Jenny Ahlstrom’s Multiple Myeloma Story
After moving to Mexico with her husband and six kids, Jenny Ahlstrom started getting rib pain and felt extreme fatigue, but she chalked it up to exhaustion from the move and adjusting to her new life.
Months later, more symptoms started to appear including blood in her urine. She was then diagnosed with multiple myeloma.
She shares how she searched for the best treatment options, underwent three clinical trials, and launched an organization called HealthTree to help other patients.
This interview has been edited for clarity. This is not medical advice. Please consult with your healthcare provider for treatment decisions.
- Name: Jenny A.
- Primary Diagnosis:
- Multiple Myeloma
- Initial Symptoms:
- Fatigue
- Blood in urine
- Rib pain
- Treatment:
- Velcade
- Thalidomide
- Dexamethasone
- Tandem transplant
- Relapse Symptoms:
- None; it was a biochemical relapse so just in the numbers
- Treatment:
- CAR T-cell therapy
Having cancer, you’re able to let go of a lot of the unimportant. None of that matters in life. It’s my family, my faith, and who I’m serving [that] give me the most meaning.
- Pre-diagnosis
- Diagnosis
- Treatment
- Taking care of your mental health amidst a cancer diagnosis
- Relapse
- What helped you decide on a course of treatment?
- Joining a CAR T clinical trial
- What are your thoughts about a cure for myeloma?
- What should a patient ask during the initial doctor’s appointment?
- What has been the biggest impact on you?
A year prior, we had moved from Utah to Mexico. We’re trying to get six kids acclimated… I had symptoms I probably didn’t pay attention to because I was just so busy and overwhelmed getting my kids in order.
Pre-diagnosis
Introduction
I’m a multiple myeloma patient. I was diagnosed in 2010 at the age of 43.
At the time, our family was on vacation. A year prior, we had moved from Utah to Mexico. We’re trying to get six kids acclimated to a new language, a new culture, and just everything new about that whole experience. My husband had been invited to launch the venture capital industry in the country so it was a big push. We sold our house, moved down there, [and] didn’t think we were coming back.
I had symptoms I probably didn’t pay attention to because I was just so busy and overwhelmed getting my kids in order. [I] had rib pain that wouldn’t heal and other things, and just kept getting pneumonia over and over again. Just thought, Well, I’m just tired. But who isn’t trying to do this?
Ended up going back to Utah and to Montana and I thought, Well, I’ve had these symptoms for a long time. I might as well just go get checked. I got a PET scan [of] my kidney area because my kidneys were kind of bugging me. They said, “Your spine and your pelvis are full of holes and you probably have cancer. It’s time to go get seen by an oncologist.”
We had two weeks left before we were supposed to leave to go back to Mexico after the summer and that was a bit of a shock.

What was your life like outside of multiple myeloma?
I grew up in San Jose, the Bay Area. I came to Utah to go to school and I ended up staying. I ended up working for IBM [and] got married. I have six kids.
I have an amazing husband who’s been very involved. He doesn’t work for the foundation, but he’s been very involved in helping create strategies so we’re [in] this great partnership. He comes up with some ideas and I execute them. He said, “You should build a university.” I said, “Okay. Do I have time for that? I don’t know, but we’ll try it.” It became one of our most popular programs. It’s been an amazing partnership to work on this, be creative, and create together what we built.
I love music, I sing, I play the piano, I cook, and I love taking care of my family. Between my family, my husband, and the foundation, I love [to] exercise and try to get some every day, but there’s not much time.
Initial multiple myeloma symptoms
It was fatigue mostly. In [my] last pregnancy, I probably had multiple myeloma three years prior. I think I had gotten it from a virus I got while pregnant.
I talked to somebody from one of the pharma companies a couple of years into my diagnosis. They said, “Oh, parvovirus B19? That has bone involvement. Did you know that?” I said, “What? No, I’ve never heard that before from any myeloma doc or anybody,” so I think that’s probably what caused it. I never really felt the same.
I didn’t gain very much weight at all. I lost weight while I was pregnant with the last one so I knew something was wrong. I was highly anemic. My doctor said, “I’m going to hospitalize you because you’re so anemic during this pregnancy.” I said, “You can’t do that. I have five kids at home. There’s no way.”
That and just rib pain that wouldn’t heal. [I] kept going to the chiropractor. It was a total miracle he didn’t break a bone trying to adjust me.
What made you decide to finally get checked?
We were in Mexico and I had blood in my urine for six weeks. I just kind of ignored it. I said, “I don’t want to go to a clinic and try to explain that in Spanish to a doctor. I’ll just wait ’til we go back home.”
The symptoms went away the day I went in. I almost didn’t go in because I said, “Well, it’s gone.” Good thing I did.
The doctor said, “You have holes in your bones and your pelvis. You need to go see an oncologist.”

Diagnosis
Reaction to the multiple myeloma diagnosis
I got a call and I was just in the car by myself. The doctor said “I’ve been trying to get a hold of you from this hospital in Montana to tell you you have holes in your bones and your pelvis.” It didn’t register. He said, “You need to go see an oncologist.”
We have already been through a really aggressive cancer experience with my brother-in-law who had AML six years prior. I probably cried, but the feeling I remember having is, “Okay, if I do have this, then we’re going to do things differently.” And we did.
I ended up going to the same facility that he went to when he was first diagnosed, which was a local center, not an academic center. Had a very reputable oncologist see me. The oncologist really wanted to treat me that Friday. He said, “Okay, I’m going to start treating you on Friday. Don’t worry. You’re not going to lose your hair. We’ll think about transplant later.”
Six years before that, my brother-in-law had waited way too long to get [a] transplant and he passed within a year. The AML was very aggressive. He caught it really late. He kind of made the mistake of saying, “Don’t go up to Huntsman because they’ll have you doing tandem transplants.” So, of course, we hit the parking lot and my husband gets on the phone with the doctor at Huntsman who convinces us, “Just come up here.”
The difference in [the] number of patients that the local oncologist was treating, even though he was a wonderful oncologist… He didn’t even do a bone marrow biopsy before he said, “I think you have myeloma.” I said, “You think? You think I have something [and] you want to start treating me on Friday? We might want to get the testing done first.”
If that had been my only experience with cancer, I probably would have just said, “Sure. Okay, I’ll show up on Friday and you’re just going to give me whatever you’re going to give me.” Then I wouldn’t have had any genetic features from my bone marrow biopsy or I just wouldn’t have had the information that I needed.
We have already been through a really aggressive cancer experience with my brother-in-law who had AML six years prior… My brother-in-law had waited way too long to get [a] transplant and he passed within a year.
I’m so happy that he made that comment because I went from a physician who was treating five cases of myeloma to 500 cases at the academic center and that doctor had come from the University of Arkansas Medical Sciences (UAMS). They have this tandem transplant protocol. At the time, the experts were fighting over single versus tandem transplants.
I said, “I’m young. I watched my brother-in-law die. I’m healthy, except for the myeloma so just go ahead.”
I had a high-risk feature so he said, “You have one shot at initial cure and a certain percent of the patients can get cured — functionally cured — right off the bat. But if you wait and go through several lines of therapy, that’s not that much of an option anymore so just try that and see.”
I went from a physician who was treating five cases of myeloma to 500 cases at the academic center.
Breaking the news to my family
My kids were three to 15. My youngest had just turned three. His birthday was while I was getting my port installed. I said, “Okay, someone [needs to] take over that birthday party because it’s not happening with me.”
We had to decide immediately where we were going to live. Do we come back here and I get treatment? Do we bring all the kids back? Am I going to be immunocompromised? Is it going to be a problem having six kids coming home with germs [and] going into two transplants? Yeah, kind of, yes.
We told our kids in the backyard. We were calm about it because we had already been through this. We just made an internal commitment [that] we’re going to do this differently. My husband did not want to be in the same situation where the doctor says, “We’re out of options. What do you want to do?”
What happened with David was very tragic and very emotional. There are eight siblings in Paul’s family and we would spend time around the clock with him. It was just a very traumatic experience so we just thought, Okay, we don’t want to have that happen again so we’re going to do everything we can to make that a different experience.
Of course, the diseases are different. I don’t know [if] we could have done anything else for David at that time because there wasn’t that much out there for AML, but we were committed to doing things differently.
What happened with David was very tragic and very emotional… We don’t want to have that happen again so we’re going to do everything we can to make that a different experience.
We had two weeks to decide what we [were] going to do. I ended up staying at my sister-in-law’s house. We prepared her house for David with [an air] filter and UV lights… a really clean house and room. One of my really good girlfriends was my caregiver.
Paul went home with the kids. In Mexico, it’s very easy to find household help so he got the help that he needed because he was still starting a business. I got the support and the rest that I needed. I could have been around six kids asking about their homework and all that going through two transplants. It all worked out.
It was good that the kids knew where I was. I was gone for six months, but they were okay because they had the attention that they needed and the support. My sister-in-law moved down there and was like [a] sub-mom and took care of them.
It all worked out. They weren’t traumatized thinking,“No, mom’s right behind that door but you can’t go talk to her or give her a hug or whatever because she’s immunocompromised.” So that ended up being a good thing.
Going to a cancer specialist with more experience
We see that all the time in the patients that we serve. Patients may think, “My oncologist is so nice and I like them.” The data shows differently. The data shows that you might live two to five years longer if you see a specialist. The University of North Carolina has data on that and so [does] the Mayo Clinic.
Myeloma is a very nuanced disease and with a lot of progress over the last many years. I think there’s been more progress in myeloma than probably any other cancer. So you look at how fast things are moving, how nuanced it is, and how myeloma is not a single disease. There are different genetic features.
Every patient has kind of a different type of myeloma and different types of myeloma inside the same patient. Somebody treating 25 different cancers, as talented as they are and as hardworking as they are, there’s no way. They’re wonderful people. But am I going to put [myself under their] care? I might go get treated.
Myeloma is a very nuanced disease and with a lot of progress over the last many years.
A lot of patients do this. They’ll go see an academic specialist for some of their care definition and then they’ll take that protocol back and say, “Okay, now I want to get treated closer to home.” And that makes sense.
The data did show that if you are treated at the academic center, you do live longer because you’re getting watched. You’re seeing early signs of relapse and they’re running the right tests. That’s the number one thing I always tell patients. If you could do one thing, find yourself a specialist. That’s job number one.
Treatment
I did a year of Velcade-thalidomide-dex. It was a triple combination. I ended up flying from Mexico to MD Anderson every week or every 10 days. I don’t even know how I did that but that was exhausting.
I was gone another half a year because you [get] Velcade on [days] 1 and 4 and then you get a 10-day break and then day 1 and 4 so I’d have to stay in Houston for four days.
Then I did a clinical trial that had dexamethasone, which was an insane idea now looking back at it that I would have done steroids for another year voluntarily. But I did do that.
I didn’t do any other maintenance. Maintenance wasn’t a thing in myeloma at the time. I was happy. The idea was [to] let your body recover and your counts come back up. Hit it hard.
In my opinion, with myeloma, you’re going to get therapy regardless of whether you get it hard upfront or you get it over time. You’re still getting it so I might as well get it hard and then have a treatment break.
That’s how we advance research. If we want a cure for these diseases, we have to step up and participate.
Participating in clinical trials
I think I participated in three clinical trials as part of my transplant process to donate samples and tissue. The first time I got a bone marrow biopsy, they said, “Do you want to donate samples?” I wasn’t sedated or anything [so] I got out of there crying and screaming. That was a terrible idea. You got to sedate me next time. That’s not going to work for me.
That’s how we advance research. If we want a cure for these diseases, we have to step up and participate. In cancer, there [is] no placebo. You’re never not going to get treatment. That’s unethical. The doctors would never do that.
They’re looking ahead and saying, “What else can we do to make the treatment better?” They’re looking for creative ways. Maybe another year of dex is not the right answer. But we have so many open clinical trials in myeloma now.
Back when David was diagnosed, six months in, they said he was out of options. He was in the ICU. He had incredibly high blood pressure and his heart was just racing. They said, “He’s ready to die and you’re being mean to keep him alive.”
Paul, my husband, had done some research showing that he had CD33 protein [in] his AML cells. He said, “Could you give him Mylotarg?” Because that was a target. [It] wasn’t approved for his indication and he couldn’t, at that point, join a clinical trial. We got permission to use it for compassionate use and he lived another six months. Within two days, he was out of the ICU, breathing fine, [and] on a stationary bike.
That type of participation in research is necessary if we’re going to advance the field. Now, if we don’t care about a cure or whatever, then we shouldn’t think about it. But lots more kids with cancer join clinical trials because their parents are willing to take them anywhere. As adults, we think, “Is it convenient?” You’ve got a job to think about, family issues, or whatever so it’s a little more challenging sometimes.
You should ask about clinical trials at every stage. There are great myeloma clinical trials for newly diagnosed patients right now, especially if you’re high-risk. We already know what your outcomes are going to be so why not try the extra stuff and try to get a longer remission? Sometimes people think about it as this last resort, but it’s not. If you wait too long, you just don’t qualify. [If] you’re too sick, you can’t join.

Taking care of your mental health amidst a cancer diagnosis
I handle the anxiety part of it by getting involved. We just had this hypothesis that David’s experience, when he used the Mylotarg, wasn’t shared with anybody at Huntsman [or] any of his peers, and that drug took another 14 years to get approved as an indication for his type of disease. Why? Why is it taking this long? And so we took that idea.
If we can aggregate patient data [and] put it together, if patients were willing to do that, we could come to a lot faster conclusions. In the meantime, I realized I don’t have a relationship with the clinicians and with any of their patients so let me just do things that I see a need for.
I want to find a myeloma specialist. Why can’t I find one online? Why isn’t there some kind of directory that helps me find that? It’s so basic. It doesn’t make sense.
I wanted to understand and read news about myeloma treatment, but it was all scientific and I didn’t understand it. Can we rewrite it and simplify it a little for the patient community [so] they still understand what the progress is and how to describe it?
I just decided, “We’re going to create a foundation. We’re going to fill some of these gaps.” There were very nice existing and supportive foundations in the myeloma space that were very well established, but there were certain things I felt like I needed as a patient that weren’t being done.
I wanted to join a clinical trial and I was panicked. “I’m going to relapse fast. This is not going to be a long remission.” I don’t know why I felt like that, but I just did. I felt this clock ticking all the time, like I’ve got to get moving. We got to do something.
I looked some trials up. I called eight facilities. I got a call back from two. ClinicalTrials.gov is a total mess. This is not easy for patients. Why is it this hard? So we started the podcast series [where we’re] interviewing investigators. It was this nice blend because they wanted to share their research, they wanted to get patients into their trials, and patients wanted to know what was going on.
Focusing on something else other than cancer
I built a website. I didn’t know how to do anything, but I just decided I was going to do it anyway. I have nothing to lose so I might as well. I felt very unqualified. If you listen to the first couple of radio shows, [you’ll notice] I’m super nervous, I’m not smooth at all, and I don’t listen very well to the doctor’s answers. But I’ve done 158 shows now and it’s fun.
I enjoy talking to them and saying, “Why would a patient want to join this trial? What are you trying to accomplish? Who can join? Where’s it open?” And just understand the science behind it because some of the new stuff [that] comes out always has a number associated with it and you don’t even know what it does or is, especially if it’s a new class of drug.
We started adding programs. I started meeting these investigators because I was doing that show once a week. I was meeting a lot of investigators and started attending conferences. Then we started a roundtable series putting together live meetings and met more that way, trying to bring those educational programs to patients.
When you get diagnosed with something, you can do one of three things.
You can say, “I’m a victim. I have myeloma. Poor me.” You can swear at it. You can do all that. It doesn’t help so I’m not sure why people do that, but they can be really angry about it.
You can also be defined by it. “I’m a cancer patient. This is part of my new identity.” I don’t think that has to be the case.
But the third thing is you can look at it as a new opportunity. Paul had a colleague in Mexico and he said, “I was telling him my wife has cancer.” [His colleague] said, “Well, congratulations.” And he said, “Hmm. Tell me about that because that’s not the normal response, you know.”
And [his colleague] said, “My son died in a regular adenoid surgery. We ended up donating his organs. We started a foundation. We’ve done 80 organ donations now. You are going to see the world differently so it’s an opportunity for you. You have an opportunity to serve in ways you couldn’t before.”
After he said that, I understood what he was saying and why. I look back on it and think, “I’ve been able to grow so many skills and talents. I’ve been able to serve so many people. I’ve been able to build a team and do things I never, ever would have done, ever.”
Having myeloma is not fun and it’s still a mental game. I still get nervous when I go get my labs run and all that. But I’ve met the most wonderful people doing this.
I’ve taught my kids. They’ve watched growing up. Some of them work at the foundation or have worked at the foundation so I’ve been able to do this together as a family and it’s been an amazing opportunity for the whole family.
Dealing with “scanxiety”
My friend Cindy says, “Every time you go get your labs run, it’s like this red card or green card. Which card are you going to get? Is your myeloma coming back? Do you need to think about it? Do you need to do something about it?”
I’ve been really blessed because my myeloma has not behaved in a high-risk fashion so I’ve had the luxury of time to work on this. Not all patients have that opportunity. Had I been on treatment constantly, I would not have been able to physically or emotionally do what I’ve been able to do so I feel really blessed.
Relapse
In 2016 or so, my myeloma started coming back. It was coming back really, really slowly. It was weird because I was stressed out for the first five years, thinking it could come back any day. But it just helped to be serving people and not worrying about my own situation or my own condition. I didn’t really hyper-obsess about it because I was busy with my family and busy working at [HealthTree].
When do you start treatment again after relapse?
In myeloma, an official relapse is a monoclonal protein of 0.5. We were watching that number and it was 0.13. I first saw it on an MRD test that I did so it was very sensitive and started seeing some early indication. I had this faint band that wasn’t measurable for a really long time, for almost two years, so you couldn’t even quantify it.
But then the numbers started growing and once it got to 0.5, I started having conversations with multiple experts. “What would you do? How would you do it? What’s your strategy?”
It took a couple of years and then once it hit 1, my doctor said “Now it is time to do something.” I got multiple opinions and I had a lot of knowledge about what my options were so I was able to weigh those in my mind.
How long did it take to reach that point?
Probably five years. It was not a clinical relapse. It was a biochemical relapse so just in my numbers. No new lesions. They kept watching for that, of course. Do we have new lesions? We have renal issues. We have high calcium. We have all those CRAB criteria. And no, it wasn’t that.
What was going through your head?
I had done my homework. I know most of the myeloma doctors who are amazing and fabulous. I ended up having consults with Dr. Orlowski, who was at MD Anderson. He did all my maintenance therapy for me so, of course, I consulted with him. I consulted with Huntsman docs — one was leaving and one was coming so I consulted with both of them. I used our own tools to find a CAR T clinical trial that I could join. I flew to the Hutch and talked to Dr. Green about joining a CAR T trial. I knew what I needed to do so I did it.
I got five different answers — five different experts, five different answers. One said, “You could repeat your transplant because you did so well.” One said, “You could do a triple combination, combinations of different combinations, and that would get you out another five years. Then maybe CAR T is a little more developed or a little more curative because now it’s not. Maybe CAR T is too early.” Some said CAR T’s just fine.
I really had to make my own decision. I love the science behind it and I’ve become kind of a geek about it, but I’m also very faith-based and so I combined those two to make a final decision about what I should do. And I determined that I wanted to do CAR T therapy.
I spent several hours looking through all the trials and totally miraculously, there was one open at Huntsman. I talked to my doctor and said, “This is what I want to do.” He said, “Because you know so much, [the] hardest thing will be decision paralysis because you know all the options.”
When I went to him and said this is what I want to do, he said, “Okay, let’s try to get you into the trial.” And that was not a very easy process so kudos to Dr. Sborov for making that happen for me. He was amazing and it was just totally amazing.
I really had to make my own decision. I love the science behind it… but I’m also very faith-based and so I combined those two to make a final decision.
What helped you decide on a course of treatment?
I wanted to see data around it. What are the outcomes, first of all? Then I want to understand [the] side effects. What are the trade-offs that I’m making? Some of it is dosing and frequency. How often am I going to be in the clinic?
Then I have to put all that together with my personal goals. What can I do? Am I working? Am I not working? Do I have a caregiver? Do I not have a caregiver? Do I mind traveling to a facility if I’m going to join a clinical trial? Can my insurance pay for whatever I want? Is it paid as part of the clinical trial, if I get in? Will I even qualify?
You have to weigh all of that. I spent so much time really understanding the science because I was doing the podcast, writing the articles, and so it took me a long time.
Then right about the time I was relapsing, we decided to create a tool called HealthTree University, which is a whole disease curriculum, because I didn’t want a normal patient to have to do what I did. I just wanted them to be able to binge-watch their way through. We have almost 700 video lessons taught by 150 myeloma experts on any topic because then, you could get through that course fast.
You need to be able to ask relevant, intelligent questions at your appointment. Some people just stick their heads in the sand and don’t want to talk about it, but somebody in the family needs to do that work. You don’t live long if you stick your head in the sand and never ask questions.
My friend Pat, who passed from myeloma, said “It’s not fair that you have to do this. You’re feeling crappy and you have this stress that you’re trying to deal with this.” But you have to. You just have to.
To get really good care, you have to advocate for yourself. You have to find the doctor that’s right for you [and] knows a lot about your disease. Those are just things you have to do.
Different myeloma treatment options
It was a triple combination. I could have done dara-Rev-dex (daratumumab + Revlimid + dexamethasone). I could have done dara-pom-dex (daratumumab + pomalidomide + dexamethasone). I could have done RVd (Revlimid + Velcade + dexamethasone). I hadn’t had that because I did VeTd (Velcade + thalidomide + dexamethasone) [the] first time.
When I first started relapsing, daratumumab wasn’t an option. I hadn’t used it before. I could do all the monoclonal antibodies. I could have chosen a bispecific antibody clinical trial but, at the time, they weren’t as far along as the CAR T trials.
One doctor said, “You could just take Revlimid. I’ve had patients on Revlimid for a long time and they’ve done just fine on it. Your disease seems to be pretty indolent or slow growing so one thing might just do it even though that’s kind of not normal in myeloma treatment to do one therapy.”
I just had a lot of options and all the logic made sense. Each one of those options made logical sense. I just had to go back.
When I did the transplants, I wanted a one-and-done therapy so I was looking more for [a] one-and-done kind of therapy. I felt like I’d done my homework on the different CAR Ts and I was happy with the trial. I felt good about it so I said, “Okay, let’s go for it.”
Joining a CAR T clinical trial
I had to be accepted into the trial so they had to have slots open. There was this very unique window of slots open when I was looking for that option. There was a slot open if I qualified and I had to have an M protein over 1 and I did — it had grown over 1 by that point.
But when we sent the sample off to the provider, they said, “According to our numbers, you’re not even at a 1 yet. You’re just barely under. You’ve got to wait a couple of months to see if your myeloma will continue to grow.” It did so we sent off a sample again.
Then I had to be randomized. There was an arm that was a triple combination and an arm that was the CAR T so it was not guaranteed and that’s fine. You never know which arm you’re going to get into. Sometimes they’re blinded so you don’t even know what treatment you’ve got. But with CAR T, that’s pretty obvious which treatment you’re going to get. It’s all computer-generated so my doctor doesn’t even know until they get word from the sponsor if it was available or not.
I went to collect cells and they said, “This will be the easiest part. We never had problems with this part of collecting the T cells.” Then I had an anaphylactic reaction to the gas and the machine. Somehow I’m like 1% of patients or something who had that.
They jabbed me full of epinephrine, dex, and everything and sent the sample off. Of course, the sample didn’t grow because it had so many steroids in it. We had to recollect and that sample worked fine. That process took from March until November.
It was a good thing I didn’t have fast-growing myeloma. I went through the protocol and there was a preconditioning regimen that I did. It was in the big deal category. It wasn’t like my transplants; that was very, very hard physically. This was not as hard. I tried to stay fit before, during, and after just so I could make sure that I was doing what I wanted to do or still could do.
What made CAR T easier to handle?
I had them put a bike in my room and I rode my bike every day. I worked the whole time. There [were] only a couple of days where I felt fatigued from the preconditioning chemo rather than the CAR T.
How long did you have to be in the hospital?
Fourteen days. The staff was amazing. My husband watched me. There was a period of time I couldn’t drive but I was still being pretty normal.
Was paperwork noteworthy?
Yeah, but big deal. You’re so lucky to be even getting into a clinical trial that is providing early access to therapy.
You’re going to have to do more testing. I’ve had to go in for more testing before and after. It was a very thorough process to get pre-tested. They had to test your lung function and all your other functions [to] make sure you’re okay and can qualify for the trial.
There was a lot of that, but the trade-off is I got early access to a therapy that’s very effective and afterward, I was MRD negative and still am. It’s been a year. I’m able to work full time and I still manage my family. And so it was great therapy.
Reflections post-CAR T
It was completely amazing because I was willing to travel, but then I would have had to be somewhere for about a month away from everything. With all that I’m trying to do, that would have been hard with my family, with the foundation, and everything. It was great that I could do it the way that I could.
I’m glad I did it. I think it was a great option for me. It fits my personal goals of that one-and-done therapy.
We’re just watching it. I make sure I get the right testing when I go in to watch for early indications.
I have a feeling of what I want to do after at the point of relapse. I’m still planning ahead, but I’m happy with what I did. I hope I get five-plus years out of this therapy. You never know. Some of the averages is about 20 to 24 months with this one.
Side effects from CAR T
Robert Kyle from the Mayo Clinic — he’s considered the father of multiple myeloma — says there are no drugs that have no side effects. You’re basically picking: which side effect am I okay with?
I knew the data. I had read the data. I went in very informed and felt this was the right thing for me.
What are your thoughts about a cure for myeloma?
When I was diagnosed, no one would say that word. If you said that word and you were a myeloma specialist, you were kind of mocked. No one’s getting cured [of] this disease. This is going to maybe become a chronic disease.
I think there is a certain subpopulation of patients that could potentially be cured. The UAMS data [showed] that functionally cured was in the 21-23% range.
Bart Barlogie really deserves a lot of credit for pushing that protocol forward to do induction therapy, transplant or two transplants, consolidation therapy, and maintenance. That wasn’t really done before. You just got your transplant and then it was nothing.
To see the progress in myeloma, to see how many companies have jumped into the space, to see the different drug classes and the sheer number of clinical trials that are being run, it’s really, truly amazing what’s happening in myeloma.
I’m super hopeful. I think CAR T or bispecifics will probably be part of that curative step. They need to use it in earlier lines of therapy. Transplant will always be good and effective. But I think it’s getting closer.
What should a patient ask during the initial doctor’s appointment?
Ask how many cases of myeloma that person is seeing to identify if they’re myeloma specialists or not. If they’re not seeing over 50 cases a year, you should look for another doctor at least to consult on your case and when you’re making decisions.
You can always go to your local center and get your local infusion. You don’t want to have to drive three hours to go get an infusion because you’re going to the academic center. Anybody can give you daratumumab, Velcade, or whatever. But if you’re making decisions, your life is worth it. Getting a couple opinions is not a bad thing.
We just actually created a document that outlines those questions and put [it] on the website. We have a whole list. What kind of myeloma do I have? Do I have standard risk? Do I have high risk? What labs should I be watching? What are my treatment options? Why are you deciding on this versus this?
We built some of those in our HealthTree Cure Hub tool. We can pull the records that a patient has and help them through that decision-making process. Rafael Fonseca [and I] had had this hypothesis ever since David was diagnosed. We came back to that in about 2018 and said, “Okay, let’s build this,” so we built HealthTree Cure Hub.
We did a 50-city tour [and] met with 850 myeloma patients to say, “Would you use a tool like this? Would you be willing to share your myeloma story with other people if it were to advance research?” Now that has 11,000 patients who participate in that data portal and they get benefits. They get to see treatment options personalized for them.
As a newly diagnosed patient, I can say, “Okay, I have this kind of myeloma. What are my treatment options?” We pull the myeloma experts to say, “How would you treat this newly diagnosed standard-risk patient or this newly diagnosed high-risk patient or somebody who relapsed after Revlimid maintenance? What do you do next? How do you sequence?”
They get back to us on how they would do it and then we build that logic into that tool so patients can do a printout of this option. This triple combo versus this triple combo, transplant, CAR T, bispecifics, or whatever it is. Then they can have this conversation with their doctor, and ask, “What are you going to do about this?”
In myeloma, you have tons of decision-making. You have a lot of choices. Great problem to have but it requires a little more on you to ask a lot of questions so just ask the questions.
There are no dumb questions. Ask your nurse. Sometimes the facilities don’t have enough time. You get this 15, 20-minute appointment and these doctors are trying to do incredible things in that time because they are asked to do too much, in my opinion.
But that’s why we have patient navigators that can help. You can say, “I need somebody to explain my FISH test results because I don’t get it.” Maybe my nurse didn’t have time for me. We’re trying to fill those gaps to help support clinics and patients.
What has been the biggest impact on you?
I have a lot of gratitude for the experts that are working on this. I have a lot of gratitude for the companies that are trying to develop products that can help you live longer. I have gratitude for my myeloma peers and it’s helped me to get to know others. I have my patient advocate friends who have been doing this for 20-plus years. I just met the nicest people ever in doing this.
It’s been a really rewarding experience. I love helping patients. If somebody calls me and says, “I don’t know what to do,” my favorite part [is] to walk somebody through. “Okay, here’s what you need to ask, and here’s what you need to do. Go do that then come back and talk to me.”
Because I was only one person, we created a coach program because I couldn’t do that all the time. I had to replicate myself.
Leaning on faith
It’s all intertwined [with] my faith. I had to get to the point where I was okay [with] dying. I was okay with whatever was going to happen with me and with God’s will essentially. [It] was not easy to come to that point. It took a lot of years to get to that point.
I think sometimes, you’re doing things out of anger or urgency. Then at some point, you have to just stop doing it out of fear and just say, “Okay. It’s okay whichever way it goes.” But that’s because I have this long, more eternal perspective of my life.
I existed before. I’m here now and I’m thinking I’m going to be fine later so that helps me, too, because it just gives me a different perspective. I don’t panic as much with that knowledge.
How I look at all adversity… First, what do I do? Then what am I supposed to learn?
Dealing with adversity
I think I went through that probably [around 2019]. When you get diagnosed, you first have to say, “What am I going to do?” The first thing you need to consider is what you’re going to do. Then, later on, you can go, “Okay, what am I supposed to learn from this experience?”
That’s how I look at all adversity, whether it’s financial, health, work, or whatever it is. First, what do I do? Then what am I supposed to learn?
Sometimes this adversity [lasts] a long time. It requires a lot of patience and doesn’t resolve quickly. You think, “Why is this dragging on so long? This is terrible adversity. Why do I have to go through this?”
You never want to be told when you’re in the middle of it, “You’re going to learn something great from this.” You may think, “That’s so annoying. Don’t tell me that.” But it’s true. You do look back on it and think, “Wow, I learned a lot from that.”
The last thing I asked myself [was], “Who can I serve through this experience?” Because that’s really where the joy and the meaning come.
We’ve had coaches who’ve come to us and said, “I was suicidal with my diagnosis and having serious mental health problems. I started coaching patients and it just changed my life. It just completely changed because my focus isn’t internal anymore. It’s external.”
Having cancer, you’re able to let go of a lot of the unimportant. None of that matters in life. It’s my family, my faith, and who I’m serving [that] give me the most meaning.
Inspired by Jenny's story?
Share your story, too!
Multiple Myeloma Stories
Clay D., Relapsed/Refractory Multiple Myeloma
Symptoms: Persistent kidney issues, nausea
Treatments: Chemotherapy (CyBorD, KRd, VDPace), radiation, stem cell transplant (autologous & allogeneic), targeted therapy (daratumumab), immunotherapy (elotuzumab)
...
Melissa V., Multiple Myeloma, Stage 3
Symptom: Frequent infections
Treatments: IVF treatment & chemotherapy (RVD) for 7 rounds
...
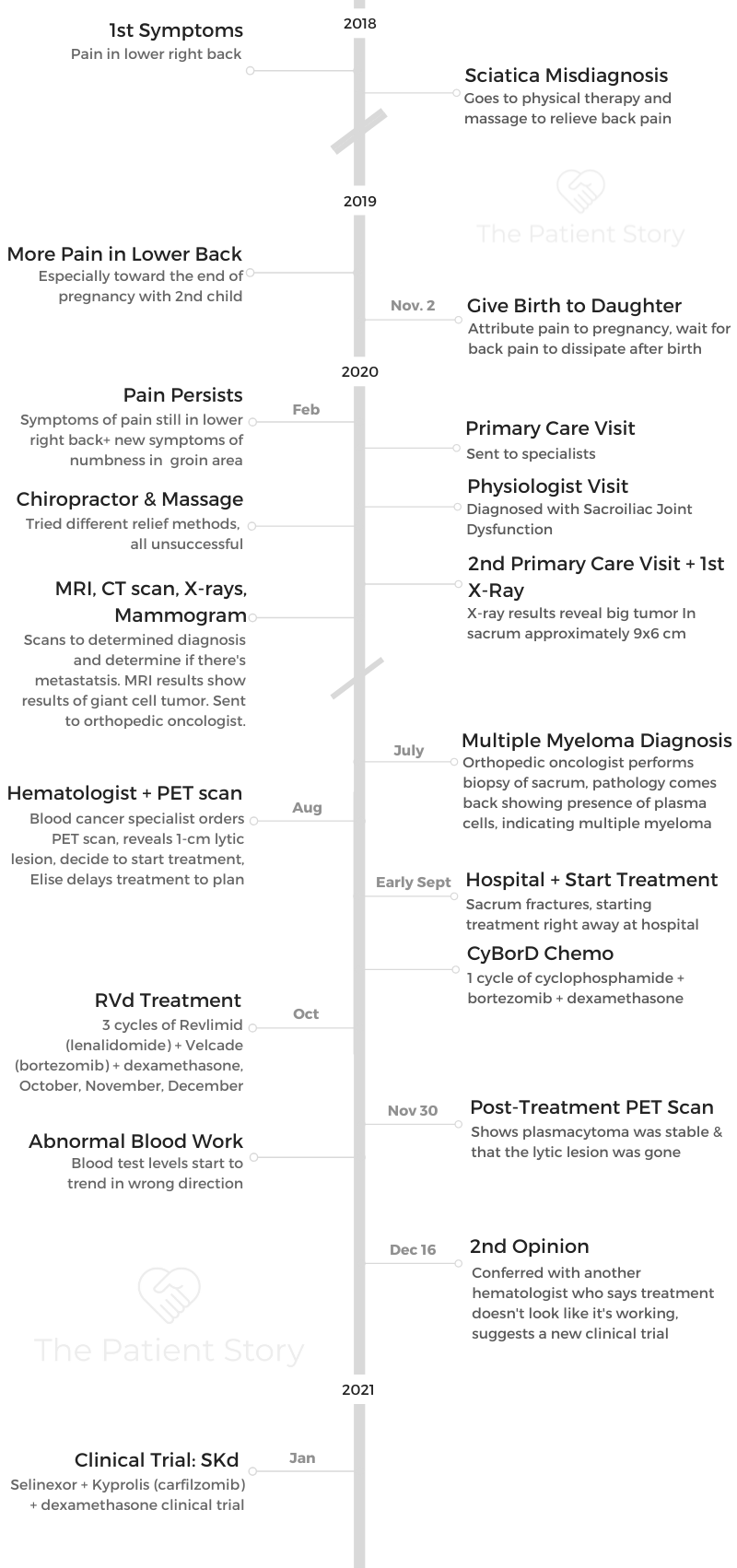
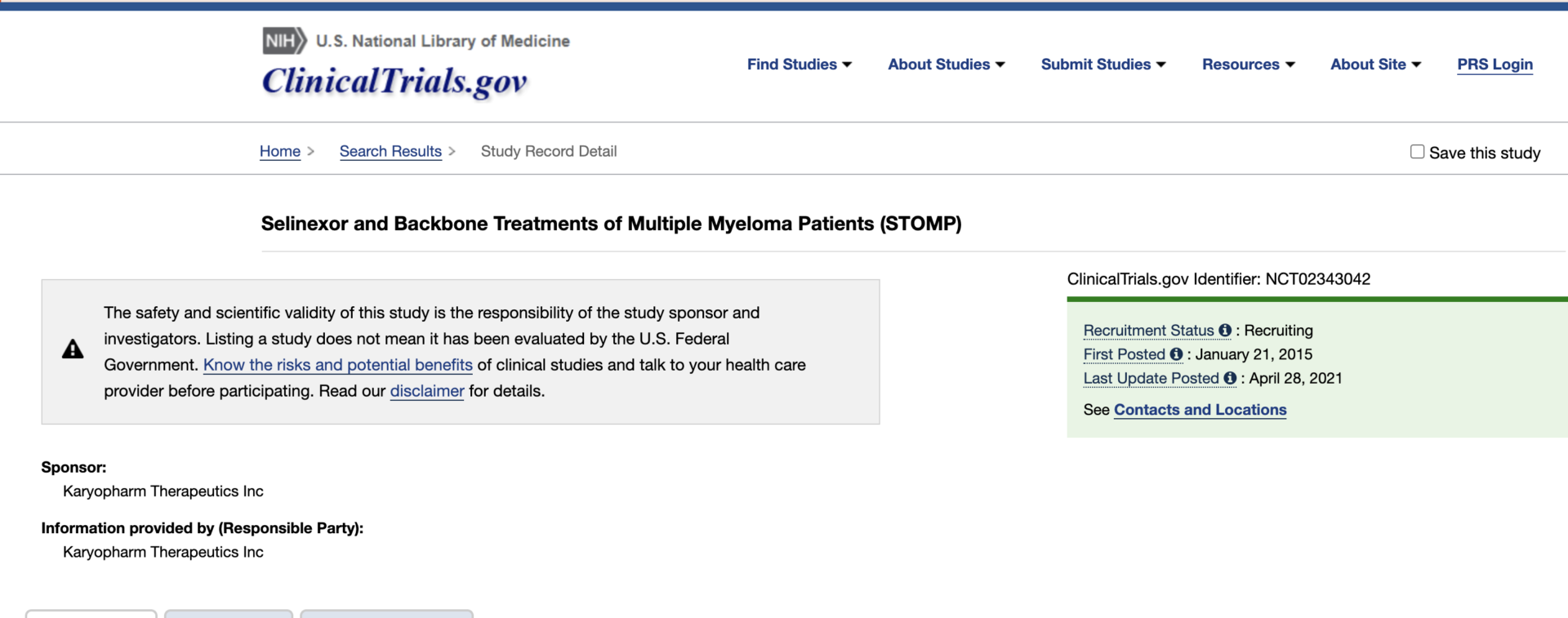
Elise D., Refractory Multiple Myeloma
Symptoms: Lower back pain, fractured sacrum
Treatments: CyBorD, Clinical trial of Xpovio (selinexor)+ Kyprolis (carfilzomib) + dexamethasone
...
Marti P., Multiple Myeloma, Stage 3
Symptoms: Dizziness, confusion, fatigue, vomiting, hives
Treatments: Chemotherapy (bortezomib & velcade), daratumumab/Darzalex, lenalidomide, revlimid, & stem cell transplant
...
Ray H., Multiple Myeloma, Stage 3
Symptoms: Hemorrhoids, low red blood cell count
Treatments: Immunotherapy, chemotherapy, stem cell transplant
...