Margie Wilson’s Endometrial Cancer Story
Interviewed by: Alexis Moberger
Edited by: Katrina Villareal

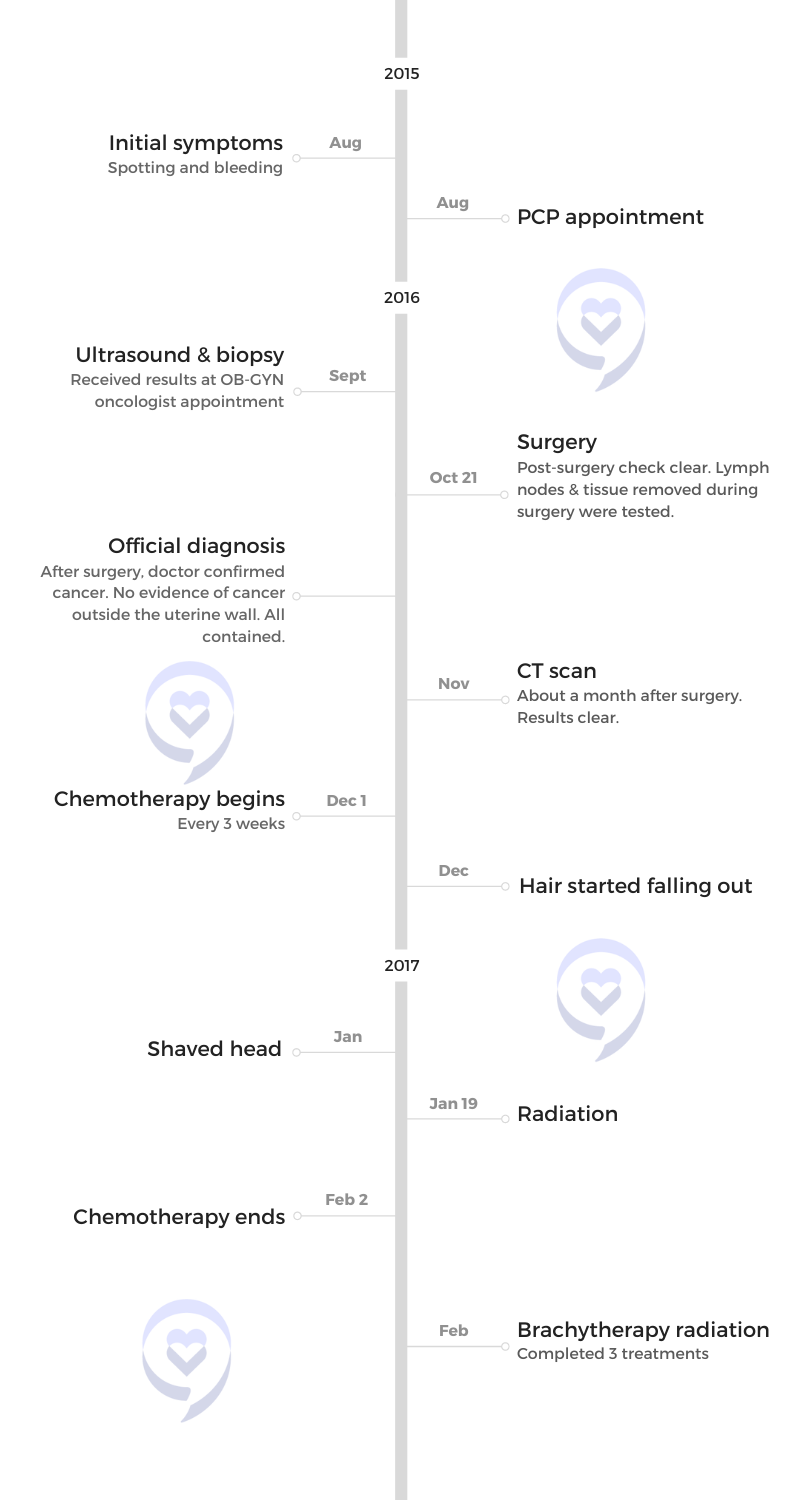
Margie shares her journey with stage 1B, grade 3 endometrial cancer. Initially attributing her symptoms to menopause, she experienced persistent irregular bleeding for years. After consulting her OB-GYN and undergoing a biopsy and ultrasound, she was diagnosed with cancer, leading to a swift progression from diagnosis to surgery, which confirmed the cancer had not spread beyond the uterine walls.
Margie’s treatment included surgery, chemotherapy, and brachytherapy radiation. Despite facing challenges with healthcare providers and navigating the medical system, she sought multiple opinions to ensure the best care. She managed side effects with essential oils and naturopathic remedies, emphasizing self-care and symptom documentation. Margie’s story highlights the importance of patient advocacy, thorough medical documentation, and compassionate healthcare providers, serving as an inspiration for others facing similar battles and advocating for awareness and proactive health management.
For more support in endometrial cancer, visit our friends at ECANA.

Thank you to Karyopharm for its support of our patient education program! The Patient Story retains full editorial control over all content.
This interview has been edited for clarity and length. This is not medical advice. Please consult with your healthcare provider for treatment decisions.
- Name: Margie W.
- Diagnoses:
- Endometrial Cancer
- Staging:
- Stage 1B, Grade 3
- Initial Symptoms:
- Persistent irregular bleeding
- Treatment:
- Surgery
- Chemotherapy
- Brachytherapy
Introduction
I live in Seattle, Washington. I’m single and have two adult girls and five grandchildren. I work with my oldest daughter at home as a grandma nanny. I do a lot of driving, preparing meals, laundry, and help around the house.
I’m the program director of ECANA: Endometrial Cancer Action Network for African-Americans. I facilitate one program twice a month. Right now, it’s chair yoga and conversations where we meet with Black women who have been affected by endometrial cancer. We provide a space to talk, share, and ask questions, and then spend 15 to 20 minutes doing some physical exercises to help people get back on their feet after their cancer treatments. That is one of my passions as well. I’m a fitness instructor, so I teach classes when I can.

I didn’t do anything about the bleeding because I thought it was part of menopause.

Pre-diagnosis
Initial Symptoms
I first started questioning that something might be going on with me when I was in the middle of menopause. When you’re going through menopause, you have all these different symptoms, like hot flashes and mood swings. You could have a cycle for two months and then not have one for three, and then have one for four months and not have it again, but you have to go one whole year without having any signs of blood.
I didn’t pay attention to my cycles, so I don’t know if I ever went a whole year without seeing any blood. I didn’t document it, so my strong suggestion is to document when you start your cycle and when it starts being weird, document how it was. When you’ve gone 12 months with no blood and then now there’s blood, go to your doctor.
I didn’t do anything about the bleeding because I thought it was part of menopause. I felt like I had a cycle every day. Nothing for two days and then I’ll have bleeding for a week, then nothing for 2 or 3 days and then bleeding again for three weeks. It went on for 2 to 3 years, but I was quiet about it.
The spotting and bleeding became heavier. I had no pain, but I just got tired of it and thought, This has to stop. I need to do something about this. On one of my visits, I mentioned it to my OB-GYN. I said, “Shouldn’t I be done? I feel like I’m spotting or I’m bleeding still. Should I still be bleeding?” She said, “Yeah, you should be done.”
Biopsy
My OB-GYN requested an ultrasound. Before I went, she took a biopsy sample in her office. She said, “It’s not going to hurt. It’ll be fine. I need to pull out a piece so I can send it to the lab because I feel like there’s something going on in here, but I’m not sure.”
It lasted only 10 minutes, but I asked her, “Am I going to be able to walk to my car when you’re done?” She was digging in my vaginal area, trying to pull something out. It was so painful. There wasn’t any pain after, but the whole process was horrible. I hope that procedure is better today than it was before. She sent me home with antibiotics.

‘They’re sending you to an oncologist? … Mom, they think you have cancer.’

Ultrasound
When I went for an ultrasound, the tech said, “The lining of your uterus is thick. We need to check that out. I’m going to set you up for an appointment with an OB-GYN oncologist. Make sure you bring somebody with you to that appointment.”
When I got home, I told my daughter. She dropped what she was doing, stared at me, and asked, “They’re sending you to an oncologist?” I said, “I think that’s what she said. OB-GYN oncologist.” She said, “Mom, they think you have cancer.” I said, “How do you know that?” She said, “Because you’re going to see an oncologist.”
She then asked, “Who’s going with you?” I said, “My friend Holly’s going to come with me.” She said, “Okay. Make sure you take good notes and find out what’s going on.” That was my introduction to the possibility of having cancer. Even after hearing that, I thought, I don’t have cancer. Calm down, people.
Diagnosis
Getting the Diagnosis
When I went to see the OB-GYN oncologist, he saw my ultrasound and I thought that he had the biopsy results. He was fast talking and had no bedside manners at all. It was so bad. I’m still like a deer in headlights and you’re telling me something’s wrong with me.
He said, “You might have cancer, you might not have cancer. You might have a carcinoma or you might not have one. You’re 58. You don’t really need all those parts. We’ll take everything out. We’ll have a complete hysterectomy. If we see any signs of cancer in there — we might or we might not — then we’re taking everything out.”
My friend who was with me said, “Excuse me. Can you slow down? Can you tell her what that means? She doesn’t know what you’re talking about.” In 15 minutes, I was on the table getting checked then I was over in the other room, making an appointment for a surgery.
He said, “We’ll know for sure after surgery. It might be, but it might not be,” and then he started naming off different kinds of cancers that it could or could not be. That’s the part I thought was weird. My friend was totally put off by him and said, “She needs her female organs. What do you mean she doesn’t need them anymore?” After making the appointment, she said, “You know you can cancel this if you need to.”

The surgery was supposed to take 2.5 hours but it ended up taking 4 hours… the tumor was too big.

Reaction to the Diagnosis
I was in shock and couldn’t believe it. It all happened so quickly. I was numb for about two months. Everything was a blur.
My youngest daughter, who lives in Chicago, said, “Let’s get the email strings going. Let’s find out what we need for care.” My friends started mobilizing. Then I realized that everybody was talking about me. It was me who’s going through this. I couldn’t see myself at that moment.
I was diagnosed with stage 1B, grade 3 endometrial cancer. The tumor stayed inside the uterine walls, but it was already 80% of it, so 20% more and it would have been out. I got my lymph nodes checked including all the surrounding areas to make sure. All of that came back clear. Thank you, Jesus. I was happy about that.
Treatment
Surgery
The surgery was supposed to take 2.5 hours but it ended up taking 4 hours. They went in laparoscopically and saw that the tumor was too big. They couldn’t get it out, so they ended up having to cut me a little to get it out, which extended the length of time that I was in surgery.
When I woke up, my daughter and some friends were in my room. I was still pretty groggy when the doctor came in. He said, “It stayed inside the uterine wall. We feel like we got it all. We did take some lymph nodes and stuff all around to double-check. We’ll get that back from pathology in about a week.” He said it was like everything dissolved in their hands when they were taken out. It was a relief to hear that he felt like he got it all. When I came in for my 10-day appointment, we received good news: everything was clear. I healed well from the surgery.

He was very calm, kept eye contact, and talked to me like I was a person instead of a number.

Discussing Chemotherapy & Radiation
I didn’t get a second or third opinion until after the surgery because my doctor said, “Let’s get it done and we’ll research as we go.” After surgery, they talked about treatments. At that appointment, he started throwing out information about chemotherapy and radiation. My insurance did not cover the chemo with that hospital, so I had to go to another hospital. He was saying I needed 6 to 8 rounds of chemo and 6 to 7 weeks of radiation to make sure because uterine cancers tend to hide.
Getting a Second Opinion
I was referred to the Fred Hutchinson Cancer Center in Seattle, Washington, for radiation. When I talked to the doctor, who was my second opinion about chemotherapy and radiation, he said, “I’ve looked at all your files and it looks like we’re going to probably do 4 or 5 rounds of chemotherapy and maybe 4 or 5 weeks of radiation after.”
He was the complete opposite of the other doctor. I was in his office for probably an hour. I had people with me who were taking notes. He was very calm, kept eye contact, and talked to me like I was a person instead of a number.

I met Dr. Kemi Doll, who was my third opinion and became my chemo doctor. She asked me questions and gave me time to answer. She went back to repeat what she already said to make sure I understood everything.

Getting a Third Opinion
My daughter, who lives in Chicago, was working and doing research as a professor at the University of Washington and UW Medicine. She met a doctor who knows the doctor who was going to be my chemo doctor. She’s emailing and texting me, “Mom, I just talked to so and so who’s going to hook you up with so and so. They’re going to call the office and then call you. You’re going to go see them because she’s an expert in this area.” That’s how I met Dr. Kemi Doll, who was my third opinion and became my chemo doctor.
She asked me questions and gave me time to answer. She went back to repeat what she already said to make sure I understood everything. She drew pictures. “This is this, this is this. If you don’t do chemo at all, here are the percentages that your cancer may or may not come back. If you do this much chemo, this is the percentage.”
She said, “We’re not going to do pelvic radiation. We’re going to do brachytherapy.” She explained what brachytherapy was and why. She said, “At your stage and from looking at all your records, this is preventative. Your chemo and radiation is all preventative. We want to make sure it doesn’t come back.”
I finally agreed to do four rounds of chemo and then brachytherapy. Dr. Doll said, “You’re way too anxious about the chemo, so we’re going to get it started as soon as possible.”

She said, ‘I have a feeling you’re going to do great. This is not going to be what you think it’s going to be.’ I was grateful to hear that.

Chemotherapy
At my first session, I didn’t have my port yet so I did it through the arm. My daughter from Chicago flew in. Dr. Doll showed up too. She said, “I have a feeling you’re going to do great. This is not going to be what you think it’s going to be.” I was grateful to hear that. Then she said, “I think you’re going to handle it well, but if you don’t, then we’re done. We’ll do brachytherapy and we can be done with the chemo.”
You have to get blood work done two days before a chemotherapy session to make sure that your platelets and your blood count are up. Otherwise, they can’t give you chemo. Before my last session, mine were low. They called me and told me to come in so they can give me a shot to boost the cells up and have my last chemo the following week. Then she said, “By the way, your insurance doesn’t cover it and it’s about $2,000.”
I said, “I’m good.” She said, “Are you sure? We’ll show you how to do it and then you go home and do it over the weekend.” I said, “No, thank you.” She wasn’t happy. She said, “If your temperature goes up, go to emergency. You’re very vulnerable right now because your immune system is low.”
I wore a mask for a week and that was in 2017. I immediately went to my list of foods because there are foods that help boost your immune system. I looked like I’m already eating lots of them, so I made sure to eat more, like twice a day. I protected myself and made sure that in the environment I was going in, nobody was infected with anything. I didn’t ignore what she said.
The next day, my doctor called me and said, “I talked to the nurse. She told me about her conversation with you and she told me your decision. I want you to know that this is your body. You make decisions for you. When you come for your last chemotherapy, they’ll do blood work right before to check and make sure that it’s at the level it needs to be. But if not, then we’ll skip it and wait another week. Or we could be done. It’s totally up to you. You decide whether you want to do that last chemo or not, or we can just call it. Let me know. Keep doing the stuff that you like to do for your own health. If you have any questions, call me or text me.”

I didn’t have one bout of nausea. I dealt with neuropathy and brain fog, not being able to focus on something for long periods of time.

When I went in for my last chemo, my girlfriend who went with me and I had two plans. We said, “If I don’t do chemo, we’re going shopping. If we do chemo, we’re going to high five and say, ‘This is the last one.’” After you check in, you sit in this little room and either they call your name or they walk over to you. They called my name, so I went right back and did my last chemo.
The nurse heard us talking and she said, “You mean you didn’t get the shots?” I said no. She asked, “What did you do?” The whole time, she was talking about my diet. I believe that the body is made to heal itself. Not that I don’t believe in all the other stuff, but I believe that and I was just done. I couldn’t give anymore.
Managing the Side Effects of Chemotherapy
I use essential oils, so I immediately checked to see which oils help with nausea. Nausea is one of the possible major side effects you could have from chemotherapy. And you know what? I didn’t have one bout of nausea.
I dealt with neuropathy and brain fog, not being able to focus on something for long periods of time. It takes away from who you know yourself to be. For the neuropathy, I soaked my feet, rubbed my feet, and wore good, comfortable shoes.
I also saw a naturopath once a month. Acupuncture helped with the nausea too, so I was grateful to have different avenues.

Because I felt good, I was pretty okay, but in the back of my mind, it’s always there.
Brachytherapy
The radiation was scheduled 6 to 8 weeks after surgery because complete healing time is about eight weeks.
Brachytherapy is internal radiation. They take a tube and put it right in your vagina.
When I went to my first brachytherapy appointment, they got me ready and put my legs up in the stirrup. They had everybody in the room to look: the interns, the specialists, and all that. I sat mortified. I’m glad I took a pill to keep me calm. Then he said, “I still see some blood up here. You are not completely healed.”
My first appointment was a wash. He kept apologizing and asked, “Where do you live?” I said, “Just down the street.” He said, “Oh, good because some people have to travel. Let’s give this two more weeks because this needs to be completely closed before we do any radiation.”
I came back two weeks later and by the end of February, I was done. I didn’t have any major side effects from brachytherapy.
Follow-up Protocol
I ended my chemo in February 2017. I saw Dr. Doll every three months. In 2018, I saw her twice a year. I went in every six months for blood work and checkups. In 2019, I saw her once and then I was good.
Because I felt good, I was pretty okay, but in the back of my mind, it’s always there. A month or two before the appointment, if I knew I was going to see her again, I would have to do a lot of deep breathing and checking myself physically, thinking, You know the signs, you know what to look for, and being aware of my own body. If I hear from her within the next 24 or 48 hours after my appointment, I wonder why. Each year got better.
The work that I do with ECANA helps, but sometimes it doesn’t because I feel like I’m constantly reliving that hard season of my life.
The only thing that still happens that’s annoying me are the sharp pains that I sometimes get in my wrist, my hands, or my feet, which I believe are side effects from neuropathy. They say it doesn’t really go away, but that’s about it.

Don’t let a doctor dismiss you or tell you that what you’re experiencing is all in your head. If they don’t have an answer, find someone who does.

Words of Advice
If you start going through menopause and your cycle starts going crazy, document everything. If you have not had your menstrual cycle in more than 12 months and then all of a sudden, you have a cycle or see blood, go see your doctor. That is the strongest message from my journey that I speak loudly about because I didn’t know to do that. I didn’t keep a journal. I didn’t pay attention. I figured I was in menopause so when it’s done, it’s done.
Find a doctor who you like, who’s going to listen to you, and who’s not going to dismiss you. It’s not okay for a doctor to presume what you’re feeling and what you’re going through. They’re supposed to listen to you.
As the patient, you are the most important person in the room. When I was at the 2024 SGO Annual Meeting in San Diego, I saw a black and white picture on a screen that said: as a doctor, if you listen long enough to your patient, they’ll tell you what’s wrong with them. Make sure the doctor listens to what you have to say. You’re not just another number.
For years, I’ve thought that the doctor knows everything. No, the doctor doesn’t. All the doctor knows is the book. You know you. Don’t let a doctor dismiss you or tell you that what you’re experiencing is all in your head. If they don’t have an answer, find someone who does. If the doctor doesn’t have your respect, leave and find one you can. That’s so important. It’s you that you’re talking about, it’s your health. You have to be able to communicate in a way that’s clear and where you feel like you’re being heard.


Special thanks again to Karyopharm for its support of our independent patient education content. The Patient Story retains full editorial control.

Inspired by Margie's story?
Share your story, too!






