Living a Full Life | Cancer Friends
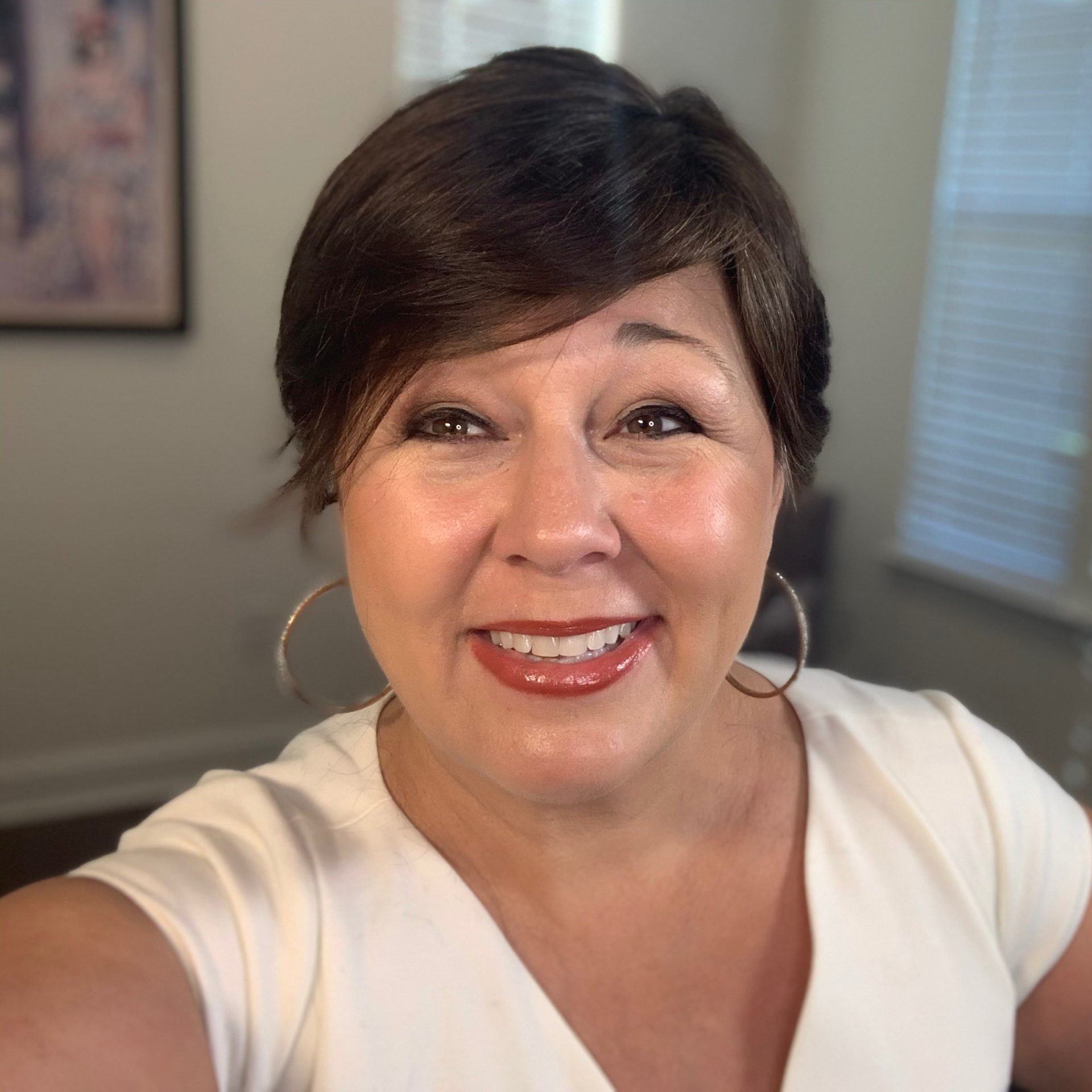
Featuring Susan Hartman
The Patient Story’s series “Cancer Friends” features Andrew and Esther Schorr. They co-founded PatientPower.info, a resource for other cancer patients and caregivers to help them through their diagnosis and treatment.
This segment focuses on Susan Hartman, a survivor of acute lymphoblastic leukemia (ALL). Susan details her first symptoms, dealing with isolation during diagnosis and treatment, and how she gives back to the community now.
- Introduction
- Symptoms and diagnosis
- Being in the ER and hospital during the COVID pandemic
- Coping with isolation while at the hospital
- Undergoing treatment
- How are you doing now?
- Writing as catharsis
- Incorporating activities back into life
- Not knowing if life would continue
- Giving back to the community
- Living a full life
- Advice for others with a recent diagnosis
- Conclusion
This interview has been edited for clarity. This is not medical advice. Please consult with your healthcare provider for treatment decisions.
Remember you are stronger than your situation. You are never alone. There are many people and many ways that people will help to lift up others.
Susan Hartman

Introduction
Andrew Schorr, The Patient Story: Hello and welcome to Cancer Friends.
Esther Schorr, The Patient Story: One of the ways that I communicate with cancer patients and with their families is through Facebook groups of patients and care partners. I was fortunate a couple of weeks ago to connect with our guest, Susan Hartman, who was actively participating in one of those groups.
Andrew, TPS: Susan is our newest cancer friend. Susan, welcome. Thank you for being with us.

Susan: Thanks so much. I appreciate you having me.
Andrew, TPS: You have been an ALL (acute lymphoblastic leukemia) patient. That’s a big deal. We’re going to learn about that in your journey, but let’s start before you were diagnosed with a blood cancer. What was life like for you in Cranston, Rhode Island?
Susan: Good. Very good. One of the things that I have always appreciated is that I’ve always felt very blessed that I had so many friends and family that were close by. [There are] a lot of things that my husband and I like to do together. [We’re] very active. We spend as much time outdoors with every season that we have. We’re in New England, so we have a nice changing weather pattern.
I had been moving into my own consultancy practice, and that was starting to get going. We were having a good time. We sail and bicycle. I swam.
In my mind, I always used to say to people that I felt like I had a charmed existence and I was very healthy. I took a vitamin. I might take an aspirin once in a while. That was it.
Symptoms and diagnosis
Andrew, TPS: What changed?
Susan: Back in 2020, coming into March, I was finding that I was having some difficulty doing [my] lap swimming. I was having trouble with really getting a good full breath, but it wasn’t slowing me down completely.
We also knew things were starting to get a little bit squirrelly. We were hearing a lot about COVID. We were listening to different broadcasts and we decided to take a real cautionary approach to everywhere we went and everything we did.
It didn’t matter, because what ended up taking place is that rolling into May, really the end of that April, I suddenly was at the point where I couldn’t get a good breath. I couldn’t manage to lie down to sleep, I couldn’t bicycle and breathe and I couldn’t make the bed.
My husband said, “You really have to get to the doctor.” Of course, I knew that he was right. It was all of a sudden. Over the course of maybe 4 weeks, it just accelerated. I thought, this is seriously wrong.
[I went] to the doctor. I figured maybe I’ve got [a] virus and I’ll get something that’ll get me over the hump. I should have probably known. When I went in, she had me go in to take scans in the same building and said, “Let’s take some scans. We’ll take a look.”

The radiologist came out, handed me a disk, and said, “I think you should hang on to this. You’re going to need it.” It never dawned on me that there should be a reason that she would do that. I just assumed it was a health care privacy thing. I took the disk, and I managed to get myself back into the car.
I’m sitting there, trying to catch my breath, when she called me. She said, “Are you in the building?” I said no. She said, “Can you come back in the building?” I said, “I really don’t think so.” She said, “You need to go to the hospital right now. You need to go to the emergency room. We’re calling ahead to let them know you’re coming.”
My husband was just down the street because and [he] picked me up. Thankfully, the hospital is very close to where we are. He dropped me off at the ER. It was a really strange time and things started rolling forward at that point.

Being in the ER and hospital during the COVID pandemic
Esther, TPS: Susan, all of that happened shockingly all at once. You acknowledged we were right at the lockdown stage of COVID. How did that impact what happened to you next and how it happened?
Susan: When he dropped me off, the exterior of the ER was tented. They would only allow me to go in. He couldn’t come with me. He drops me off. I go in. They check me. I then proceeded to sit in an emergency room cubicle for about 5 hours, waiting for something to happen.
The place was just bonkers. This is Rhode Island Hospital, which is one of the best hospitals in the region. It has an alliance with Brown University Medical School. For oncology, they have a very close alliance with Dana-Farber out of Boston.
I waited and waited until finally they could put me into a room, and they still didn’t know what this was. I was hearing from different people, asking me different questions and trying to understand what was wrong, what was happening, what had I done, and where had I been?
At that point, they decided to keep me overnight. I’ve never been in a hospital in my life. I didn’t have children. I married a man with two sons and that’s great. That’s instant family. Not having ever been in a hospital, even to have children, I didn’t have a clue what this was going to be about.
The first night, I remember waking up at about 1:00 in the morning because I couldn’t sleep. I just sat there, and I thought, “What’s happening? What does this mean? What do I do? I don’t understand how to deal with this, and I don’t know what’s going on.”
You always feel like the people that are supposed to be there in your life show up when you need them the most. The next day, there was a doctor who came in, this woman full of energy and very positive. She said to me, “You need to do your biopsy tomorrow, but this is what we think you have.” She alluded to ALL.
I’m thinking, “I have no idea what that is.” Of course, I’m online Googling this. I still was having trouble breathing, but I said, “Look, I have a biopsy scheduled tomorrow morning. I will be here, but I need to go home tonight. I need to go home and be in my house. I need to see my husband.”
She agreed to that and I came back the next morning. I don’t know whether that would have changed certain pieces of this or not. When I came back in that next morning, they did the biopsy. They did a procedure that removed the fluid in my right lung. At that point, I needed to wait until I had a full diagnosis and I was introduced to an oncologist.
Then I had to take a COVID test. Before they could admit anybody, everyone had to have a COVID test. The bizarre thing that happened is that my COVID test came back positive. I was more aggravated about that than anything else, because we had worked so hard to be so careful. I couldn’t understand how it was possible.

The hospital was in chaos because everybody was moved around. They had taken over floors of the hospital to care for all the COVID patients. Everybody’s walking around in full garb. They couldn’t come in and out of rooms without all of the gear that they had on.
In the meantime, they’re waiting to see if I present any symptoms. The odd thing is I never presented symptoms. That is a blessing. The oncology team was extremely concerned because they had [never] seen that together. I was only the second patient that had shown up that had the two things happening potentially at once.

I spent about 10 days floating around in those rooms until they finally felt that I was free and clear. I had to do a double test negative. They moved me into the oncology space, which strangely was still not the normal oncology floor, because they didn’t have room there. I ended up in the children’s oncology department.
Andrew, TPS: Because of COVID, nobody could visit you.
Susan: Nobody could visit me. This entire time that I’ve now been back in the hospital again, I’m by myself. Any conversations I have, it’s just me. My husband would be on the phone when we talked to the doctors. If they had anything serious they needed to discuss and any process, plan, or any outcomes, they would bring him in on the phone. The entire time I was there, I was by myself. That started, I think, May 4th, and I finally came out on May 27th.
Coping with isolation while at the hospital
Esther, TPS: During that time, Susan, how did you cope with that? Tell us how you managed that isolation and confusion about what was going on.
Susan: I’m sure anyone who might hear this and has gone through this knows what I mean when you say it’s totally surreal. You’re just not believing that this is all what you’re hearing or what you know. It’s kind of an odd thing that throws you off. It makes you feel very insecure [and] makes you feel shaky.
Several people have said to me, “It’s a good idea to journal things. Write things down because you won’t be able to keep track of things, and it’ll be a good way to know the details.” That’s a really important and [something] I started to do. I did a lot of journaling.
I also leaned on a lot of the things that I’ve done in the past through yoga practice, through meditation, through listening to music or sounds of nature. Whatever it is that soothes you, I would spend a lot of time with that. I found that that was how I was able to calm my mind, relax and get some sleep at night.
Your head is whirring around, and you’re having all kinds of crazy dreams. You’re awake in the middle of the night for various reasons. This was how I would manage all of that.
Then the other side of it was – I kept in touch with very select people, namely my family. I spoke to them. I had a regular pattern of when I would speak to them, so they knew they would hear from me. I knew that I would talk to them or FaceTime with them.
My husband would send things to the hospital for me. He became really good at baking these phenomenal pound cakes that were one of the few things that I could eat and that I loved. He would have pound cakes delivered, candy, or more clean pajamas and socks. You can’t have enough good socks, I have to say.
Because he was trying to deal with all of this himself, he started biking more actively. What I would do is tell him where I was in the hospital, which room I was in, and I’d say, “Okay, this tree, that park, whatever.” He would come.
At the appointed time, I knew he was down there. I’d have my tea, and he’d bring his coffee. We’d chat on the phone, and I could look at him. We had a regular schedule of visitation that way.

Undergoing treatment
Andrew, TPS: Susan, the good news is [you were] treated successfully with this acute blood cancer. You were in the hospital [for] how long?
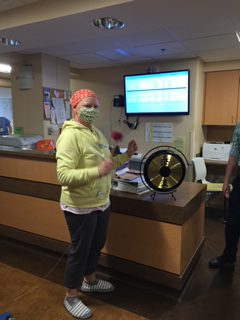
Susan: That first visit was probably 24 [or] 25 days. Then the cycle that I was on is called a hyper-CVAD treatment. Because of my age and the level of invasiveness that I had — which wasn’t extreme, it wasn’t full on into my marrow — they said, “Okay, these are the drugs that we’re going to work with. This is the methodology. This is the process.”

It meant I was home for two weeks, then I’d come in for a week, home for two weeks, and so forth for 8 cycles. From May until the end of November of 2020, I was in and out of the hospital for that whole duration.
Andrew, TPS: Just to be clear, at what age were you diagnosed?
Susan: I would be 58. Then I started the maintenance cycles after that, and I’m still finishing the maintenance.
How are you doing now?
Andrew, TPS: How are you today as far as ongoing treatment, and how do you feel?
Susan: It’s a world of difference this time this year than it was even last year. This is the second year of the maintenance. I’m scheduled to finish in December. I asked my doctor, “You can tell me the details later, but how do we close this out? Are we going to break up?” She said, “It’s going to be cold turkey. That’s it.” I had to laugh because I thought, “What a great expression.”
Then I finish taking the outpatient medicines and that’ll be done in December. I feel immensely better. I have highs and lows based on any of the extra things they might need to give me along the way. They’re part of this process, but I usually know when I’m having a low, I’m going to come back up again.
It’s cyclical. Just have the patience, have belief and trust in the process and just roll with it. Just keep going. You’re going to be okay. It’s going to be okay.
You just keep moving through that. That’s that whole fierceness I had. I’m like, “I’m going to just keep pushing and pushing and pushing.” I wasn’t going to stop pushing. We just kept on going. So far, the care they’ve given me is incredible. They’ve been an amazingly great team.
Writing as catharsis
Esther, TPS: You’re over that initial very intense treatment crisis. How are you living your best life now? What are the things that you’ve incorporated back into your life that give you pleasure?
Andrew, TPS: What’s the through line with that writing you started during COVID? Tell us how this has propelled you.
Susan: I’ve said this to several friends of mine who have been diagnosed with different cancers over the past two years.
I said, “Write this stuff down. If nothing else, it’ll help you to remember what’s going on, what’s being said, and who you saw. But the other thing is it’s a safe place. Get it out of your head, take it out of your body, and put it on that piece of paper. It’s there for safekeeping.”
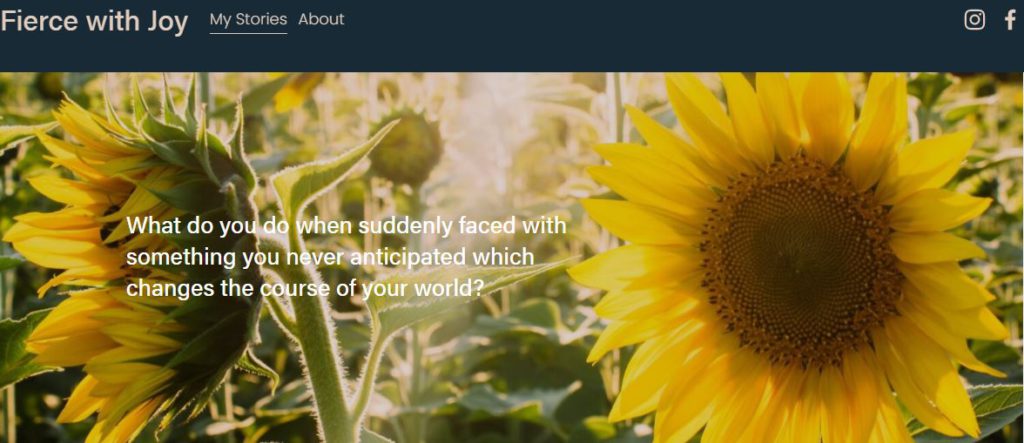
I started writing every day for the last three years. As a result, I started to put some of my writing into blogs and that was the site I started, called FierceWithJoy.com. I started writing my stories and experiences.

Incorporating activities back into life
Susan: Gardening is very big for me. In fact, I’m hoping to complete a Master Gardener program this winter, which would be really exciting, so I can help to do different gardening programs in the community afterwards. Playing in the dirt is great. I highly recommend it.
I did finally find a dog. I was very excited. We finally were able to find one. During COVID, pets were being scooped up, and we couldn’t have a pet at that time. When we found this little dog — or he found us, one or the other. That’s been a lot of fun.



Andrew, TPS: What’s his name?
Susan: His name’s Cormac. It’s a funny little Irish name, and he’s a funny little dog. He’s a mix of a bunch of things. When people look at him, they think he’s either a corgi, an Australian shepherd, or all of those smushed together. He’s quite the character. He’s very cute.
We’ve also gotten back on the boat. The boat didn’t go in the water in 2020, and we really didn’t get out to the boat much last year. But this summer, we’ve had better opportunities to go and do overnight or day sails, and we’ve brought the dog. That’s been really nice. It’s an amazing feeling to be out on the water, just feel the sun and the wind, and be a part of all of that again.


I’ve been doing a lot of water rowing. I have a water rower. I started building in some exercise elements because the treatments really decimate you physically. “I’ve got to get some strength back, if nothing else,” I thought. I’m building it up, and then eventually I’ll get back out on my bike.
Not knowing if life would continue
Andrew, TPS: How would you describe the fullness of your life now, given that when you were in the hospital, you didn’t know if you’d pass on?
Susan: Where that hit me the most was, when I really thought, “Is this it? Is this going to be it?” It’s amazing where your head goes. That’s why I was so grateful that this doctor came in, and she just was like, “Nope, this is what I think we’ve got. We have great success, and I’m going to connect you to this other woman oncologist.”
I’ve had all women caring for me. This has been spectacular and unusual.
I feel like I always appreciated my life. I never took it for granted. I never took any days for granted. But I feel like I have a different approach to how I want to spend my time and where. I have always been one to contribute to my community and donate time.
Giving back to the community
Esther, TPS: That’s what I was going to ask about, Susan. You’ve mentioned your master gardening and that you wanted to give back to the community. Can you talk a little bit about this idea of giving back and what that means for you?

Susan: We live in a historic community, actually. One of the houses that I grew up in is a 1700s house. We have a very old community and a lot of tradition and activities. I like giving to that community in terms of helping with whatever we’re working on in the town.
The other thing that I do is to support the gardening elements, which I really wanted to expand out. [I want to] help move into communities and areas where people are doing more with gardening, or they want to understand more about how they can do it and have access to it.



The incorporation of nature has a very soothing effect for a lot of people, and it makes a big difference. We’re not terribly connected to nature. I think this would be something I could help to bring into some areas, and they seem to be interested. The program itself seems to be looking for that.

Living a full life
Andrew, TPS: [How] you would describe this, Susan? A, do you feel like you’re living a second life? B, is it a full life?
Susan: I would say it’s a new life, and it’s a full life. [I’m ] working on it. I don’t have all the answers yet. I haven’t figured it all out yet. I’m sure there are other things I’m going to want to do and ways I’ll give back. I figured I needed to get through all of what I’ve done and be past that a little bit, and then determine how it fits or where my contribution is wanted and how I can help.
In doing this site that I built, one of the big elements of this is that I really wanted to help other people to get through this process and to assist them. Not in the counseling way, but connect the dots, get people to the resources they need, help them to understand they’re not alone, and offer support and encouragement.
It’s so important, and it’s so important to stay positive through all of this as best you can. There is another side that is a great side. You can feel that change once you get through it.
Advice for others with a recent diagnosis
Esther, TPS: You’ve given some advice already by just talking about your story to other people who have gone or are going to go through this, unfortunately, at some point. What would be your advice to them [about recapturing zest for life]?

Susan: Remember you are stronger than your situation. You are never alone. There are many people and many ways that people will help to lift up others. One of the things that was the most remarkable, enlightening thing I found — and this was even while I was in the hospital — is the humanity is just incredible.
You end up being handed the grace from other people for them to want to help you as a perfect stranger. That humanity is so incredible. You can’t deny that that’s a part of what this is about. I don’t know what the reason is that I got through all of this, but I knew I was going to get through all of this.
I really felt like being positive and moving forward and doing all of the things that you need to do. Trust the process and be your own advocate. Those were like the key things that just kept popping into my head. All of those things, I felt, were just really important. Partly because I thought it, and partly because people said that to me.
They would send me messages, and they would forward texts to me. I’d wake up every morning, and I’d have a bunch of texts from people. My West Coast people would be in touch with me later, and then my East Coast people would get me in the early part of the day.
It was like this continuum of connecting with people, which was really key. I don’t think it was because of the pandemic. I think it was largely because that’s the nature of what this is about. Very few people are not touched by this or haven’t had a family member touched by it in some way. We need to lift each other up. I think it’s important.
Conclusion
Andrew, TPS: I think you said it just now, but also what I read into it is you were touched by the human-to-human connection of other people, people who never met you before. What it sounds like you’re doing now with the gardening, with the writing, with the dedication to your community, is you’re in touch with that humanity within you and now paying it forward, if you will.

Andrew, TPS: I think that’s a beautiful, beautiful thing. Even after a very potentially fatal condition like ALL, an acute condition, with the right care hopefully, there is life afterwards. You can get back to giving. You get up in the morning. Sounds like with all the things you listed, you say, “It’s another day. Let’s go.”
Susan: Yeah, absolutely. Absolutely. I do. I always joke that I’m the busiest unemployed person I know.
Esther, TPS: There’s no such thing as retirement.
Susan: I have so many things I want to do.



Andrew, TPS: We’re so delighted that Esther connected with you cross-country, San Diego to Cranston, to bring this story to others. Susan Hartman, we wish you all the best as you continue your recovery. Thank you for being with us.
Susan: Thank you both. I really appreciate that. It was great to talk to you.
Andrew, TPS: This is what Esther and I do with our Cancer Friends series, and we’re delighted that we’ve connected with Susan Hartman. We look forward to more Cancer Friends stories. We always welcome suggestions. Thanks for [reading].
Esther, TPS: Remember, knowledge can be the best medicine of all.

Inspired by Susan's story?
Share your story, too!