Mike’s Stage 4 Diffuse Large B-Cell Lymphoma (DLBCL) Story
Interviewed by: Taylor Scheib
Edited by: Chris Sanchez

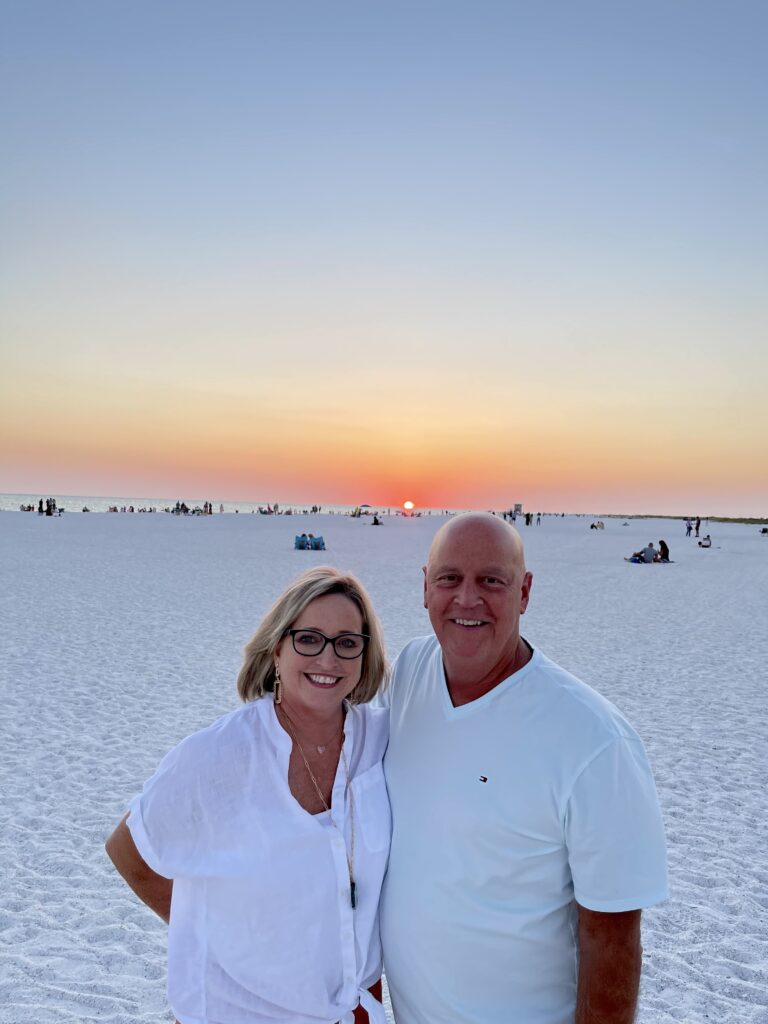
Mike got through stage 4 non-Hodgkin diffuse large B-cell lymphoma (DLBCL). He has been in remission for 3 years now.
Mike did not experience any initial symptoms at all. His cancer was uncovered quite by accident. In the process of setting up his new house, Mike supposedly hurt his back and began to experience profound, persistent pain. His back pain got so bad that at one point he thought he was experiencing a heart attack. A visit to a chiropractor worsened the situation; a chest adjustment led to Mike experiencing a shock throughout his entire body, and a few hours later, he could barely walk.
An MRI revealed the cause of Mike’s pain: a spinal tumor. His surgeon removed the tumor, and it was found to be cancerous. Mike’s oncologist also put him on chemotherapy. Mike responded well to his treatments, despite struggling with side effects like intense leg pain, hair loss and, strangely, weight gain; he was still able to work while undergoing chemo.
Aside from his treatments, Mike also credits the steadfast care and constant attention provided by his wife, a nurse, and his family, as well as the comfort and stability provided by his faith and his friends, for his recovery. His story underscores the importance of finding care — not only medical care, but also emotional support, given the toll cancer can take on one’s emotions — as well as how crucial faith can be during treatment and afterwards as well.
- Name: Mike E.
- Diagnosis:
- Diffuse Large B-cell Lymphoma (DLBCL) (Non-Hodgkin Lymphoma)
- Staging:
- Stage 4
- Symptoms:
- No noticeable initial symptoms
- Persistent, significant back pain which led him to have the MRI that exposed his spinal tumor
- Treatments:
- Surgery: removal of spinal tumor
- Chemotherapy: R-CHOP (cylophosphamide, doxorubicin, vincristine, rituximab, prednisone)
This interview has been edited for clarity and length. This is not medical advice. Please consult with your healthcare provider to make informed treatment decisions.
The views and opinions expressed in this interview do not necessarily reflect those of The Patient Story.
Everybody has a different journey.
It is your game… play it the way that you need to. You will know when to do it.
You know it is your game to play.
Introduction

My name is Mike.
I live in Rincon, GA, which is about 20 minutes outside of Savannah, GA. I’m originally from Savannah.
I had non-Hodgkin diffuse large B-cell lymphoma. I have been in remission now for 3 years.
Pre-diagnosis
My symptoms, well, I did not have any symptoms. I guess I may have, but I didn’t notice, and it was all found by chance.
We moved into a new house. I bought some big pots to put out in front, and you must bear hug them to get them off the truck, and that is what I did. I thought that I had pulled a muscle in my back.
So, for about two weeks, I dealt with the pain of it, and it just kept getting worse and worse. The week that I was diagnosed, the pain got so intense that I had thought I was having a heart attack.

We called the ambulance and took a little ride to the hospital. It turned out that my heart was fine, but I still had pain, so a couple of days later, on a Thursday, I went to a chiropractor.
When he adjusted me in the chest area, I had a shock go from the tip of my head to the bottom of my feet. By the time I had left his office, drove a mile down the road to Walmart, and got out to walk in, I could barely walk. I went back to him that afternoon, and he just did not know what was going on. That evening, when I got home, I had to use a walker.
On Friday, the day afterwards, we set up an MRI with the neurosurgeon that I had used before. But I could not do it, because I could not lie down.
Saturday rolled around, and my wife, who is a cardiac nurse, set up for me to go to the local hospital here in Effingham County, where I successfully got an MRI.
Discovery, Diagnosis and Treatment
Surgery
Well, in the MRI, I did not know it then and there because no one told me, but they saw a tumor on my spinal cord.
On Monday, December 21, 2020, I checked into the hospital. On Tuesday, I had surgery, and stayed in the hospital overnight.
Then we went down to Tybee because we had rented a house down there for Christmas.
When we were down there, the tumor was sent off so they could check it to see if it was cancerous. However, the surgeon had already known that it was; I guess he had done so many surgeries like that, that he could already tell if it was cancerous or not.
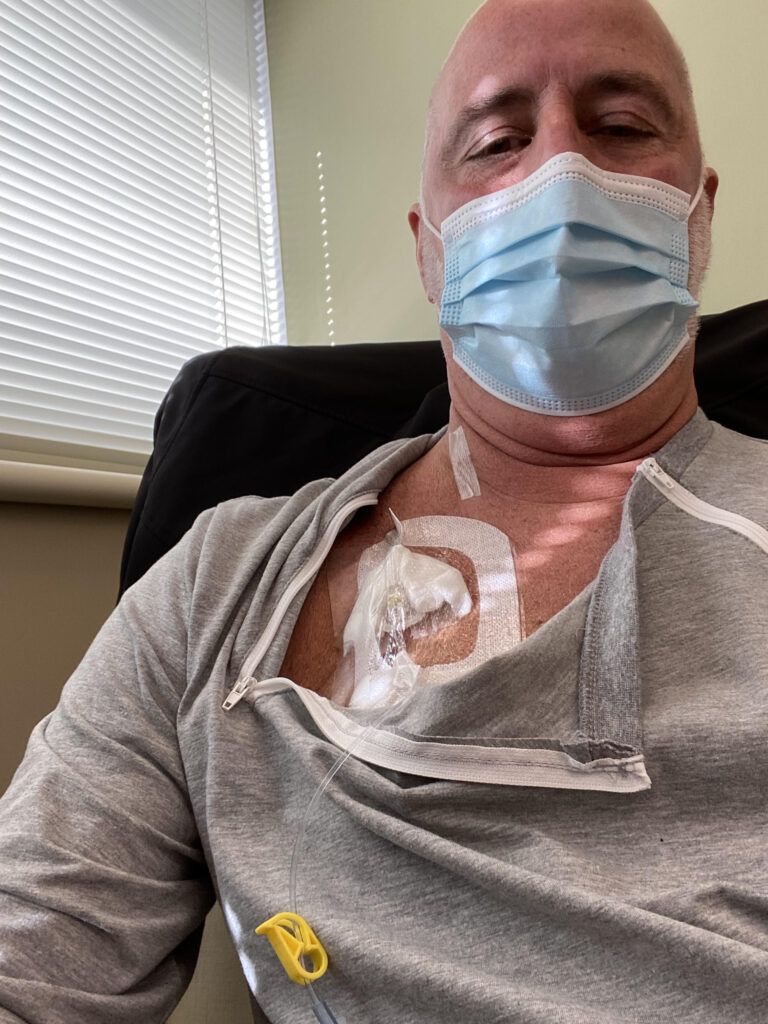
A couple of days later, we had a meeting with an oncologist to discuss my treatment. The combination of drugs I would be taking is known as R-CHOP.
It turned out to be a pretty rough treatment.
Chemotherapy
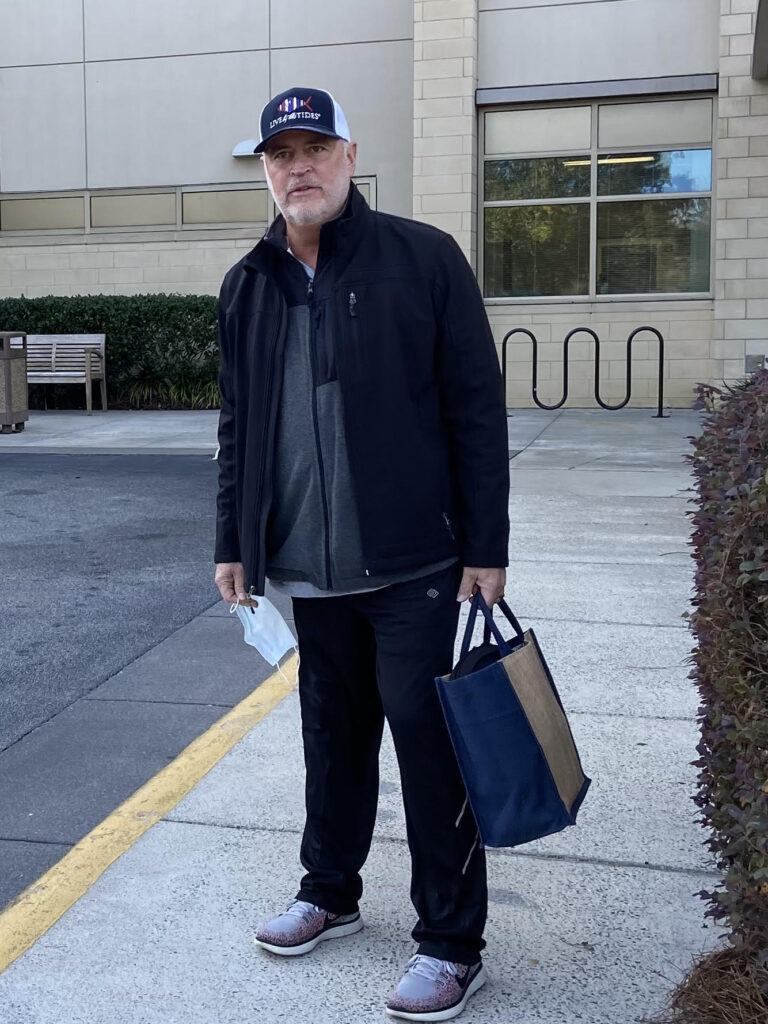
The first treatment was on that infamous day of January 6, 2021, and everything was going on in Washington, D.C.
Not only that, but Covid was going strong, so no one could go with me to have chemo, and so I was kind of on an island by yourself. I got used to it–and as you’ll see, I wasn’t actually left alone.
The people in the hospital who administer the drugs are wonderful. They have a big heart for people like us and they made it easy. Of course, wearing a mask the whole time you are there is no fun, but they did make it very easy.
I had 6 rounds of R-CHOP every 3 weeks.
Effects of the treatment regimen

During the first round of chemo of R-CHOP, I was told that it was so important to stay hydrated. So when I would get home after treatment, I felt like I would almost drown myself because I had drunk so much.
I had been told that one of the side effects of my treatment regimen would be nausea, but it was a pleasant surprise that that was not the case for me. I think I had needed to take only 2 nausea pills the entire time, which was awesome.
Another thing too that was a bit unusual was that I actually gained weight during my treatment. People normally lose a lot of weight, but I actually gained 30 pounds.
I also lost all my hair after the first rounds of chemo. That was a big thing for me.
Additionally, I had intense leg pain after my infusions. They gave me Neulasta for that, and that is something that I still struggle with today because of the neurological damage done to my system.
I was also informed that I needed to watch out for the third round of chemo. I go to church with a guy who said to me, “Wait until your third round.” But it was not the third round that kicked me in the behind; it was the fourth round. It just wiped me out.
I would have a treatment on a Friday afternoon, and it lasted about six hours. I would get home, and I would be wired that whole afternoon and all night. Then I would not go to sleep until about noon on Saturday. I would just be wired, not hungry but we did have somebody at the church that would make me some vegetable soup and banana bread, and that helped me out tremendously for a bunch of days after I had my treatment. The part of being wired, that was always the worst part of it. Then, by Tuesday, I would be able to go back to work.
I am in sales, and I do not see how anybody in a factory job or anything like that could go through it and keep a job. That being said, I was still able to function for the most part while I was on chemo.
As a matter of fact, I continued to work the whole time I was being administered R-CHOP. On days that I did work, sometimes it was a pain, and on the whole I felt like I was in a cloud. I was still able to work, though, which is great.
I complained one day to the neurosurgeon about why I was not walking better, and he commented that I should feel blessed that I was even walking.
Remission
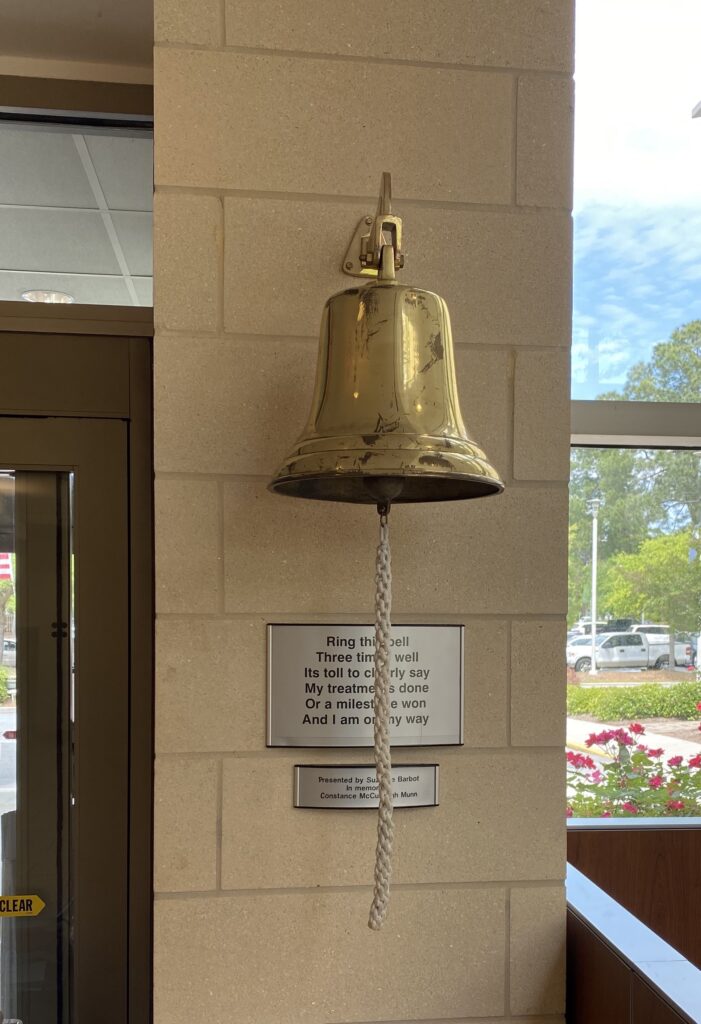
After I had finished my treatments, I went for a PET scan.
It showed 2 lumps in my stomach that were lit up. My oncologist said, feel free to search for a second opinion. So we did that.
My wife, the nurse that she is, spoke with my sister and a good friend of hers whose brother is an oncologist in Atlanta, and he suggested going to Moffit Cancer Center down in Tampa.
We went down there, and he did some tests that my oncologist here did not do.

All the tests determined that the lumps were not growing at all.
So this means that the treatments were successful and my cancer was in remission.
I have been in remission now for 3 years. I go every 6 months to have a check-up.
PTSD
I may be cancer-free now, but there are moments that I have PTSD. I experience some triggers that remind me of things that were not so pleasant during my treatment time.
Just as an example, I have some photos of the Red Devils, part of the chemo that they call the Red Devils. Those are potent. Anytime I look back and see the pictures of those, I can almost taste them. They were that bad.
That being said, though, I can say that I’ve come away stronger.
Before all this happened, I could not take an MRI, PET scan or CT scan or anything like that without being sedated. Now I have learned how to deal with everything like that.
I think the last MRI I had lasted about an hour and 30 minutes, and it was not bad at all. Getting my port taken out was easy. I am not afraid of needles. I am not afraid of MRI machines, PET scans, or CT scans, either. Not any more.
Looking forward after remission
My experience has changed my life.
You start to think more about your family than about material things that do not really mean a whole lot. The shoes, the watches, the shirts, you know—they do not mean that much.
I am semi-retired now, and cannot wait for the time that my wife will retire, too. As I mentioned earlier, we had built a house about six months before I was diagnosed. We had just moved into the house and were getting things done around the house, and then I was diagnosed with cancer. So, there were a lot of things put on hold, but a lot of those things just do not mean anything to me any longer.
The only thing I want to do now is buy a motorhome and travel. Have a smaller house and travel back and forth. My wife is not quite on the same page with me, but she is getting there, and so I am hoping that that dream will come true. All she wants to do is spend time with our 3 grandkids, which of course is wonderful also.
We have done a lot in our life together. We’ve been to the Caribbean a few times and rented boats and sailboats. We spent time out, about ten days, on a sailboat sailing around the British Virgin Islands, which was nice.
What helped Mike during his treatment
Wife and family

I have nothing but praise for my wife, who is a terrific nurse, and she took such good care of me while I was in the thick of treatment.
She was my rock when I needed a rock, gave me my pills, set my appointments, cooked supper. She was beside herself because she could not go to me for my treatments. But she was still able to drive me to them and drive me home.
With her being a nurse it just came naturally. I did not have a bell to ring, but she was always there for me and was willing to do anything that I needed. She took over.
It’s so important to have somebody to talk to; there were a lot of times that I would get upset, it is an emotional time, and when you are diagnosed with cancer, it tugs at your emotions. So, there were many times that my wife and I would sit there and talk about things.
Anytime that I was uncomfortable, and there were a lot of times my back was hurting from the surgery, I have a 12-inch scar in the middle of my back where they took the tumor out. So, to make me more comfortable, she rubbed my back, her and the grandkids too. They would get a rolling pin and roll it up and down my back, and that always felt good.
I’m well aware that it was no walk in the park for her. She had to take care of the house and its day-to-day concerns. That right there is a huge burden, paying bills and things like that. That weighs heavy on those people and the caregivers.
Faith and friends
My faith and our church family have also really risen to the occasion and have really helped me through this whole thing. A big part of how I have been able to deal with the last three years is because of my faith.
Our faith in God got us through these tough times. I talked to God a lot during those days, and I had peace. I would not say that I was worried because I looked at it this way: If I go first, I win.
You know, sometimes people say it takes a village, and it really does. I just thank the Lord.
I would not say that I was worried because I looked at it this way:
If I go first, I win.
Lessons Mike wants to share
Be mindful of the caregivers too
When I know that somebody has cancer, it is not only “How is that person doing?”, but also “How are the caregivers doing?”
You know, because it is tough on them, and you can see it if you are around people enough. They need prayer, too. They need just as much prayer as the sick person.
My advice to the patient would be to be patient with the caregiver. You are both walking down a road that you have never been down before, and they are going to think one way, and you are going to think another way, but always remember to be patient.
You know, we all run out of patience from time to time, but for me, as a patient, getting upset with my caregiver, I did not like that, and I apologized because, yes, it is a tough thing to go through, and I am the one going through it, but they are going through it also.
They need their time, and they need their respect, and as patients, we have got to give it to them and love them because they love you the best way that they can. We have got to love them the best way that we know how.
Without them, it would be a lot harder. It is hard enough, but going through that time without my wife as my caregiver… I do not know if I would have made it.
We are all on different journeys
My final message would be: everybody has a different journey.
You can ask a question about how you get through chemo and all that, but I think everybody is going to have a different answer. My answer would be: it is your game; play it the way that you need to.
If you feel like doing something, do it. If you are tired, and that is another thing, fatigue, good grief, the fatigue is just unbelievable, and if you do not feel like doing something, do not do it.
Eventually, you will have to get up and do something, but you will know when to do it.
You know it is your game to play.

Inspired by Mike's story?
Share your story, too!
More Non-Hodgkin Diffuse Large B-cell Lymphoma (DLBCL) Stories
Anna M., Diffuse Large B-Cell Lymphoma (DLBCL), Stage 4
Symptom: a rRapidly growing, painless lump on the breast
Treatment: Chemotherapy
Ashley P., Diffuse Large B-Cell Lymphoma (DLBCL), Stage 4
Symptoms: Feeling like holding breath when bending down or picking up objects from the floor, waking abruptly at night feeling “off,” one episode of fainting (syncope), presence of a large mass in the breast
Treatments: Chemotherapy, bridge therapy of chemotherapy and radiation, CAR T-cell therapy
Melissa B., Relapsed Diffuse Large B-Cell Lymphoma (DLBCL)
Symptoms: Lump in the left breast, persistent rash (started near the belly button and spread), intense fatigue and energy loss
Treatments: Chemotherapy (R-EPOCH), Neulasta, radiation therapy, surgery (to remove scar tissue and necrosis), autologous stem cell transplant
Jen N., Diffuse Large B-Cell Lymphoma (DLBCL), Stage 4B
Symptoms: Blood-tinged phlegm, whole-body itching, shortness of breath, lump near collarbone, night sweats, upper body swelling, rapid weight loss
Treatments: Chemotherapy, immunotherapy, lumbar puncture, autologous stem cell transplant



