Melissa’s Life After DLBCL Relapse: Finding Strength in the In-Between
Melissa’s experience with diffuse large B-cell lymphoma (DLBCL) isn’t just about scans and chemotherapy but what comes after relapse. Diagnosed at just 30 years old, Melissa never imagined the lump in her breast would lead to a life-altering diagnosis, let alone a relapse nearly six years later. DLBCL, aggressive and fast-growing, quickly reshaped her world—twice.
Interviewed by: Taylor Scheib
Edited by: Katrina Villareal
Her first encounter with DLBCL was frustrating and terrifying. Doctors initially diagnosed her with an infection, but the prescribed antibiotics made everything worse. When she ended up in the ER, a CT scan finally led to a biopsy and a phone call that changed everything.

Melissa’s initial treatment was intense. Six cycles of R-EPOCH chemotherapy and 20 rounds of radiation therapy left her physically and emotionally drained. Side effects like bone pain and severe fatigue made everyday life nearly impossible. She pushed through but never stopped feeling afraid, especially before every scan. That lingering fear of relapse haunted her, even when she was trying to live as fully as possible.
And then the relapse came.
Just after Christmas 2023, a painful lump under her arm set everything in motion again. This time, Melissa had to undergo a stem cell transplant, preceded by grueling high-dose chemotherapy. The process was not just physically taxing but also mentally and emotionally overwhelming. From losing her job to navigating endless appointments, to being isolated due to a wiped-out immune system, life after relapse never went back to “normal.”
Melissa describes feeling deep depression after her transplant. She expected to feel joy, but instead, she felt stuck. Recovery wasn’t just about healing her body; it meant rebuilding her mental health, confidence, and ability to trust her body again. Slowly, she emerged. She reconnected with family, leaned on her incredible support system (shout out to her sister!), and began doing the things that bring her joy.
Melissa continues to deal with anxiety around scans (scanxiety), but she’s more focused on living than worrying. She emphasizes the importance of self-advocacy, especially when less likely diagnoses, like DLBCL, aren’t immediately considered. Her story is an honest, empowering reminder that survivorship doesn’t mean everything is fine. Life after relapse is complicated, but it’s also filled with second chances and deeper appreciation for the everyday.
Watch Melissa’s story to find out more about:
- What gave her the strength to keep going when everything changed
- When she realized that her voice mattered
- Who became her rock through every scan, treatment, and tough moment
- Why she decided to share the hardest parts of cancer
- How she rebuilt her life after her DLBCL relapse
- Name: Melissa B.
- Age at Diagnosis:
- 30 (relapsed at 36)
- Diagnosis:
- Diffuse Large B-cell Lymphoma (DLBCL)
- Symptoms:
- Lump in the left breast
- Persistent rash (started near the belly button and spread)
- Intense fatigue and energy loss
- Treatments:
- Chemotherapy: R-EPOCH
- G-CSF: Neulasta (pegfilgrastim)
- Radiation therapy
- Surgery (to remove scar tissue and necrosis)
- Autologous stem cell transplant

Thank you to Genmab and AbbVie for supporting our independent patient education content. The Patient Story retains full editorial control.
This interview has been edited for clarity and length. This is not medical advice. Please consult with your healthcare provider to make informed treatment decisions.
The views and opinions expressed in this interview do not necessarily reflect those of The Patient Story.
- Introduction
- When Something First Felt Off
- I Experienced Other Symptoms
- Finding Out I Didn’t Have an Infection But Needed a Biopsy
- The Moment Everything Changed
- My First Treatment Plan
- What Life Was Like Between My Original Diagnosis and Relapse
- A Second Lump Appeared
- Finding Out the Cancer Was Back
- The Only Time That I Ever Feared Relapse Was Right Before a Scan
- Navigating DLBCL Relapse with My Loved Ones Was Hard
- The Plan Moving Forward
- How I Prepared for My DLBCL Stem Cell Transplant
- What Recovery Looked Like After My Stem Cell Transplant
- How Treatment Impacted My Day-to-Day Life
- What Survivorship Looks Like for Me
- I Still Experience Anxiety Before Scans
- What I Want Others to Know
- Why Self-Advocacy is So Important
I noticed a lump in my left breast… I went to my primary doctor. She ran some blood work, told me I had an infection, gave me some antibiotics
Introduction
I was diagnosed with diffuse large B-cell lymphoma twice. The first time was in 2017 and unfortunately, I relapsed in January 2024.
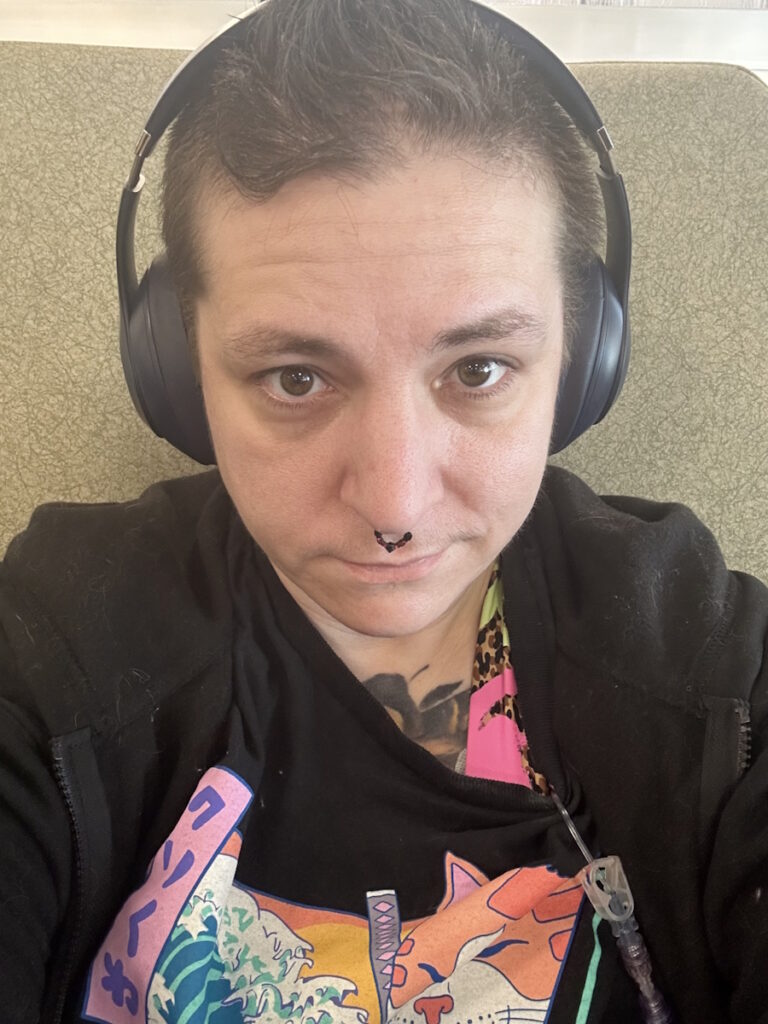
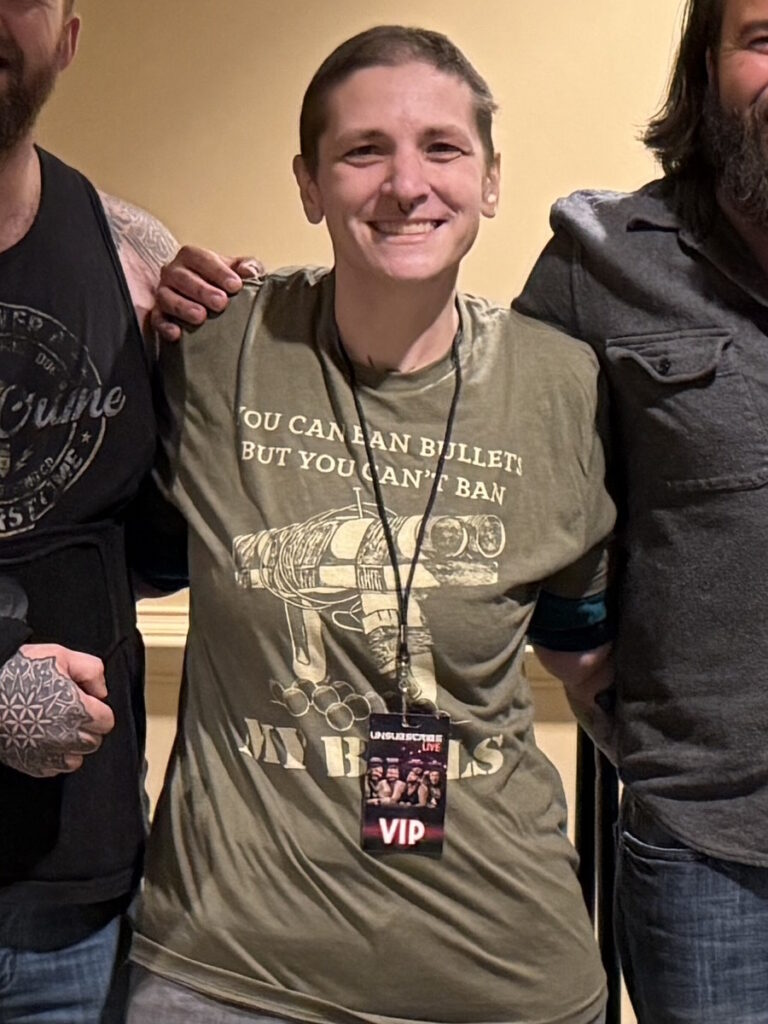
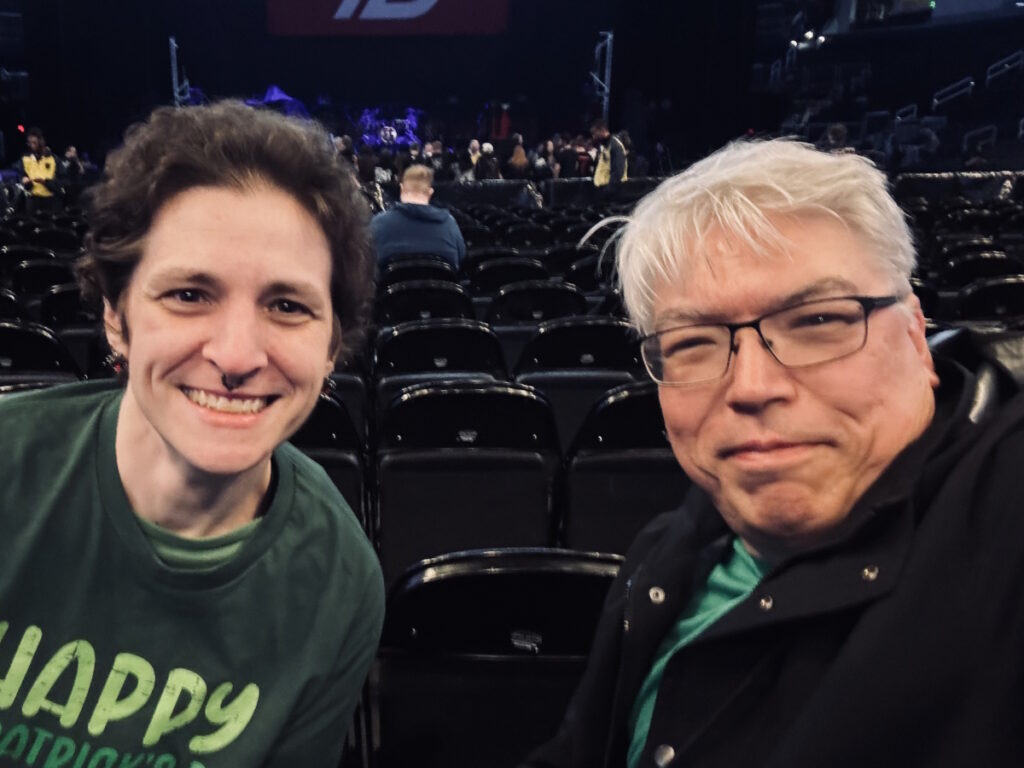
I’m a concert junkie, so I go to as many as I can afford to. I love tattoos and have quite a few. I have five cats who are my children. I love them. I like riding roller coasters. I love going to karaoke. I play video games. Sometimes, I enjoy relaxing and watching a movie.
When Something First Felt Off
I noticed a lump in my left breast. The kind of cancer I have is very aggressive and grows very quickly, so it went from a little lump to twice the size within a couple of months.
I went to my primary doctor. She ran some blood work, told me I had an infection, gave me some antibiotics, and sent me home. She even joked at one point and asked if I had a breast implant on one side because it was so much larger. That joke left a bit of a sour taste in my mouth.
I took the antibiotics, but I got worse. I was freaking out, so I called my mom and she said, “Go to the emergency room. They’ll probably lance the infection. You’ll be fine.”


I Experienced Other Symptoms
I got a bad rash, which is very common with lymphoma. It started around my belly button. At first, I thought I was allergic to the metal in my belt buckle. Then it started going down my back and my legs. I thought I was allergic to my laundry soap or body wash, so I started switching everything to unscented. I thought it was an allergy, so I put cortisone cream, but nothing was working.
I was also incredibly tired all the time. I didn’t want to do anything. All I wanted to do was go home to sleep. I wasn’t the sleepy kind of tired. I was drained and had no energy, so I didn’t want to do anything. I thought I was experiencing the usual side effects of having an infection. I wasn’t having fun. I was going to bed super early. I was taking naps. The rash didn’t hurt, but it itched and there was nothing I could do to relieve the itching.
I didn’t think it was serious. I was 30 years old. Cancer doesn’t cross your mind at that age.
Finding Out I Didn’t Have an Infection But Needed a Biopsy
When I took the antibiotics and my symptoms got worse, I got scared. The doctor told me what to do, which I did, but it didn’t work, so I decided to call my mom. My mom was trying to calm me down, telling me everything was fine, and to go to the emergency room so they could take care of me.
They did a CT scan. When the doctor walked in and said, “It’s not an infection,” cancer never crossed my mind. They gave me a request for a biopsy and told me to have it done immediately. I thought it was weird. At the time, I didn’t think it was serious. I was 30 years old. Cancer doesn’t cross your mind at that age.
I set up an appointment and, luckily, they had one available in a couple of days. When he walked into the room, he looked at me and said, “Did they tell you that you might have breast cancer?” Cancer wasn’t even in the realm of possibilities and that’s the first thing he said to me. I started bawling. He left the room and the nurse came over and comforted me.
When he came back, he explained what he was going to do. He showed me the giant needle that they were going to use to collect the sample for the biopsy. The procedure was ultrasound-guided, so I watched everything. He was professional, but for subsequent things that I needed a surgeon for, I specifically requested not to have him again.

The Moment Everything Changed
I heard back about a week later. It was a Monday morning and as I was getting ready for work, I got a call from Virginia Oncology Associates. They said, “We need to schedule an appointment.” I said, “May I ask why?” They said, “Oh, have you not talked to the surgeon yet?” I said, “No, I hadn’t heard from them yet.” It was an awkward conversation.
As I was on the phone with them, I got a call from the surgeon. He doesn’t have me come into the office but tells me over the phone. He said, “It’s not breast cancer, but you have this other type of cancer.” It took a minute before the tears began to fall. I went back to the other call and made the appointment with the oncologist.
After I hung up, I called my boss. I had been telling my boss about what was going on and my boss said, “You’re not coming to work today. Go be with your family.” I went to my mom’s house and shared the news. It was difficult to tell people.
I knew lymphoma was a type of cancer, but I didn’t know specifics about it. People are aware that cancer exists, but the various types aren’t widely known. I had no idea what to expect. I didn’t know what it would look like. I wasn’t sure I would be okay. I don’t know what kind of treatment. I knew nothing.
Every time I got a scan, I would get nervous a week or two before getting one.
My First Treatment Plan
My first treatment regimen was R-EPOCH. I had a port put in and I was in the hospital to receive chemotherapy for 24 hours over four days. They would give me 15 minutes off in between bags of chemo to take a shower. I would get premeds to try to help with the side effects and then I would get hooked up to another bag. On day five, I received rituximab. I would go home and get two weeks off in between cycles before I had to go back and do it again. I had to do that six times.
After each round, they gave me a shot of Neulasta (pegfilgrastim), which is designed to boost the immune system. For me, it felt like every bone in my body was breaking at the same time. It hurt badly. I took pain medicine, but nothing worked.
After chemotherapy, I did 20 rounds of radiation.
(Editor’s Note: R-EPOCH is an abbreviation for a chemotherapy combination used to treat certain types of non-Hodgkin lymphoma. It includes the drugs rituximab, etoposide phosphate, prednisone, vincristine sulfate [Oncovin], cyclophosphamide, and doxorubicin hydrochloride [hydroxydaunorubicin]. -National Cancer Institute, )

What Life Was Like Between My Original Diagnosis and Relapse
Anytime I got a rash or noticed anything off, I freaked out. I ended up getting another lump on my right breast at one point, so I went to the surgeon, but it turned out to be a fibroid. Everything was fine, but with every little thing, I was terrified.
I tried not to let it overwhelm me too much. Every time I got a scan, I would get nervous a week or two before getting one. I would freak out that something was going to show up and, thankfully, nothing ever did.
My very first follow-up scan showed scar tissue and necrosis, so they had to do surgery. After that, everything was perfectly fine. Anytime I would see scan results, I would always ask, “What does this mean? Is this bad?”
I try to live life to the absolute fullest, enjoy myself, and not let the little things bother me. I do things I’ve always wanted to do. I’m planning a trip that I’ve always wanted to go on. I’m going to start doing things on my bucket list because I think I’ve earned it.
I kept trying to tell myself that I would be fine. The first time I got diagnosed, I believed that I was fine. Now, it’s hard to tell myself that I would be fine because the first time, I wasn’t.
I was still hopeful. Though in the back of my mind, I knew that it could be DLBCL again.
A Second Lump Appeared
Right before Christmas, I started noticing a painful lump under my right armpit. I decided to have it checked because it hurt so badly. I went to the ER the day after Christmas, but they did nothing. They didn’t scan it, test it, or do blood work. I waited for four hours only for the doctor to see me for about 45 seconds and say, “Go see your surgeon.”
At that point, I was having scans every two years. I started having them every six months, then every year, and then every two years. I had a scan about eight months prior, but there was nothing. Again, this disease pops up and grows very quickly, so it could be nothing and then a week or a month later, there it is.
I had always been told that tumors do not hurt, which is true. Tumors themselves do not cause pain, but this lump hurt badly, so I thought maybe it was something else. Even when I went to see the surgeon, he agreed. He said the fact that it hurts is a good sign.
I was still hopeful. Though in the back of my mind, I knew that it could be DLBCL again. But I was past the five-year mark, almost at six years.

Finding Out the Cancer Was Back
Luckily, I was able to see him within a week. He did a biopsy, but this time, instead of the giant needle, they removed a lymph node from under my arm.
I got my biopsy results on MyChart. I was at work when I got the notification. I decided to take a look. When I read it, I thought, “This can’t be right. Are these my old test results?” I checked the date and saw that it was current. Then I broke down right in front of my boss. We talked for a little bit and he told me to go home, so I left for the day.
I called the surgeon’s office and, luckily, he called me back pretty quickly. He said, “It wasn’t what we were hoping for.” They gave me a referral back to the oncologist. I originally saw the same oncologist, but because they recommended that I do a stem cell transplant, I had to go with a different doctor.
I wasn’t ready to die, so I was going to do whatever the doctor told me to do, no matter how bad it sucks.
The Only Time That I Ever Feared Relapse Was Right Before a Scan
The only time that I ever feared relapse was right around a scan. I was afraid they would find something. Other than that, I tried hard not to think about it too much. If you’re constantly thinking about it and worried you’re going to get it again, it’s going to eat you alive.
They said to keep an eye out for the symptoms that I had. They also said that relapse occurs mostly within the first two years. It can come back after that period, but the first two years are the critical time.


Navigating DLBCL Relapse with My Loved Ones Was Hard
After I came home, I called my husband immediately, then called my mom. I was crying the whole time. I was scared. I didn’t know what was going to happen. Was it going to be as brutal? Was it going to be more aggressive because it’s the second time? How is this going to progress?
I had moments at night when I’d be lying with my husband and I would break down and say, “I can’t do this. I don’t want to do this. This isn’t fair.” But at the end of the day, I wasn’t ready to die, so I was going to do whatever the doctor told me to do, no matter how bad it sucks, and I’ll get through it. I still have a lot of life left to live.
I had a couple of close friends who were very supportive. My older sister lives 20 minutes from me and she is my absolute best friend in the entire world. She was there when I did chemotherapy the first time. She was with me in the hospital almost every morning. We would have a list of questions and when the doctor would come in, we would talk about them together. She went the second time when I did the stem cell transplant. She was there all the time. She is my ride or die. I love her to death.
‘There are different second-line treatments for relapse and stem cell transplant is one of them. We feel you’re a good candidate for it.’
The Plan Moving Forward
I talked to Dr. Burke first and he said, “There are different second-line treatments for relapse and stem cell transplant is one of them. This is going to be your best course of treatment because not everybody qualifies for that. We feel you’re a good candidate for it. Your body is strong enough to handle it, so we want you to do this. We think it’s your best chance of getting rid of this for good.”
They went in-depth. He introduced me to the new doctor who took over from there, who was also wonderful. His name is Dr. Simmons. He’s an amazing man. He’s very detailed. Anytime we went over anything, he would write it out. He drew charts, which I always appreciated because I’m a very visual person.
My medical team was pretty thorough. When they recommended it to me, they explained it in detail. They told me what was involved, how it worked, and how it’s recommended for certain situations.
I also learned not to research too much because though the Internet is full of knowledge, it’s also full of crap. When you try to Google your symptoms, everything comes up as cancer. It’s the same thing once you already have cancer. Everything looks awful. You’re going to die. You’re going to have all these horrible side effects. I limited my research because when I didn’t, I scared the crap out of myself.


How I Prepared for My DLBCL Stem Cell Transplant
To prepare for the process itself, they had to do a bone marrow biopsy to make sure my stem cells were cancer-free and everything was fine. I had to have my entire body examined from head to toe. I had to get dental clearance. They had to make sure that my body was strong enough to handle the chemotherapy and the transplant.
Before they do the transplant, you have to undergo six days of high-dose chemotherapy to wipe out your system because the transplant is like a restart. You have to make your body handle that because it’s hard. I was sick.
When they take out the stem cells, you sit in a room and can’t leave for about six hours, where they hook you up to a machine. I had the port on one side and a big catheter with tubes hanging out on the other side, which I had for weeks beforehand and had to be covered with a bandage.
The machine takes your blood out. It has two tubes. In one tube, the blood comes out and goes through the machine. It takes out the stem cells and then, through the other tube, the blood goes back. Someone comes in once in a while to check on you. Once they have your stem cells, they send them off.
They have to test the stem cells, make sure that they have enough and that they’re good to use. If they don’t get enough, you have to go back another day or however many days until they get enough. Thankfully, I got enough from a single apheresis session because it was horrible having to sit in a chair for six hours. It was so boring and the machine is loud.
Then you’re admitted to the hospital to undergo chemo. When it’s time for the transfusion, they bring your stem cells, which are frozen in a bag, and thaw them out. But it’s still cold and I could feel it while it was entering my body. The transfusion only took a few hours. They monitor you in the hospital for a while. I was there for two and a half weeks.
I didn’t know that when you do a stem cell transplant, it resets your immunity, so I had to get all of my immunizations all over again.
What Recovery Looked Like After My Stem Cell Transplant
Recovery took a while because I was in the hospital for two and a half weeks. I barely got out of bed, so it messed up my back. I couldn’t walk very well for a while. I had to go to physical therapy and a chiropractor for several months to try to regain some strength and fix my back.
I had to quarantine for a while until my immune system started rebuilding. I had to stay away from people. I was on so many medications. I recently stopped taking an antiviral.
The first anniversary of my transplant was on July 8, 2025. They said I had to take the antiviral for a year and now I don’t, so that’s one less pill I have to take. I didn’t know that when you do a stem cell transplant, it resets your immunity, so I had to get all of my immunizations all over again. Six months after the transplant, I’ve had four appointments, wherein three of them were six shots each.
I have to get a few more. Some are live vaccines that they can’t do within the first two years of the transplant. I still have a couple of appointments sometime in the summer of 2026 to get more shots, but I’m done this year. I was so excited. The last appointment I went to, when she said, “You’re done for the year,” I did a little dance.
I still have a lot of doctor’s appointments. I get blood draws very regularly and get scans every six months. I had one done in May 2025 and it came back totally clear. My doctors’ appointments are starting to slow down. For the first few months, it seemed like I had an appointment every week or two. I was constantly doing something.

How Treatment Impacted My Day-to-Day Life
I tried to do the treatment while working, but I was taking so much time off from work because I got so sick from the treatment. I ended up losing my job, so I was out of work for a little over a year. I only recently started working again.
It’s hard. The first time around, because of the intensity of the treatment, there was no way I could work. By the second time, I tried to continue working, but I was so sick that I was missing so much work.
There are things outside of treatment that aren’t talked about enough, especially after finishing treatment. It’s not the end of it. There are still challenges. You’re still sick. You’re still dealing with doctors’ appointments. You’re still dealing with bills. Even with insurance, medical bills can get crazy and there’s a lot that you don’t think about. Navigating life with no immune system, I would be afraid to leave my house because a cold could take me out.
Getting anxious about it isn’t going to help the situation. It’s going to happen if it’s going to happen. If it’s not, it’s not.
What Survivorship Looks Like for Me
I went through a deep depression for a little while. After I finished, I thought I would be happy and celebrate, but because I was confined for so long, I couldn’t go out. I’m stuck and can’t do anything.
Once I was finally rebuilding, starting to get my immune system back, and able to venture out a little more, I came out of it and now I’m enjoying and living life to the fullest. I go out as much as I can. I see my family and friends. I do everything that I can.
I appreciate my family and my friends. I appreciate things more than I used to, like doing normal everyday things such as going to the grocery store. When you go through a time when you can’t do those things, they mean a lot more. Things on my bucket list that I’ve always wanted to do are much higher priority in my life now.


I Still Experience Anxiety Before Scans
I still feel a little bit of anxiety, but it’s not as bad as the first time around. At this point, getting anxious about it isn’t going to help the situation. It’s going to happen if it’s going to happen. If it’s not, it’s not. There’s no point getting worked up over it.
I’ve only had two scans so far. I had my remission scan in October 2024 and then a follow-up scan in May 2025. The only thing I hate is having to drink barium. There are different flavors, but they don’t help. It’s like a runny, chalky yogurt. It’s awful. And you have to do it every scan.
I don’t mind the scan itself. MRIs are loud and scary, so I don’t like them. PET and CT scans are fine. It’s just the barium. I hate the barium.
If you feel that something is up, even though they tell you that you’re fine, go to see a different doctor.
What I Want Others to Know
During DLBCL treatment, life sucks. There’s no way around it. They give you all kinds of medications to help with the side effects, but it’s going to suck. You’re going to be tired. You’re going to be sick. But know that there is an end to it all. It gets better. You come out the other side. Most people have a completely different appreciation for life and I definitely did.
The only thing that’s weird for me is when I go to doctors’ offices and you have to fill out forms that ask if you’ve ever had cancer before and I have to check yes. That still weirds me out.

Why Self-Advocacy is So Important
Don’t give up. You have to be your own advocate because nobody else will. People in the medical field do their best, but a lot of the time, they’re so far removed from it because they don’t want to get overly emotional. It seems they don’t put their best foot forward when it comes to that. It almost seems like you’re just a number.
It hurts and it sucks that that’s the truth. Especially in the ER, they have to get you in and out. But if you feel that something is up, even though they tell you that you’re fine, go to see a different doctor. Do something else. You have to be your own advocate.
Listen to your gut. Don’t always listen to the doctors. Listen to yourself. You know yourself better than anybody else knows you. I’m living proof of that.
Thank you to Genmab and AbbVie for supporting our independent patient education content. The Patient Story retains full editorial control.

Inspired by Melissa's story?
Share your story, too!
More DLBCL Patient Stories
Ashley P., Diffuse Large B-Cell Lymphoma (DLBCL), Stage 4
Symptoms: Feeling like holding breath when bending down or picking up objects from the floor, waking abruptly at night feeling “off,” one episode of fainting (syncope), presence of a large mass in the breast
Treatments: Chemotherapy, bridge therapy of chemotherapy and radiation, CAR T-cell therapy
Melissa B., Relapsed Diffuse Large B-Cell Lymphoma (DLBCL)
Symptoms: Lump in the left breast, persistent rash (started near the belly button and spread), intense fatigue and energy loss
Treatments: Chemotherapy (R-EPOCH), Neulasta, radiation therapy, surgery (to remove scar tissue and necrosis), autologous stem cell transplant
Jen N., Diffuse Large B-Cell Lymphoma (DLBCL), Stage 4B
Symptoms: Blood-tinged phlegm, whole-body itching, shortness of breath, lump near collarbone, night sweats, upper body swelling, rapid weight loss
Treatments: Chemotherapy, immunotherapy, lumbar puncture, autologous stem cell transplant
Jim Z., Diffuse Large B-Cell Lymphoma (DLBCL)
Symptoms: Sudden and severe head and neck swelling, purplish facial discoloration, bulging neck veins
Treatments: Surgery (resection and reconstruction of the superior vena cava), chemotherapy


