Tim’s Stage 2 MCL Non-Hodgkin’s Lymphoma Story
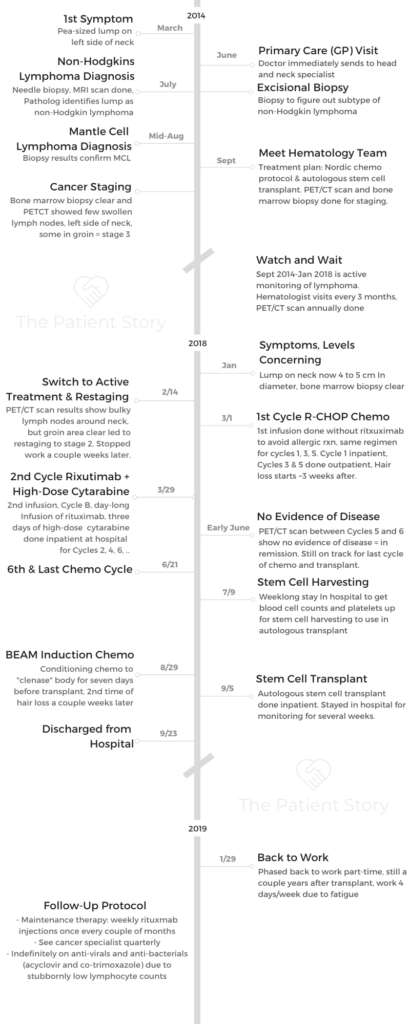
Tim shares his in-depth story on getting through stage 2 mantle cell lymphoma, including the Nordic chemo regimen, BEAM induction chemo and a stem cell transplant. Tim also talks about how he approached work during treatment and what support was most helpful to him.

- Name: Tim H.
- Diagnosis (DX):
- Non-Hodgkin’s lymphoma (NHL)
- Mantle cell lymphoma (MCL)
- Stage 3, then re-staged 2
- Age at DX: 50
- Treatments
- Watch and Wait (3.5 years)
- Nordic chemotherapy regimen
- Alternating cycles A & B
- Cycle A: R-CHOP
- Cycle B: R (rituximab), high-dose cytarabine
- BEAM Induction Chemo
- Conditioning chemo before stem cell transplant
- Autologous stem cell transplant
- Mantle Cell Lymphoma 1st Symptoms
- Non-Hodgkin Lymphoma (NHL) Diagnosis
- Mantle Cell Lymphoma (MCL) Diagnosis
- Staging the Mantle Cell Lymphoma
- Watch and Wait (Active Monitoring)
- Switch to Active Treatment (Chemotherapy)
- Nordic Protocol Chemotherapy Regimen
- What was the overall chemotherapy regimen plan?
- Describe Cycle A (Cycles 1, 3, 5)
- Describe Cycle B (Cycles 2, 4, 6)
- The constant drug through all cycles: rituximab
- You skipped rituximab first cycle, added on after last cycle
- You got infusions through the IV (cannula) and also PICC line. Which did you like more?
- You eventually moved to a Hickman line
- Chemotherapy Side Effects
- Stem Cell Harvest (Autologous Transplant)
- Conditioning Chemo Before Stem Cell Transplant
- Autologous Stem Cell Transplant
- Recovery after Stem Cell Transplant
- Reflections
- When did you stop and return to work?
- How did you family take the cancer diagnosis and treatment?
- What support was the most helpful to you?
- Has the cancer diagnosis and experience changed your life perspective?
- Do you ever experience anxiety about getting the cancer again?
- Last message to other patients or caregivers
This interview has been edited for clarity. This is not medical advice. Please consult with your healthcare provider for treatment decisions.

Life is what you make it, to a large extent. The way I’ve approached this all the way through is one of curiosity.
It’s about talking to the medical experts about what you’ve got, what the treatment options are, and trying to take that in. One of things I always did was take my wife to appointments so she could take notes, and I’d make notes as well.
It’s about using that interaction with the medical professionals for me to understand as much as what was going on as possible. Try to prepare yourself for each individual step. There’s lots of good advice out there.
Tim H.
Mantle Cell Lymphoma 1st Symptoms
What were your 1st symptoms?
It was something and nothing. I was 50 when I was diagnosed. My wife and I had gone on a trip to Hawaii. We were in the bathroom one night, and I was shaving, getting ready to go out to dinner.
I was complaining about a very small lump on the side of my neck, not much bigger than a pea or something like that. It was getting in the way of my razor. I said something properly unprintable about it.
My wife had a look and said I should probably see the GP (primary care doctor) when we got back. I thought it was probably nothing. It was just a cyst or something like that, because I’d had a few on my back before. It felt the same, no pain or anything like that.
What happened at your first doctor’s appointment?
When we got home early June, I went and saw my general practitioner, and he referred me to the local hospital very quickly.
In fact, there and then he said, “It’s probably nothing, but we ought to get you checked out.” It really went quickly from there.

Non-Hodgkin Lymphoma (NHL) Diagnosis
How did you get the first diagnosis of non-Hodgkin’s lymphoma?
I went and saw the specialist at the hospital. They initially did an MRI and a needle biopsy on the lump to see what it was. That came back positive for non-Hodgkin’s lymphoma.
Describe the needle biopsy
The needle biopsy is really quick and quite painless. Depending on your tolerance of pain, they can do it by putting a very small fine needle into the lump and draw some of the fluid and matter in it.
In my case, I’m squeamish, so they gave me some local anesthetic and did it. It was painless and over and done in about 5 minutes or so. For results, they were pretty quick, certainly within a couple of weeks.
Describe the MRI
I’ve only had one MRI scan, and to be honest, I don’t ever want another one again. It’s quite a noisy process. The MRI scan is confined as well.
They gave me that when they were still trying to figure out whether it was a lymphoma or head and neck cancer or whatever. That’s why they scanned my head in the MRI.
The biggest problem for me was keeping still for the 20 to 25 minutes that they took to do it. I still remember being encouraged from the control room to keep still and not breathe too much, to make sure the image was actually sharp.
I deliberately forget about the MRI bit because I really didn’t like it very much. But when you think about treatment in general, if that was the worst bit of treatment, that’s actually not too bad!
For results, it was about a couple of weeks after the MRI and the excisional biopsy — they were done around the same time — to get the full diagnosis.
How did you process the cancer diagnosis?
It was a bit surreal. The first conversation I had with the doctor was when he was giving me the news about the specific type of lymphoma that it was, non-Hodgkin’s lymphoma. He was there with the specialist as well.
In the UK, if you get a cancer diagnosis, you get a nurse specialist assigned to you, as well as someone who can integrate the various bits of the health system for you, to look after you. My nurse specialist has been with me all the way along my journey, including the other specialists.
It was a conversation with them. I sat there and went, “Yeah, yeah, yeah.” I went into a side room with the nurse specialist, and he gave me various literature to read from Lymphoma Action. They were helpful guides about what to expect.
I still sat there and was like, “Yeah, sure, but it’s going to be alright. I’ll work through this.” He was like, “Maybe not with this one because the treatment’s fairly tough, and not a lot of people tend to work full-time through it.”
There was still some degree of denial at that point. Also at the time, when I had that first meeting, they hadn’t worked out whether it was one they needed to treat immediately or not.

Watch and wait vs. active treatment
I went fairly quickly after that meeting for some more tests and procedures to help them figure out whether they needed to act straight away — that was the presumption originally — or whether it was something suitable for watch and wait.
At the time, when I was going through diagnosis, I think something like 10 to 15% of patients were considered suitable for watch and wait. Now, it’s closer to 30 or 40% with mantle cell lymphoma who go through that, because the diagnostics have gotten better.
The understanding of the disease has gotten better, and the treatments have gotten better in the last 5 to 6 years that I’ve been living with this thing as well.
There was a presumption I’d be treated right away. Actually, when I went in for a bone marrow biopsy and further blood tests, that was when they said, “Hang on, we can probably afford to wait with this one before we actually start you on active treatment.”
Mantle Cell Lymphoma (MCL) Diagnosis
You had to undergo more testing to figure out NHL subtype
At that point, they didn’t know what that was.
I went in for what they call an excisional biopsy, where they put you under general anesthesia and remove the lump or possible lump from the neck.
Describe the excisional biopsy
That was interesting. I was probably more frightened of that than most things, but actually, it was pretty much a non-event.
It was done as a day surgery at the local hospital. I went in 7 or 8 in the morning. They gave me pre-meds, made sure I was comfortable, and the next thing I remember is waking up in the recovery room a couple of hours later. I think the process literally took them minutes to do.
How was recovery from that excisional biopsy?
I remember feeling incredibly hungry after it and them feeding me sandwiches. I was home that afternoon and had a dressing (bandage).
It was perhaps a week or 10 days after I got it done, we went to Africa on safari for a couple of weeks to celebrate our 50th birthdays, so it couldn’t have been that bad.
When did you get the results from the excisional biopsy?
That was all done in the morning. I got the results back a week or 2 later, which confirmed that it was mantle cell lymphoma.
That was odd, because it’s a pretty rare type of non-Hodgkin lymphoma, and there’s only 400 or 500 people a year diagnosed with it in the UK.
Your family member had already gone through MCL treatment
My mother-in-law, my wife’s mother, happened to have been one of them previously. She’s also had mantle cell lymphoma and been treated successfully for it as well.
That gives you a fair bit of confidence that it is treatable and people do come out of the other end.
I remember my consultant telling me with my wife that that’s what I had got. My wife, Jane, was like, “Well, that’s what my mother had.” The doctor nearly fell out of his chair.
The odds of 2 people having it who knew each other, let alone within the same span of family, is vanishingly rare. He suggested that I do the lottery for it or something. I can’t quite remember the conversation!
That’s how I was diagnosed, and I was fortunate in that the GP I saw was relatively newly qualified and suspected that there was possibly something more to the lump than what it initially appeared to be.

Staging the Mantle Cell Lymphoma
Describe the bone marrow biopsy
There were 3 things I went through that I had not experienced before as I went through procedures for my first preliminary diagnosis.
One of them was the bone marrow biopsy. What they do with that is give you a local anesthetic in the small of your back. I don’t mean to make this sound too gruesome, but what it’s like is a drill or something. What they’re trying to do is try to take some matter from the bone marrow, take a sample out of there.
One of the things with lymphoma is it impacts the blood and the bone marrow, which is where the white blood cells are made. They’re doing that to understand if the lymphoma is present in the bone marrow, and if so, how much the bone marrow is affected. It’s part of the staging process.
Describe the PET/CT scan
The other thing I went for was a PET/CT scan. It’s different than the MRI in that the machines are much more open. It’s like lying on a giant photocopier, is the best way to describe it.
There’s a big donut around you as well, and you pass backwards and forwards through the machine. I actually quite like PET/CT scans; they’re good fun.
There were a couple swollen lymph nodes in my neck. What they were checking was to see whether there was anything else in my chest or in my groin and leg area, where the other lymph nodes were. That helps them stage the cancer.
What were the results of the bone marrow biopsy and PET/CT scan?
The results probably took at least a week. What they found with those 2 tests was there was nothing visible in the bone marrow at all.
As far as lymph nodes were concerned, the only ones that were swollen at that time were the couple in my neck and a suspicion of a couple in the groin as well. There was nothing in my chest cavity or anything else.
What was your staging at this point?
That got me staged at 3. That’s unusual itself, because a lot of mantle cell lymphoma patients, since the lymph nodes are systemic, it’s usually stage 4, but I was stage 3.
For MCL patients, it really doesn’t make a lot of difference to the outcome. The treatments are good regardless of your stage, which is encouraging.
If people hear stage 4 cancer, they tend to get very, very freaked out. That’s not necessary with MCL because the outcomes are much more dependent on variables like age, progression of the disease, than staging.
Describe the MUGA test
I had also undergone the MUGA test. It’s to check the heart functions and make sure if I would undergo chemotherapy, then I would be able to withstand that. I came through well on that one.
Watch and Wait (Active Monitoring)
Period: Sept 2014 – January 2018
What was the schedule during watch and wait?
I had consultant appointments every 3 months or so and a PET/CT scan approximately yearly (the last regular one was in November 2017).
The lump on the left-hand side of my neck grew to around 4 to 5 centimeters in diameter. Nothing was visible elsewhere. Between September 2017 (about 4 or 5 months before I started treatment) and January 2018, when I saw my consultant, the right-hand side of my neck, which had shown some activity but not much, decided to overtake the left-hand side in size in about 6 weeks.
I looked a little like Frankenstein’s monster! I’d also started itching. Even when the lump was that big, it wasn’t causing any problems with breathing, and it wasn’t painful. I just looked frightful!
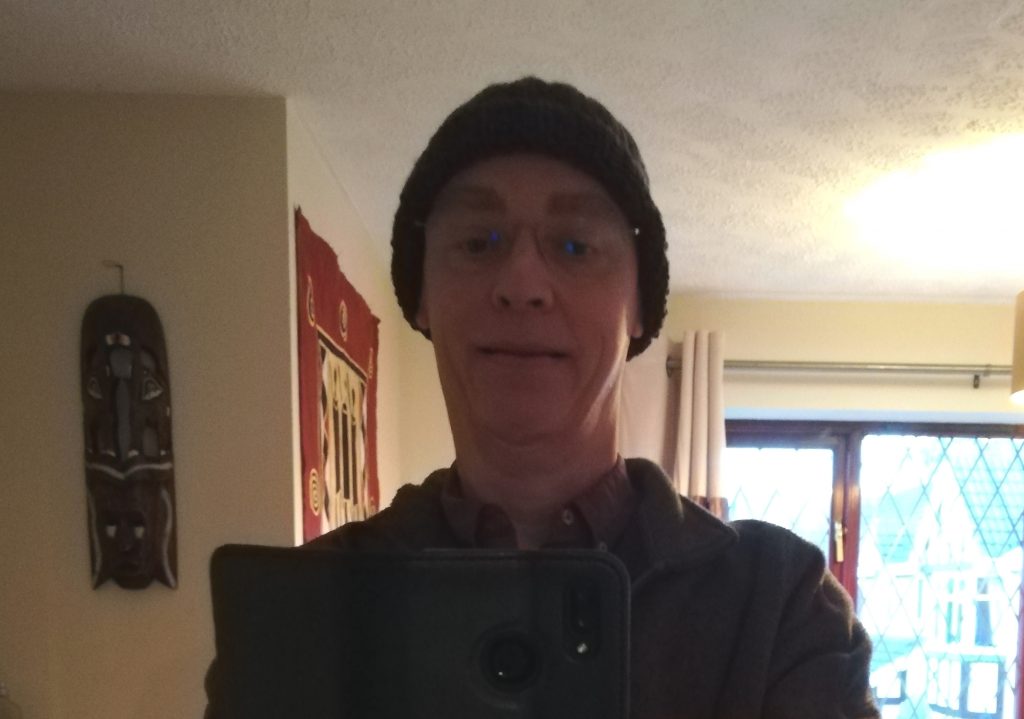
You can see the development or growth of the lump through pictures
This was taken as a Christmas present by a professional photographer, so taken in December 2015, about a year or so after the first diagnosis.

The other is a selfie of me and my wife around the same time. This one, you can see the extent of the lump on the left-hand side of the neck, which is probably 3 centimeters, an inch-and-a-half across.

It was something that was just growing gradually, certainly throughout the first 2 or 3 years after diagnosis. Normally when people talk about lymphoma, they talk about them being low-grade or high-grade.
High-grade tends to be fairly rapidly growing, and because of that, they need treatment straight away. They’re usually okay to treat. Low-grade ones can rumble along for years without really needing any treatment but are usually harder to cure.
Mantle cell lymphoma is what they call intermediate, so it sits between the 2.
Sometimes it acts as a high-grade lymphoma and needs treating really, really quickly. Other times it acts very indolently or very slowly like a low-grade lymphoma. The best course of action there is to wait until it becomes more of a problem.
How did you get through this 3.5-year watch and wait period?
When I was originally told that, it was hard to get my head around. The general view in the press and if you talk to people is that it’s cancer, and the best way to deal with cancer is to treat it immediately.
Actually, with something like mantle cell lymphoma, that’s not really the case. If you look at the research that’s been done around this and the various treatments, what it shows is actually if you can afford to be on watch and wait, if it’s slow growing or indolent like mine was, then your outcome is better to wait than to start treatment straight away.
The amount of average time of remission you get after treatment is about the same, regardless of when you actually start. That’s why staging doesn’t make so much difference in this particular case.
That’s how I managed to get my head around that, thinking this was rather good. I would be able to get a few more months or years, potentially, of healthy life before I had to worry about treatment.
It also gives you the ability to prepare yourself for treatment when it starts.
You made the most out of the watch and wait period
What started out as, “Are you sure about this [watch and wait]?” turned into something that was actually fabulous.
I did some great stuff in those 3.5 years, things I’d been putting off doing that I finally got around to doing.
My pride and joy that lives in the garage downstairs is the Caterham 7 sports car. I’d wanted one of those since I was a teenager and it was one of those things I’d been putting off.
Eventually, getting the diagnosis convinced me to go out and get it. I’ve had a lot of fun in it in the last 4 or 5 years.

Switch to Active Treatment (Chemotherapy)
When did your consultant suggest a switch to active treatment?
At my regular consultant appointment in January 2018, it was the size of that swelling coupled with my right lump that encouraged my consultant to say, “Actually, it probably is about time now for us to start active treatment because it looks quite bulky.”
Given the other side of my neck, it ballooned in the space of 3 months what it had taken the left-hand side of my neck 3 years to get to that size.
I was given another bone marrow biopsy appointment. The result was still clear. I also had a PET/CT scan appointment. The results of this led to a final decision on February 14 to start active treatment, as the lymph nodes were very bulky in and around my neck. It was time to treat it.
Why were you re-staged to stage 2?
The swollen lymph nodes in my groin had gone, however, which resulted in me being re-staged as stage 2.
It was bizarre. When I was first diagnosed with the PET/CT scan in 2014 to 2015, the lymph nodes in the groin were nodules, so on the small size. When they restaged me with the PET/CT scan before I started treatment, it showed everything in the neck and shoulders. That was quite bulky disease at that point.
But what was in the groin had gone. If you looked at the doctor’s report, it said, “He’s stage 2.” I had gone back a stage.
That wasn’t the main thing that decided treatment. It was the bulkiness that got in my neck. The largest lymph node at that point was about 5.5 centimeters across, or 3 inches. It was pretty bulky, and there were multiple of them.

Nordic Protocol Chemotherapy Regimen
What was the overall chemotherapy regimen plan?
That was one of the first discussions we had at diagnosis. The standard of care in the UK for someone of my age, which is relatively young for mantle cell lymphoma at 50, is to go through what’s called the Nordic protocol chemotherapy, followed by a stem cell transplant from my own cells that they harvest.
What Nordic chemotherapy consists of is 2 different combinations of drugs that are given over 6 cycles of treatment, 3 or 4 weeks apart.
Describe Cycle A (Cycles 1, 3, 5)
The first cycle is what they call maxi-CHOP, with 4 different drugs, and that was given as an outpatient infusion. I was there for the day. It’s just a set of infusions.
There was a steroid tablet I had to take, prednisone. The others were given as bolus injections into the arm. They were fairly quick.
Describe Cycle B (Cycles 2, 4, 6)
The even-numbered cycles were where they gave me a high dose of something called cytarabine. They give it as 3 8-hour infusions.
Obviously, if it’s going to take 8 hours for you to take one of those infusions, you’re going to be there for a while. What they do is keep you as inpatient for 3 days.
The constant drug through all cycles: rituximab
The other drug that’s been constant through there is also my maintenance drug post-transplant. It’s called rituximab, which is a monoclonal antibody. That’s the terminology for that. It’s part of the cocktail.
They didn’t give me that in the first cycle because if the disease is bulky, rituximab can have quite an interesting impact on it in that it can be too effective.
People potentially struggle with it, so they left that until the second cycle. Then they gave me the rituximab really slowly. It was only over time as they figured out my tolerance for that drug that they actually sped that part of the treatment up.
Now when I go in for my rituximab maintenance every couple of months, it literally takes 10 minutes or so to get that drug as an injection.
The first time I got it, the infusion was probably about 4 or 5 hours. They treated that one with a fair amount of care.
You skipped rituximab first cycle, added on after last cycle
Then the sixth rituximab infusion, they gave me as a standalone treatment after the sixth cycle was finished. I got 6 lots of the rituximab.
You got infusions through the IV (cannula) and also PICC line. Which did you like more?
That’s interesting in itself. It’s different in hospitals across the country. Mine recommended that because I had reasonably good veins, I could go IV.
There’s a tradeoff with something like a PICC line or Hickman line versus a cannula. If you got a PICC line, there’s always a chance of infection. The way my medical team preferred to give it was, if they could, they would give it through a cannula.
I went through that and had a cannula put in for the first 5 cycles of chemotherapy. On the fifth cycle, I’d gone through having the cannula putting in. They managed to give me the rituximab and the first 2 doses of cytarabine.
But then, because I’d slept overnight, the cannula had moved. They found it then impossible to put the cannula into me. The way they finished the fifth cycle was to put a PICC line in me, which was all right. I had the PICC line for the end of the fifth and the sixth cycle.
It was actually quite nice having it because it was easier for them to take blood and all the rest of it. That was it. I don’t like needles, but I didn’t mind getting the cannula in.
You eventually moved to a Hickman line
That PICC line had to come before I had my stem cell harvest because what they give you at my hospital. They put in a Hickman line into the chest. That has 2 lumens in it, or 2 filaments, rather than the 1 that they would give the chemotherapy through.
They needed the 2 lumens to move through the stem cell harvesting machine. They left that in for the stem cell transplant as well, where they also gave me chemotherapy before.
Chemotherapy Side Effects
How did the 2 cycles compare in terms of side effects?
Talking to other people who’ve been through this as well, I think I’m in the minority in that I coped better with the cytarabine part of the chemo (Cycle B) than the maxi-CHOP (Cycle A). For me, the maxi-CHOP after the third cycle, I lost most of April trying to recover from that.
I wasn’t keen on the CHOP part of it. The cytarabine was far easier for me. Again, other people I spoke with said, “No, the CHOP part was really easy. The cytarabine was what I couldn’t stand.”
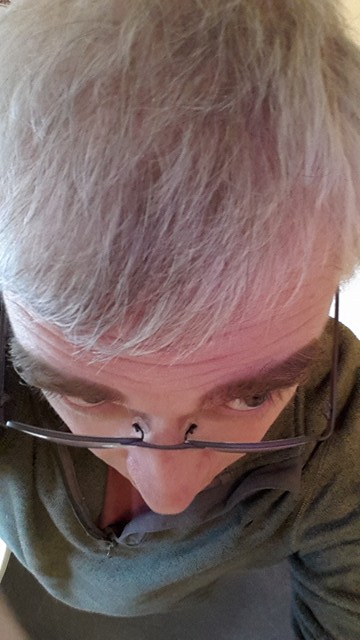
Describe the hair loss
On the whole, I probably got off lightly. The one thing they guarantee as a side effect of this treatment is hair loss. My hair started to come out between the first and second cycles. It was starting to thin just before I went in to have my first Cycle B chemo.
My hair was a lot thicker 5-6 years ago than it is today. I did lose all of my hair, including my eyebrows, which is still quite prominent today. I had lost everything about the time the second cycle had started, 3 or 4 weeks into treatment.
After I had the 6 cycles of the Nordic chemotherapy, there was a couple-month gap before I started the stem cell transplant phase, so my hair had started to grow back by the time I went in for my stem cell transplant.
Of course, the chemotherapy drugs they give you before the stem cell transplant remove the hair again. I lost my hair twice, in fairly quick succession.
It didn’t really bother me, to be honest.
The only thing that bothered me was that my head was permanently cold, so I was forever wearing a wooly hat, even when it was during late summer to early fall. It felt cold and drafty most of the time.
»MORE: Dealing with hair loss during cancer treatment
How were the other side effects of chemotherapy?
Summary: taste change, weight loss, fatigue
It hits differently for different people. The taste of food changed; I got a metallic taste. I was still able to eat and kept eating all the way through, but what I could taste and how I could taste it was different. I found things like strongly tasting foods and drinks were far better for me.
I went off things like coffee and tea, which I drink gallons of normally. Instead, I went to things like this Scottish sugary drink, diet Coke, that kind of stuff.
Anything that was more strongly tasting was better.
I didn’t lose a huge amount of weight through the process either. I started 93 kilograms (205 pounds) when I started treatment. My lowest, I was about 80 kilograms (176 pounds), so I dropped about 13 kilograms (29 pounds). I’m back up to the weight I was when I started treatment.
Fatigue, certainly. I felt pretty washed out after each of the treatment cycles. Usually it would kick in a couple days afterward and would persist for maybe a week or 2.
»MORE: Read about other patients’ side effects
Describe how you’d feel during the 3-week gap between chemo cycles
The 3-week gap between the cycles felt like the first week after treatment was going down the dip, not feeling terribly good. The second week, things started to stabilize.
By the time you got to the end of the cycle in the third week, I felt pretty good again. You get used to going on that roller coaster all the way through the process.
I was fortunate. I didn’t suffer from any infections or anything like that through the process. I got away with it fairly lightly, I think, on the whole.
We took pretty good precautions at home. Lots of hand washing and making sure people weren’t in the house with me. Actually, it’s like living now during COVID! We got a preview of it a couple years ago.
It wasn’t particularly pleasant. It’s not something I’d want to go through again.
But looking back on it, just from talking to other people who’ve been through similar treatments, I do think I got away with it a bit lightly, especially for that stage of using the chemo.

When did you know treatment was working?
Something that was very noticeable was the lumps on my neck had started to shrink pretty quickly after the first cycle. They weren’t visible by the end of the third cycle.
Then a PET/CT scan between cycles 5 and 6 showed no evidence of the disease at that point. It was pretty effective stuff, that’s for sure.
How did you process news of no evidence of disease?
It was a great sense of relief. I went into treatment knowing that that treatment was pretty successful at putting people into remission.
I think the stats showed something like 96 or 97% success of either achieving complete remission or a good partial remission, so we knew it would hopefully be effective.
I’d read stories also of people where their lumps magically disappeared after 1 cycle and them feeling really great. Of course, mine didn’t. Mine took a little bit longer to go down.
Actually, I was probably a bit more worried in Cycle 2 and Cycle 3, wanting to know if they were really shrinking. My wife, Jane, would say, ‘Yes, they are.’
Stem Cell Harvest (Autologous Transplant)
Describe the stem cell harvest
I finished Cycle 6 of chemotherapy and was basically booked in about a week or so after that into a bigger hospital to have the stem cell harvesting. They take your Hickman line and filter the blood through this machine. There was a big centrifuge that sat in there.
The pink liquid in the photograph (below) is the stem cells that they harvested. The liquid on the left with the brown color, that’s plasma. They also take that chrome and mix the plasma with the stem cells together before they give it back to you as part of the transplant.
That whole process of being on the machine took about 6 hours or so for them to harvest the stem cells.

It can take a while before you’re ready for the harvest
They did the stem cell harvest on a Friday. The way that they organize it is they say that it could take up to a week to get enough stem cells from you.
When I showed up to the hospital on the Monday morning before, they took my blood and took one look at me and said, “There’s no way we’re putting you on that machine because you don’t have any white blood cells, you’re anemic, and your platelets are too low as well.”
The first 2 days, I went back and forth to the hospital for them to harvest. They would give me blood and platelet transfusions instead to make me better, because the one thing the chemo does is it really knocks your blood counts down. By the second day, I was not doing too badly.
You had to get injections to increase stem cell count
The other thing they’re looking for before they harvest the stem cells is that there are a sufficient number of them there to harvest. There’s a blood marker that says whether it is.
They give you injections (filgrastim/Neupogen or pegfilgrastim/Neulasta), which stimulate the production of stem cells.
I’ve been taking those since the end of the sixth cycle, injecting myself nightly with the shots through the cycle and through the week I was in that hospital trying to harvest cells.
Those counts only came up fairly slowly. I don’t remember the level, but it needed to be over 10 before they’d hook you up to the machine. By Thursday, I’d hit 9.6, which was still too low for them to put me on the machine.
At that point, they called out what they call “the big guns,” which is an injection called plerixafor (Mozobil). They gave it to me on the Thursday.
When I went back on Friday, that mark was up at about 23 or something like that. That’s when they put me on the machine, quickly, before the stem cells went.
That seems to be quite a typical process. Very few people actually turn up for stem cell harvest and tick all the boxes so they can do them on the first day.
I was probably a little bit slower than usual, but they got them, and they got the right quality of them, as well as the right quantity. I think they were aiming for a couple million of these things, and they got about 2.8 million or something like that.
It’s like Groundhog Day. They take the blood test every day, but they do get there in the end!
You asked for a month break before the stem cell transplant
I really didn’t want to carry straight through. Having August was really nice. We managed to get away for a week on holiday — not too far from home — in a beautiful part of the country.
It was just nice to recharge and not be a patient for a month or so.
Conditioning Chemo Before Stem Cell Transplant
Describe the BEAM induction chemotherapy
That was 7 days running of different chemotherapy drugs. BEAM is the acronym.
- B is carmustine (BiCNU)
- E is etoposide
- A is cytarabine (Ara-C)
- M is melphalan
How well did you tolerate BEAM chemo?
The really nasty one is that last one, the melphalan. They give that to you the day before you have the transplant. The point of that whole chemo regimen is called conditioning chemotherapy.
They’re trying to kill off any last trace of the lymphoma, and so they do that by throwing 7 days of chemotherapy at you straight. The aim is to move all that cancer out.
As a consequence of that, what happens a few days after you finish those bags of chemotherapy drugs is your white blood cell counts drop to zero, so you’re incredibly vulnerable to infection.
The way they do it in the UK, which is slightly different from some centers in the States, is that it’s done completely inpatient. You’re given a room in isolation for the 3 weeks or so that the transplant process takes.
They don’t want you to wander outside too much or have too many visitors. They try and keep everything as clean as possible. The 3 weeks I was in there, it was a bit like living on a plane for 3 weeks. There was that sort of noise.
What helped make the weeks in the hospital better?
The best investment I made was to buy a set of noise-cancelling headphones to wear and sleep in. Without those, I probably would have gone madder than I am now!
It was a great way of getting through the noise of the air filtration system. I’m probably making it sound worse than it was, but it was a constant buzzing. It’s a whiny, drony noise.
Autologous Stem Cell Transplant
Describe the actual stem cell transplant (SCT)
After they wipe everything out, they give you your stem cells back. It’s actually a bit of an anticlimax.
It took about 30 minutes or so in total [for the transplant]. At that point, they tell you it’ll get really bad a few days after the stem cell transplant, when the blood cell counts drop really low.
I was actually feeling pretty good at that point. I was eating and drinking okay, felt okay and like myself. Sure enough, everything hit about 3 or 4 days after the transplant.
What were the side effects after the transplant
I had some fairly nasty side effects from the chemo drugs because it affected my windpipe, so it was pretty painful and sore. I also developed an infection. In the middle of the night, it was a case of them giving me a chest X-ray.
It took them 3 X-rays to get it right. Apparently I’ve got really long lungs and didn’t fit on the X-ray plate. They gave me intravenous antibiotics.
If I look back at the diary that I kept, Day 3 and Day 4 after the transplant felt pretty horrible. They were not pleasant days to live through. By Days 5 and 6, I’d started to perk up a bit, and I was discharged on Day 11 after the transplant.
Altogether, I was in the hospital about 20 days in total, which is pretty fast-going. They think the stay will be, on average, about 20 to 21 days. Some people are in for 5 weeks. Not many people escape much earlier than I did.
Any more guidance on how to make the long hospital stay more palatable?
Take things that make you feel comfortable. I took things like blankets and dressing gowns from home that weren’t too hospital-y. Books, DVDs, box sets.
There was a BBC detective series in the 70s and 80s called Shoestring, which only ran for 2 seasons. I consumed all of those. I rewatched other programs, just stuff to keep myself entertained. Because I was in a room by myself, I could entertain myself.
I slept a lot as well. I did my exercises, too. All those sorts of things to get a routine into the day. Moving away, making sure I was still mobile.
They give you a lot of good advice before you go into the hospital. It’s about following that advice but also thinking, “I’m going to be locked up in here for 3 weeks. I’m going to take things that I want to have. Things that remind me of home, maybe a couple of soft, cuddly toys like Eeyore.”
Anything that makes it feel a little bit less like a hospital room and more like a hotel room.
Recovery after Stem Cell Transplant
How was recovery at home post-transplant?
The medical team keeps pretty good track of you for the first 2 to 3 weeks after the stem cell transplant. About a week later, I was back at the hospital for them to remove my Hickman line that I had put in for the transplant.
I was also still in contact with the team that I’d had at my previous hospital. I went and saw them around 2 to 3 weeks after the transplant.
My nurse also came to see me at home once a week when I had the Hickman line in, before they took it out, to make sure it was clean. They keep pretty good tabs on you and also give you an emergency card.
If I felt the slightest unwell, thought I had a temperature or anything, I’d call that number that would get me straight through to the hospital specialists who treat lymphoma patients.
If they’re the slightest bit worried, they’ll take you in overnight and look after you.
I only had to use that once. It was sometime after transplant. I went through my counts dropping quite a bit. I’d also maybe eaten something that made me feel unwell, so they kept me in for a night.
The support systems are there, and it’s about using them and making sure that you’re comfortable in doing that.
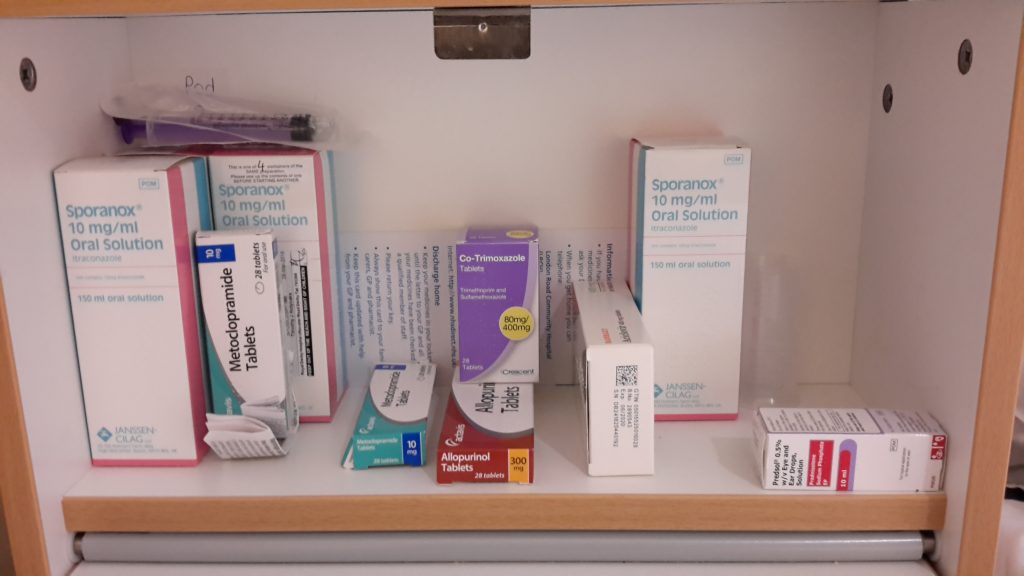
Describe the maintenance chemo you’ve been on since the stem cell transplant
When I was originally diagnosed with mantle cell lymphoma, the process was to do the 6 cycles of Nordic chemo, do the stem cell transplant, you’re done.
What happened in between was research that showed the benefit of, after the stem cell transplant, having maintenance rituximab every couple of months for 3 years, which is the process I’m going through right now.
Every couple of months I get a rituximab injection. It takes about ten minutes to administer. That helps to keep on top of the MCL.

Reflections
When did you stop and return to work?
I started chemo on the 1st of March 2018 and went back to work the second or third week of January 2019.
I went back to work just under 11 months in total.
My employers were terrific about it actually. The insurance also helped, so there hasn’t been any financial worry with [paying for treatment]. I recognize I’m fortunate in that, in terms of the employee scheme I’ve got.
How did you family take the cancer diagnosis and treatment?
They reacted pretty well. I got an awful lot of support from the wife and from my 2 daughters as well. That was good. In some ways, because my wife has also recently had cancer treatment for a different cancer, I found it much easier to be a patient than I have been to be a carer or caregiver, if I’m perfectly honest.
They were there for me. The support was great from them, and particularly also from friends and work colleagues. I was fortunate in that I had some support network.
Having sat both sides of it now, I much prefer being a patient to being a carer or caregiver. It’s much easier to cope with your own stuff.
What support was the most helpful to you?
It was just people staying in touch with me, whether it was friends or through work. The flowers were sent from people at work when I was going through one of my lowest points of the initial chemotherapy, so about Cycle 3 or Cycle 4.
That was terrific. It was completely unexpected, but it was lovely.
I was getting some messages of support. People were popping up and saying, “How was I? How was I coping?” Those socks are from some friends of mine for a birthday. They’re called Happy Socks! They’re great. I still have and wear them.


It was just nice to have those socks in the hospital because they were different from the standard black and gray socks I’d always worn to work. They also made the nurses smile.
I didn’t want to be surrounded by people going, “Aww, no.” I just wanted people to treat me as normal. One of the most amusing things that happened was one of my colleagues at work came in and saw me on the morning that I was having trouble with the cannula during my fifth cycle.
He’d come to just pop in and say hello, bring me some bars of chocolate. He ended up staying with me for most of the day because it was like, “We need to put in this PICC line, we need you to step outside for a second.” So he did; he stepped outside.
Then it was X-rays to make sure the PICC line was in properly. It wasn’t, so they wheeled me back in and down again. It was great to have him around actually, just through something like that.
It was nice to know people hadn’t forgotten me, but also not being completely overwhelmed by people as well. It was literally, ‘Talk to me about anything other than what I’m going through.’
I’ll talk about what I’m going through, but don’t give me advice about what to eat, drink or what have you. I’ve had plenty of that from medical experts, and I know what I like.
Has the cancer diagnosis and experience changed your life perspective?
That’s a really difficult question to answer. It has impacted possibly what I will put up with and what I won’t put up with. The job that I do means that I’m customer and client facing a lot of the time. I work a lot with our sales people as well.
Sales people can be a breed apart at times. I guess I’m less prepared to put up with some of the nonsense today than I was maybe 5 or 6 years ago, before I went through cancer treatment. But I’ve always had a similar sort of outlook on life.
I’m probably more conscious about trying to squeeze as much out of my time as possible as well. And not putting off things that I wanted to do.
That car is a really good example of that. It goes back to the TV series “The Prisoner,” in the opening titles for that. They show the star driving one of those cars.
That was where I first fell in love with the car, when I was a kid in the 70s watching the show. It was always like, “It’d be really cool to have one of those!”
Then, of course, was life, the wife, family, kids. Everything else sort of gets in the way. When I was diagnosed, it was like, ‘Right. When am I going to do what do I want to do?’
That was one of the things that was on the list, getting a hold of one of those cars, buying it and driving it. It’s been just great!

Do you ever experience anxiety about getting the cancer again?
I must admit I try not to think too much about it. The prognosis with mantle cell lymphoma and the treatment I’ve gone through along with the stem cell transplant is people inevitably or invariably relapse at some point.
The point of doing that watch and wait period, having the most rigorous chemotherapy regime I could tolerate based on age, then going through the maintenance treatment is to prolong that remission.
Again, mantle cell lymphoma is one of these diseases that’s a relatively recent diagnosis. I think it was diagnosed as a separate type of lymphoma in the 90s, something like that.
If you look back at the average survival time for people with MCL going back even a decade or a bit more, people were talking about average survival times of about 3 years or so.
It’s different now, clearly. I’m 6 years past diagnosis and still going strong.
Doctors understand this disease better and its progression better, along with the various subtypes within MCL and different ways that it presents. The treatments have gotten better. The most recent research suggests that the average remission time for people like myself is maybe somewhere between 7 and 13 years.
That’s a long time. A lot can happen in that time. Some of the newer treatments used for relapse are like BTK and ibrutinib. They are now showing great success in putting people back into remission after initial treatment.
Of course, there’s the CAR T-cell therapies as well starting to be developed. There’s also CAR T trials happening in the UK. That opens up other avenues of treatment for people who relapse.
The way I’m looking at it now is rather than it being a life-ending condition or life-threatening condition, it feels more like a chronic condition that I live with and that I manage.
The only thing I do get is a little bit of fatigue. I manage that by working 4 days instead of 5 days a week. I also try to make sure I don’t overdo it, because if I do, I tend to pay for it a couple of days afterwards. That’s the way I’ll carry on approaching it.
Last message to other patients or caregivers
One of my bits of advice is don’t give advice. Life is what you make it to a large extent. The way I’ve approached this all the way through is one of curiosity.

It’s about talking to the medical experts about what you’ve got, what the treatment options are and trying to take that in.
One of things I always did was take my wife to appointments so she could take notes, and I’d make notes as well.
It’s about using that interaction with the medical professionals for me to understand as much as what was going on as possible. Try to prepare yourself for each individual step. There’s lots of good advice out there.
Not only your own medical team, but organizations (Lymphoma Action in the UK) that provide good booklets and information about lymphoma and the various types of lymphoma. They act as a patient support and patient advocate group as well.
It’s those sorts of organizations that really help patients get through the process. They certainly helped me get through the process as well. It’s about getting good advice.

Inspired by Tim's story?
Share your story, too!
Mantle Cell Lymphoma Stories
Cherylinn N., Mantle Cell Lymphoma (MCL), Stage 4
Symptom: None
Treatments: R-CHOP chemotherapy, rituximab
Stephanie R., Mantle Cell Lymphoma (MCL), Stage 4
Symptom: Elevated white blood cell count
Treatments: 6 months of rituximab + ibrutinib, 4 cycles of hyper-CVAD chemotherapy
Jason W., Mantle Cell Lymphoma (MCL), Stage 4
Symptoms: Hives, inflamed arms
Treatments: Calabrutinib, Lenalidomide, Rituxan
Bobby J., Mantle Cell Lymphoma (MCL), Stage 4
Symptoms: Fatigue, enlarged lymph nodes
Treatments: Clinical trial of ibrutinib + rituximab, consolidated chemo of 4 cycles of Hyper-CVAD




