Callie’s Stage 2B, Grade 2, IDC, ER+ Breast Cancer Story
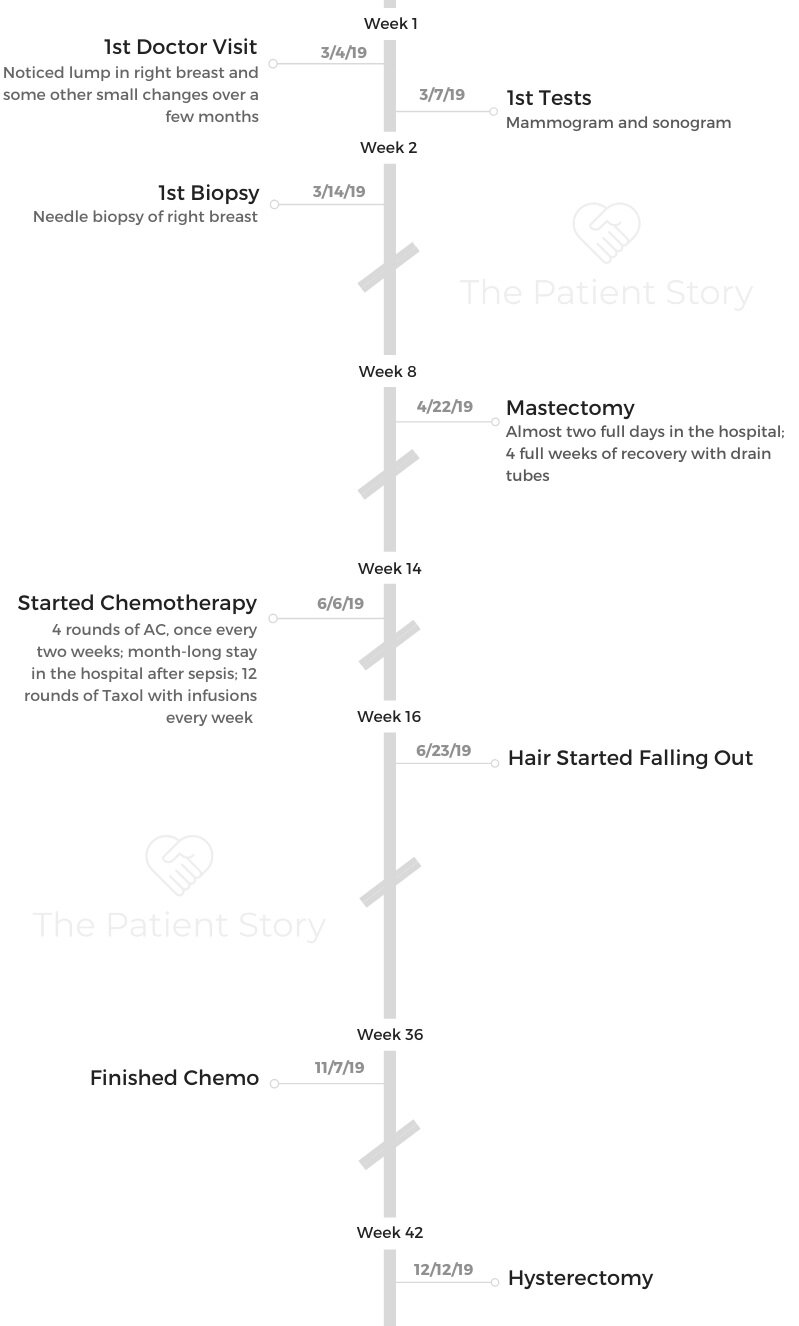
Callie shares her stage 2B ER+ breast cancer story, detailing her mastectomy and chemotherapy.
In her story, she highlights how she was able to mentally and emotionally process diagnosis and treatment, managing through hair loss, and how her children dealt with the cancer experience.

- Name: Callie M.
- Diagnosis (DX):
- Breast cancer
- Invasive ductal carcinoma in right breast, ER+
- Age at DX: 38 years old
- Staging: 2B, grade 2
- 1st Symptoms:
- Breast changes
- Dimpling at top of right breast
- Lump found
- Treatment:
- Surgery
- Mastectomy
- Hysterectomy
- Reconstruction
- Chemotherapy
- ACT– Adriamycin, Cytoxan (cyclophosphamide) & Taxol
- 4 rounds (8 weeks) of AC; 12 weeks of Taxol
- ACT– Adriamycin, Cytoxan (cyclophosphamide) & Taxol
- Surgery
This interview has been edited for clarity. This is not medical advice. Please consult with your healthcare provider for treatment decisions.

We laughed a lot. We found joy in moments.
At one point, Logan (my oldest son) found my fake boob in my car. He held it up and goes, ‘What’s this?’ I was like, ‘It’s my fake boob, son.’ He was like, ‘Oh my God, oh my God, oh my God!’
It was like a hot potato. There were moments like that, and they were just funny. Stuff like that was a byproduct of the cancer, but we have to laugh about it.
Callie M.
Diagnosis
How did you know that something was wrong?
4 months before I was diagnosed, I noticed a little change in my breast. The top part had dimpled just a little bit. It was really minor. You really wouldn’t have noticed it unless you knew.
My husband had said something to the effect of needing to keep an eye on it because it could be a bad sign.
I brushed it off because I was young, and I had a lot of experience with cysts in my breasts. They had never come back as anything. I wasn’t super concerned about it.
My husband worked nights at that time, so it had been a significant amount of time since we had gotten ready to go somewhere for a date.

We went on vacation for our anniversary. While we were on vacation, I was getting out of the shower in our hotel room, and my husband looked over. He’s an RN. He said, “Oh my gosh, that has changed a lot.”
I had noticed it, but I wasn’t super worried about it. He freaked out, though. He looked at it really close.
We noticed there was a bulge underneath the dimpling. He was scared about it. He didn’t think it was a cyst.
We went to the doctor, and I knew there was something wrong when my primary care saw it. She didn’t say anything, but she said she needed to get me scheduled for a mammogram and ultrasound as soon as possible.
I could tell by the way she was looking at me that she thought it was cancer right away.
When I went to get the mammogram 2 days later, the radiologist came in and looked at everything with the technician.
I knew that meant there was something they were looking at. He said, “I need to talk to you after you get dressed.”
How did you get the diagnosis?
He came in and said, “Your mammogram was a category 5.” I didn’t even know they categorized them. Category 1 would be totally normal and shows nothing of concern, and a 5 is very rarely given.
That means they can see the cancer on the mammogram. He showed me a picture of the mammogram and said, ‘See these white dots? This is highly suspicious of cancer.’
He got me scheduled for a biopsy a week later.
What was the needle biopsy like?
It was weird because my tumor was big for a breast cancer tumor. You could actually see it with your naked eye because of the way my breast bulged.
When they went in with the needle, it bruised really bad. They go in with a tool to mark where they’ve pulled tissue out, and it sounds like a staple gun. It was so weird. I had a little bit of a freak-out hearing that clicking sound.
How did you react to your diagnosis?
I had always been very aware of my breasts. My maternal grandmother died of breast cancer at 35. My mom was 10. My mother has never had any issues, but I’ve always had abnormal results of some kind.
Ever since about age 28, I get flagged for a mammogram. I’ve always felt like I had weird breasts that produced cysts. I had really dense breast tissue.
It was probably not as far of a jump for me as it would’ve been for someone without that family or medical history.
It was kind of a process for me. My dad passed away in 2016 from lung cancer. I was very involved in his process from diagnosis to treatment.
I had kind of been in this cancer bubble a year before. My first reaction was, “Here we go again.” I also had a little disbelief. I was only 38.
I called my mom. Then I called my stepmom because I knew that of all the people, she had been on the journey with me with my dad. She knew that I knew this journey was going to be difficult.
»MORE: Patients share how they processed a cancer diagnosis

Mastectomy
What was the prep for the mastectomy like?
I met with my surgeon, and he told me my tumor was very large for a breast cancer tumor. He told me I had options, but you could tell he thought the mastectomy was really the only way to go.
He said he just felt like we needed to get it out before it progressed any further. We decided to do the surgery so I wouldn’t have to do radiation.
When I got to the hospital, I met with my surgeon. I was nervous. I hadn’t even met my oncologist or nurse navigator yet.
I had a bunch of questions I wanted to ask and didn’t have anyone to ask yet. I was super nervous because I had never had a major surgery like that.
Describe the mastectomy recovery
I spent 1 night and almost 2 full days at the hospital in recovery. It took me 4 full weeks at home to recover from the surgery. I had drain tubes in the whole time. It took the full month of May. The recovery was pretty long.
The mastectomy process totally knocked me on my butt. To me, it felt like major surgery. I really had a hard time recovering from how bad it hurt.
I was exhausted all the time. I think a lot of that was mindset because I was still in my ‘I have cancer’ bubble.
I have lymphedema from them removing lymph nodes. It’s not horrible, but it’s something I do have to take into consideration in my life.
I did physical therapy for the whole month of June just about. I have limitations in my mobility. It’s so amazing what you use your arm for that you don’t realize until you can’t.
Chemotherapy
What was your chemo regimen?
My regimen was ACT: Adriamycin, cyclophosphamide (Cytoxan), and Taxol. I did Adriamycin and Cytoxan together for 4 rounds at 2 weeks apart from early June until the end of August or so. Those were hard because they caused a lot of nausea and vomiting.
Adriamycin is also called the “red devil.” It wipes you out for sure. I lost my hair and eyelashes. Then in August, I had a month-long period where I couldn’t get chemo because I went septic.
They think I had a bladder infection, and I had no white blood cells hardly because of the chemo. The antibiotic they gave me to fight the infection caused me to crash.
My kidneys started to shut down. There was a week or so where it was really bad. It was scary.
I was being monitored constantly. I had to get a blood transfusion. My blood numbers went really wonky. They would fix something, and then that would cause something else to go wrong.
Then I had 12 weeks straight of Taxol. I went in every week, but it wasn’t as serious. It made me really tired, but it didn’t wipe me out like Adriamycin. The fatigue was pretty bad.
What side effects did you experience?
Nausea, vomiting, fatigue, and chemo brain. I definitely had some continuation of thought issues. I was very scattered. I think that was a result of the chemo, because the further I’ve gotten from that, the better that’s gotten.
My nurses were really proactive about preventing mouth sores at the cancer center. I didn’t have any issues with that, thankfully. I did have some dryness issues, though, in my nose, mouth, and pretty much everywhere.
I was constantly putting on lotion, using lubricant in my nose to stop the nose bleeds, and my mouth is still pretty dry to this day.
One of the big side effects you can get is neuropathy in your hands and feet. I wore these cold gloves and socks during infusions, and I never experienced any there.
I did have some neuropathy in my legs, but it was nothing like I’ve heard other people describe.
»MORE: Cancer patients share their treatment side effects
Have you started the reconstruction process?
I was really nervous about the reconstruction. I met with the plastic surgeon. It’s a 3-part surgery. The first part of the process is putting in the expander so they can put the implant in to recreate the breast you lost.
When he first told me, it sounded like no big deal. When I met with him again right before, he said it was going to be similar to my mastectomy. I felt like the mastectomy knocked me on my butt.
I had my first surgery on January 31st, 2019, and it hasn’t been too bad. I would say the pain was as bad as the mastectomy, but the recovery didn’t last as long. They reopened the whole mastectomy scar to put the expander in. It was pretty major.
Starting in a few weeks, he’ll go in and start putting fluid in. It’ll take him about 2 or 3 months to get to the goal amount. I’ll go in every 2 or 3 weeks to get some fluid added.
Then in May, I’ll have the second surgery, where he’ll actually go in and put the implant in. I’ll get one on both sides so they look the same.
In September, he’ll go in and fix the area at the top of my right breast that is sunken in from where they took so much tissue.

Reflections
How did you mentally and emotionally process the cancer experience?
For me, it was a really big deal to get everything done by the end of 2019. I had been really excited because 2018 was not a really good year for me.
When 2019 came around, I was like, “This is my year!” Then I got diagnosed with cancer, and I thought, “Okay, maybe it’s not my year.”
It was really important for me to have everything done by 2020 because I just wanted a firm stopping point.
I was glad I had my hysterectomy in December. I was done with everything that was directly treating the cancer by the end of 2019.
Then I had a moment when I was sad that I wasn’t done with my reconstruction already. My really good friend had the best way of putting it. I was really bummed about it.
She said, “You know what, Callie? You’re rebuilding in 2020.” That really stuck with me and helped me. This is my year of rebuilding.
It’s not just about getting back to the way I was, but I’m becoming better.
I’m going and getting my yoga certification and my reiki healing certification. I’ve gotten into restorative yoga so I can help other people with cancer. I’m getting back to Callie, but I think it’s a better Callie than before.
How did cancer affect your relationship with your husband?
It certainly tested it. It was hard on him because he had to pick up the slack for me. I couldn’t cook and clean. Over time, you could tell he was ready for me to start feeling better.
»MORE: Read different experiences of a cancer diagnosis and treatment

We came out of it stronger because you have to appreciate each other in a whole new way. He was really supportive.
Can you talk about hair loss?
That was probably one of the roughest things for me. I had gotten my second AC treatment. We had gone to Dallas to buy stuff at market for the bookstore I own. I wasn’t going to miss it.
We rented a motor scooter for me to take so I didn’t have to walk. I was so sick. I knew where every bathroom and trash can was in that place.
We were on our way home, going down the highway, and all of a sudden, it was like my hair just released. I felt it. It was the strangest thing I’ve ever felt.
Sure enough, I run my fingers through my hair, and it just starts flaking off. It was falling out, but it didn’t all come out.
»MORE: Patients describe dealing with hair loss during cancer treatment
I was trying to keep this brave face, but then the next morning I went to wash my hair, and it was coming out in clumps. I knew this was coming.
I had prepared. I had cut it short. Still, I bawled like a baby. You know it’s coming and you think you’re prepared, but it doesn’t sink in until it happens.
I called my hairdresser, and she shaved it for me. She did a mohawk first. It was awesome to have fun with it, but the hair loss was probably the most emotional thing for me.
How did your kids handle your cancer diagnosis?
My oldest son has autism. He was 16 when I was diagnosed, so he’s 17 now. The first thing I did was call both my sons’ therapists. They’re a husband and wife team, and one sees each of my sons.
I met with them and asked if they would help me with Ben and Logan. I wasn’t sure if Logan would understand because of his autism.
My dad had just died of lung cancer, so the only reference they had of cancer was someone dying. It was really important to me that they understood I was not going to die. I had a 95% chance of surviving.
Logan’s therapist and I told him together. At one point, he said, “I understand that my mom has cancer, and that’s not okay, but I understand.” That was a big deal for him.
He never went to any of the chemo appointments or anything with me, but he would ask, “How’s your cancer today?” He hated when my hair fell out. He did not like my bald head and would voice that.
Ben was 14 when I was diagnosed and is 15 now. He went to chemo school with me. He went to one of my appointments with me. It was important for me to make sure that he knew it wasn’t scary. His school counselor admitted to me that every time I went to chemo, Ben would go to see her.
It affected him. It made our relationship a lot better, though, actually. He realized his mom was human. For a teenage boy, he loves his momma and wants to spend time with me.
As a family, it made us value family time more.
»MORE: Parents describe how they handled cancer with their kids
What advice do you have for someone who has just been diagnosed?
Cancer is a head game. That is really overlooked. That was one component of my treatment that I wished was emphasized more.
The way I dealt with it mentally and emotionally affected the way I went through it physically.

Make sure you are supported on the emotional and mental side. You could always tell when people were in a good place or not in the infusion center.
We laughed a lot. We found joys in moments. At one point, Logan (my oldest son) found my fake boob in my car. He held it up and goes, “What’s this?” I was like, “It’s my fake boob, son.”
He was like, “Oh my God, oh my God, oh my God!” It was like a hot potato. There were moments like that, and they were just funny.
Stuff like that was a byproduct of the cancer, but we have to laugh about it.
Just focus on today and what today brings. Don’t worry about next week’s chemo treatment or the reconstruction process.
Even though that’s your treatment plan at the beginning, it might not be your treatment plan later. You have to learn to roll with what’s going on.
Be kind to yourself. Some days, you’re not going to be a superhero. Some days, you’re not going to take on the world, and that’s okay.
Be kind to other people because you truly never know what they’re going through.
There were so many times when I was bald, and people would come up to me and say, “Are you going through treatment? I’ve been in remission for 5 years,” or something like that.
It’s like a club you get to be a part of. People are so willing to share with you that there is hope on the other side.

Inspired by Callie's story?
Share your story, too!
Invasive Ductal Carcinoma Stories
Amelia L., IDC, Stage 1, ER/PR+, HER2-
Symptom: Lump found during self breast exam
Treatments: TC chemotherapy; lumpectomy, double mastectomy, reconstruction; Tamoxifen
Rachel Y., IDC, Stage 1B
Symptoms: None; caught by delayed mammogram
Treatments: Double mastectomy, neoadjuvant chemotherapy, hormone therapy Tamoxifen
Rach D., IDC, Stage 2, Triple Positive
Symptom: Lump in right breast
Treatments: Neoadjuvant chemotherapy, double mastectomy, targeted therapy, hormone therapy
Caitlin J., IDC, Stage 2B, ER/PR+
Symptom: Lump found on breast
Treatments: Lumpectomy, AC/T chemotherapy, radiation, hormone therapy (Lupron & Anastrozole)
Joy R., IDC, Stage 2, Triple Negative
Symptom: Lump in breast
Treatments: Chemotherapy, double mastectomy, hysterectomy




