Planning for the Future | Cancer Friends
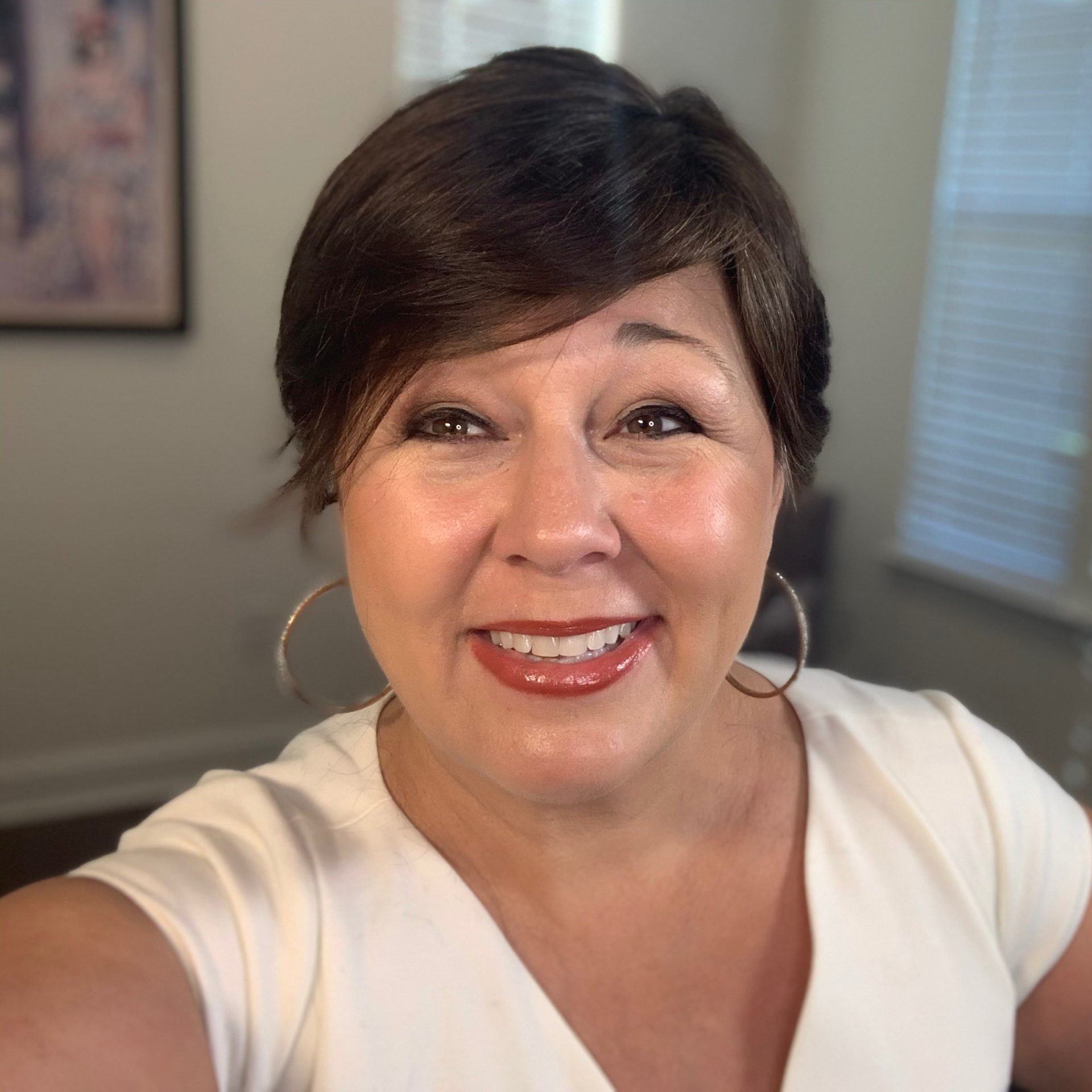
The Patient Story’s new series “Cancer Friends” features Andrew and Esther Schorr. They co-founded PatientPower.info, a resource for other cancer patients and caregivers to help them through their diagnosis and treatment.
In this segment, Andrew and Esther discuss how to plan for the future while dealing with the uncertainty of a cancer diagnosis. They tell the story of deciding to have another child, as well as their mentality of saying yes to life.
This interview has been edited for clarity. This is not medical advice. Please consult with your healthcare provider for treatment decisions.

If the plan has to change, the plan will change, but we’re not going to assume that we can’t do those things.
Esther Schorr
Planning with Cancer
Andrew: Hello and welcome to another edition of Cancer Friends. I’m Andrew Schorr.
Esther: And I’m Esther Schorr.
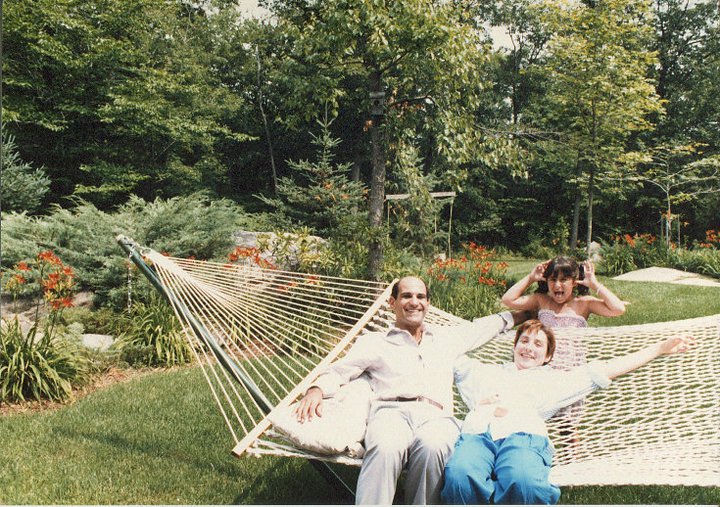
Andrew: We’ve been dealing with cancer for 26 years, me with a diagnosis of chronic lymphocytic leukemia. Then about 11 years ago, the second blood cancer diagnosis, myelofibrosis. But here I am, and Esther’s been every step of the way. We’ve been married 37 years.
We’re doing several segments on the uncertainty that comes with a cancer diagnosis and how you cope and overcome it. What we want to talk about now is, how do you plan? How do you plan for today, tomorrow, next month, next year? [Esther], you’re a planner.
Esther: I am. We’re going to have a chat about this. You and I have different approaches to planning and that has definitely played a part in how we’ve planned after your diagnosis. My first reaction was, “How do we plan anything?”
Andrew: Because I’m going to die.
Esther: It took a little while, took a little counseling together and separately, and it took a little bit of distance from the initial shock to say okay. The way that I’ve planned it in my head, for myself and then for us together, is like planning for the best and anticipating the possibility that longer-term plans may change.
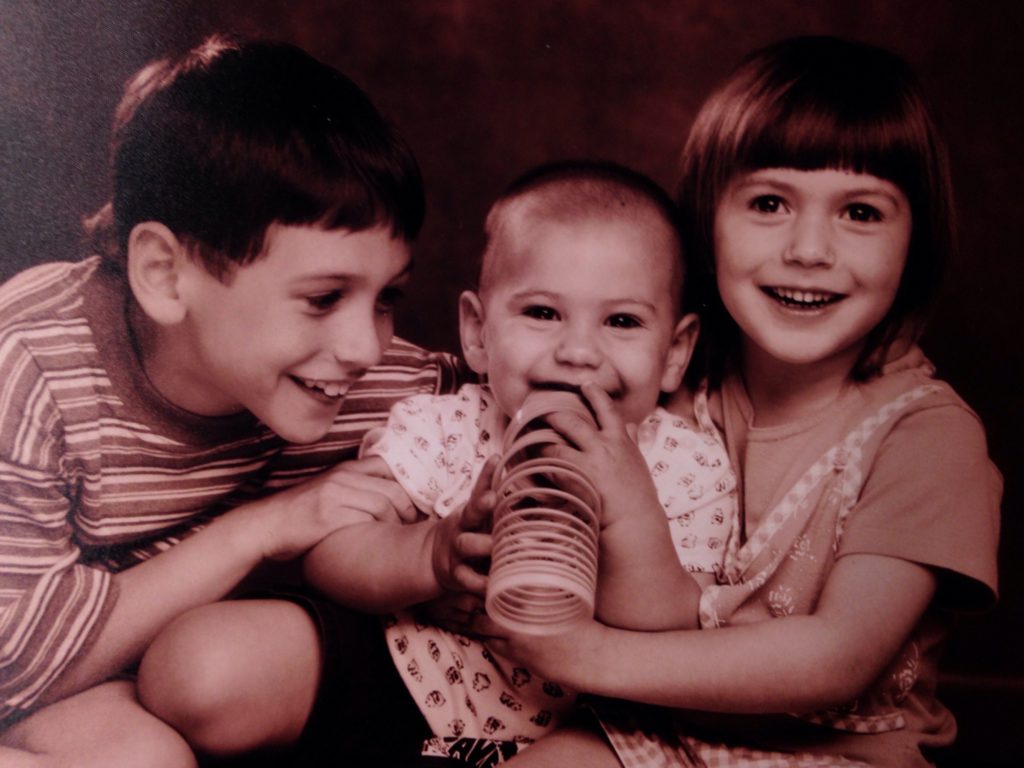
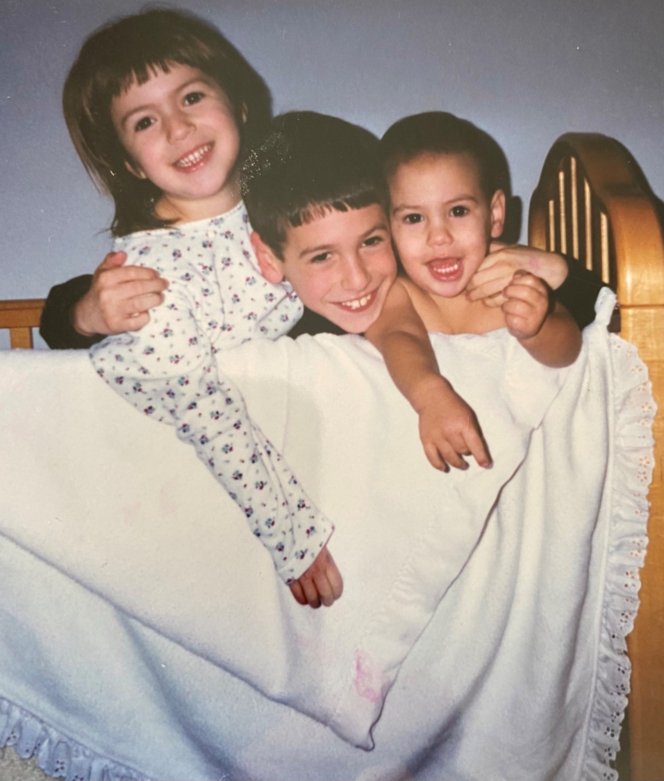
That’s kind of a coping mechanism for me, saying, “You’re here now. We’re here together. We have 3 kids. They’re now grown.” When Andrew was diagnosed, two of them were really little.
[One wasn’t born] yet. At least for me, the planning was, okay, let’s plan for the next year. Let’s see what’s going to happen.
Having another child after a cancer diagnosis
Andrew: Well, let’s tell that story. I was 45 and didn’t get married until I was 35. We had these two little kids, Ari and then Ruthie, about 4 years apart. We’d always wanted to have a third child. I was diagnosed with the most common adult leukemia, chronic lymphocytic leukemia — with the emphasis on “chronic.” Not acute, but chronic. So I had to learn what that meant.
Esther: That was still cancer.
Andrew: You’re living with cancer. My doctor at the time was a world-famous doctor, Michael Keating at MD Anderson in Houston. Esther and I said, “Hey, we had hoped to have a third child. Should we?”
Esther: He gave me a big hug, and he said, “Go have your third child. By the time Andrew needs treatment, we’ll have something good for him. You should live your life.” They did, and Andrew went into a clinical trial and got a long remission. Meanwhile, that third kid is 25 years old and in the music business.
Andrew: We call him the miracle baby. He hates that.
Esther: But at the time, that was a big planning step.
Andrew: That was a major plan. Have the child, so now you’re in the day-to-day stuff of raising three small children. Anybody who’s been through that knows they need, what they need, when they need it, which is often right now. The baby’s crying. Somebody needs a bottle. Somebody needs a ride to school or to soccer practice.
»MORE: Parents describe how they handled cancer with their kids
Planning with chronic vs. acute cancer
Esther: The other thing I think we have to pay some attention to, or at least acknowledge, is you mentioned “chronic.” All the messaging we were getting about your diagnosis was, “This is not a do not pass go and something terrible may happen right away, or even just treatment right away.”
We were fortunate in that we had the time to plan and feel comfortable doing that. I just feel like in this conversation, we have to acknowledge that somebody diagnosed with acute cancer may have to approach planning a little differently than we did.
Andrew: Inflammatory breast cancer Boom. Acute myeloid leukemia. Boom.
Esther: Or a stage 3 or 4 of something.
Andrew: They say, “We’ve got to do this quickly.” Then you’re saying, “Oh my God.” Fortunately, we were given some time. My friends who’ve dealt with CLL, chronic lymphocytic leukemia, know that you often go many years — for me was 4 and a half — until you require treatment. Swollen lymph nodes, enlarged spleen, fatigue, high blood count, etc. Then there are other shoes that drop, and then you have to revise your plan a little.
Esther: I think during the time that you were in treatment, at least that first time in the clinical trial, I remember thinking, “What’s it going to look like on the other side in terms of planning?” The hope was you’d have a long remission, and we could sort of go back to whatever normal was. To a great extent, we did.

Planning for the future now
Esther: If we sort of step back from it, I think our journey together, a lot of it has been we’re going to just continue to make our plans and to live our life. Even now, 20-something years later and a second cancer diagnosis, we’re planning stuff that’s 6 months from now or a year from now. In my head, Andrew, it’s like we’re going to just go do this. If the plan has to change, the plan will change, but we’re not going to assume that we can’t do those things.
Andrew: You make some accommodation. I get some shots every 3 weeks now, I take oral medicine every day and I get an infusion once a month. I have to work around that or fudge those schedules a little. We like to travel, and now hopefully with less COVID, we’re starting to do that carefully.
We did something last night that we hadn’t done before, and that is we bought airline tickets. We paid more on the advice of our doctor [for] refundable tickets. We said to one of my doctors, “Hey, we want to take this trip.”
Esther: And it’s not until the beginning of next year.

Andrew: She said, “You probably can, but get refundable tickets.” So that’s in her hip pocket.
Esther: We’ve taken that approach with a lot of things. There have been milestone events that have come up in the family, where we just proceeded with planning a daughter’s wedding or planning to go visit relatives in another state.
It’s kind of like we’re planning to do it, and if we can’t do it, we’re going to just have to accommodate it. We have to have things to look forward to. That’s a big part of the planning that you and I do together. We need stuff to look forward to.
Being at important events
Andrew: Some people have heard this story before, but if you haven’t, I’ll repeat it. When I was diagnosed, our [oldest] son, Ari, was about 7. We explained that Dad had a sickness in his blood. He said, “Will you be at my bar mitzvah?” [It] seemed to him like it was way in the future.
Esther: That would be when he was 13, and he’s 7.
Andrew: Six years later. Right. I didn’t know, but I said I would. Now, fortunately, with treatment, I was in remission. Flash-forward to the parents, Esther and I, being in the front of the synagogue, in front of all of our friends and family, next to Ari, who’s the bar mitzvah boy. We give a little speech. My speech was recounting telling Ari that I plan to be at his bar mitzvah, but I didn’t know. Now, six years later, here I am. Everybody started crying.
Esther: The same thing happened at our daughter’s wedding, which was three months ago.
Andrew: It had been put off by COVID. Lots of planning. Would I make it? It was a great wedding, and I did. Now we continue to plan.
Saying yes and being spontaneous
Andrew: I believe in saying yes. Somebody is going to call and say, “Hey, can you go out to dinner tonight? I know it’s short notice. Can you go?” Sitting outside now, with COVID. I always want to say yes. Right, Esther?
Esther: Yeah, 9 times out of 10 (or 9 and a half times out of 10), we both say yes.
Andrew: Yeah, or I’ll say to Esther in the morning — we wake up, and I’ll say, “It’s a beautiful day. Let’s go for coffee.” It costs like 4 bucks a cup now, whatever.
Esther: Despite the fact that we have an espresso machine.
Andrew: Yeah, but I just say, “Yes, let’s go for it.”
Esther: [Some of] that go-for-it attitude, I had to learn from you. You said at the beginning of this that I’m a planner, and that meant that I was less spontaneous about things. I sort of needed to know when the next thing was going to happen, and if this happened and that didn’t happen. More of a real planner.
You’ve really taught me through all of this to be more spontaneous and live in the moment. I think in some ways, your cancer journey has impacted mine as a care partner, because I’ve learned — what have you said? That life is a terminal condition anyway?
Andrew: Right.

Esther: When people have asked me, “How do you stay positive married to somebody on a cancer journey?” I said, “Well, I have two choices. I can either crawl in a hole and be depressed and not live life, or I can just say, ‘You know what, I’m going to worry when I need to worry.'”
Andrew: Spontaneity, I would say, is a really big deal. Live your life that way to the extent you can. Now, look, we’ve been married 37 years. Conversely, some people live alone. But there’s a world out there. There are neighbors. Maybe you go to a church, maybe you go to a synagogue, maybe it’s the Elks Club you can join.
Whatever it is, there are people that you can interact with, and there are opportunities that come out of those relationships. Maybe it’s just reading the book you always want to read. Take time for yourself. I believe that is a wonderful strategy.


I really believe that the health care community — and health care is kind of a screwed-up industry, but there are good people in it. There are people really fighting for us to do better on our cancer journey. There are people trying to research cures, so be their partner. Every day, work with them. If they make recommendations on things you can do yourself to help yourself feel better, do that.
One other thing I would just mention. When I wake up in the morning, I sit on the edge of the bed for a minute, and I kind of take stock. Some people say, “Do you have 10 fingers and 10 toes?” But I say, “Does it ache anywhere? Do I have energy?” Because my energy is different from day to day. But when I get up, I say, “I’m going to make it the best day I can, however I feel. This is a day — I’m religious — that God has given me, and I’m going to make the best of it.”
Esther: I think our partners and caregivers need to do the same thing. If somebody that you love is the patient or the survivor, the care partner has to adopt as much of a positive, forward-looking outlook as they can, too. How you interact with the world and with people that you love is really important for their mental health and emotional health as well.

Using the time you’re given
Andrew: Recapping a couple of things. We all live with uncertainty. People have said this to you probably: “Well, you could get hit by a truck tomorrow.”
Esther: And that’s true.
Andrew: And that’s true. What does the medical team try to give you? Time, so you have to decide how you’re going to use that time. You’ve been given time, more than probably you would have had if you did not any treatment at all. The cancer just ran amok, if you will. How are you going to use that time? That’s what I think about.
Then I hope that there are better medicines that will come along to give me more time or even, knock on wood, a cure. Keep at it. Be spontaneous. Have those relationships. Look on the bright side, because there is brightness. There has been progress.
You are here today watching this, and you didn’t know you would be for sure. I hope this gives you a little inspiration. I know that’s the way Esther and I feel. We have other programs in this series for our Cancer Friends, which is you, on coping with the diagnosis, overcoming it, your relationships with others, and also the role of care partners.
Esther: We’re looking forward to having other individuals and couples join us.
Andrew: Right. Thank you so much for being with us. I’m Andrew Schorr.
Esther: I’m Esther Schorr.
Remember, knowledge can be the best medicine of all.
Andrew & Esther Schorr

Inspired by the Schorr family's story?
Share your story, too!