Holly’s Myelofibrosis Story
Interviewed by: Taylor Scheib
Edited by: Chris Sanchez

Holly was only 25 when she was diagnosed with primary myelofibrosis.
Holly’s diagnosis was only one of a series of sad and traumatic occurrences at that particular time in her life. She had earlier lost her unborn daughter at 32 weeks due to a blood clot that passed through her placenta, and had to be placed in intensive care afterwards due to the discovery of more blood clots elsewhere in her body. Two weeks afterwards, she experienced a seizure and thrombosis stroke.
Over the succeeding year, Holly increasingly experienced symptoms that led to her undergoing a bone marrow biopsy, which revealed her cancer. What’s more, she discovered that her cancer might have had something to do with her daughter’s passing.
Holly continues to grieve her loss, but her life has taken a turn for the better. Her treatments have been effective — and she is now expecting another little girl.
Holly’s story is a testament to her resilience, the inner strength she gained, and her ability to glimpse the blessings in her life behind all her negative experiences. She shares her story with us today to help others who may find themselves in similar situations.
In addition to Holly’s narrative, The Patient Story offers a diverse collection of stories about myelofibrosis. These empowering stories provide real-life experiences, valuable insights, and perspectives on symptoms, diagnosis, and treatment options for cancer.
- Name: Holly S.
- Diagnosis:
- Primary myelofibrosis
- Initial Symptoms:
- Severe fatigue
- Throbbing pain in left calf
- Significant weight loss
- Itching and rashes
- Bruising
- Shortness of breath
- Treatment:
- Oral chemotherapy: hydroxyurea
- Immunotherapy injections: peginterferon

This interview has been edited for clarity and length. This is not medical advice. Please consult with your healthcare provider to make informed treatment decisions.
The views and opinions expressed in this interview do not necessarily reflect those of The Patient Story.
I feel like I can overcome anything as long as I just remain positive.
Introduction

My name is Holly. I’m from Invercargill. It’s a small city at the bottom of New Zealand.
I am a single mum to a boy called Ambrose, who is five, turning six in October.
I was recently diagnosed with primary myelofibrosis in September of 2023.
And, yeah, just been navigating life as a single mum and just dedicating my time to him. Whilst dealing with this.
Pre-diagnosis
Initial symptoms
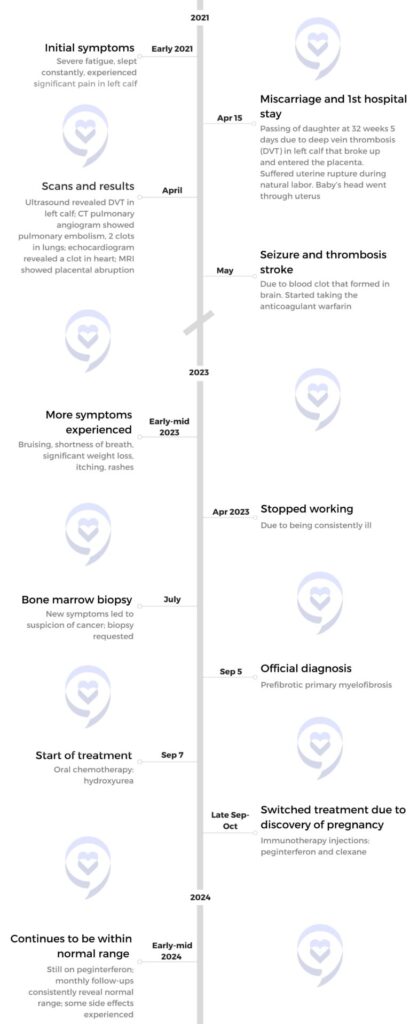
My first real symptoms of primary myelofibrosis basically start back in 2021 and April.
I was 32 weeks with my daughter and I started getting pain in my calf, just throbbing pain.
So I was getting constant massages to try get rid of it. Initially thought it was pre-eclampsia. I was also experiencing extreme fatigue a lot throughout the pregnancy.
And then one day I was in the supermarket and I started getting a lot of pressure in my abdomen. I didn’t really think much of it and went home.

And then I started having contractions around 9 p.m. and they lasted until 3 a.m. I started experiencing fevers and sweats and because I had had such a horrible experience with my previous midwife, with my son, I left it and I didn’t want to bother my current midwife.
And so then I’d contacted her in the morning about it, and we went down to the hospital.
She did an ultrasound and found that there was no heartbeat.
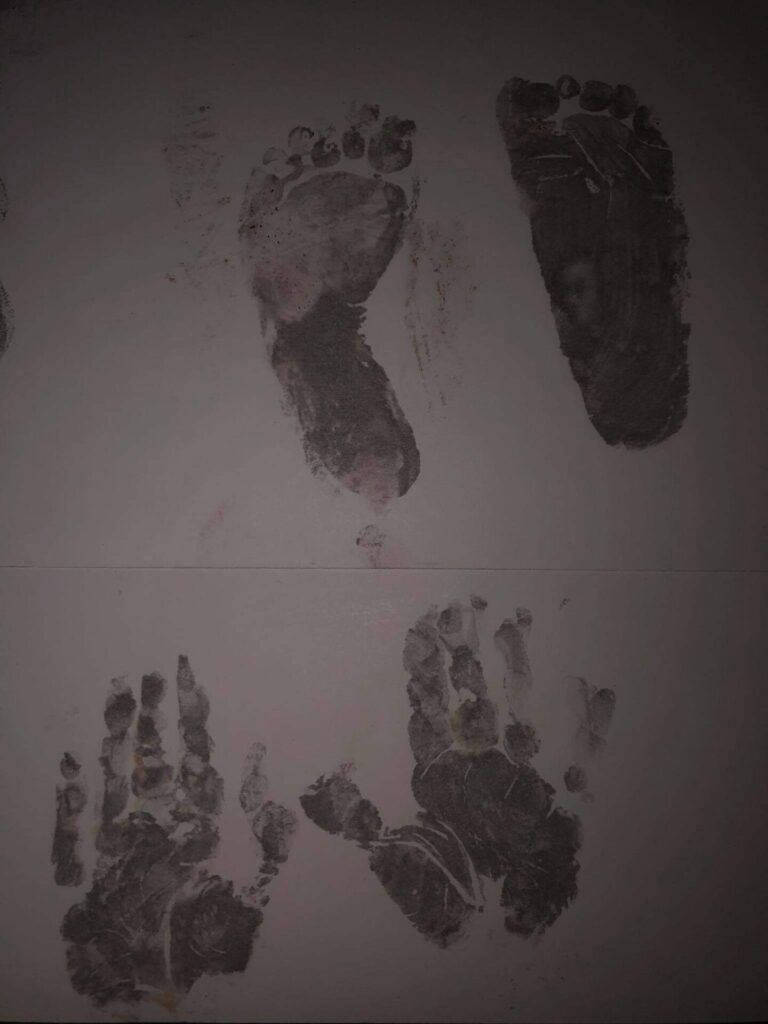
Loss of her daughter
So then I had to give birth to my daughter. And it was just a horrific, horrific delivery.
Yeah, it lasted for a few days, and I was put on these inducing pills. They gave me too many of them. And her head basically went through my uterus; I suffered a uterine rupture during labor.
So then I was rushed into theatre, and I lost 1.5 to 1.7l of blood. After that, I was in an ICU for about a week due to complications, including pneumonia.
I had a really high heart rate. I had heart failure. And they didn’t really understand what was going wrong.
And then they found that I had had a blood clot in my heart, in my lungs, and a DVT (deep vein thrombosis) in that right calf. So I’m guessing all the massaging had possibly broken the blood clot off into different parts of my organs.
So they think they also think that it caused my daughter’s death. A blood clot had passed through my placenta, causing a placental abruption.
Seizure and stroke
So I left hospital, and then two weeks later, I had a seizure and a stroke, and I was rushed back into hospital. They had found that I had had a thrombosis stroke in my brain.
So I was put on warfarin for well over six months max. And then, originally the hematologist thought that I had blood clotting disorder.
So she put me on warfarin, then took me off it for about a year just to see how my blood platelets were going to be. And they weren’t coming down, they were rising.
Discovery and diagnosis

That’s when I started having my other symptoms. And they came on quite, quite quickly because I wasn’t on any sort of medication at that time.
I started just being extremely, extremely fatigued. My arms were really, really weak. I lost 20kg without even trying, within 3 months.
I started bruising, like all over my body and the weirdest places. Itching. Crashing randomly. Constant shortness of breath.
It was it was horrible and I just I couldn’t function at all. Throughout the day.
So then the doctor sent me to have a bone marrow biopsy. I was officially diagnosed with primary myelofibrosis in September 2023.
Reaction to the diagnosis
I guess that unknown feeling I felt within those two years of not knowing. It’s sort of hard to really know. I guess I was just going through day by day.
I initially thought because I had two blood transfusions, I thought that it was all the blood transfusions that were actually causing all these symptoms, and I just thought that was normal. And I also thought because of all the physical complications I went through, my body was taking a longer time to try and heal from all of that.
And then, straight after all of that, I was thrown straight back into being a parent, single parent. Yeah, it was pretty crazy.
So when I went in for the bone marrow biopsy, I felt really numb to it all, I think because so much had happened previously, I was just on autopilot, like, okay. Yep. We’ll do this.
After I got the diagnosis, I was absolutely distraught because I didn’t know much about the disease at the time.
And I didn’t know anything. If I was going to lose all my hair, or if I was going to have to take more time being away from my son. So many thoughts running through my head.
But there’s more. As it turns out, my cancer might have had something to do with my daughter’s passing.
When my cancer was diagnosed, they didn’t really say that they thought that I had it when my daughter had passed. It wasn’t until a few months ago that they had sort of written it in doctor’s notes, speculating that it had caused my daughter’s passing and that I’d had it while I was pregnant with her.
But yeah, the feelings around it. I was more so angry at the hospital and my midwife for not monitoring me closely enough, but I guess they couldn’t really do anything about it.
But yeah, it was a terrible, terrible time. I really lost myself and my relationship fell apart; I just wasn’t coping.
I had turned to drinking a lot, so that was like my medication while trying to be a single mum and trying to just push, push forward.
And yeah, so when they had told me that they thought that I might have had it when I was pregnant with my daughter, I’d already had a huge feeling that it had caused it before they even said anything.
Treatment
Oral chemotherapy: hydroxyurea
My treatment plan was to go on an oral chemotherapy called hydroxyurea.
So I started on 500mg. My platelets weren’t really doing anything. So they were going to double the dosage.
Discovery of pregnancy, and shift to immunotherapy injections: peginterferon
And then a week later I found out I was pregnant. And I was a mess because I thought, I’m gonna have to terminate this baby.
Then they congratulated me, and put me on peginterferon. It’s immunotherapy that’s administered through an injection. I do this myself, once a week, on Sunday nights.
So I’ve been on peginterferon and aspirin, um, throughout this pregnancy and it’s brought my platelets right down.
I’m also on clexane as well, just to prevent blood clotting.
I’ve been in normal range for the last few months, and I’ve felt the best that I’ve felt in the last few years, and everything’s just looking amazing with this pregnancy.
So I’ve been really privileged, even, I guess, divinely orchestrated.

Side effects
That being said, I’ve been experiencing some side effects for the immunotherapy.
I’ve had a lot of hair thinning, acne, a lot of fatigue. And loss of appetite. I don’t really have much of an appetite. I’ve started bruising again, too.
But I actually had more symptoms with the hydroxyurea than I did with the peginterferon.
So at this point I don’t have any bone marrow scarring. I just have a lot of fibrosis.
Looking forward
New treatment plans haven’t been discussed with me at all because I’m pre fibrotic with the primary myelofibrosis.
So they for now they haven’t discussed anything with me. And I am open to other treatments if need be.
A stem cell transplant has been brought up. But I’m sort of on the fence about it, because I’ve heard such horrific stories of people that have gone through it.
I don’t know if I want to put myself through that.
… over time, this cancer, it’s really taught me how resilient I am. And how much I’ve just trusted that whatever’s meant for me is meant for me.
Even if the cancer does get worse over time, it really has taught me to live in the moment and live in stillness and just be grateful for even the smallest things.
Takeaways and lessons
In the beginning, my mental health was really, really bad. I was thinking the worst of everything.
But then over time, this myelofibrosis, it’s really taught me how resilient I am. And how much I’ve just trusted that whatever’s meant for me is meant for me.
Even if the cancer does get worse over time, it really has taught me to live in the moment and live in stillness and just be grateful for even the smallest things.
Yeah, it’s been a huge challenge, but it’s been one of the best things to happen to me as regards my mindset.
I feel like I can overcome anything as long as I just remain positive.

I guess I also really started to find myself. After I got diagnosed with myelofibrosis, I had an answer as to why my daughter passed away. And then I knew that it wasn’t my fault, because for a long time I blamed myself. And I felt that I could finally move forward. I had that closure.
Then that’s when the healing really started. So when, when they got the diagnosis, the healing really started. So I guess it was a little blessing in disguise, even though it was what caused it all.
Now, I’m pregnant with another little girl. I have obstetricians monitoring me every four weeks, and also multiple scans.
I am 33 weeks at the moment, and they’ve planned all these scans to make sure that everything’s fine. I’ve got phone consults with my hematologist, monthly blood tests.
And my midwife, she’s amazing. She was like, don’t worry. If you know you have an issue, just ring me and I’ll come down in the middle of the night. We can check. She’s very, very onto it.
And she’s always happy to do extra tests and scans and things to make sure that everything’s good. So they’ve really looked after me now, this time round.
I’m due on the 2nd of July, but they’re going to get me an early C-section at 37 weeks due to the uterine rupture that I previously had.
In closing, I guess my message is, you know your body better than anybody else does.
If you have an inkling of whether you’re pregnant or you may have cancer if you have an inkling that there’s something wrong—put yourself first and go and get it checked.

Inspired by Holly's story?
Share your story, too!
Related Cancer Stories
More Myelofibrosis Stories
How to Support Someone with Cancer: Karina & Jesse's Myelofibrosis Story
“I underwent a lot of sadness, hardship, and difficulty, and all that entails. But I pressed forward in hope for sure. There was a lot of hope that just kept me going all those years.”
Demetria J., Essential Thrombocythemia (ET) progressing to Myelofibrosis
Symptoms: Extreme fatigue, stomach pain (later identified as due to an enlarged spleen), dizziness, shortness of breath
Treatments: Spleen-shrinking medication, regular blood transfusions, bone marrow transplant
Neal H., Prefibrotic Myelofibrosis
Symptoms: Night sweats, severe itching, abdominal pain, bone pain
Treatment: Tumor necrosis factor blocker, chemotherapy, targeted therapy, testosterone replacement therapy
Andrea S., essential thrombocythemia (ET) progressing to Myelofibrosis
Symptoms: Fatigue, anemia
Treatments: Targeted therapy (JAK inhibitor), blood transfusions, allogeneic stem cell transplant