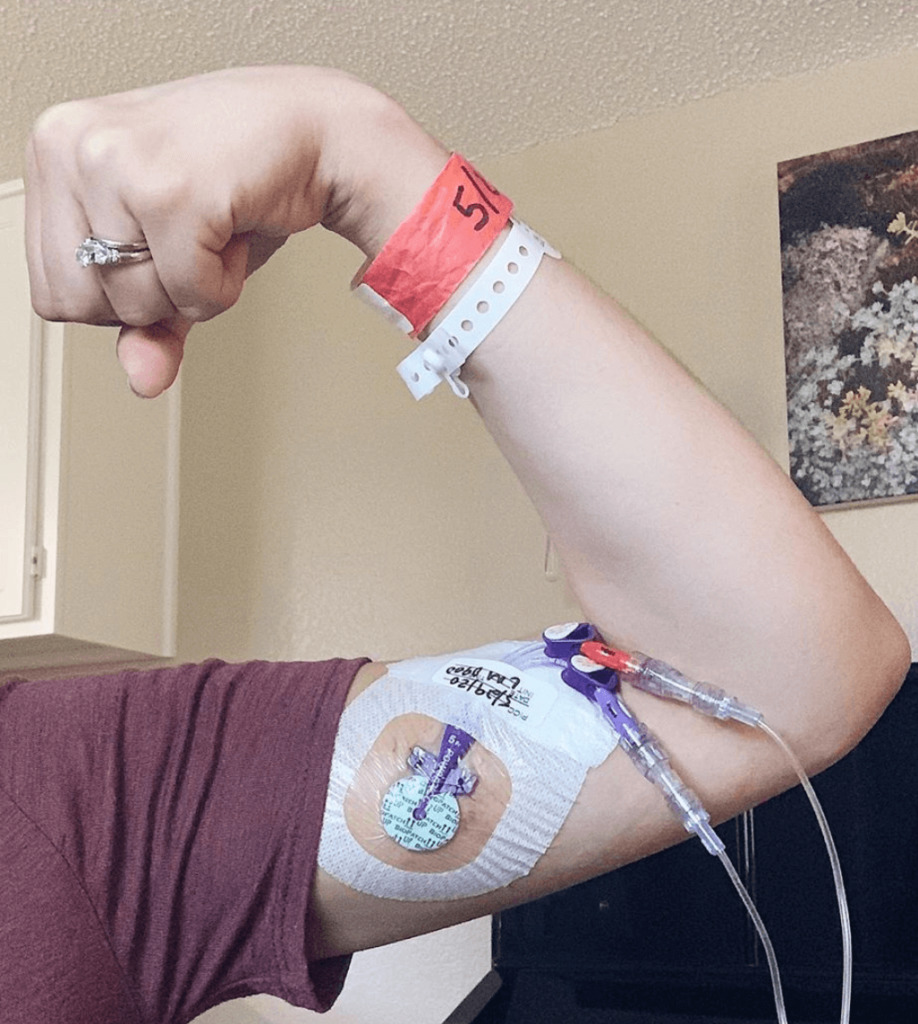
What was it like having a PICC line?
I wanted a port, but there’s a greater risk of infection with leukemia, so I needed a PICC line.
I had it for about 5 or 6 months, but my skin wasn’t healing underneath, so we had to move it to the other arm. It was raw and itchy, so they moved it.
It was just annoying. It would get snagged on everything. Especially with the Blincyto, I had a tether constantly attached to me.
»MORE: Read patient PICC line experiences
What was your chemo regimen?
The first 2 phases of my chemo, which was a cocktail of drugs and then an added fanny pack drug, lasted about 9 months.
I had 8 intrathecal chemo treatments of rituximab into my spinal column, and then 2 or 3 months of vincristine, dexamethasone, and pegaspargase.
I got infusions about 5 times in the first month. Once I achieved remission, it went to once every other week.
Blincyto drug (monoclonal antibody)
Then I started 5 rounds of Blincyto. That’s the fanny pack I had to wear and go get bag changes for every other day. Blincyto is typically used for relapsed patients, but my doctor felt like I had a greater chance of staying in remission if we did that since I was a pretty unconventional patient.
I did Blincyto 4 weeks on, 2 weeks off. It’s a continuous infusion for those 4 weeks.
Blincyto side effects
I had some super random side effects that would come and go. I didn’t see a rhyme or reason to them. I had fatigue, like most people do. I got moon face from the dexamethasone (steroid). There was some major swelling going on.
I had really bad bone pain during the winter. My doctor said it was probably a result of rituximab. It caused bone pain and muscle weakness.
I would be walking, and then all of a sudden I would be on the ground. I didn’t have very bad nausea, which was nice. I have more of that now on maintenance.
I’ve had a really bad chemo cough. That’s from the methotrexate I’m on now for maintenance. On the steroid, I get bad mood swings. I know it’s happening, and I can’t control it.
I never lost everything, but I did have a lot of hair loss. It was enough that I ended up shaving it super short. It was easier to manage that way, and it was less traumatic.
I’ve been very warm while going through chemo. Because of my meds and because I’ve been on the Depo shot, I had some night sweats.
»MORE: Cancer patients share their treatment side effects

Working toward remission
With ALL, the goal is to achieve remission within the first 30 days. After the first month, they did a bone marrow biopsy. They saw that I had minimal residual disease.
Just because you achieve remission doesn’t mean they can stop. My doctor told me that if we stopped when I achieved remission, my cancer would be back within a week.
I always knew we would keep hitting it for a while after.
Follow-up protocol
Now I have a bone marrow biopsy about every 6 months. If I have any funny feelings or if they see something’s not right, we’ll do one earlier, but so far I’ve stayed in remission.
What’s your maintenance chemo like?
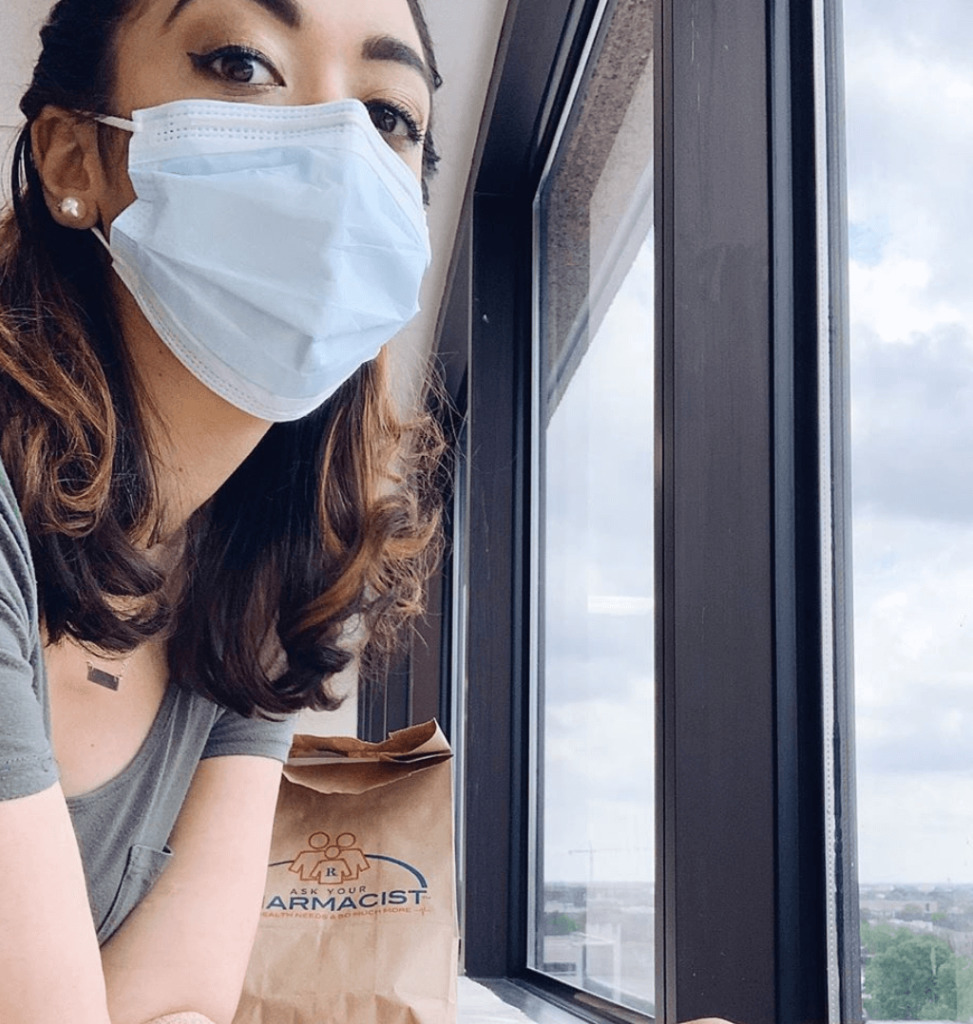
I’ve been going down to Houston once a month. I get blood work done, and I see my doctor.
I get IV chemo. After I finished the other 2 phases, I got my PICC line taken out. Since it’s just once-a-month chemo, I don’t need a port or PICC line anymore.
I get vincristine at my MD Anderson visit. I take mercaptopurine daily, methotrexate once a week, and the first five days of the month I take mass quantities of Prednisone.
About two months ago, they stopped my Vincristine. I was having some pain in my feet and hands, so we stopped.
Reflections and Quality of Life
What was the hardest part of treatment for you?
When I was having bad bone pain. It was Christmas week of 2017, so it was in the thick of my chemo. There was nothing I could do or take that would give me any sort of relief. I was in excruciating pain on the couch.
I couldn’t walk, hold a glass of water, or crack an egg. I was trying to be self-sufficient and make myself breakfast, and I couldn’t.
I tried Epsom salt bath, massages, medications that were prescribed, and nothing helped. That was the worst of it.
What helped you through the most stressful times?
My faith. My relationship with God and my family. My church has been so supportive. I’ve had some people really step up, and some people who have disappeared. It’s been really cool to see the people who are willing to step up.
My relationship with God has progressed, my relationship with my husband has progressed, and it makes me so proud to see how far we’ve come through this.
My husband and I were talking the other day, and we know if something horrible were to happen — like if we found out I wasn’t in remission — we could get through it. We’ve been through so much, and we’ve gained a new perspective from it.
What were some practical ways that people supported you?
We have a tendency to say, “Let me know if there’s anything I can do to help.” The majority of people are not going to actually let you know. It’s hard to ask.
Instead say, ‘Hey, I want to bring dinner over for you. What day works for you?’
That’s so much better. To specifically mention things that you are willing to do is so much better. I’ve very open about my appointments. I’m not one to be hush-hush about things because I know I need help.
»MORE: What kind of support cancer patients say helped the most
Dealing with long commutes to treatment
It was really hard. My husband had to drive back and forth from Austin to Houston for about 9 months.
Thankfully, my parents live in Katy, so I basically lived with them for 9 months. With my drugs, I was at the hospital every other day for 9 months.
I would stay with them, and my husband would work during the week and drive down on the weekends to be with me. His brother moved from Atlanta to help him with his business.
When I was first diagnosed, we had been married for a little over 4 years. I felt like we reverted to dating again.
I didn’t want to be living with my parents, I didn’t want to be sick, and I didn’t want to be away from him. That was a really hard time to not get to live together and only see each other a few days each week.
When I did get to go home back to Austin and only had to check in with MD Anderson once a month, it was hard reintroducing us being us again.

Was there a talk about fertility preservation?
Everything happened so quickly. From the time that I got the blood work, it took a week to start chemo. After they put my PICC line in, there was a conversation about it, but there wasn’t any time to do anything about it.
There wasn’t time to even think or talk about. That wasn’t really even an option for us. I don’t know if that’s the case for everyone, but it was for us.

I don’t think they said definitively whether I would be fertile still or not. It seems like we just don’t know. It’s up in the air.
The conversation basically went, “We don’t know if you’ll be able to have kids or not after all this, but just know that it can affect fertility.”
That’s been a very big deal to us. We have tough conversations about that even to this day.
If I wouldn’t have gotten diagnosed when I did, we would most likely have a baby right now. We were getting really close to starting a family around the diagnosis.
I was and still am really angry because that was taken away from us. It’s potentially forever, but at least for many years. That decision was made for us, and that’s frustrating beyond belief.
It stresses my husband out when we talk about it because he wonders what would happen if we did wind up having a kid, then my cancer comes back, and he’s left with a kid by himself.
We’re always carrying the beast of relapse in our minds, so it’s a hard topic to think about either way.
»MORE: Fertility preservation and cancer treatment
How do you handle the anxiety of potential relapse?
Right now, I don’t. I’m still going through chemo, so I feel like when I finish, it’s going to be a big deal. On one hand, I’m so excited to not have to go get maintenance chemo once a month anymore, but I also know that there’s going to be so much more emotional work to get done after I finish.
I’m going to have to deal with the idea of relapse. At that point, I have to figure out what my life will be like again. For the past few years, my life has been cancer treatment. I know how to do that.
When I stop, everything will change. I’m no longer actively fighting the cancer at that point, and I just have to have faith that it worked and it worked long-term.
How has cancer changed your life perspective?
I find the positives. The key to getting through this has been integration. I have to find things that bring joy, and I hold on to those. I’m also more open with people and how I’m feeling. I’ll continue that practice for the rest of my life.
One of the biggest revelations I’ve had has been that I don’t need to force relationships. We all have a limited amount of time. We have work and all these responsibilities.
To spend our free time on people who aren’t invested in your life and don’t really care isn’t worth it.
There are plenty of people who want to have a relationship that want to be around me and be my friend, so I focus on them.
You can’t force family and friends to be close to you, so I’ve learned to let go. I don’t focus on the things I don’t have. I focus on the blessings that I do have.

Advice for someone who has just been diagnosed
With ALL, it’s going to be a long journey, but don’t put your life on hold. It will be hard and take up a lot of your time and energy, but don’t stop traveling, eating the foods you like, or spending time with the people you love.
Don’t stop living your life and say, ‘I can’t wait for this to be over.’ Don’t shut your life down while you wait for this experience to end. Continue to do things you love.
Is your energy level different? Sure. You might not be able to do everything you loved the way you could before you got sick, but you can still do them. Rest when you need to, but keep living.

It may take some time to get past the initial shock and grief, but once you get your footing, do things you enjoy again and just keep going.
Don’t let anyone tell you how to have cancer or how you should feel. It’s your journey, so be as open or closed as feels right, stand up for yourself in being your own advocate, and be bald, wear a wig or no wig.
It’s all up to you. Fight this disease and carry on in your journey on your own terms.

Inspired by Ciara's story?
Share your story, too!
Acute Lymphoblastic Leukemia (ALL) Stories
Lauren M., T-Cell Acute Lymphoblastic Leukemia (T-ALL)
Symptoms: High fever, trouble breathing while lying flat, bad cough, headaches
Treatments: Chemotherapy, radiation, lumbar puncture
Christine M., Acute Lymphoblastic Leukemia (ALL)
Symptoms: Enlarged lymph nodes, pain in abdomen, nausea
Treatments: Chemotherapy, bone marrow transplant
Lauren J., Acute Lymphoblastic Leukemia (ALL)
Symptoms: Extreme fatigue, easily bruised
Treatments: Chemo pills, chemotherapy, spinal taps, total body radiation, bone marrow transplant
Renata R., B-Cell Acute Lymphoblastic Leukemia, Philadelphia chromosome-positive (Ph+ALL)
Symptoms: Fatigue, shortness of breath, nausea, fevers, night sweats
Treatments: Immunotherapy, chemotherapy, TKI, stem cell transplant (tentative)



