Joy’s Stage 2, Grade 3, IDC, BRCA1+, Triple-Negative Breast Cancer Story
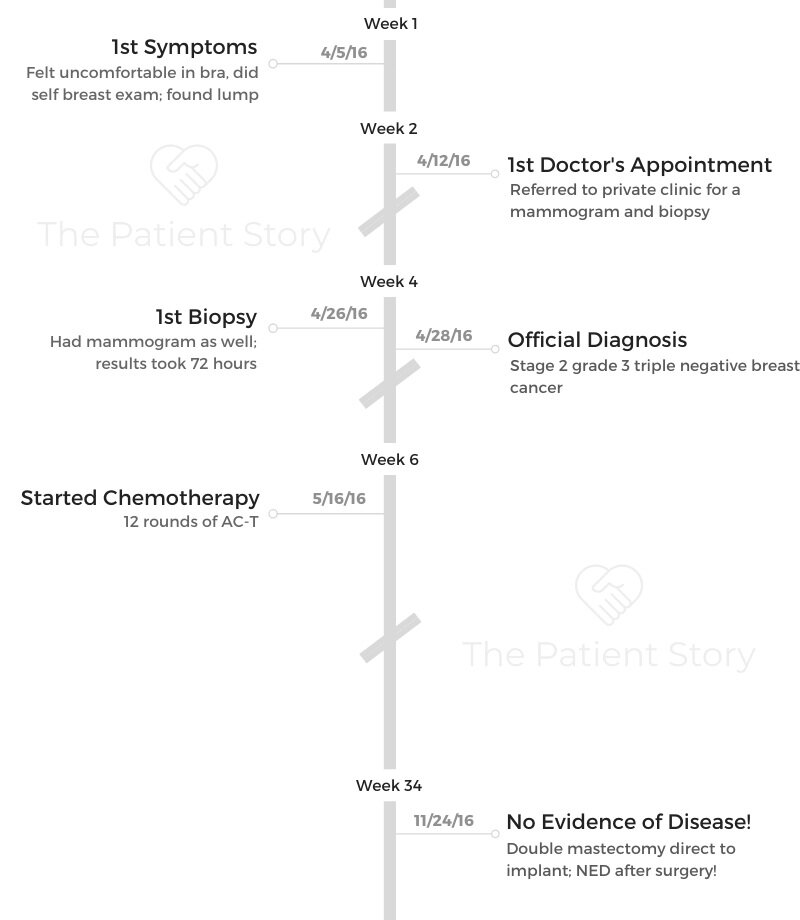
Joy shares her stage 2 triple-negative breast cancer (TNBC) story and how testing positive for the BRCA1 genetic mutation altered her treatment path, including chemotherapy, a double mastectomy, and hysterectomy.
In her story, she also highlights dealing with scanxiety post-treatment, how cancer impacted her marriage, and the way she handled the diagnosis with her children.

- Name: Joy R.
- Diagnosis:
- Breast cancer
- Triple negative
- Invasive ductal carcinoma (IDC)
- BRCA1+
- Staging: 2
- Grade: 3
- Age at DX: 35 years old
- 1st Symptoms:
- Discomfort in bra
- Found lump
- Treatment:
- Chemotherapy
- 12 rounds of AC-T
- Adriamycin, Cytoxan, Taxol
- Surgery
- Double mastectomy direct to implant
- Hysterectomy
- Chemotherapy
On my first day of chemo, my friend called me and said she wanted to wish me congratulations.
I was like, ‘For what?’ She said, ‘You’re taking your first step on the road to recovery.’ I loved that.
Breathe and know you’re on your road to recovery.
Joy R.
This interview has been edited for clarity. This is not medical advice. Please consult with your healthcare provider for treatment decisions.
Diagnosis
Finding a lump
I had started doing breast checks because a friend of mine was diagnosed a year before. She was still going through chemo and all that, so I started doing checks on myself.
One day, I was feeling kind of uncomfortable. I thought my underwire had gotten messed up or something. I came home, and I checked. I found a lump and panicked. I showed my husband.
We both agreed that I check enough that it shouldn’t be something serious.
I called my friend, and I called my doctor. I went in, and sure enough, it was a very fast-growing cancer.

What happened at the first appointment?
I made an appointment with my family doctor. The year before, I had a breast reduction.
My doctor said that maybe it was just scar tissue. It probably wouldn’t pop up that late after surgery, but it was still a possibility.
If I was going to try to get in with the hospital, it was going to take about 3 weeks to get an appointment. If I wanted to, though, there was a private clinic we could pay for and get into right away to get checked out.
My family doctor gave us a referral and wanted me to get it checked. She was on the fence about it and what it might be.
I went to the private clinic, and I went alone because no one really thought it was anything. They started with an ultrasound, and from that, he was pretty confident that it was breast cancer.
Then we did a mammogram and biopsy. I was texting my husband and friend in between all of this.
They said they would call me in 72 hours with the results of the biopsy, but he was pretty confident it was breast cancer.
Sure enough, he called me 72 hours later with the news.
Describe the biopsy
It looked like a hole puncher. They put a little bit of topical anesthetic. It felt like a piercing almost. They took samples from 2 different spots because he wanted to make absolutely certain.
They had to cover it and put pressure on it, and I went home bandaged.
Waiting for the results was hard. I wasn’t really eating or sleeping.
»MORE: Dealing with scanxiety and waiting for results
Treatment Decisions
How did you decide where to go for treatment?
I decided to go to the hospital instead of sticking with the private clinic. My friend who had already gone through breast cancer told me, “If you want, this is my oncologist. I’ve already done all the research. Here’s the information.”
My doctor at the clinic transferred all the files over to the hospital, and within days, the hospital called me. I had the appointment with oncology pretty quickly.
He started scheduling a bunch of tests to make sure I was healthy enough to go through chemo. It was a week straight of tests.
How did you find out your treatment plan?
First, I met with the oncological surgeon, and then I met with my oncologist. When I met with the surgeon, I was kind of hoping that because my lump was so localized, I would just need a lumpectomy.
He said because I was triple positive, he wanted to start with chemo in the hopes that it would shrink enough to make my surgery a minor one.
Because it was so fast-growing, he was afraid that if we started with surgery, there would still be leftover cancer cells in my body.
I was devastated, of course, when I found out I needed chemo. My first thought was losing my hair.

He said we would do 16 rounds of chemotherapy and then surgery after about a month break. During that time, we also did genetic testing.
Throughout my chemo, we found out that I had the BRCA1 gene mutation. Doing a lumpectomy came off the table, and we would do a double mastectomy and hysterectomy.
What was the genetic testing process like?
They asked me a few questions about my family tree. There had been no history of cancer in my family. Other than that, it was blood tests.
They said they would get back with me in a few weeks with results, and they came back positive for BRCA1.
»MORE: Read our interview with a genetic counselor
Chemotherapy
What was your chemo like?
I had 12 weekly treatments. Then we switched drugs, and I was supposed to have another 4 treatments of that drug. It was supposed to be every 2 weeks at that point.
I ended up getting an allergic reaction to that chemo, though, and everything paused because I had to stay in the hospital.
My doctor had to go to the chemo board because he didn’t know what to do. He said I needed the drug even though I was having a bad reaction to it. It’s the one that every breast cancer patient gets, basically.
What they did was give me a smaller dose of it over a longer period of time. We did it once every 3 weeks instead of once every 2. I made it through all 4, but I was very sick from it.
During the first 12 treatments, I was pretty tired. I had some nausea. Once I changed drugs, I was very sick. I had pieces of my tongue and gums fall off. I couldn’t speak. That was so scary.
What side effects did you experience?
Even during the chemo I tolerated well, I still had to delay treatment a few times for my numbers to come up. We couldn’t control my nausea.
I had every anti-nausea drug known to man, and we still couldn’t control it. Other than that and feeling rundown, the first 12 weeks were okay.
When I had my last 4 treatments, I was not functioning. I was literally a picture-perfect version of the worst chemo patient you can imagine. I was emaciated and curled in a ball. It wrecked me.
For the first 12 weeks, my hair thinned, but I didn’t lose it all. When we switched drugs, everything was gone. I lost my eyelashes and my eyebrows, too. I was so sick, and I looked so sick.
How did you deal with chemo mentally and emotionally?
It was really hard. We had a countdown for when it would be done. I started speaking with a psychiatrist. We have kids at home, so I had to just focus on that end date and make it. I just went into survival mode at that point.

Surgery
What do you remember of going into the mastectomy?
I ended up getting 6 weeks in between chemo and surgery because I was so beat up from treatment. The morning of the surgery is when everything really hit me.
Through chemo, I was just fighting through it that I didn’t process anything. That morning, I thought, ‘I can’t believe I have cancer. I can’t believe I’m about to cut my breasts off my body.’
It was a hard morning.
My plastic surgeon was the same one who had done my breast reduction. Originally, the oncological surgeon was supposed to start, and the plastic surgeon would come in to do reconstruction later, because it was a 5- or 6-hour surgery all together with reconstruction.
The significance of having a doctor you trusted
I asked my plastic surgeon if he could be present when I was being put to sleep, though, because he’s almost a comfort to me. He’s someone who knew me before I was sick.
He did show up, and I was crying so hard. He took me in his arms, and he said, “You’re going to be okay. You’re going to wake up. Let’s just get this behind us.” He was joking, too, and he said, “You’re going to wake up with a brand new set of boobs!”
As I was falling asleep on the table, I couldn’t stop shaking and crying. He came next to me and ran his hands through my hair.
I stared at him as I fell asleep. He was trying to calm me down and put me at ease, so as I fell asleep, he was trying to comfort me.
What do you remember of waking up from surgery?
There was a nurse next to me when I woke up. I asked her, “What time is it? Was he able to go directly to implant?”
She said yes. Then I asked if my port was removed during my surgery. I really wanted it out. She said they were also able to do that, too.
I was in pain and a little bit of nausea, but I was glad it was done. Honestly, it wasn’t as painful as waking up from my reduction.
Since I had the reduction done, I was able to keep my nipples because they weren’t connected to anything. They were just there for show. There was no fear of spreading to them.
With the reduction, there was pain in my nipples and bleeding from them that would stick to the bandages, and there wasn’t anything of that with the mastectomy.
It was easier to handle. I had drains, which was definitely uncomfortable, but that didn’t last forever and was manageable.
What was the recovery from surgery like?
I’m an extremely stubborn human being. I slept in the hospital overnight. The next morning, they came in to check on me and see if I could be released.
The resident came in, and I was in the bathroom brushing my teeth. He was like, “What are you doing? You can’t get out of bed by yourself!”
I was like, “Well, I wanted to brush my teeth. I have buttons that move the bed up and down.”
My husband and I both work in the medical field, so there was nothing they could do for us in the hospital that we couldn’t do ourselves. I wanted to be home. I wanted to be in my own bed. I wanted to be with my kids.
They released me. For the next few days, we just had someone with me. We had full-time babysitters for me basically. I was very stubborn with that. I would still get out of bed and do things.

I wanted to go back to work as soon as possible as well. My surgery was in November, and I went back to work in January. Since I had 6 months of chemo, my oncologist said I needed 6 months of recovery.
He was not very happy with me, but sitting at home wasn’t going to be healing for me.
I needed to get back to work and my life. That’s what was most healing for me. It was a struggle to go back to work, and I was tired and achy. I still very much wasn’t myself, but I enjoyed being back in my routine.
»MORE: Read more on how others dealt with work after a cancer diagnosis
Describe the hysterectomy
That happened in June, so that was 6 months later. It was a joke compared to everything else, honestly. I wanted it done by my gynecologist. I asked if he could do it.
They said they wanted the gynecological oncologist to do it, but I pushed for it. They jokingly said, “Okay, if he can fit you into his schedule.” I texted him, and he said of course he would do it.
He’s a very funny and sarcastic person. I love him. He’s the coolest person. Going into it, I was joking about it with him. I was like, “I’m never gonna get my period again? Let’s do it! I’m all for it!”
I was so nonchalant about it. My gynecologist walked in and said, ‘Alright, let’s get you into menopause,’ and I was like, ‘Woohoo!’
Afterwards, I was bloated because he did it laparoscopically, but I’ve been bloated before. I was just like, “Okay. No more period. No more cancer concerns.”
It was so not a thing for me.
Did treatment put you into menopause?
I didn’t really have menopause symptoms after the surgery. I had those symptoms during chemo. My period had only come back once in between chemo and the hysterectomy. I don’t think my body ever came out of that menopause from chemo.
I had some hot flashes after surgery a little, I guess. The bulk of my symptoms were during chemo, though. Again, the hysterectomy was not a big deal for me.
What is your follow-up protocol like?
They said I had no evidence of disease (NED) and that I just needed to be monitored closely for 5 years. I was seeing my oncologist every 3 months, and at my last appointment, he just bumped it to every 6 months.
I’m a little nervous about that because I like seeing him. It calms me to go in and see him. My oncologist is amazing, and we run into each other all the time. I know if I have questions or concerns, I can reach out. He answers my emails in minutes. He’s great.
Reflections
Do you still deal with scanxiety?
I do have anxiety in between scans. I take very good care of my body. I’m not a smoker. Before cancer, I would work out literally 6 days a week.
I was in the best shape of my life. For me to get cancer, my big thing is, it can happen to anyone. I know it’s cliche, but it’s true. If I can get cancer, anyone can.
If it happened to me, I think, “Maybe it’ll happen to me again?” At work, there’s a carpet at my desk. It had gotten wet and had some water damage. I said, “Oh no, this needs to come out immediately. The last thing I need is mold and to get secondary lung cancer.”
I don’t cut my hair because I don’t know if I’m going to lose it again. My mother thinks I’m morbid, but I’m just being realistic.
I know I’m not immune to a secondary cancer. It happens to people. It can happen to me.
I’m not a hypochondriac, but at the same time, I wonder if things are cancer-related.
The scans, blood tests, and even just seeing my oncologist gives me peace. It calms me down and grounds me. I only start to feel nervous once I’ve gotten some distance from a scan.
»MORE: Dealing with scanxiety and waiting for results

Can you talk about your support system?
The biggest thing for me was people helping my husband out. My son’s best friend’s mom organized a meal train for us.
It would come from strangers even. It was so beautiful.
My husband is a director of emergency services and is pretty much always on call, so for him to be at every chemo with me, I noticed he was getting a little antsy and short-tempered.
We started a schedule of different people who could take me to chemo. My in-laws took me, my parents took me, and my best friend went with me like 3 times.
My parents live 2 blocks from us, and our kids have bedrooms at their house, so they could go stay with them if they needed to or if we thought they were getting sick.
My parents really took on that role with my kids. My mother-in-law works from home, so she was able to be flexible and help out a lot.
Everyone around us would offer to pick up groceries or anything we needed. Everyone was so helpful.
They all said it was time for us to learn how to accept help, because we’re always helping everyone else.
»MORE: What kind of support cancer patients say helped the most
Describe the hair loss
Hair loss was horrible. It was the worst part of everything for me. I’m somewhat of a vain person, I guess. I wasn’t okay with losing my hair.
I was not someone who was comfortable walking around bald or with just a hat. Nobody saw me without a wig on.
The day I was hospitalized from my allergic reaction, I went to the hospital wearing just a hat and no makeup.
My oncologist knew it was serious because you’ll never see me without nail polish on, without makeup on, or without my hair done. It was horrible.
I cut it and donated it, and then I let it fall out. I was not okay shaving it.
»MORE: Patients describe dealing with hair loss during cancer treatment

How did cancer affect your relationship with your husband?
It’s funny because if you speak to my husband and you speak to me, it’s 2 different stories. I’m a huge control freak, so for me, in my mind, I feel like I was still very involved with everything.
My kids or my husband will make a comment about something, and I’ll be like, “When did that happen?” They’ll say, “Well, you were sick.”
My husband cried the first time I put on my wig. My family was in survival mode with us.
I was always nauseous, so I wasn’t eating very much. If it was 3 in the morning and I wanted McDonald’s, my husband would get up and go because he wanted me to eat.
We had a Christmas party, and some friends made a cake for me with a cancer ribbon on it. My husband made a speech, and he broke down.
»MORE: 3 Things To Remember If Your Spouse/Partner Is Diagnosed With Cancer
Parenting with cancer
It was horrible. We’re very snuggly. My kids were little. My daughter was 7, and my son was 3, turning 4.
They very much needed mommy and snuggles, and the fact that I couldn’t kiss them without the fear of getting sick was really hard.
I was as honest as possible with my daughter. She came once to a blood test. She walked around the chemo floor with me. She became a spokesperson or cheerleader, and that was so special. To this day, she’s so positive about it.
»MORE: Parents describe how they handled cancer with their kids

What advice do you have for someone who has just been diagnosed?
What my friend told me was, “Just breathe.”
You’re going to be fine. You’re going to go through a bad time, you’ll get through it, and you’ll have stories to tell.
On my first day of chemo, she called me and said she wanted to wish me congratulations.
I was like, “For what?” She said, “You’re taking your first step on the road to recovery.” I loved that.
Breathe, and know you’re on your road to recovery.

Inspired by Joy’s story?
Share your story, too!
Invasive Ductal Carcinoma Stories
Amelia L., IDC, Stage 1, ER/PR+, HER2-
Symptom: Lump found during self breast exam
Treatments: TC chemotherapy; lumpectomy, double mastectomy, reconstruction; Tamoxifen
Rachel Y., IDC, Stage 1B
Symptoms: None; caught by delayed mammogram
Treatments: Double mastectomy, neoadjuvant chemotherapy, hormone therapy Tamoxifen
Rach D., IDC, Stage 2, Triple Positive
Symptom: Lump in right breast
Treatments: Neoadjuvant chemotherapy, double mastectomy, targeted therapy, hormone therapy
Caitlin J., IDC, Stage 2B, ER/PR+
Symptom: Lump found on breast
Treatments: Lumpectomy, AC/T chemotherapy, radiation, hormone therapy (Lupron & Anastrozole)
Joy R., IDC, Stage 2, Triple Negative
Symptom: Lump in breast
Treatments: Chemotherapy, double mastectomy, hysterectomy




One reply on “Joy’s Stage 2, Grade 3, IDC, BRCA1+, Triple-Negative Breast Cancer Story”
Thank you for your stories!! I’m about to begin and needed some real experiences.
You’ve helped me❤️