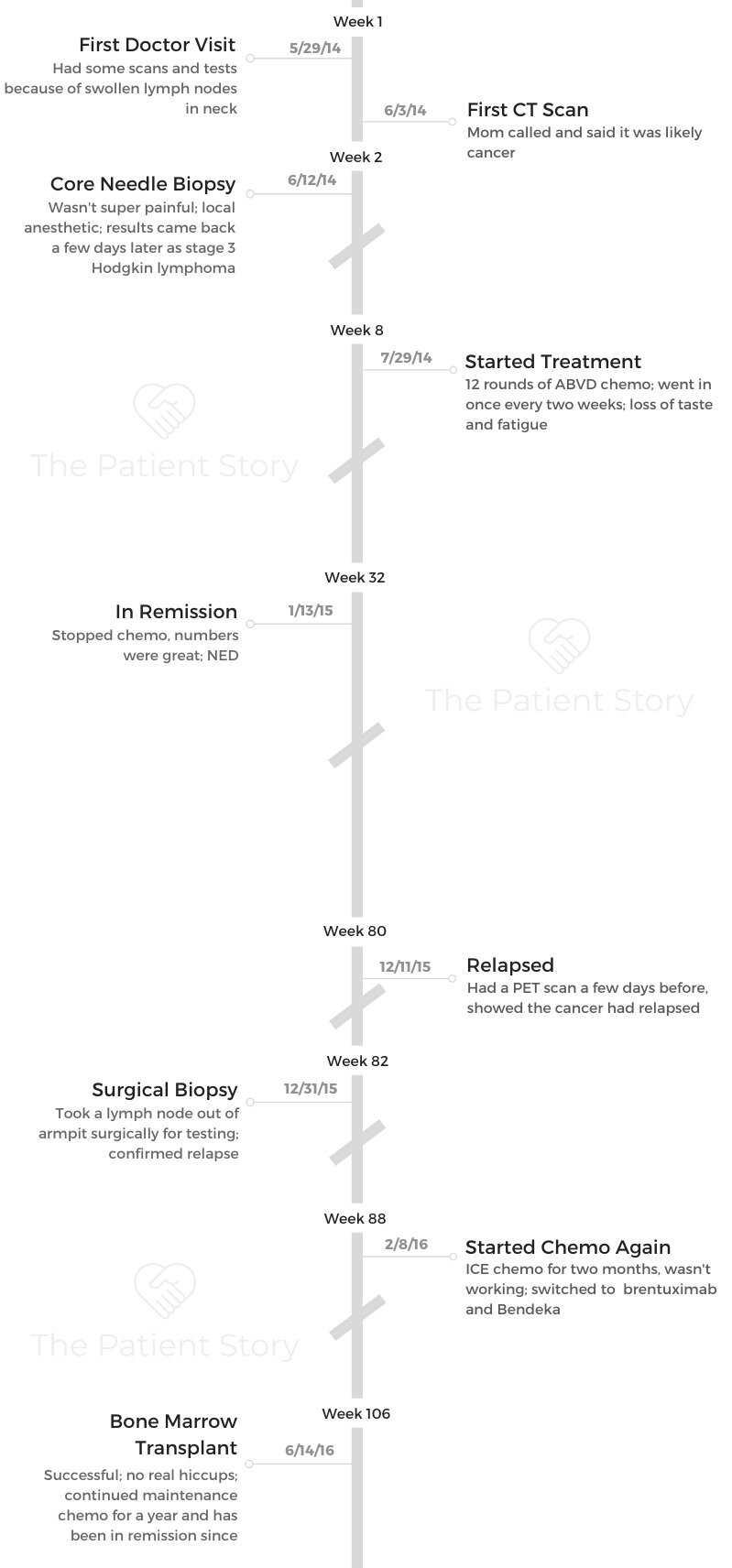
Tylere’s Stage 3 Relapsed Classical Hodgkin’s Lymphoma Story
Tylere shares his stage 3 Hodgkin’s lymphoma story, undergoing ABVD chemo and then suffering a relapse. He was able to get into remission after more chemo, immunotherapy and a bone marrow transplant.
Explore below for more on how he also navigated life with cancer, fertility preservation and the kind of support he needed during treatment.

- Name: Tylere P.
- Diagnosis:
- Classical
- Staging: 3, Relapse
- Age at diagnosis: 24
- 1st Symptoms:
- Swollen lymph nodes in neck
- 1st-Line Treatment:
- Chemotherapy
- 12 rounds of ABVD
- Chemotherapy
- 2nd-Line Treatment:
- Chemotherapy:
- 2 rounds of ICE
- ifosfamide
- carboplatin
- etoposide
- Bendeka (bendamustine)
- 2 rounds of ICE
- Targeted therapy
- Brentuximab
- Bone marrow transplant
- Chemotherapy:
This interview has been edited for clarity. This is not medical advice. Please consult with your healthcare provider for treatment decisions.
One thing is when I finished maintenance chemo, people would say, ‘You’re done with chemo, so you’re done with cancer!’
No, I’m not. I have a hard time saying I’m a survivor. I still have a check-up every 6 months, and the fear is always still there. I’m thriving after cancer, and I prefer the term “thriver” over survivor. I guess they kind of mean the same thing, but I like it better.
Tylere P.
Diagnosis
What were the first signs something was wrong?
I noticed I had swollen lymph nodes on the left side of my neck. My mom is a nurse practitioner, so I showed her when I was visiting one weekend.
I asked if we could go get it checked out. I asked her what it could be, and she said I could have some type of infection — or worst-case scenario, that it could be some kind of cancer. I was like, “Oh. Okay.”
We went to the doctor. They gave me some antibiotics, but the swelling didn’t go down even after a week of that.
Then I had a CT scan, and my mom was actually the one who told me first that she thought I had some form of cancer.
Lymph node biopsy
I was referred to the University of Michigan. They did a biopsy on one of the lymph nodes. That’s when it came back.
I had it biopsied and then had all these other types of tests to confirm that it was cancer and not some type of allergic reaction or infection.
The first biopsy I had was a core needle biopsy in my neck. I had one biopsy in my neck where they just went in with a needle, and I had another one where they used local anesthetic and actually pulled out some of the lymph nodes. That was a weird experience.
He was like, “You wanna see it?”
It looked like a white jelly bean. They just put a band-aid on the place where they took the sample from, and I was good to go.
When I relapsed later, I had a biopsy under my arm. That one was surgical. I had been under general anesthesia before, so I wasn’t super nervous.
When you’re going in for a biopsy, just make sure you follow the doctor’s instructions. Don’t overthink it. I think they told me not to eat for a while before. Just follow all those types of directions.
When you’re there, you’re probably going to be there for a while because of all the paperwork and getting checked in. That’s where some of the nerves can really kick in.
It’s really not a big deal, though. I remember being in the operating room for the surgical biopsy.
It was pretty much just the best sleep of my life. That’s about it.
Processing the diagnosis
I honestly think I blocked that out. I just remember the phone call from my mom saying she thought I had cancer.
Once I got diagnosed, I was just worried about the next steps. I just had meeting after meeting and test after test. I was just going through the motions.
»MORE: Processing a cancer diagnosis
1st-Line Treatment
Getting a port
That was another moment when I went under. Not a big deal. The first few days after getting the port placed is weird, though. I was very aware that it was there.
About a month or so later, I didn’t even realize it was there anymore. It became a part of me. It was probably weirder to get it removed than it was to get it placed.
ABVD chemotherapy regimen
My first time on chemo was 12 rounds of ABVD chemo. I went in once every 2 weeks. I did blood work and had my port flushed on weeks I didn’t have chemo.
My white blood cell count was too low a few times, so we had to delay chemo a bit and do some Neulasta shots.

ABVD side effects
The chemo regimen was pretty easy. It didn’t have too much of an effect on me.
I was prepared for vomiting and being sick all the time. I was ready for my hair to all fall out right away, but it didn’t fall out until the second month or so.
I lost my taste — or it changed, at least. Water had a metallic taste and was the most disgusting thing ever. Ice cream was terrible, too.
I found some fruity drinks, and those were good because they didn’t just taste like chemo.
Other than that, I was just really tired for a day or so after chemo. I didn’t really get nauseous or anything like that. My mom would drive about 3 hours to come stay with me after infusions.
Halfway through the treatments, I started to feel bad because I felt like she wanted me to be sick so she could take care of me, but I wasn’t feeling sick.
I think she wanted me to, but I didn’t really need her because I tolerated everything well.
Relapse and 2nd-Line Treatment
When did you find out you had relapsed?
I got a scan during chemo to check everything out. About 2 days after starting chemo in January, my lymph nodes went down.
After finishing chemo, I had a scan a few weeks later, and everything still looked good. Then I got one every 3 months after that.
The December after finishing chemo, that’s when they told me it was back. I kind of felt like something was up. I had a swollen lymph node under my arm, so I was anxious to get it checked.

At that point, I was almost a year out of treatment. I had been getting back into being active and living my normal life. I was getting excited with what I was going to do with work, and everything changed because I relapsed.
Relapse was definitely harder than the first time. The first time around, [the diagnosis] was new and almost exciting.
I’m someone who likes to be challenged, so I was just ready to figure the process out.
They had told me chemo was going to be so hard, and I was like, “Is it really?” I just wanted to see if it was going to live up to the hype. For the most part, it didn’t.
I’m happy about that, but I was also like, “Aw, man. I feel like I missed out on the cancer experience in some ways.” I’m also really happy I didn’t struggle through that chemo, though, don’t get me wrong.
The second time around, I felt like, “Well, damn. What now?” It sounded way more serious and aggressive, and it was a bummer for sure.
Describe the 2nd-line chemotherapy (ICE)
My surgical biopsy results came back sometime in January. I started my new chemo the first week of February.
That was ICE (ifosfamide, carboplatin, etoposide) chemo. That required a 3-day hospital stay. I would get it infused twice a day. I did that once a month for 2 months.
They weren’t happy with how little my numbers had dropped, so we had to change up my regimen.
The new one was brentuximab and Bendeka. According to all the billing, those were very expensive drugs.
I didn’t have any side effects with those 2 drugs.
My hair still grew. It was a quick infusion. It started working, and they were happy with the results. Then it was time for a bone marrow transplant.
Bone Marrow Transplant
What was the preparation for the bone marrow transplant?
I donated my own marrow. That made it easier. They told me all the terrible things that could happen with the transplant, but it actually went pretty smoothly, too.
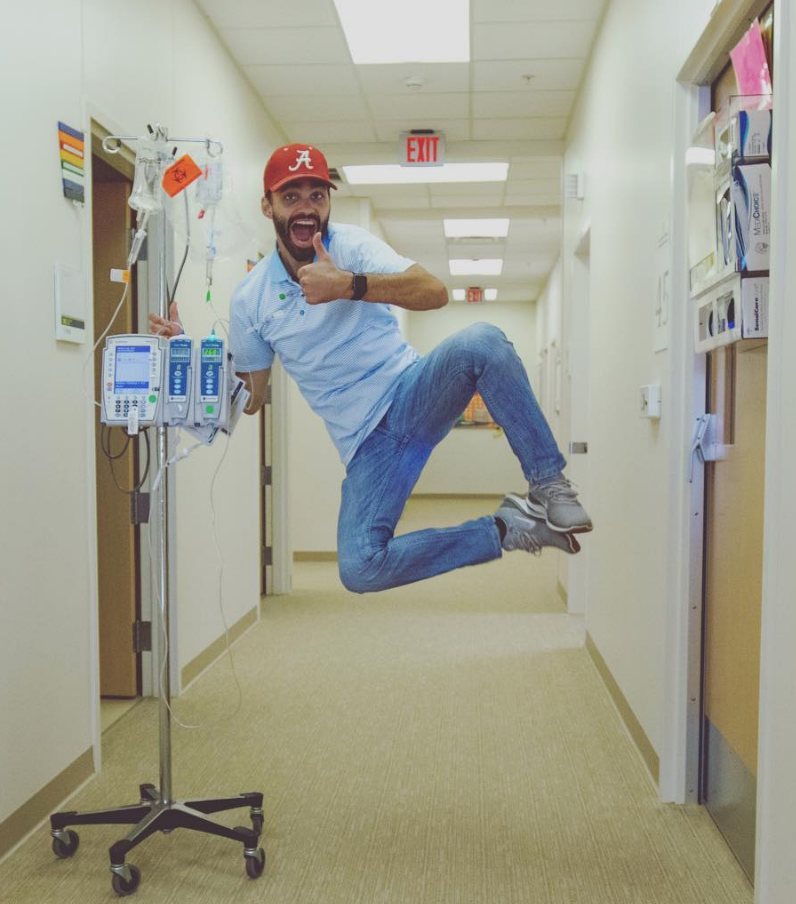
They wanted me to be active while I was in the hospital and get up and walk around.
For the week before the transplant, I got some really high-octane chemo. It basically destroyed everything in my body. I would walk for 20 to 30 minutes a day during that point.
Side effects of the chemo before transplant
There were a couple of days I was constipated, but that’s about it. My temperature was rising a little bit after the hardcore chemo, and we had to watch that, but it never got so high it was scary.

Describe the bone marrow transplant
The collection is pretty cool. When they take your blood out, you’re sitting in this room for like 4 hours.
There’s a big metal rod for one arm, and it’s taking blood, so you can’t use that arm.
Then in your other arm, it’s putting the blood back in, but it spins out all the cells it needs before giving the blood back to you.
What was the transplant itself like?
When you get it back in, it looks like everything has just been on dry ice for however long. They put in a PICC line.
I didn’t use my port for anything bone marrow transplant related. They just push the cells back in your body through your line.
Apparently, for the next few days, you and your room smell like creamed corn. I couldn’t smell it, but my room just had this odor.
I felt bad for anyone who came in, but it went away for a few days.
Recovering from the BMT
12 days after the transplant, I could take handfuls of hair out. Aside from that and losing a ton of weight in the hospital, I didn’t really have any side effects.
I probably lost about 20 or 30 pounds in those 3 weeks I was in the hospital.
I could ride in a car, but I couldn’t drive for 10 days. I couldn’t be outside in direct sunlight. I had to wear pants, long sleeves, hats and lots of sunscreen. For 100 days, I couldn’t drink tap or well water. I had to drink bottled water.
Maintenance chemo protocol
I had to get maintenance chemo once every 3 weeks for a year after the transplant. That was just the brentuximab.
The worst part of that chemo wasn’t even the drug itself. It was the Benadryl. I would just drive myself, and they wouldn’t let me go home until that wore off. I asked if I had to have it, and I didn’t, so we stopped that.
Either going into the transplant or afterwards, a doctor mentioned remission to me. Essentially, I was in remission during the transplant. Then I had to do the maintenance chemo just to make sure.

Survivorship
Transitioning back into everyday life
This summer will be 3 years since my last chemo. They gave me a certificate at my last treatment, and I rang the bell.
That was kind of it. It was like, “Okay. Now what do I do?”
I started my own business right before the chemo for the bone marrow transplant, actually. I started a business doing photography and videography.
That’s been my life for the last 4 years. I’m not sure if many people start a business while they’re going through chemo, but that’s what I did.
I didn’t know if I was going to be able to work during any of this. I didn’t know if I should apply for other jobs. I didn’t want to have to deal with any of that.
It was easier to start my own thing with odds and ends here and there, and it turned into something a little bigger and better. Now that’s what I get to do all the time.
One thing is when I finished maintenance chemo, people would say, “You’re done with chemo, so you’re done with cancer!”
No, I’m not. I have a hard time saying I’m a survivor. I still have a check-up every 6 months, and the fear is always still there. I’m thriving after cancer, and I prefer the term “thriver” over survivor. I guess they kind of mean the same thing, but I like it better.
It’s just strange to have a life-defining moment that lasts for years and then to have it just be over.
Dealing with the fear and anxiety that comes with survivorship
For me, faith plays a big part in that. I trust that what’s going to happen is going to happen. There’s only so much I can do and control. I try to focus on the things I have control over.
That’s something that this cancer experience has taught me. I don’t have to stress out about the things I can’t control.
In college, I was big into leadership stuff. I listened to a lot of motivational speeches and things. My biggest takeaway from all of that was that the main thing we can control is our attitude towards things.
Even when I was diagnosed, that’s why I was like, “Okay. Cool.” I could’ve asked “Why me?” or any of those questions, but it just wasn’t worth it.
I acknowledge those bad thoughts when they come, but then I choose not to dwell on them and move on instead.
Mental and emotional side effects of cancer
I never had any terrible breakdowns. If I was bummed sometimes, I would just be bummed. I’d say, “You’re not going to get anything done today. That’s okay.”
I would just sleep all day and rest up for the next day, when I hopefully felt better.
I felt like I wasn’t doing enough a lot of times. I feel like life kind of went on pause. I saw my friends getting married and having kids, and I was living in my parents’ basement.
That wasn’t anything I had any control over. That’s the situation I was in, and I just had to recognize the bad days.
Even now, if there’s a day when I know I have stuff to do, but I’m going to struggle through it and not be productive anyway, I’ll just take the day and chalk it up to a personal day.
Reflections
How can loved ones support the patient?
As the patient, you can set boundaries and tell people how you want to be supported. One thing I would like to see more people do is say, “This sucks. I’m sorry this is something you’re having to deal with. It’s terrible.”
Rather than saying, “Hey, we’re thinking of you.” That’s more validating. Then ask if there’s anything you can do to help.
You don’t want to put the onus on the patient to ask for help, so you can offer ways you can help and see if they take them. In my experience, it was easier to just communicate those needs I had.
People would say, “We’ll send you food or whatever you need.” I don’t like a lot of clutter and things, so I was like, “I don’t want anything like that.”
It’s a hard thing to say no to people, but you can set boundaries. The easiest way to support someone is to just ask, “How can I best support you?”
Maybe it depends on your love languages.
Can you talk about hair loss?
The first time, it definitely sucked. When I found out I was gonna lose it, I had been trying to grow my hair out and was pretty pumped about it.
I just had to accept it. I probably held onto it for a week longer than I should have.
I decided to shave it, and we had this whole big thing with friends. We videoed me shaving it, and a lot of them shaved their heads, too. That was super fun.

That first shower or 2 I took after shaving my head was crazy. I realized there was a whole process I didn’t have to go through anymore. It was a bit colder in the shower, but I was also in there for less time.
The second time, I vlogged the whole experience, pretty much. I wanted to show people what going through it was like, and to show that I could still be a normal person.
It was something I could point to when people asked me questions as well. That way I didn’t have to keep answering the same questions over and over again.
By the third time, I was actually kind of excited. The first 2 times, I buzzed it. The third time, I was literally able to just pull it out. It was coming off so easily.
People don’t have to shave their head with you. They can just be there for you. Let’s say you don’t have that kind of support, and you’re doing it by yourself.
Still, throw a party for yourself when you go to shave it.
Make it fun. The whole experience sucks, so finding fun in it was the best thing I could’ve done. Laugh through the pain. That makes it a little easier.
»MORE: Dealing with hair loss during cancer treatment
Financial toxicity: paying for cancer treatment
Dealing with health insurance was probably more stressful than dealing with any of the chemo.
Leading into the bone marrow transplant and everything else, I was still on my previous employer’s health insurance. I kept that through COBRA because everything was already pre-approved.
I was also on Medicaid for the next year to do the maintenance chemo and scans. That was hard because I could only make so much money in order to stay on this insurance plan. It made it hard to grow my business.
I got a denial for one of the chemo treatments. That’s the only real reason I know how much it costs. Insurance still denied it, even though my doctors appealed the first denial.
I didn’t hear anything for a few months, so I thought it was taken care of, but then I got another bill. I asked how I ended up with this bill.
The hospital’s response was, “Remember when you came in here at the beginning and were super stressed out and anxious and dealing with a cancer diagnosis, and you signed all those forms accepting financial responsibility in case insurance didn’t cover something?”
I was just like, “Sure. I don’t understand how this works.” What if I didn’t want that chemo had I known this could happen? I was trusting the doctors and hospital staff to get all that approved and taken care of before giving me the treatments.
I appealed the decision again. I had to do a bunch of stuff. I don’t understand why I, as the cancer patient, had to be doing all this.
Finally, the financial services office at the hospital took care of it. Being low-income had its advantages.
Advice for others on dealing with cancer payments
I got a 3-ring binder and would put everything financial- and insurance-related in there by date.
All of a sudden, you start receiving bills, explanations of benefits and all that. I wish I would’ve gotten the binder sooner.
Fertility preservation
I don’t remember how it was brought up, but I think it was my first meeting with the doctors. Either my mom or the doctors asked me.
I was like, “Obviously, it’d be nice to have kids one day, and I’d like them to be mine.”
I did the whole preservation thing. I had a sample frozen. That’s also expensive to store. It’s about $900 a year just to store it.
That’s already going to be a pretty expensive kid. I’m glad I did it, though, because I’ve talked to people who didn’t, and now they’re bummed that they don’t have the option.
»MORE: Fertility preservation and cancer treatment
Message for someone who has just been diagnosed
Try to be a light everywhere you go, especially at the hospital. Try not to be [rude] to your nurses and doctors. They’re there to help you.
Unless you’re living in some weird universe where they’re not. Then I would find new doctors. Hospitals are already a dark place. Just try to be a light.

Ask questions, but don’t act like you know more than the doctor or nurse because you saw something online. If you did see or hear something, you can bring it up. Just don’t be rude.
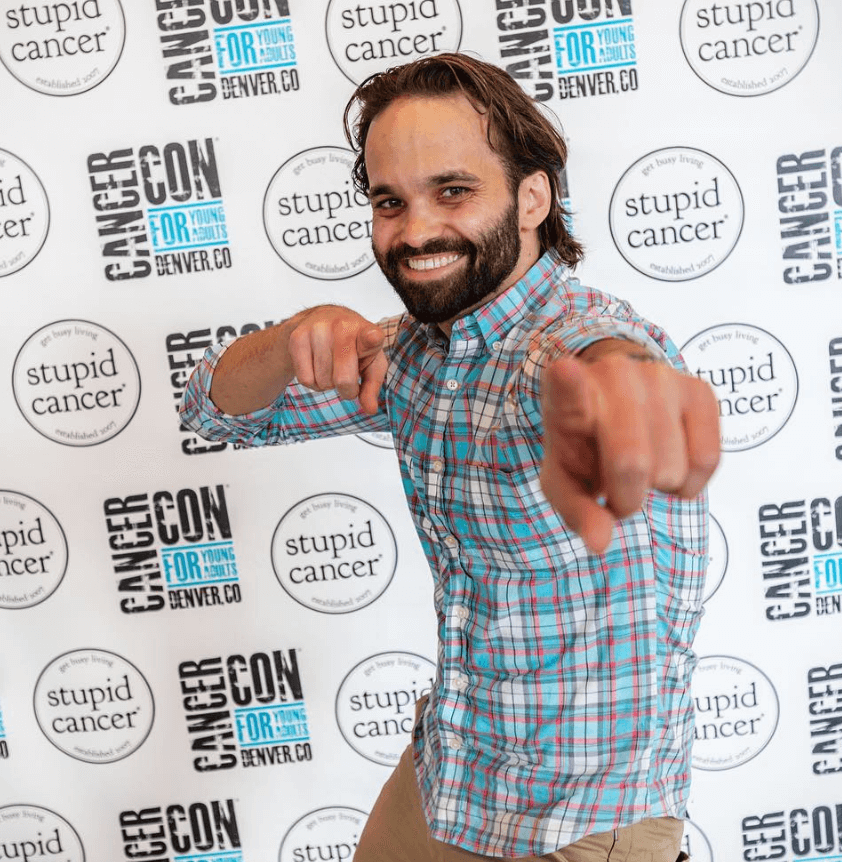
There’s the organization Stupid Cancer, and they put on CancerCon. I went last year, and that was the coolest thing. It was a room full of people who have experienced a lot of the same things that you have.
Wash your hands. Literally just become really good at washing your hands. Get really good at washing your hands.
Even through chemo, I traveled a lot. I asked if I needed to wear a mask, and they were like, “Oh, those don’t do anything. Just wash your hands.”
Also, maybe find a hobby. For me, that was learning to sew. I would watch Netflix and sew.
That was a good time killer, and it was a good way to keep my mind busy.
A lot of it is just embracing what you’re going through. Keep some normalcy.

Inspired by Tylere's story?
Share your story, too!
Hodgkin’s Lymphoma Stories
Jessica H., Hodgkin’s Lymphoma, Stage 2
Symptom: Recurring red lump on the leg (painful, swollen, hot to touch)
Treatment: Chemotherapy
Riley G., Hodgkin’s, Stage 4
Symptoms: • Severe back pain, night sweats, difficulty breathing after alcohol consumption, low energy, intense itching
Treatment: Chemotherapy (ABVD)
Amanda P., Hodgkin’s, Stage 4
Symptoms: Intense itching (no rash), bruising from scratching, fever, swollen lymph node near the hip, severe fatigue, back pain, pallor
Treatments: Chemotherapy (A+AVD), Neulasta





