Stephanie’s Stage 3 PMBCL Non-Hodgkin’s Lymphoma Story
Stephanie Chuang was diagnosed with stage 3 non-Hodgkin’s lymphoma, primary mediastinal b-cell lymphoma (PMBCL) subtype with double expressors. She describes undergoing IVF to preserve fertility options before going through 6 cycles of chemotherapy, as well as experiencing hair loss and what support was most helpful.
- Name: Stephanie Chuang
- Age when diagnosed: 31
- Diagnosis:
- Non-Hodgkin’s Lymphoma
- Diffuse large B-cell, then determined more likely primary mediastinal large B-cell
- Stage 3
- Double expressors (can complicate the prognosis, usually doesn’t affect 1st-line treatment decisions)
- Symptoms:
- Swollen neck/jaw area because tumor was pressing up against artery that drops blood into the heart (superior vena cava)
- Fatigue
- Infrequent but guttural cough (once or twice in the morning)
- Misdiagnosis: Mono
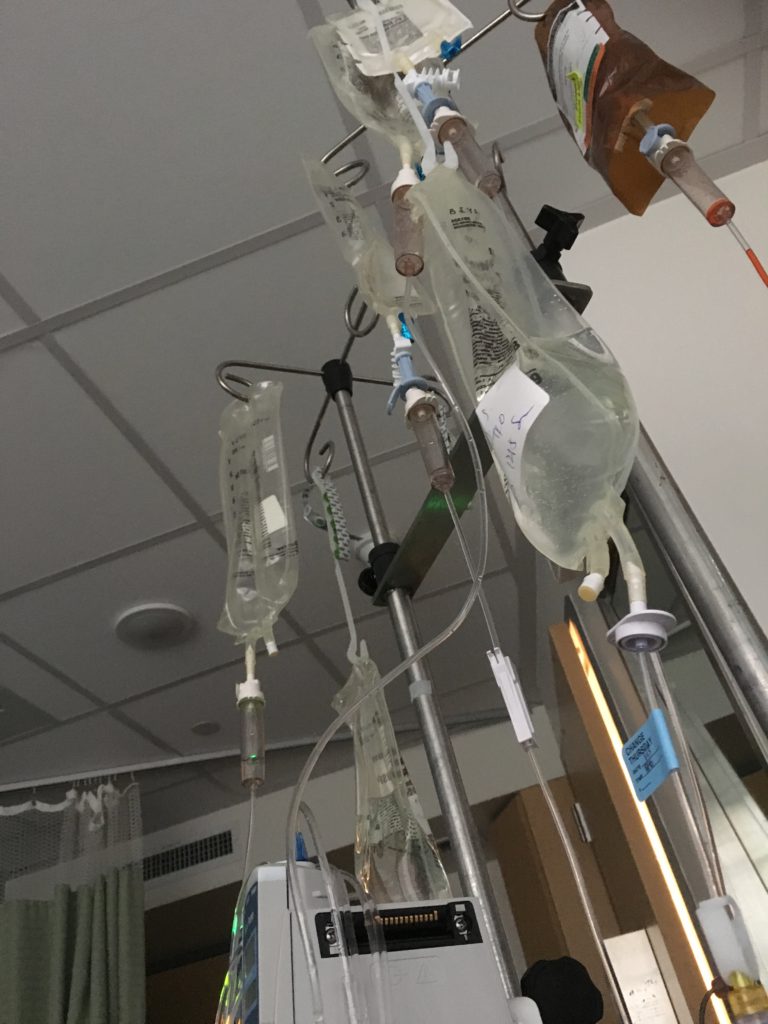
- Treatment:
- Chemotherapy: R-EPOCH (dose-adjusted)
- 6 cycles, each cycle = 3 weeks
- Week 1: continuous infusion through PICC line (arm) or port (chest) for 24 hours, lasting 5-6 days
- Week 2: side effects tend to kick in, ranging from nausea to mouth sores
- Week 3: typically the healing week when blood cell counts recover
- NOTE: If your white blood cell count (WBC) doesn’t rebound back into the standard range, your next chemo cycle may be delayed.
- Outpatient: driving in each day to get the chemo bag changed, wearing a small pump (in a bag) at home instead of inpatient, where you get the infusion and stay overnight at the hospital

- Diagnosis
- What were the first symptoms and red flags?
- How did you get diagnosed?
- Gene testing
- Describe each test and biopsy you experienced
- Nasal passage
- Excisional lymph node biopsy
- PET and CT scan
- Bone marrow biopsy
- How did you choose hospitals?
- Did you go to a smaller or biggest hospital? What did you like about it?
- How was your medical team?
- Did you get a port or PICC line?
- How was the PICC line?
- How was the port?
- Chemotherapy & Side Effects
- What treatment regimen did you undergo?
- Describe in detail what happened each cycle
- What was Cycle 1 of chemo like?
- Did the chemo cycles get better or worse?
- What were the side effects of chemo, and what helped prevent them?
- Anything you wish your doctor would have told you to help you prevent them?
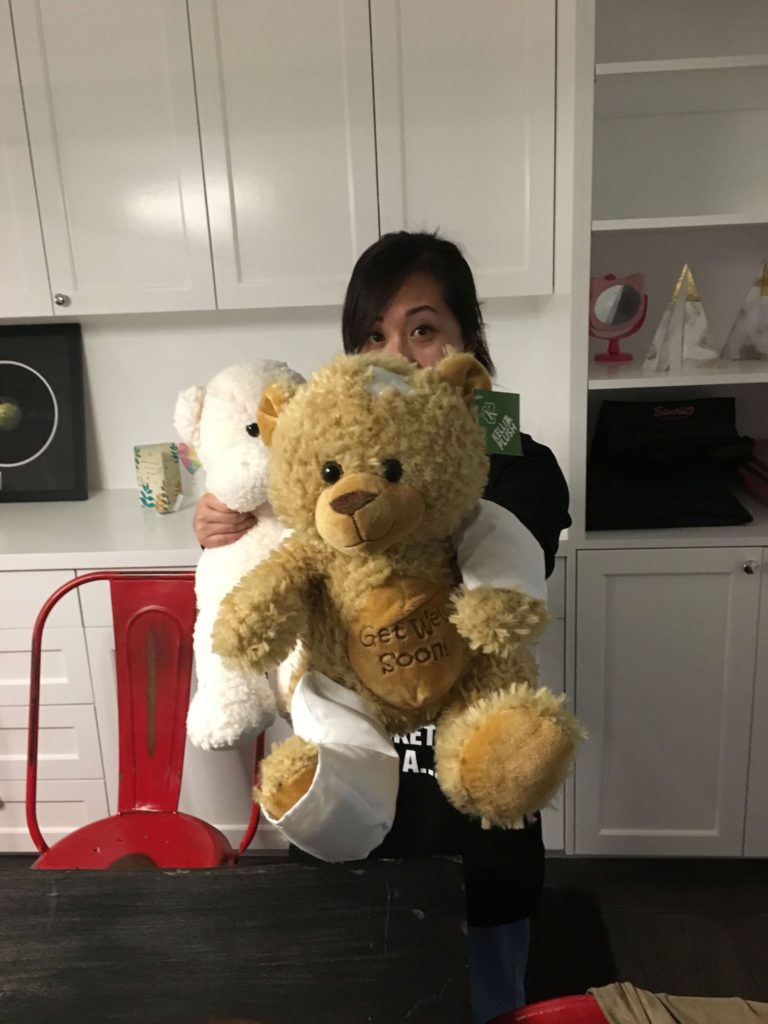
- Hair loss from chemo
- Were you surprised by your reaction to losing hair?
- What helped with the hair loss?
- What was the worst part of treatment?
- What helped you get through that worst part?
- What scans did you undergo, and how frequently?
- How long did you have to wait for results?
- Were there any big surprises during treatment?
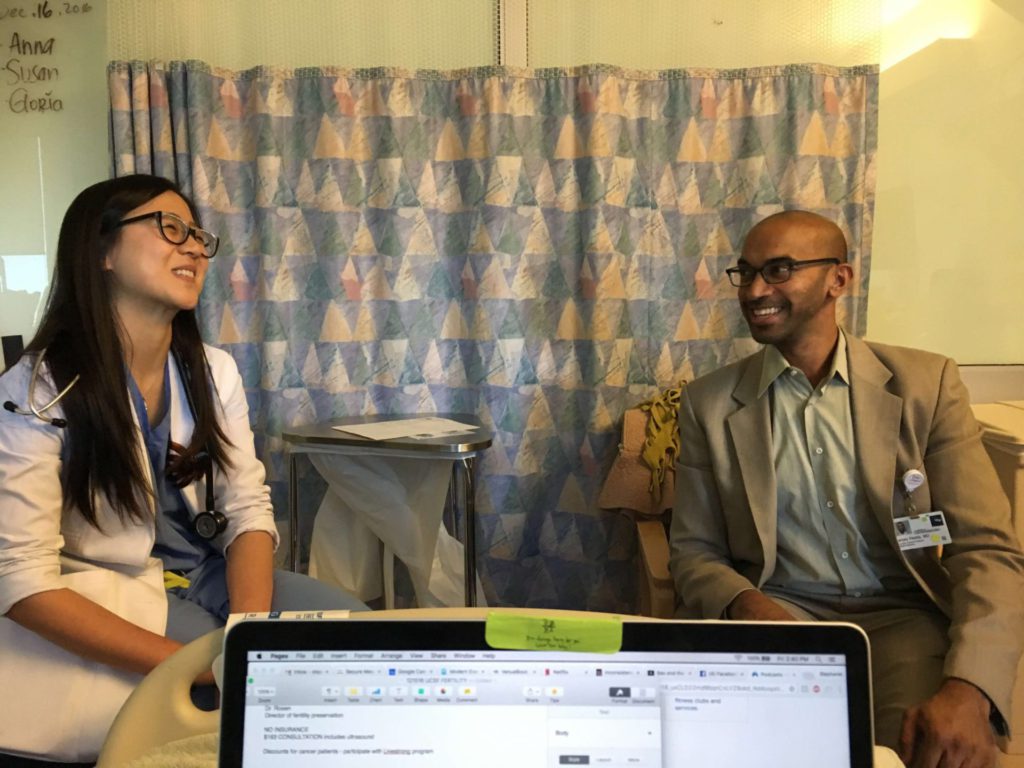
- IVF Before Chemotherapy
- Who brought up fertility concerns?
- How did you find your IVF doctor?
- Describe that first meeting with the reproductive health doctor
- Describe the process before egg retrieval
- What were the concerns with the IVF process for a cancer patient?
- What do you remember from the egg retrieval?
- What were the side effects after the egg retrieval?
- Any last words on the IVF process?
- Life Outside Treatment
- Did you use alternative or holistic medicine?
- What helped you manage your emotions and thoughts?
- What got you through the toughest times?
- Were there moments you had to advocate for yourself in and out of treatment?
- Could you work through treatment?
- How was the financial aspect of dealing with treatment?
- What do you wish you had known to help with the financial process?
- Did you have help around the house?
- How important is it to have caregivers?
- What’s your advice to others who are just now getting diagnosed?
This interview has been edited for clarity. This is not medical advice. Please consult with your healthcare provider for treatment decisions.
I know it feels lonely and overwhelming right now. It won’t always ‘be okay,’ and that is okay. Dealing with cancer treatment isn’t easy, but it helped to give myself permission to feel all of my emotions, including the negative ones. Only then was I able to truly move on.
Cancer is a trauma I wouldn’t wish on anyone. It taught me to sit still and know peace in a way I would have never learned had I not gone through this experience.
You are not alone. We are here to help you in any way we can. Big hugs.
Stephanie Chuang
Diagnosis
What were the first symptoms and red flags?
I was feeling lethargic and sleepy for weeks, but attributed it to my most recent work schedule. For about a week, I would wake up with a swollen jaw and neck. As the day went on, the swelling would subside, so I thought I was just bloated.
It wasn’t until I woke up one morning and had a very deep cough that came from a place I’d never experienced. It happened just once in the morning, but I was a bit freaked out by it. It happened again the next day, and that’s when I realized that something wasn’t right, that I wasn’t just bloated. I decided to make a same-day doctor’s appointment.
How did you get diagnosed?
I thought I was fine because I had just had a physical that checked out fine about a month before. Before the appointment, I definitely searched online with the symptoms, and some shades of cancer came up.
When I saw the doctor in the late afternoon, I mentioned this, acknowledging that I shouldn’t use “Dr. Google.” She told me I probably had mono.
The entire appointment was great until she decided about 15 minutes in to check for lumps. I had some swollen lymph nodes around my upper neck, but she said that was common for infections.
She then felt down around my upper chest. Her entire expression changed. She said, ‘Hmm, this is a red flag.’
I felt everything in that room shift. She assured me it was still probably nothing but essentially said it was either mono or something more serious.
She ordered blood tests that early evening because that center has a lab for that, but then she instructed me to get a chest X-ray and ultrasound of the neck.
I tried to schedule those, and that was the first time I realized that even though cancer might be hanging over my head, I still had to deal with logistics, insurance and waiting for tests to be done. I could do the chest X-ray anytime because it was first come, first served, but the ultrasound had to wait a week.
A week. I was in shock that ‘the system’ wasn’t catering to my concerns of cancer. How could I wait that long to find out?
I’ll never forget her words.
“I just heard back from the radiologist. I’m sorry, Stephanie, it doesn’t look promising.”
The next words out of her mouth were, “It looks like lymphoma.”
Gene testing
Thankfully, UCSF has free gene testing (if you qualify, not sure what that entails). My diagnosis was a bit iffy. It was stage 3 non-Hodgkin’s. Stage 3 because the multiple tumors were above and below my diaphragm. The reason I had been getting a swollen face and neck was because the biggest tumor mass was pressing up against my superior vena cava, the main artery that drops blood into the heart.
The initial typing was diffuse large b-cell lymphoma (DLBCL) with double expressors, which just means the diagnosis was less straightforward than what I’d hoped.

We wanted clarity on what exactly I had, so after the gene testing, it was determined that my disease presented more like primary mediastinal. I was thankful for that because I had heard that primary mediastinal responded better to the chemo.
Describe each test and biopsy you experienced
Summary: After the initial X-ray and CT scan, I had a CT scan and PET scan to figure out the masses. Then a camera stuck down my nasal passage into my throat (with a gross anesthesia sprayed down so it would hurt less), another CT scan before a lymph node biopsy, bone marrow biopsy, an MRI, PET/CT scan.
Nasal passage
This was during my initial time in the emergency department. The ENT fellow told me he needed to do this to make sure that the masses pressing up against my heart artery wasn’t damaging my voice box.
The anesthesia numbed it enough so that I wasn’t experiencing too much pain, but it was definitely very uncomfortable. The anesthesia was also pretty gross-tasting.
Excisional lymph node biopsy
Doctors wanted to determine my type of non-Hodgkin’s, so they took out an entire cancerous lymph node on the left side of my lower neck. I was given full anesthesia for that operation, so I didn’t feel anything. I just remember feeling pretty scared before being put to sleep.
After the surgeon double-reassured me that I wouldn’t wake up midway through the procedure, I dozed off and woke up a bit delirious from the drugs, but also feeling fine. As the drugs wore off, my neck did start to feel quite tender.
PET and CT scan
They injected some colored sugar dye in me. The cancerous activity is supposed to light up through that. Just FYI, and they do warn you, when the dye goes in, you feel hot everywhere in your body. You also feel like you have to pee, but you don’t. The scans were done in a big tubular machine where you are lying still, told not to move and are moved mechanically by the machine to go in and out of the tube.
Bone marrow biopsy
The most painful one of the bunch because the doctor only used localized anesthesia. The blood cancer fellow came in. Here’s what I wrote in my blog:
“Dr. V. came by my hospital bed in the morning with a lot of tools and 2 techs behind him, one who was towing behind her a very large computer machine. She had on the usual gloves but also this visor thing and a lot of cords around her. My stomach sank. I was really straightforward as soon as the crew entered the room.
‘Okay, what can I expect? I’m super squeamish. I’m a wimp when it comes to needles. How long does this last? How many injections? I’m sorry, I know this is annoying. But do people cry? What does it compare to? Does the lidocaine hurt? Does it hurt more?’
Yes, I was THAT patient. But they were all quite patient with me. They talked me through, and I built up the worst of expectations in my head to try and mentally ready myself. It hurt, but I had channeled myself elsewhere during the procedure.
It was specific and very vague at the same time. I imagined myself along the Embarcadero (street). I saw beautiful water scenes. Then suddenly I was swimming in the water.
I could feel the doctor shoving the needle in different directions after pulling out what felt like 5 feet of bone marrow. That’s because the next step was trying to get actual bone matter for testing.
It’s just achy and sore, similar to my neck wound. It’s nothing compared to what I think I’ll go through during chemo. Since my lymphoma appears quite aggressive and looks like it has spread, my chemo regimen will probably be just as aggressive. I’ll need tips on how to look cool with a bald head.”
How did you choose hospitals?
Our friend David is a doctor at UCSF, though not in oncology. He was the one in our home an hour after getting the diagnosis over the phone. That doctor on the phone mentioned in a second call that we might want to go to the emergency room but left us with more questions than answers.
David insisted we go to the emergency department instead of waiting for an oncology appointment, which would likely take many days. He said that doing this would get us ‘into the queue.’
As a local doctor, he was able to call the nearby center where I’d gotten my X-ray and CT scan, and after hours pick up those images and drop them off to our emergency department.
Did you go to a smaller or biggest hospital? What did you like about it?
I went to a large teaching hospital in the city.
- Pros: I like that there’s access to a lot of different services. You have a lot of incredibly smart people who are considered leaders in their respective fields.
- Cons: Sometimes you feel like everything is quite impersonal, at least in terms of how you can get in touch with people.
How was your medical team?
I really appreciated my medical team. From the start, they showed that they cared. Just a head’s up — you will meet a bunch of new faces at a teaching hospital like UCSF.
The first set of people were the emergency department nurses and doctors, then it was the internal medicine, finally the lymphoma specialists. In the hospital, I didn’t meet the oncologist who’d take care of me through treatment until a couple weeks later.
Did you get a port or PICC line?
I got a PICC line, then a port, then back to a PICC. Unfortunately, I did end up having issues that are probably more rare but worth knowing about perhaps.
My overall conclusion is that I actually liked having the PICC line because the port just never felt right. Again, I’m definitely in the minority here, as I heard a lot about how much patients preferred the port.
How was the PICC line?
This was put in instead of a port because my biggest cancerous mass was too big and close to where the port needed to be. Doctors wanted to shrink my tumors with at least 1 cycle of chemo before putting in the port, so I got a PICC line.
At UCSF, you have to go to a different site to get the PICC line and ports surgically put in (interventional radiology was at a different campus).
»MORE: Read more PICC line experiences
How was the port?
Big preface: what I experienced is apparently very rare. I finally got my port put in after the first cycle.
Unfortunately, it never felt right. I was awake for the procedure with only localized anesthesia applied. When I came out, it never stopped looking swollen and red and bruised.
It wasn’t until weeks later when a nurse may have accidentally put in the wrong length needle to access the port for my chemo infusion that I woke up with a pool of blood on my port site.
The needle had ripped the skin. This led to an infection of the port site, and it had to be drained, then eventually surgically removed. Because it was an infection, the surgeons couldn’t close the hole, so they ended up having to stuff medicine-infused gauze into the hole every other day for a couple months until the skin tissue healed.
To be honest, you may encounter your own version of this — not this specifically, but just ‘another thing to deal with’ that makes you feel pushed over your limits.
I definitely got upset at having to deal with ‘another thing,’ and I think it was just pushing me mentally and emotionally to be more disciplined. I learned to do deep breathing when I felt overwhelmed, and that really helped!
Then I had to get a PICC line put in again. I actually really liked the PICC line, even though I had heard a majority of people really like the convenience of the port.
For me, a family friend who’d had cancer and had a PICC line sent me an arm covering called a LimbO that helped me keep the line dry during showers. The line never hurt me and was just more seamless for me than a port.

Chemotherapy & Side Effects
What treatment regimen did you undergo?
I had 5 cycles of dose-adjusted R-EPOCH chemotherapy after 1 cycle of R-CHOP chemotherapy. They had to do that because my mass was too big to put a port in for that first cycle, and R-CHOP required less chemo time.
Describe in detail what happened each cycle
Each cycle was 3 weeks long. Week 1 was the infusion that was 24 hours a day for about 5.5 days in a row. Week 2 was when the side effects hit hardest. Week 3 was when my white blood cell counts were rebounding, although a couple times they didn’t rebound quickly enough and my next chemotherapy cycle had to be postponed by a day or 2.
I was outpatient for 5 of the 6 cycles, which meant I would just go into the hematology clinic every day during Week 1 to get my chemo bag changed out of this portable pump that I was connected to (wore it like a bag) 24 hours a day, every day for 5.5 days straight.
What was Cycle 1 of chemo like?
The first cycle was the worst one for me.
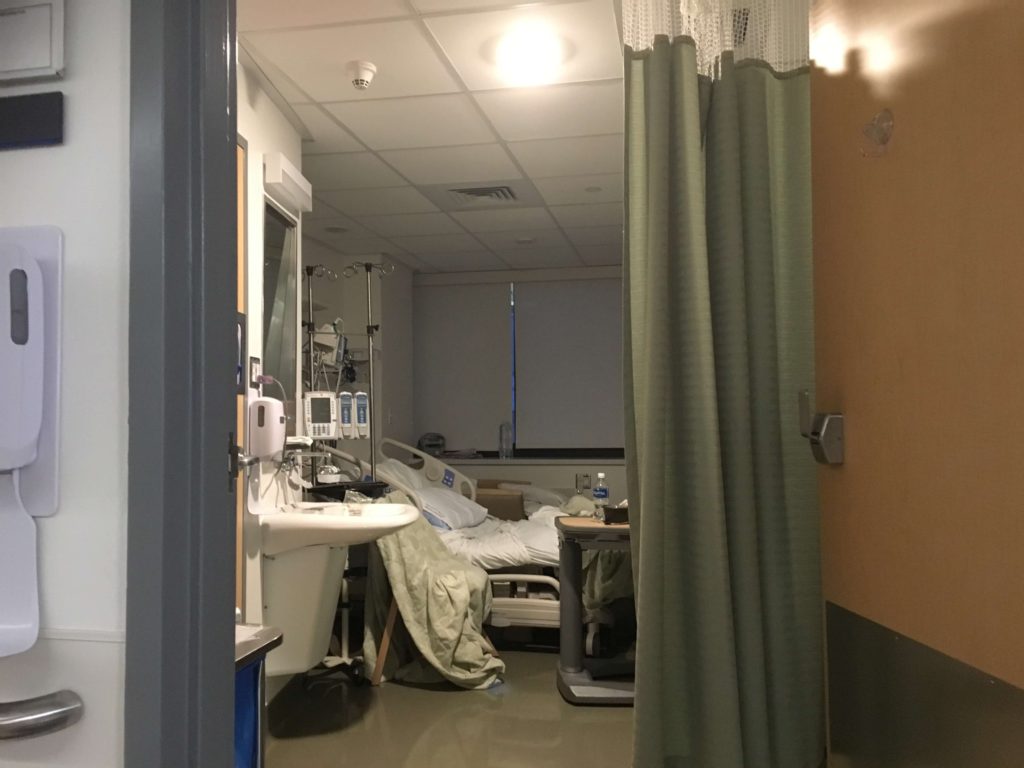
I had just undergone egg retrieval because I was nervous about my fertility after chemo. Because my biggest mass was located near the heart, they couldn’t put a port in for my chemo, so I had to do the first cycle inpatient at the hospital using a PICC line.
I had my biggest side effects reaction there with nausea that resulted in vomiting. I would throw up again when I went home. This was the only cycle that happened.
I also had an extreme reaction with mouth sores, at least 2 dozen of them on my tongue, cheeks, inside my lips, back of my throat, everywhere. It was an absolute nightmare.
This is why, in part, I really wanted to start a platform where patients could get this kind of information ahead of time. Doctors are so inundated with patients and work. Their first priority is to save your life. I think there’s a lot of we can do to help people with their quality of life during treatment.
Did the chemo cycles get better or worse?
I know this varies for people, but it got better for me thankfully! After experiencing terrible side effects in Cycle 1, I told my doctor and stressed I wanted remedies. She ended up recommending some various medications to help prevent things like the mouth sores and nausea.
While the nausea continued, it did get better as I began to take the anti-nausea meds more proactively. I also never had mouth sores again after she prescribed medication to prevent them. They weren’t a guarantee, but thankfully they worked for me!
The cycles got better physically in that the side effects were more manageable because I knew how to deal with them in a better and more efficient way.
But the emotional and mental impact was cumulative. They added up over time. I kept looking at the next cycle and tried not to think beyond that, or else it would have felt like the end would never come.
What were the side effects of chemo, and what helped prevent them?
Summary: Nausea, vomiting (first cycle), fatigue, weight gain (steroids), mouth sores (first cycle), bone pain (Neulasta and Neupogen shot)
- Nausea: This is the one that stayed with me throughout all 6 cycles of chemotherapy. It’s a pretty bad feeling because it sneaks in and out. It affects your mood so easily because it’s so much discomfort.
- What helped: The key here is to take nausea-preventative medications like Ativan as soon as possible so that you can get ahead of the nausea. It’s too late if you’re already feeling it. I would time out my anti-nausea medications so that I could avoid even feeling it a little bit.
- What helped: The key here is to take nausea-preventative medications like Ativan as soon as possible so that you can get ahead of the nausea. It’s too late if you’re already feeling it. I would time out my anti-nausea medications so that I could avoid even feeling it a little bit.
- Vomiting: Only happened in the first cycle, and there’s really not much you can do about it other than try to take anti-nausea meds in a preventative measure to help keep you out of that danger zone. My vomiting happened as a reaction to the chemo drugs the first cycle.
- Mouth sores: I am so, so grateful this only lasted the first cycle. This was maybe the worst side effect of them all because it impacted everything. I couldn’t eat, drink, nor talk without pain. I had about 2 dozen mouth sores all throughout my mouth. They covered the inside of my lips, my cheeks, my throat, my tongue. It was incredibly painful.
- What helped: Acyclovir! Ask for this drug. It may or may not be as effective for you as it was for me, but it’s worth a shot. It was the magic key for me in never getting mouth sores again. For my first cycle when I didn’t know about Acyclovir and already had mouth sores, I tried magic mouthwash. It didn’t help much, though it did numb my mouth for maybe 20 minutes or so, just long enough to allow me to drink something or eat something small.
- Canker sore patches: Ended up being the best solution, over canker sore gels and numbing meds. The patches covered up the holes enough to provide some relief and allow the sores to heal more quickly. I had to drink smoothies to get my calorie intake because eating was just too hard.
- Fatigue: This is another side effect that is hard to avoid because of course you’re going to be tired. It’s easy to forget but your body is working hard – in overtime- especially with the kind of aggressive chemo I was undergoing.
- What helped: I didn’t do this enough, but I think what helped most was moving around. Staying active.
- What helped: I didn’t do this enough, but I think what helped most was moving around. Staying active.
- Weight gain: The damn steroids really did not help here! I ended up gaining weight on the chemo because of the prednisone (steroid). It made me hungrier. Actually, a lot of times food helped with the nausea. I wasn’t moving around as much. There was fluid retention.
- What helped: Again, I needed to move around way more. I wish I had!
- What helped: Again, I needed to move around way more. I wish I had!
- Bone pain: This was a direct result of Neulasta or Neupogen shots that were given to boost my white blood cell counts after chemotherapy did a number on them. It felt like pinprick pain in my bones. This got better for me the last half of chemo (last 3 cycles).
- What helped: I took Claritin after hearing it could help. I thought there was a difference for sure, though I’m not sure I can attribute it 100% to the allergy medicine.
Anything you wish your doctor would have told you to help you prevent them?
Yes, I did not know that taking acyclovir might help! Had I known about it, I think I would have saved myself a cycle of absolute oral torture (no exaggeration).
I know it may not work for everyone, but I think just knowing what I can do or take to prevent side effects would help me feel some sense of control. That’s all I wanted.
Hair loss from chemo
This was so hard. I knew it would be hard. The lead-up to shaving my head was the most painful part, actually. Like clockwork, the hair really started to fall after my first cycle of chemo. Seeing the clumps of hair on the floor wasn’t as shocking because I always had long hair, and it would shed frequently.
What did upset me was the sight of clumps of hair on my pillow every time I got up from bed. It was so hard to see that because I think I equated that with me losing my ‘normal’ life.
So I went and got my head shaved on one side while my hair stayed long to get a ‘cool’ hairdo that I would have never gotten. It felt so empowering. I even recorded it on Facebook Live so that my friends could be with me as it happened. I got so many compliments on how cool it looked.
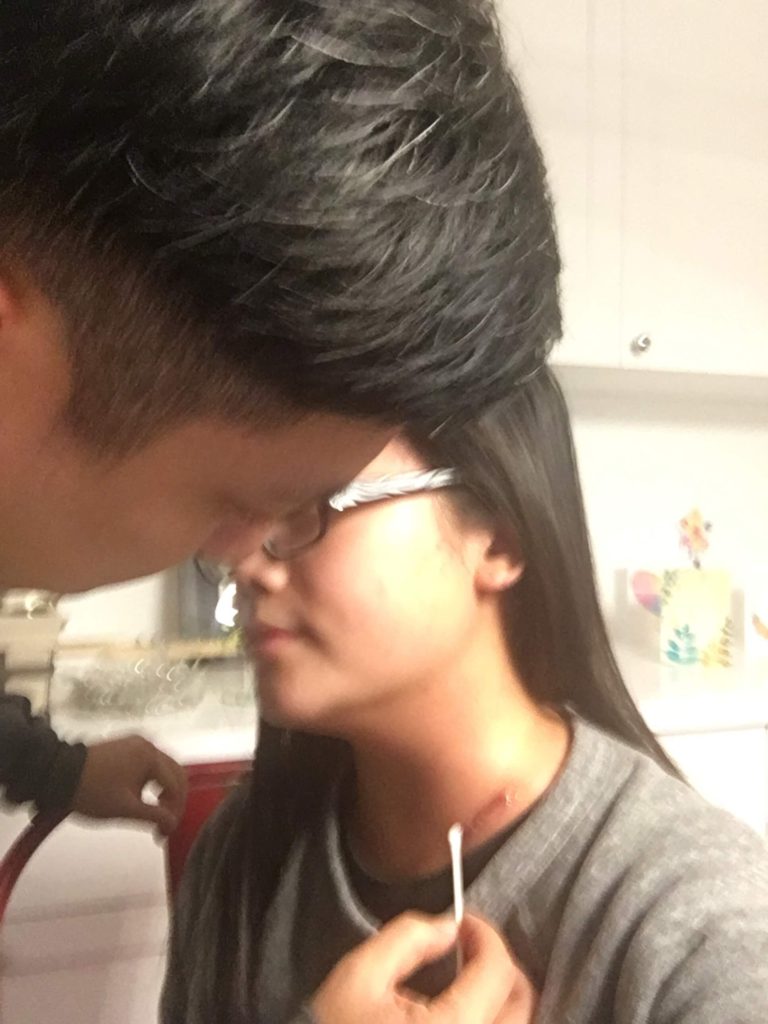
That lasted a couple weeks before the hair was just falling out way too much and too often. I still wasn’t ready to part with my hair all the way, so I had my mom cut my hair to shoulder length.
That lasted a week and a half maybe until I had my husband shave my head in front of my parents and sister. It would be liberating, but I definitely felt numb in that moment.

I was told that I would know when it was time, and I actually did. The pain of seeing my hair fall and feeling helpless became too much, and being able to take control of the situation by shaving my head was absolutely liberating and empowering.
Were you surprised by your reaction to losing hair?
To be honest, no. I knew I would hate it. I always loved my long hair. It had become, to me, part of my identity. Not having it and to be forced to lose it was so unbearable.
What did surprise me was how free I felt when my head was finally shaved. I really do think I viewed it as me dictating my own life. This would happen, but on my terms.
I wouldn’t wait till I saw obvious bald spots. I wanted to say when and where, and it felt good to be able to do that in front of my closest family.
What helped with the hair loss?
I didn’t try cold caps because my oncologist told me my chemotherapy was so aggressive that cold caps likely wouldn’t do much. I didn’t even want to get my hopes up, so I decided to just lose my hair all the way.
I bought a human-hair wig, and it was so expensive: $2,000. I don’t know if it’s because I live in a city where prices are just crazy everywhere, but I was shocked by that price.
I heard insurance may cover it if you have your doctor write a note about how this is a necessity for your emotional and mental health. But even if the wig price was easier to digest, the actual wig itself was so uncomfortable because it’s hot and can get itchy. That’s how it was for me.
So the best thing for me was to wear baseball caps that had a wig attached to it, because the top of your head is covered by a nice cotton fabric instead of itchy material.
This was the best, even through the point when my hair started growing back. For me, hair growth was about 6 weeks after chemo. Of course, it took months for the hair to grow up long enough to style!
»MORE: Dealing with hair loss during cancer treatment
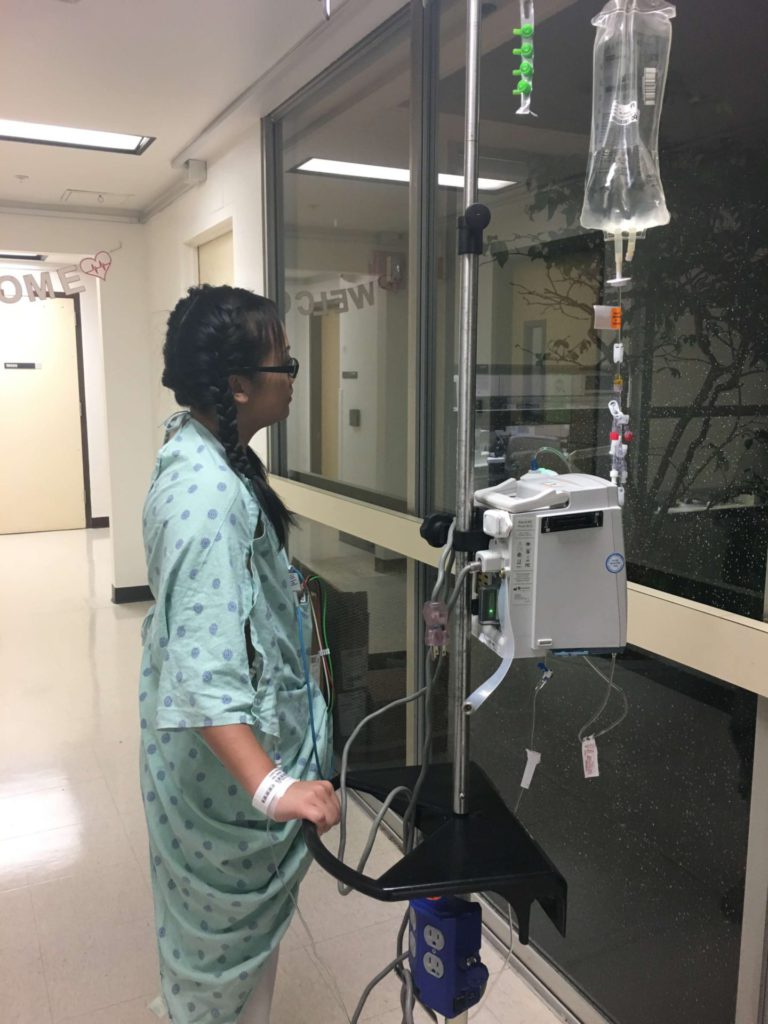
What was the worst part of treatment?
I wish I could just say everything. I think the fact that I was feeling absolutely sidelined because the chemo was so aggressive and side effects were pretty harsh, as well as frequent.
It was physically taxing, but the emotional and mental portions of it were the worst. I felt isolated because while my closest friends and family loved me and tried to support me, they didn’t fully understand what it was I was going through.
I would watch nonstop TV. It was too hard to go outside or even look outside the window because it felt like I was getting left behind while the world kept turning. That was a really tough piece to swallow, especially for a Type A person like me.
I had to also physically isolate myself (I called it quarantine) because my white blood cell counts were so low that my risk for infection was high all the time.
That restricted my ability to go out and also limited whether people could come over to my house.
If they did, we’d all wear masks just to be safe. When the flu started going around my husband’s work, he would have to wear a mask around me, too.
What helped you get through that worst part?
Mentally and emotionally, what helped the most was connecting with others who had been in my shoes.
I felt they understood truly what was happening and how I was feeling. I was also so lucky to have my dedicated husband and also my incredible parents and sister constantly surround me, making sure that I was taken care of.
My mom actually lived with us during the week and then went home — she lives under an hour away — for the weekend to give me and my husband privacy. She would cook for us, clean, tend to everything that I couldn’t. She was such a godsend.
Physically, what made me feel better was eating. My mom’s home-cooked meals did so much for me. That and strong drugs, honestly. I have always stayed away from taking pills. I grew up ignoring my headaches until they went away instead of taking Tylenol.
During chemo, I had to learn how to take pills proactively before side effects would hit.
What scans did you undergo, and how frequently?
I had a PET/CT scan after the first round to make sure that my main mass had shrunk enough to allow interventional radiologists to put in the port in my chest area. That was abnormal.
I had my next scan after the fourth cycle of chemo, another PET/CT scan after my last cycle, and then again about 8 months after that to determine whether I’d need to get more.
What I did need to do all the time was get my blood drawn. If you get blood cancer, you will have to get blood tests for the rest of your life, essentially. The first year after treatment, it’s every 3 to 4 months, then twice a year, and then maybe 5 years and beyond it goes down to just once a year.
How long did you have to wait for results?
The wait is one of the worst things you have to endure.
The PET/CT scan results usually came back in 48 hours. That was too long for me. I actually scheduled my scans on Monday, not end of week like Thursday or Friday, because you rarely get responses on the weekend, if ever.
You usually have to also schedule a check-in with the oncologist around that time, so I would try to schedule the scan for Monday morning and the appointment with my oncologist late Monday. I felt she could then work on getting the results, no matter how preliminary, and that information would be better than none at all!
»MORE: Dealing with scanxiety and waiting for results
Were there any big surprises during treatment?
Yes, and those are unfortunately never good. The first was that port infection. That made things so much harder to digest because, again, it was “one more thing.”
The other was actually after treatment was over. I was neutropenic, meaning my blood cell counts were so low that my risk for infection was quite high, for 5 months after.
For the first few weeks when my blood draws showed those low WBCs, my oncologist was unbothered. She said it was just my body taking a little longer to rebound. By the time it had gotten to 2 months of neutropenia, her attitude changed. She mentioned that I might have to undergo another bone marrow biopsy.
My heart sank, and the tears sprang to my eyes. I remembered some of the bone marrow biopsy — not the physical part, but the fact that it was during a time of questions, chaos and anxiety. It was to answer questions. Waiting for the results was excruciating because I just wanted to fast forward to the results. Had the cancer spread?
Now, months after chemo had already ended, I was being subjected to the possibility that I’d go back to what I considered Square 1. I was so emotional, and it didn’t get better as the neutropenia persisted.
It wasn’t until I went to an amazing cancer retreat program hosted by an organization called Commonweal that I started to feel a shift. I was eating healthfully and drinking herbal teas suggested by a Chinese medicine doctor.
After 2 weeks, my white blood cell counts were up. It could have been just my body finally recovering, but either way, it felt like I could resume life again.
IVF Before Chemotherapy
Who brought up fertility concerns?
I did. The thing I thought of right after my mortality was my fertility.
At the time of diagnosis, I was 2 months from getting married. Being 31 and thinking about family life meant that chemo scared me on another level outside of its general impact on my body. Questions flooded my mind like:
- Can I get pregnant naturally after undergoing such aggressive chemotherapy?
- What would my options be to protect my reproductive health from the chemo toxicity?
- What are my options if I can’t get pregnant after chemo?
So on the first or second day of the first week of my hospitalization, when the medical team was still trying to get the specific diagnosis, I brought up how important of an issue this was for me.
My oncologist would later tell me that anecdotally, she had patients who went through R-EPOCH chemo who were able to conceive naturally.
That honestly wasn’t enough to allay my fears. I was pretty stuck on going through with the egg retrieval as long as it didn’t compromise my health significantly to delay chemo by a couple weeks.
The good news here is also that as a cancer patient who needs treatment, your IVF process is expedited into a couple of weeks instead of over a period of months.
How did you find your IVF doctor?
I was already in the UCSF system, so I was referred to a reproductive health/fertility specialist within the UCSF system, Dr. Mitch Rosen. I would have gone outside the network had there been a more reputable place to go.
Lucky for me, UCSF and Dr. Rosen are top notch, so that decision was pretty easy and smooth.
Describe that first meeting with the reproductive health doctor
I think the total visit was about 60 to 90 minutes, including an initial ultrasound exam. Dr. Rosen’s consultation portion was 30 to 45 minutes or so. He went into detail explaining the IVF and egg/embryo freezing processes. We went over my personal route, factoring in things like age.
Here’s another instance where I think either recording the meeting and/or taking notes is important. There’s a lot to learn!
Neither my husband nor I had a real understanding of what IVF and the process meant. Dr. Rosen was patient and even drew some diagrams to help us better understand how my reproductive system works, how age impacts fertility, and how something like chemo might also impact the reproductive system.
Describe the process before egg retrieval
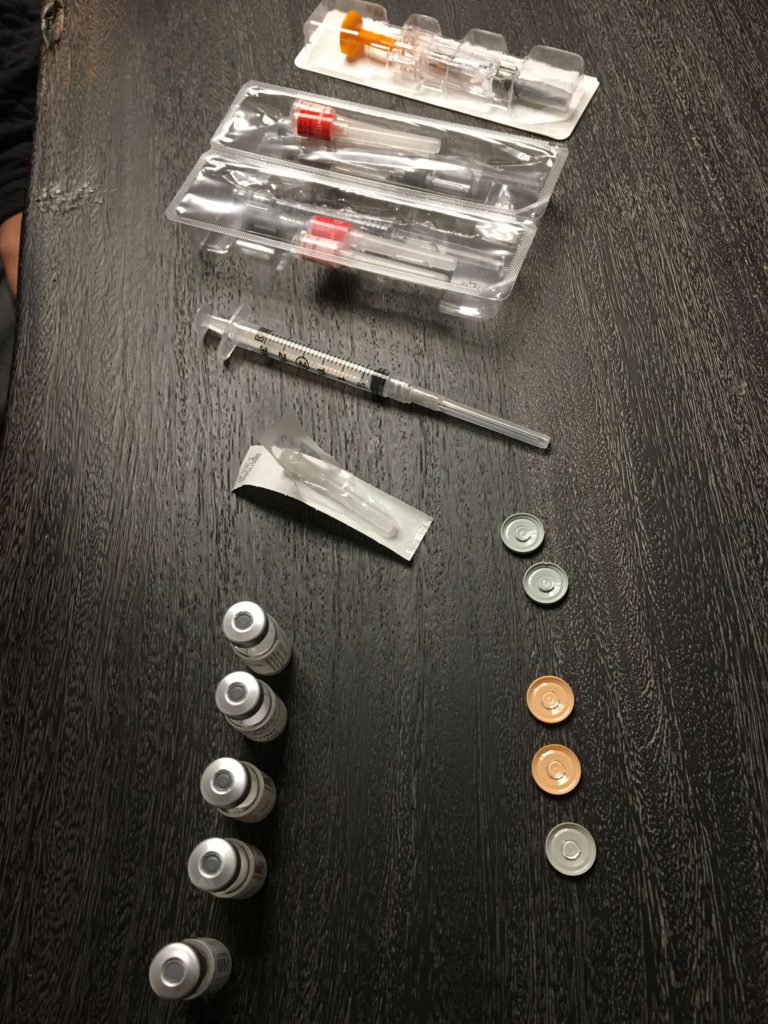
I had been shooting myself multiple times a day in the tummy, injecting myself with a cocktail of hormones. I had the same experience as fellow The Patient Story community member Joyce Yu, who was gracious enough to document the entire process in this IVF journal written specifically for this platform.
For info on fertility and pregnancy after chemotherapy, click here →
What were the concerns with the IVF process for a cancer patient?
After injecting myself daily, I got some stomach-churning news: I was told that there were some concerns with proceeding. I was devastated. They were telling me I might get to the last day and not be able to finish.
Why? Part of adding so many hormones in at once means fluid shifts in the body, which could compromise me in my cancerous state. Suffice it to say, I felt incredibly weighed down with a million emotions I had no idea how to process. There were 3 days of feeling mentally and emotionally drained with no break.
I had to undergo an extra echocardiogram, oncology consult and cardiologist appointment spread over 3 days later. Thankfully after all that, I was given the green light.
What do you remember from the egg retrieval?
I remember going in early ahead of the morning egg retrieval procedure start time.
What were the side effects after the egg retrieval?
I want to preface with this: I feel so grateful to have been able to complete the IVF/egg retrieval process. After going through it all, I am so happy we went through with it and knowing what I went through after, I still wouldn’t change my mind.
I did suffer ovarian hyperstimulation syndrome (OHSS) on top of it all. The nurses did not warn me about this, and I wish they had. Perhaps they avoid discussing this in detail with patients to avoid psychosomatic tendencies and experiences. Whatever the case, I am the type of person who appreciates a good head’s up so I can ready myself. This is what I’ve been dealing with post-egg retrieval:
- nausea
- vomiting
- bloating
- stomachaches + cramps
- extreme fatigue
- coughs (some fluid build up)
- sharp, side-splitting cramps that tear up the insides
Any last words on the IVF process?
Most importantly, I am so glad I was able to do this. While this will be an option for most cancer patients looking for fertility preservation options, it doesn’t always work out for everyone.
It’s important to understand that situations like fluid buildup around the heart may occur for patients. You could start the hormone injections and get all the way to the second week where you’re on the verge of doing the “trigger shot” before the egg retrieval, and suddenly, your body does something that complicates the situation and prompts the doctors to stop the process.
They will always prioritize our health first. If that means not risking harm by continuing the IVF process, as difficult as it is, it is what they have to do in our interest.
»MORE: A patient’s IVF journal
Life Outside Treatment
Did you use alternative or holistic medicine?
I didn’t while I was going through treatment, though now I wish I had done acupuncture because I’ve heard so many great things about how it helped to combat chemo side effects for other patients.
To be honest, my parents had been going to get acupuncture for years and suggested it as something that could help bring my white blood cell counts, but I didn’t believe in it.
I discovered Eastern medicine at the cancer retreat I mentioned before, about 4 months after treatment ended. They taught Qi Gong, a practice of mind, body, spirit that looks like tai chi, as well as acupressure. They couldn’t do acupuncture for liability reasons.
At the retreat, I was finally open to listening to all different types of healing methods, including Eastern medicine, and when I returned home from the retreat, I sought out some acupuncture and herb tea help.
Maybe it was just that my body was about to rebound, but my white blood cell counts did rebound finally, and it was the most incredible feeling.
I think at the very least, the Eastern medicine and Qi Gong gave me some peace of mind and helped me to relax. I think that always helps your body, no matter what.
What helped you manage your emotions and thoughts?
I took a mindfulness class that helped me slow down my reaction to thinking. I learned that you can’t control what you think and feel, but you can influence how you react to those thoughts and feelings. It calmed me down.
I would try to enjoy everything and live in the present as much as possible. That meant really washing every cup and plate and utensil when I did the dishes instead of rushing through it like a chore. That meant trying to really feel the water on my skin every time I showered instead of rushing through it like another chore.

The deep breaths really helped. You don’t even have to meditate. Just taking deep breaths really slows me down in such a peaceful way.
The other thing that helped was sharing my story via my blog. I am a private person. I never thought I’d blog, but I did, and sharing my raw emotions with the world was incredibly cathartic.
What got you through the toughest times?
Support and love from the people close to me. That always made a big difference. I had friends who flew cross-country just to be near me. It happened a couple times, and they let me know a very important message:
“No pressure. We are just here if you need us.”

That did wonders for me. I understand why many people drop off. They don’t want to bother you or add to your plate. That’s nice and all, but it honestly felt so much more isolating when that happened.
I didn’t need people tending to me at every moment, but a message every once in awhile was uplifting. Truly. Especially if it started with “no pressure to respond.”
Meditation also helped. I don’t mean the kind of deep meditation that takes constant and deep practice. For me, it was as simple as deep breathing to remind myself to live in the present and to know that things would be okay.
Were there moments you had to advocate for yourself in and out of treatment?
Yes, and it has nothing to do with how good my oncologist or medical team were. It’s pretty simple: sometimes the incentives feel a bit misaligned. The doctors are also so incredibly busy, so for a patient to get lost in the mix isn’t as rare as I had imagined before going through treatment.
For instance, the port was supposed to be fairly hassle-free. It is for most people, from what I hear. But it never felt right. It stayed bruised for quite some time. When I brought this up, it was often met with disbelief. Here’s a blurb from my blog, The Refract, showing what would happen before my fourth cycle: my port got infected.
How does that happen, you ask? Well, one part of it took place a couple of weeks ago. A nurse putting in the needle for my chemo used the wrong size, so it ripped my skin overnight.
We still don’t know exactly what happened. I wish I had listened to my body more and voiced the concerns, because only I live with my body. Medical opinions can only go so far. I spent too much time and energy worrying about being the hypochondriac-seeming patient. I didn’t want to be bothersome.
Moving forward, I have no problems speaking up as long as I balance the feelings with rational thought. It also doesn’t do anyone any good to think the sky is falling, but I believe the message has to swing more the other way, because it can often feel like our culture punishes patients for asking too many questions.
» MORE: How to Be Your Own Advocate
Could you work through treatment?
It felt like this would be just about impossible. Each cycle of the chemo regimen (R-EPOCH) is 5.5 days of continuous infusion. The second week is when the side effects usually hit.
The third would generally be the only possible week for work. It’s the recharge week.
If someone works at a computer and is able to do it remotely, it’s possible they could get work done during that time. For me, my body was taking a longer time recovering from each cycle. My white blood cell counts were consistently lower than my oncologist wanted. Low WBC ended up delaying one of my cycles by a few days.
How was the financial aspect of dealing with treatment?
I was very blessed in this regard because my health insurance (through my husband) was wonderful. Most everything was covered. The most costly procedure was what wasn’t covered by insurance: the egg retrieval/IVF process.

What do you wish you had known to help with the financial process?
Disability insurance.
In California, you can file for disability insurance anytime 9 days after the start of your disability. Very importantly, you have up to 49 days after the start of your disability to file, “or the claim is considered to be a late claim and you may lose benefits,” according to the State of California.
This is important because you will need your physician to fill out some paperwork in addition to your own. The sooner you can get this in, the sooner you can forget about the process and start getting some financial support while you go through treatment.
I wish I had known about this from the start, but as a cancer patient, I was so overwhelmed by the medical questions, including those for the IVF process I went through ahead of chemotherapy.
If you are unable and/or don’t have people who can help you figure this stuff out, try to seek out a social worker at your hospital or clinic.
They generally have people who specialize in helping patients and families figure out financial processes.
Did you have help around the house?
I was so blessed with the amount of support and help I got. My family (parents and sister) live less than an hour away. They were all so instrumental to my healing. They visited me and helped me with day-to-day tasks, even the smallest ones like changing clothes with a PICC line. My sister helped me wash my hair when I still had it.
My mom ended up staying with us a lot of the week to help cook us food and clean the house, things I definitely didn’t have energy for. My husband did a little bit of everything, but the most important was his calmness and love he had ready for me at all times of the day, every day.
I still ended up having plenty of time by myself. I think what’s important here is to understand that even with a lot of help around, there will be moments where the person you have to rely on for physical, emotional, mental help is you.
This is where the concept of learning how to ‘sit still’ was foreign to me. I couldn’t just get up and go do something outside. I had to reconcile with all my emotions, many of them negative, while just sitting wherever I was. I had to confront them.
In hindsight, this was one of the most important skills or tools of my entire cancer experience. Again, being someone who was always on the go and looking for “the next step,” I learned how to truly be present, even when it was so damn uncomfortable. This will be and mean different things for different people.
For me, it meant I used the deep breathing to lead my mind to understanding that things would be okay. And even if they weren’t okay, they were largely out of my control. What I could control was how much stress and energy I devoted to whatever issue was occupying my mind. This is something I’ve benefited from greatly since treatment.
How important is it to have caregivers?
From pre-diagnosis through treatment into survivorship, this cancer experience is definitely not easy. But like with other traumas or difficult life events, it’s always better to have people around you who can support you.
For me, having a caregiver in my mom and my husband allowed me to deal with the daily emotional and mental battles I put myself through. Just drumming up enough energy to have a really nice conversation with a loved one took a lot out of me. I was easily out of breath and out of motivation.
It’s nice to have people who can help you with tasks like preparing a meal or vacuuming. It frees up some of your mental bandwidth.
If you don’t have people physically close to you, perhaps there are other ways for this to happen. Have a friend put up a GoFundMe or any other crowdfunding initiative so that people can help put money towards getting you help.
Or they can fund a meal train remotely. Don’t be afraid to ask for help — you deserve every bit of it.
What’s your advice to others who are just now getting diagnosed?
There is so much wisdom in self-love. Be kind to yourself. Slow down. Remember, your body is doing a lot of work through treatment, even if you can’t see it for yourself. So take it easy on yourself.
If it helps, think of how the treatment is working whenever you are feeling side effects, including that hair loss. The drugs, the radiation, whatever it may be — they’re working to kill the cancer cells. It’s an unpleasant experience as well, but they can exist in tandem. Feeling negative and positive emotions at the same time are not mutually exclusive.
On that point, I felt it was so important for me to not shove my anger, sadness, fear under the carpet. It was productive to acknowledge them, have a good cry, hopefully paired with a good conversation, and then move on. I was unable to move on if I pretended those negative emotions just didn’t exist.
Most importantly, you will get through this. None of us goes through the same experience. We don’t have the same results. But this experience largely gives us a different perspective on life if you let it. It can be terrible for sure, but you do have some control over your own outcome in how you approach treatment.
Don’t be afraid to reach out to others. We’re all part of this club none of us signed up for. Hugs to you all.


Inspired by Stephanie’s Story?
Share your story, too.
Primary Mediastinal B-Cell Lymphoma Stories
Lauren D., Primary Mediastinal (PMBCL)
Symptoms: Dry cough, extreme fatigue, trouble breathing, swollen and discolored left arm, lump under the arm
Treatment: Chemotherapy
Daniella S., Primary Mediastinal B-Cell Lymphoma (PMBCL), Stage 2
Symptoms: Prolonged cough; low-grade fever; night sweats
Treatments: Chemotherapy (R-EPOCH), radiation, CAR T-cell therapy
Stephanie V., Primary Mediastinal (PMBCL), Stage 4
Symptoms: Asthma/allergy-like symptoms, lungs felt itchy, shortness of breath, persistent coughing
Treatments: Pigtail catheter for pleural drainage, video-assisted thoracoscopic surgery (VATS), R-EPOCH chemotherapy (6 cycles)
Stephanie Chuang
Stephanie Chuang, founder of The Patient Story, celebrates five years of being cancer-free. She shares a very personal video diary with the top lessons she learned since the Non-Hodgkin lymphoma diagnosis.




