Nicole’s Stage 1 DCIS Breast Cancer Experience: How She found ‘Beauty in the Breaking’
Nicole is a self-described “bubbly” career coach and avid solo traveler, but everything changed when she felt a small lump in the shower. She was 41 and had never had a mammogram. Still, she went on a planned trip to Milan, but cut it short to get her lump checked. Imaging led to a biopsy, then a meeting with a nurse navigator that made everything feel real. Days later, during her annual exam, she heard the official words: ductal carcinoma in situ (DCIS) breast cancer, a very early form.
Interviewed by: Ali Wolf
Edited by: Chris Sanchez
Nicole remembers sitting in a paper gown, mind racing about deductibles as a self-employed person, then driving straight to her brother’s office, repeating, “She said it’s cancer.”

Nicole’s DCIS breast cancer was fast-growing and aggressive, but caught early. Her surgeon told her she had saved her own life by finding the lump when she did. Within 13 days of meeting her care team, she underwent a lumpectomy with clear margins and no lymph node involvement. Then came one of the hardest decisions: whether to do chemotherapy. She had the choice because her Oncotype score was right on the cusp. After prayer and reflection, she chose chemo as a preventive measure to lower the chance of recurrence.
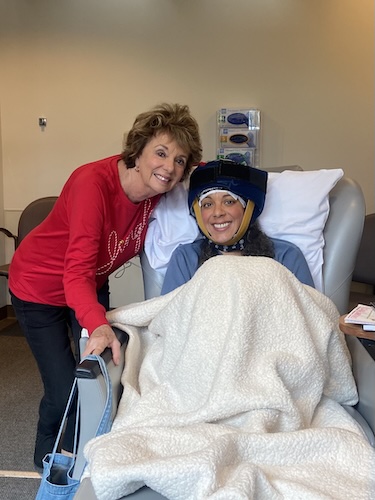
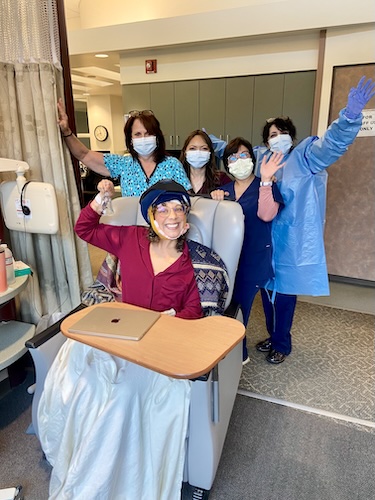
Her treatment plan included four rounds of chemotherapy, a month of radiation, and ongoing tamoxifen. Throughout it all, Nicole fiercely protected pieces of herself, especially her curly hair, through cold capping.
Today, Nicole describes herself not just as a survivor, but as someone transformed: softer, more empathetic, and more willing to sit with others in their darkest moments. Looking back, she calls her breast cancer experience “the most beautiful” of her life, not because it was easy, but because of how it expanded her capacity for love, faith, and connection.
Watch Nicole’s video or read the interview transcript below to know more about her story.
- Her DCIS breast cancer experience started with a self-detected breast lump before a trip abroad, showing how fear and denial can live right alongside intuition
- A theme in Nicole’s story is the importance of community; once she shared her diagnosis, she discovered a powerful network of family, friends, survivors, and patient advocates who held her through every phase
- Her relationship with her mom deepened as they navigated caregiving, vulnerability, and independence together, transforming two strong women into a softer, more mutually supportive team
- Through this experience, Nicole’s perspective shifted: she now sees her body as resilient, her life as “a blessing” simply because she is alive, and her cancer chapter as lesson in empathy that allows her to sit with others in grief
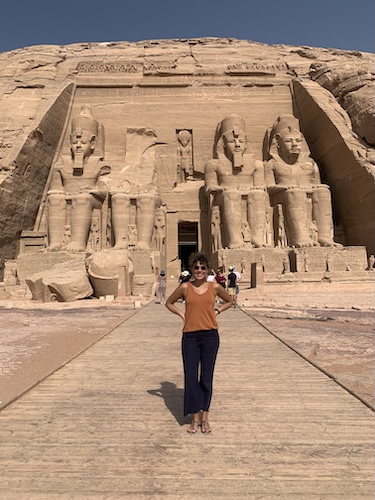
- Even after treatment, she keeps her “bubbly” identity and love of travel, integrating cancer into her story without letting it define or diminish the parts of herself that bring her the most joy
- Name: Nicole F.
- Age at Diagnosis:
- 41
- Diagnosis:
- Breast Cancer (Ductal Carcinoma in Situ or DCIS)
- Staging:
- Stage 1
- Symptom:
- Appearance of a lump in the right breast
- Treatments:
- Surgery: lumpectomy
- Chemotherapy
- Radiation therapy
- Hormone therapy: tamoxifen
This interview has been edited for clarity and length. This is not medical advice. Please consult with your healthcare provider to make informed treatment decisions.
The views and opinions expressed in this interview do not necessarily reflect those of The Patient Story.
- My name is Nicole
- My bubbly personality and love of community
- Travel, faith, and what lights me up
- Faith, perspective, and traveling alone
- Perspective, advocacy, and humanitarian work
- Food Network to Genentech and oncology work
- The first sign that something was wrong
- Delaying the doctor to take a dream trip
- First mammogram, biopsy, and realizing it was cancer
- Hearing “It’s cancer” at 41
- Financial fears, travel plans, and an amazing care team
- From hiding the lump to feeling deeply supported
- Meeting the care team, and my fast‑growing tumor
- Oncotype score, tough chemo decision, and prevention
- Chemo side effects, hair, and cold capping
- Hair trauma, mom as caregiver, and the chemo cut
- My mom, our small family, and caregiving
- Chemo, radiation, and tamoxifen
- Living as a stage 1 breast cancer survivor
- Beauty in the breaking, and how cancer changed me
- Grief, anger, and the feeling of drowning
- Owning “bubbly” again after cancer
My name is Nicole
I live in San Francisco, born and raised in the Bay Area, and in October of 2023, I was diagnosed with stage one breast cancer.
My bubbly personality and love of community
Yeah, so I think the word I get most is “bubbly,” which I’ve gotten since I was young. I’m like, is that young? But I love bringing joy. I love bringing people together, building community.
Whether that’s at church, in my volunteer work, or in my work as a career coach, I think most people are just like, “I really like the energy you bring. I feel like I could be really comfortable with you,” and I love that. I love that people can just be themselves and find a place.
Travel, faith, and what lights me up
On my first trip abroad, when I was 16 years old, I went to Romania to work with kids on the street. Then I studied abroad in Florence years later, and I loved the freedom that came with travel. I’ve been solo traveling since my first sabbatical, when I was at a company called Genentech, when I was 29. I love learning new things through culture.
Travel has been such an extensive part of my life that that’s where I’ve always spent my money and my time. I’ve been to all 50 states, 70 countries on seven continents, and I think about five Canadian provinces. I love learning about people, and I love learning about myself through other people’s eyes. “I love learning about people, and I love learning about myself through other people’s eyes.”
Faith, perspective, and traveling alone
I’m a believer and a woman of very deep faith. So to me, when I travel, I see the mountains, the seas, and the cities as love letters to me. It’s like you go out and you see that I know what I know, and I don’t know what I don’t know. When I go out beyond myself, I learn so much more about empathy.
Empathy is a very big thing for me, and I think the best way to see that is to be in other people’s shoes as much as you can. You can’t always do it. But I’m so filled; I’m filled to the brim when I’m traveling and learning new things, seeing how far I can push myself, and strengthening the muscles of resiliency. To me, it’s really important to see the difference between being lonely and being alone, and knowing that I can travel alone and survive it. I can sit at a table and eat alone, and I can meet new friends.
I love Airbnb experiences because I’m always meeting new friends and new people. The quote that says, “A stranger is a friend you just haven’t met yet,” is so true. I now have friends all over the country and the world because I love meeting new people and seeing the world through other people’s eyes. When I come home, I feel so full because I realize that my little thoughts are so small in comparison to everything else.
Perspective, advocacy, and humanitarian work
That’s what I’ve been dancing around. The perspective that other people bring makes you vote differently. It makes you talk to people differently. It makes you represent yourself differently. It makes you speak out for the other.
Some people don’t have voices, and I love speaking on behalf of those people. I’ve done a lot of humanitarian work as well. Seeing what life looks like in other places is a new perspective. “The perspective that other people bring makes you vote differently, talk to people differently, and speak out for the other.”
Food Network to Genentech and oncology work
Well, I started my career at the Food Network in New York City, in Manhattan, downtown. It was so cool. But then I wanted to move back to the Bay Area, and my aunt at the time was like, “You need to work at this company called Genentech.” I was like, that sounds boring because science — and I was a broadcast journalism major in college. So I thought, “Science, I don’t know if it’s up my alley.”
Honestly, my eight years at Genentech were the highlight of my career. I worked in oncology. I worked on Herceptin; I worked on all of our oncology portfolio and met amazing physicians and nurses — salt of the earth, the best people ever created — and salespeople who were changing the face of cancer in real time, which was really cool because Genentech’s products were standard of care. From that, I did a lot of meeting planning. I met a lot of patients. It was a really cool experience, and the people there were phenomenal. The products we were making were earth‑changing for people.
The first sign that something was wrong
I found, I felt, a lump on my right breast when I was in the shower. It was one of those things where you’re just kind of doing your thing. I was not being super responsible and doing a breast self‑exam and all those things. I hadn’t even had my first mammogram. I thought, “This feels weird.” I felt it with this part of my wrist, and I thought, that feels weird that there’s something there.
You kind of think about it, but it never happens to you. It’s not supposed to happen to you. So I didn’t think too much.
But then I mentioned it to my best friend. I said, “It just feels weird. There’s this thing here.” She said, “Let me feel it,” as girls are wont to do. I asked, “What do you think?” She said, “It feels like a blueberry.” Then I went to my mom and asked, “What do you think?” She said, “It’s better to get it checked.”
Delaying the doctor to take a dream trip
Being that I love to travel, I had a trip to Milan scheduled, and I really didn’t want to miss it. I thought, “If this is cancer, I don’t want them to tell me I can never travel again.” So I actually went to Milan for two months, knowing this, knowing that this lump was here.
Women are so intuitive, and as I was there, I thought, “This just feels weird.” I kept feeling weirder and weirder. I did leave a little bit earlier to come home, and that’s when I showed it to my mom. That week, I went to my physician because it was there. It was not there, and then it was there. It wasn’t gradual.
I want to speak to that. There is a fear. You don’t think it’s going to be you, but you’re also like, if it is me, I don’t want to face it, maybe. I don’t want to uproot my life, even though this is a very big deal. Cancer is a big deal. Illness, grave illness, is a big deal. But I just thought, I don’t want it to upset my life. I don’t want it.
First mammogram, biopsy, and realizing it was cancer
So I went to my doctor. It was so fast. I went to my GP, who I’ve gone to since I was in high school. She said, “Okay, we’ll see. You’re due for your first mammogram anyway.” So we did an ultrasound and a mammogram, a bilateral mammogram.
It was very interesting because the radiologist came in and said, “This feels suspect; you need to come in for a biopsy.” I thought, “Okay, kind of no surprise.” I had friends who were like, “Oh no, I’ve had to have a biopsy before.” But then they walked me into the nurse navigator’s office, and I thought, “Why am I here?” I went by myself. My mom didn’t think she needed to come to my first mammogram with me. I’m sitting in this office, and she’s saying, “If this is cancer, these are the next steps you take.”
I was like, what? I’m so confused. Why is that me? I’m so confused as to why we would be talking about this. I got home because we have a family dinner at my mom’s house every Tuesday, so all my appointments were on Tuesday. I got home, my brother was there, my two nieces were there, my mom was there, my sister‑in‑law had a night off, and I just started crying. I absolutely started — I think I knew then what it was. I think I cried more then than when she told me it was cancer.
I went and got the biopsy on a Monday. I had my annual physical on a Wednesday. It was so apparent that they were like, “There’s no way that we’ll know by Wednesday.” I had an appointment on Friday, and I found out on that Wednesday, after the Monday biopsy, that it was cancer.
Hearing “It’s cancer” at 41
I was 41.
It was like, are we — so my mom was supposed to be with me again, but I was just going to my annual appointment. My physician said, “I have the results here if you just want to know.” My mom was supposed to be with me, and I kind of knew. I thought, if it wasn’t anything, she would have just said, “It’s nothing,” and off we would go.
I’m sitting there in one of those paper gowns, getting ready to have a Pap smear, and she said, “Do you still want your Pap smear?” I said yes. Another big thing for people is that I’m self‑employed. I pay for my own insurance. I was already imagining my deductible going through the roof. I only have a certain number of visits. I was off my Genentech, my Meta, my Airbnb — everywhere I had worked — plans and had to have my own insurance.
I just remember being there. I was shocked, and then I started crying. She said, “Can I hug you?” and I thought, “That’s the least you could do. I’ve known you for 20 years.” I was stunned. I didn’t know where to go or what to do. I immediately texted my friend Kirk, and then I immediately called my friend Elaine, one of my nurses from Genentech, a hematology nurse, and she talked me off the ledge.
My doctor also didn’t know too much. She said, “All I know is that it’s cancer. I can’t really tell you anything else.” I thought my mom would be at Bible study, so I drove to my brother’s office, my big brother. We’re all very close. He was out; his receptionist had him come back. I just kept saying, “It’s cancer. She said it’s cancer. She said it’s cancer.” I was also crying there. I was a bit hysterical, but you’re in shock, like, what is happening? The shock was absolutely overwhelming in the moment.
Financial fears, travel plans, and an amazing care team
I was actually supposed to go back to Milan in the fall, right when I was diagnosed again. I was telling my friends over there, “I don’t know if we can make plans, because this thing is happening.” It’s true: my whole world shifted. I’m sure for people with kids, it shifts even more. This is not how it was supposed to turn out. I was supposed to be able to do all these things.
I told my brother, who’s a financial advisor and therefore my financial advisor, “This is not what I saved my money for.” He said, “In fact, it’s exactly what you saved your money for.” I thought I was supposed to be traveling. It sets off a ripple. But my care team was so phenomenal that any question I had was immediately answered. I felt surrounded.
I’ve thought about this: we’re so scared to find out because it is life‑altering. It changes the trajectory of your life. My team said, “If you could have any diagnosis for breast cancer — not that you want one — this is the one to have because it’s run‑of‑the‑mill. We’ve got it. We can treat it.” The fear of handling it alone or not knowing pales in comparison to what happens when you get the news and find out how surrounded you are by people, by patient advocates, by friends, by family, by people you didn’t even know had breast cancer or a type of cancer. You find out so many more people, and they surround you. That’s a really beautiful thing that comes out of being in the cancer community.
From hiding the lump to feeling deeply supported
If I go back to that time in Milan, I wasn’t telling anybody, because obviously that would be irresponsible. There would be so many things about living with a lump in your boob for two months and not doing anything about it. I want to name that, because sometimes we let things go, and we should address them. I would have just been scared by myself, because I knew something was different with my body, and I was living in this dream world where nothing would happen, even if I got it checked and nothing happened.
When I finally did share, I had friends who came immediately. They were shopping for me. They were on my couch, answering questions. You find out, oh my gosh, I’m so supported and so well loved, even by people you don’t know. It doesn’t have to just be your family; there are people, survivors. It’s an amazing community.
The amount of conversations I’ve had across from people, just having tea together, to be an encouragement — saying, “I’ve been there. I understand. I understand the grief. I understand the fear. I understand not knowing how to navigate the insurance or having to call weekly to say this should have been approved, but it wasn’t approved” — is huge. You’re constantly doing it when you’re feeling well and when you’re not feeling well.
Talking about my energy, I would go to different appointments, and they’d say, “Are you really going through chemo? Are you going through radiation? Were you just diagnosed?” Because I would be, to me, to be alive is a blessing. That’s it. That’s what’s great. At the same time, the chemo part of it was really hard because I didn’t understand how I couldn’t will my body to feel a different way. I thought, “Oh my gosh, you’re letting me down.” But at the same time, my body also protected me. We’re these resilient beings. It protected me and kept me safe through all of it.
Meeting the care team, and my fast‑growing tumor
One of the best things my care team did was to have a nurse navigator. She made sure I knew who everybody was. We were supposed to have a call on Friday because I was told on Wednesday. She moved things around; we had a call on Wednesday. By Monday, I was meeting my care team: my radiation oncologist, my surgeon, everyone. I didn’t get to meet my medical oncologist right away because my insurance didn’t cover the person who was on.
I thought, “I don’t need chemotherapy. I’m super great.” My surgeon, whom I met, said, “We can get this; it’s in a great place; it’s going to be a lumpectomy, not a mastectomy,” all these things. I met the whole care team while I was still stunned. My surgeon said, “Six months ago, this wasn’t here.” It was a fast‑growing, aggressive tumor. She told me that I saved my own life. She said, “If you had waited even a couple more months, this would be a totally different conversation.”
While I was sitting in Milan, being like, “Should I? Should I not?” — it was growing exponentially at a 40% rate, which is quite high for a Ki‑67 score. Within 13 days, it was out. I had an MRI to make sure it hadn’t spread. There were so many appointments, but between the time I knew and my lumpectomy was 13 days.
I thought, “We’re going to be totally fine.” There was no lymph node involvement. They had clear margins. They got it right out. My surgeon called my mom and told her I was cancer-free. That was mid‑October, and in early November, I saw my oncologist for the first time. “My surgeon told me, ‘You saved your own life; if you had waited a couple more months, this would be a totally different conversation.’”
Oncotype score, tough chemo decision, and prevention
I kept trying to move that oncology appointment earlier because I was pretty sure that with a high Ki‑67 score and how aggressive the tumor was, my oncotype score would be high. That’s the score used to figure out whether chemo is necessary for premenopausal or postmenopausal women. It was right on the cusp, and I had to decide to do chemo.
My oncologist said, “You’re on the cusp. If it were this, I’d say yes, chemo. If it were that, I’d say no. But you’re on the bottom where you don’t need to, but with this margin of error, what is the difference?” I went home and thought about it. I prayed about it. My mom gave me space. Then I decided, “Okay, we’ll have to do it. We’re going to do chemo.”
The one thing I didn’t want to do, from the moment of getting the diagnosis, was chemo. Please don’t let me do chemo. I did not want to lose my hair. I found out afterwards that it’s the biggest concern for many people. I did not do any online sleuthing because I thought, “This is only going to depress me.” For me, as a big personality with big energy, my big curly hair was a huge part of my life. Being mixed race, it took me a long time to appreciate my hair. It was a very big thing to be like, wait, you can’t take it from me. This is a huge part of me.
Women think about their hair all the time. If you have long hair, cutting it to a pixie cut would be a huge decision. That was what I was thinking, but I said, “We’ve got to do it. My being healthy and alive is more important.” At that point, chemo was preventative. It was to cut down my recurrence rate. That was a very tough decision.
Chemo side effects, hair, and cold capping
It’s a huge thing. I kept saying to everybody, I don’t care how sick I get with chemo. I don’t care about all the horror stories with chemo. I can be throwing up in the toilet for 21 days straight as long as I don’t have to lose my hair. I thought, “My body is resilient.”
My friends said that because of my traveling, I have never gotten sick while traveling. We’re talking street food in Thailand. I’ve never gotten sick. They said, maybe you have so many antibodies or whatever. I didn’t really get very sick during chemo. I did the usual three days afterward, where I was lethargic, and my body felt weird, but thankfully, I was able to handle most of the chemo side effects.
You’re right, the hair is a huge deal. The hair is what makes people look at you and think, “She’s sick, even after chemo.” How long would it take for my hair to grow back? Years. Even now, it would be super short. I was blessed that I did cold capping, and it totally worked for me. I would say it didn’t, but it did. Everyone else was like, “You can’t even tell.” I would say, “I can tell,” but it was a blessing that they have that now as a treatment.
My sorority sisters pitched in — our alum group — my friends helped pay for it because it is pricey. But to keep your dignity, I think it’s an amazing option.
Hair trauma, mom as caregiver, and the chemo cut
My hair was — if you asked me, I’d say it was not unscathed — but it was much thinner. My friends said, “Well, you had a lot of hair to lose.” My mom and I were religious about hair care. My hair was in braids, just soft braids, the entire time. Anytime you see me in a cold cap, you’ll see me in braids.
She would wash my hair. When you wash, no matter what, some is going to come out. A huge heartbreak for me was that my mom was the one who washed my hair, because we did it in the sink. I never got into the shower; nothing ever touched my head. We used a pitcher, and she was the one seeing it come out. I kept thinking what it must be like for her to be taking care of her adult child with the hair coming out.
It was on my birthday. This was all happening through the holidays. My birthday is in January. My 42nd birthday was after round three, and that was the first time I saw bald spots here and here. I remember a picture of me blowing out my candles with my family. At Christmas, my sister‑in‑law’s family saw me in a dress and high heels, my hair big, and they were like, I’m so sorry; I thought Nicole was sick.
For my birthday, I remember seeing it. My mom said, “No one else can tell.” I said, “I can tell.” I could tell that under here it was all gone and thinning. It is very, very traumatic. So much of the journey is sad. It’s just sad. There’s no other word for it. I speak about grief, definitely, but sometimes it’s just really sad.
For all intents and purposes, I remember in May of 2025 going to my hairstylist and friend and saying, “It’s time. It’s long enough here. Let’s do it.” It was this small little bob, but it was my chemo cut. I called it that because my hair was back. Now it’s grown even more.
My mom, our small family, and caregiving
Thankfully, my family was there the whole time. My brother left work early so we could meet my care team and then go to my mom’s house. We’re a very small family unit. Growing up, it was my mom, my brother, my grandma, and me. My grandma passed about ten years ago. My brother has been married for 20 years, so my sister‑in‑law and I are very close, and I have nieces. But growing up, it was the three of us.
When this happened, it was the three of us again. My mom just stepped into action. My mom was a single mom, very strong, very resilient. I think I learned a lot of my independence from her. She stepped into action, and I’m so blessed she took care of me in the home I grew up in. It wasn’t some weird place; I felt so comfortable there. My friends felt comfortable there. I call her the Martha Stewart of the West. It was Christmas, so the whole place was decorated. It was warm.
I did arrange my meal train. She said, “Well, Nicole, I’m not the one who’s sick,” acting like she could do it all. I thought there would be an emotional toll. So I called our friend from church, and she helped organize, because I wanted my mom to be able to take care of herself. I knew she would want to be strong for me, and that’s even more exhausting.
During radiation, I would walk to the women’s center. It took 45 minutes, but I said, I’m going to keep my walks up. She would watch me walk by myself and get teary because my body was weak after chemo. This was just weeks after chemo. There was a space between her wanting to take care of me and her letting me be myself. She walked that line so beautifully.
We learned so much about each other. Our relationship has never been — as two strong women — it’s never been better. She learned how to soften for me, and I learned how to soften for her, needing each other in this time. It was good for us both. There are so many beautiful gems that come out of an experience like this, even though it’s sometimes hard to see. That’s one of them for me.
Chemo, radiation, and tamoxifen
I had four rounds of chemo and a month of radiation. Then I was put on tamoxifen. All this time, I’m planning my next trip because I’m like, “I’m out of here.”
I did four rounds of chemo, 21 days of radiation. Then I met with my oncologist, and she said, “Okay, let’s get you on tamoxifen”—five years of that hormone. I’m two years into the tamoxifen now.
Living as a stage 1 breast cancer survivor
It’s weird. I think the only way to say it is weird. Going through it, I thought, “Well, it’s only stage 1. I only have four rounds. I’m on TC; of my four rounds, it’s a pretty manageable chemo regimen.” My nurses would always say, “No, no, no, no, no.”
Elaine, my dear friend, would say, “The experience is still the experience. It’s still valid. It’s still life‑changing.” I always thought, “I don’t have ‘that’ story. It’s not stage 4. I’m not terminal.” But it’s still the story. It’s still the experience of going through it.
When you’re in it, you think it’s never going to end. Then suddenly you’re two years past it, and you’re like, “Oh.” Suddenly, you’re five years past it, and you’re like, “Oh.” You forget your tumor size, which you thought you’d remember forever. It’s weird to think, “I’m a cancer survivor,” because it is in the past. From diagnosis to my last day of radiation was six months. I wouldn’t even have a baby at that time if I were pregnant; new moms go through longer.
I think it’s about honoring the story, honoring my experience, and saying, “You still did it.” Being thankful for my body, thankful that my body was able to heal, that it handled chemo so well. I would talk to my body. I’d be here in my living room having quiet time, holding myself and saying, “Thank you for keeping me safe.”
Sometimes we think, “My body did this; something mutated and now there’s this thing.” But it also rallied. The immunity rallied around everything else to keep you healthy. For me, it really did, and that’s how I looked at it. But yes, it’s sometimes weird to be like, “Oh yeah, I had cancer.”
Beauty in the breaking, and how cancer changed me
There is a book called “The Beauty in the Breaking,” and I think that title captures it. The idea that I can now sit with people who have gone through deep grief and heartbreak is the most beautiful thing. I have a friend whose husband just went through stage 3 colorectal cancer at 40. I told her, “If you will let it — and this is not all pink roses and rosy glasses — if you allow it, it can be the most beautiful thing that comes out of your life.”
For me, it was. I became a softer person, a more understanding person, a more empathetic person. I became somebody who understands grief, which is not easily understood. Sadness and sympathy, yes, but to sit with people in deep sadness and deep grief is something you can only get by going through it.
I would say this experience has been the most beautiful experience of my life. I can’t remember the author’s name for that book, but “The Beauty in the Breaking” is an absolutely beautiful way to say it.
Grief, anger, and the feeling of drowning
There is not a part of me that I grieve now. In the middle of it, I thought, “Why me? This is not supposed to be me.” Going back to me being a believer, I thought, “I believe in a good God. Why would this happen?” You ask all the questions: why do bad things happen to good people?
In the moment, yes, you’re grieving. There’s pain. I was overcome. There were times I would just yell — not at my mom, but around her — “Why?” Anger. Also, I was on steroids. When you’re in it, it’s like being in a well.
The way I explained it to friends was that I felt like I was drowning. It was after my third infusion. I thought, “I do not know how people do longer than four.” I was tired of being tired — the mental part of it. It feels like I’m drowning, and I know I’m going to survive because people kept saying, “You’re almost done, you’re almost done.” But when you’re drowning, you’re still suffocating. You’re still underwater. Knowing you’re going to survive and someone is going to save you doesn’t make it better.
In the midst, you’re grieving. But looking back at it and looking back at the woman I’ve become, I can only rejoice in it. I talked with a friend, another Genentech gal who has a PhD in something with breast cancer. She lives in Milan as well, and I adore her. We talked about how we would never have this perspective if it weren’t for cancer.
We talk about my traveling, offering different perspectives. We would never have this perspective if it weren’t for cancer. She had her own diagnosis; I had mine. She’s in the clear. I can’t grieve it because so much beauty came out of it, but yes, I was deep in grief when it was happening.
Owning “bubbly” again after cancer
I would still describe myself as bubbly. I am back. I still go to see my infusion nurses. When they see me, it’s, “Oh, there she is.”
There’s a scripture that says, “We are oppressed, but we are not destroyed,” and that’s how I felt throughout. I was oppressed, but I was not going to let cancer have the final word. That’s why I walked to my radiation. That’s why I was always joyful going into my infusions. Cancer was not going to redefine me in that way. It would only redefine me in a better way.
I still feel very bubbly and energetic, still a person people love to talk to. It’s one more thing I bring. I had a client call the other day. We talked about coaching things, and she said, “I saw that you were a cancer survivor.” We talked for half an hour about that, and how she’s also a cancer survivor, and what that looks like.
As I mentioned in the beginning, there’s a camaraderie in being seen and being able to tell your story.

Inspired by Nicole's story?
Share your story, too!
More Ductal Carcinoma In Situ (DCIS) Cancer Stories
Nicole F., DCIS, Stage 1
Symptom: Appearance of a lump in the right breast
Treatments: Surgery (lumpectomy), chemotherapy, cold caps, radiation therapy, hormone therapy (tamoxifen)
Erica C., DCIS, Stage 0
Symptoms: Indeterminate calcifications found on a routine mammogram
Treatment: Double mastectomy
Margaret A., IDC & DCIS, Stage 2B
Symptoms: Pain in left breast, left nipple inverting
Treatments: Double mastectomy, chemotherapy (AC-T), radiation
Alison R., Partially Differentiated DCIS, Stage 4 Metastatic
Symptom: Lump in underarm/breast
Treatments: Chemotherapy, surgery, radiation, targeted therapy