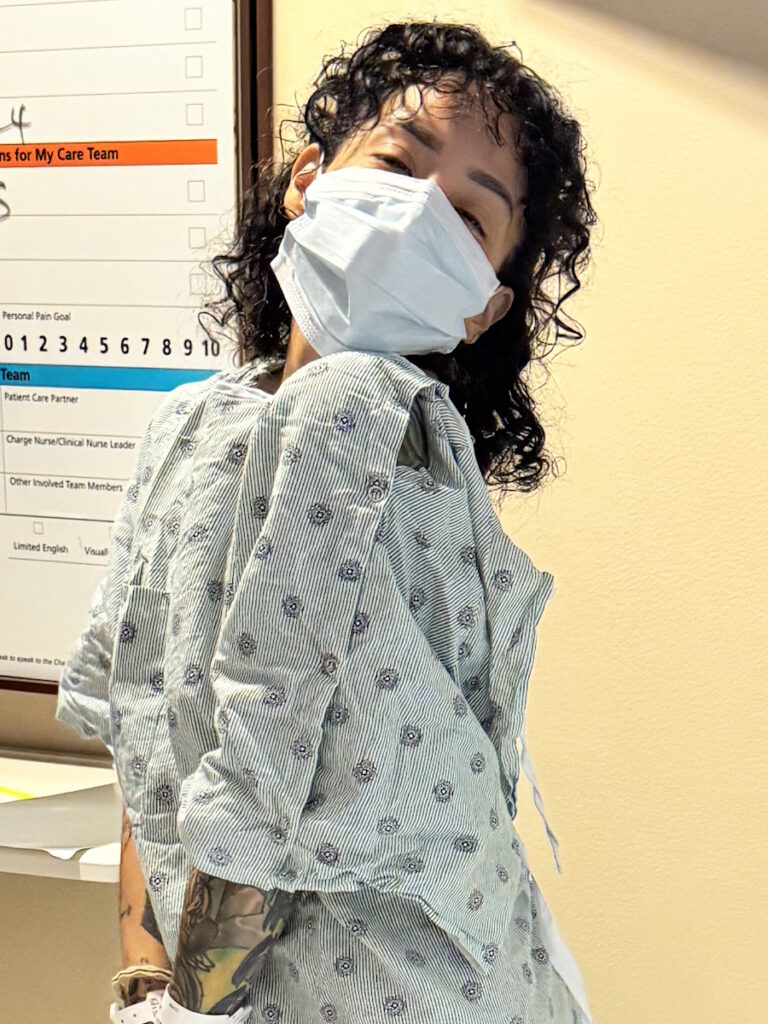
Alyssa’s Stage 4 Stomach Cancer Story
Alyssa was diagnosed with stage 4 stomach cancer after 2 ½ years of multiple doctor visits and normal test results. She initially experienced extreme fatigue and elevated resting heart rate. Subsequent symptoms like heartburn, weight loss, and difficulty swallowing prompted further medical consultations and tests, eventually leading to a GI specialist who performed an endoscopy and colonoscopy, where a biopsy revealed gastric cancer.
Interviewed by: Taylor Scheib
Edited by: Katrina Villareal
Upon diagnosis, Alyssa was shocked but sought a treatment plan. She was referred to a cancer specialist and a treatment center that acted promptly. She joined a support group, on which she relies heavily.

Her treatment involved chemotherapy and surgery, including a gastrectomy and oophorectomy. However, a laparoscopy revealed cancer spread to the peritoneum, changing the course of treatment to ongoing chemotherapy. She eventually joined a clinical trial that offered targeted chemo and surgery, but post-op results showed aggressive cancer with limited success from previous treatments.
Alyssa now waits for further scans and relies on a strong support system, faith, and therapy to cope. She emphasizes the importance of self-advocacy in healthcare, urging others to persist in seeking answers and appropriate care.
- Name: Alyssa B.
- Diagnosis:
- Stomach (Gastric) Cancer
- Staging:
- Stage 4
- Symptoms:
- Fatigue
- Elevated resting heart rate
- Heartburn
- Difficulty swallowing
- Weight loss
- Treatment:
- Chemotherapy
- Immunotherapy
- Surgeries: total gastrectomy; partial esophagus removal; bilateral oophorectomy and fallopian tube removal
- Clinical trial

This interview has been edited for clarity and length. This is not medical advice. Please consult with your healthcare provider to make informed treatment decisions.
The views and opinions expressed in this interview do not necessarily reflect those of The Patient Story.
It was not like me to have low energy, especially at my age and with my health history.
Introduction
I’m from Houston, Texas, and I was diagnosed with stage 4 stomach cancer in 2023.
Pre-diagnosis
Initial Symptoms
The first symptom I experienced was extreme fatigue. I was tired all the time. I didn’t have the energy to have a social life anymore. It was work, home, sleep, repeat, and that was not like me at all. I thought maybe there was something wrong. My family has a history of thyroid issues, so I wanted to have that checked out.


When I first saw my doctor, she agreed that it was not like me to have low energy, especially at my age and with my health history, so we ran some blood work to see if it was my thyroid or if we would uncover anything else.
Unfortunately, everything came back normal, so we didn’t get answers to what was causing the fatigue. She said maybe it was stress or I was exhausted from work. She wanted to do blood work every couple of months and keep checking in to see how my energy levels were.
A couple of months later, I started getting notifications on my smartwatch letting me know that my resting heart rate was over 100 bpm, which would happen when I was sitting down and relaxed. I thought it was a glitch, but after a few times of that happening, I thought it was something I needed to take back to the doctor to see what was going on. They did a quick EKG, which came back fine, but she didn’t want me to continue experiencing elevated resting heart rates, so she put me on a beta blocker. We redid the blood work and everything came back normal again.
A couple of months later, I experienced heartburn. I’ve never had heartburn, so I thought, “What is this burning sensation? Why is it so uncomfortable?” From the moment I got it, it happened every time I ate, no matter what I ate.
I went back to the same clinic but saw a different doctor because she had availability sooner. She told me, “It’s probably your age. You’re getting older, so maybe you can’t handle acidic foods anymore.” I told her I’ve never had it before and it’s happening constantly, regardless of what I eat. She said, “Let’s start this new medication and try to cut back on acidic foods.” I started the medication, but it didn’t do anything.
I was frustrated because I was taking more and more medications, but I wasn’t getting answers as to what was causing all of these symptoms.
I told her I wanted to figure out what was going on with my heart because I was taking medication, but we didn’t have answers. She said, “We can do a test, but it’s probably not going to come back with good results because you’ve been on the beta blocker for a couple of months.” I wanted to go ahead with the test to see and then we could go from there.
Sure enough, the results came back normal heart and she said, “It’s probably because it’s regulated by the beta blocker.” I was frustrated because I was taking more and more medications, but I wasn’t getting answers as to what was causing all of these symptoms. I’ve never had health issues before.
I told her I wanted to start over. I said, “I want to wean off of this medication. I don’t want to take this medication for heartburn anymore. Let’s do testing first, figure out what’s going on, and then we can go to medication if that’s what’s needed.”
Over the next couple of months, I slowly weaned off the pill that slowed down my heart rate because I didn’t want to have any adverse effects and within two months, I lost a lot of weight. I lost 15 lbs. I’m a very short person, so 15 lbs is a lot for my frame. Everyone noticed.


Then I started having difficulty swallowing. I would eat something and it felt like the food would get stuck halfway and I couldn’t breathe. When I would try to drink something, it would feel like I was drowning. I thought it was a one-off situation, but when it happened again, I said I wasn’t going to wait for a third time.
I booked the first appointment available. Again, my primary care doctor wasn’t available, but the other doctor at the clinic was and she told me, “We know that everything’s been normal. I don’t see any issues.” I told her I wanted to redo my blood work, but she was hesitant.
She started going through my chart, saw my weight loss, and said, “Oh, wow, you did lose a lot of weight in a short period. I don’t like what you’re saying about the difficulty swallowing, so let’s get you to a specialist.” I redid my blood work that day.
I was already two and a half years into this, spending all this money, but still had no answers.
Meeting with a GI Specialist
Two months later, I met with a GI doctor and she was concerned with the symptoms I was experiencing. She said, “I want to redo blood work. I also want to do a stool sample, an endoscopy, a CT scan, and possibly a colonoscopy.” I did all of that and the blood work came out great. The CT scan looked great as well. The only things left were the endoscopy and colonoscopy and they were going to be done on the same day.
By that point, four months had already passed doing these tests. I was already two and a half years into this, spending all this money, but still had no answers. Is it even worth it to do these last tests? If I get no answers, I’m still stuck in the same place. My spouse told me to stick with it. We needed to see if this could give us the answers that we’ve been looking for.


Biopsy
When I woke up from the procedure, the person who performed it told me, “We found one polyp in your colon. We removed it and it doesn’t look concerning, but you had a lot of inflammation in an area that we don’t typically see. It’s where your esophagus meets your stomach and the inflammation is pretty bad. I’m going to take a biopsy and send it off.” I asked, “Is that why I’ve been having difficulty swallowing?” He said it’s definitely why. I asked, “Will that also explain why I lost so much weight within a short period?” He said it could be.
Then he took a deep breath and said, “Does cancer run in your family?” I wondered where this was coming from. I had just woken up from the procedures, so I was trying to think and remembered two distant relatives but nothing stomach-related. He said, “Okay. Well, like I said, we’re going to send it off. I’ll call you back with the results in a couple of days.”
I had a million questions, but I didn’t even know where to begin.
Diagnosis
Getting the Official Diagnosis of Stage 4 Stomach Cancer
He called me back five days later and said, “Hey, it’s me. I performed your procedure,” so I called my spouse to hurry and come over. He was beside me right in time to hear that I had gastric cancer.
Reaction to the Diagnosis
We were both in complete shock. We didn’t react and were just staring at each other. It was like we weren’t in that conversation anymore.


I didn’t hear anything else said. I finally came back to what was going on when the person on the phone asked, “Do you have any questions?” I had a million questions, but I didn’t even know where to begin. The only thing I could think to ask was, “What’s next? Where do we go from here?”
He said, “Pretty hopeful that we caught this early. I know you’re scared, but you’re young and healthy. We’re going to take care of this and you’ll be okay. We’re going to do another scan higher up because we weren’t expecting to see that inflammation so high up. From there, we will get you with the oncology team and they will go from there.”
In addition, he told me that I had the bacteria H. pylori, which caused my gastric cancer. It looks like I got it when I was a child and because I never had symptoms, it went untreated and turned into gastric cancer. He said, “We need to clear that up first. You need to do the scan and then you can start treatment.”
After that, it was a little frustrating because I had another scan and the doctor said the scan looked good. He was going to call in my prescription and I said, “When do I talk with the oncology team?” He said they should be calling me but gave me the number. After that weekend, I went ahead and called them.
I found Stomach Cancer Sisters and it was specifically for women who have had or have stomach cancer. I joined and was immediately welcomed.
Referred to an Oncologist
They told me that they weren’t taking new oncology patients and I could be referred out, which turned out to be a blessing in disguise because the cancer specialist and the treatment center I was referred to was a complete 180. They moved with a sense of urgency. They said, “We book your appointments. We don’t call to confirm if it’s okay with you. If it’s not okay, call us back and let us know.”
Immediately, they made me an appointment with an oncologist and a surgical oncologist. They scheduled my blood work and scans. They were going to redo everything, which I knew was going to happen because it was a new provider.

Finding Online Support Groups
Before I got to those first appointments, I was searching for support. I knew I had cancer, but I didn’t know how to feel and I didn’t want to get lost in the emotions. I wanted to try to connect, especially since one of my friends told me her mom benefited from support groups.
I found some support groups, but I wasn’t getting what I needed. There were so many members and so many people talking about so many different types of cancers that it felt so overwhelming.
I found Stomach Cancer Sisters and it was specifically for women who have had or have stomach cancer. I joined and was immediately welcomed. I was asked about what type of stomach cancer I had and I had no idea. Someone asked if I could share my reports with her and so I did, and she told me we had the same type of cancer. She told me what was going to happen, including having to remove the entire stomach. Nobody’s told me this, but that empowered me so much that I felt ready to go to my appointments.
‘I have to do a laparoscopy. The type of cancer that you have doesn’t show up well on scans.’
Treatment
Meeting with the Surgical Oncologist
I met with my surgical oncologist first and he went through the plan. “We are going to do scans and blood work. We’re going to do another endoscopy. During the first one, they were looking around but now that we know you have cancer, we’re going to do it with an ultrasound as well.”
“We need to go ahead and implant your chemo port because you’re going to need to start chemo as soon as possible. We’ll have to do four rounds of chemo, then surgery to remove your entire stomach, and then four more rounds of chemo.”
“Before we can start that, I have to do a laparoscopy. The type of cancer that you have doesn’t show up well on scans, so we have to cut little holes in you, go in with cameras, look around, and look for signs of spread. We don’t want to see it spread to the peritoneum, which is very common. There’s no cure for it. At that point, you would be stage 4 and surgery would not be an option.”
There was a lot of information and a lot of steps, but I felt calm and confident because we had a plan in place.


Laparoscopy Results
I got a call from my surgical oncologist and he said, “Unfortunately, during the laparoscopy, I took some biopsies and they came back as cancerous. It has spread to your peritoneum. It’s stage 4 stomach cancer and, at this point, surgery is off the table.” That rocked my world because I knew that removing the stomach was the only cure for this type of cancer.
He said, “We’re going to pivot you back to your oncologist and you will work with her. You will do chemo and that’s it.” I asked him how I could get surgery back on the table. He said, “It’s not common for us to do that with stage 4 patients, but, in four months, we will check in with you. We could do a procedure called HIPEC (hyperthermic intraperitoneal chemotherapy) where we apply chemo directly to your stomach. But at that point, I want you to do four more months of chemo, so it depends on your progress. We will check in.”
I had two scans where one scan picked up a cyst on one of my ovaries.
Chemotherapy
My oncologist confirmed that I will have to do chemo essentially for the rest of my life to prolong my life. I said, “I understand that is your goal. However, my goal is to get surgery back on the table and I want you to know that’s important to me. I’m willing to do whatever you need me to do to get to that point. If there are any trials available, I would love to do that. I need to know how.”
At that point, there weren’t any trials available. I started chemo and did four months. During that time, I had two scans where one scan picked up a cyst on one of my ovaries. There weren’t any big notes on it, so we didn’t talk about it.


Joining a Clinical Trial
In October, my oncologist told me that there was a new trial available specific to the type of cancer I had (stage 4 stomach cancer) and the spread I had. She said, “With this, you would receive chemo directly to your peritoneum and have surgery to remove your stomach. They’re hoping to find a cure for the spread that you have.” It’s exactly what I wanted and needed so I asked her to sign me up. She said, “Okay. We have to do another scan to make sure there are no signs of spreading anywhere else because that would disqualify you.”
The scan showed that the cyst on my ovary got larger and she said, “Now we’re concerned. We need to make sure that that’s not cancerous. We need to do an ultrasound.” We did the ultrasound and after that, I met with my surgical oncologist.
During that appointment, he told me that the ultrasound came back as non-definitive, so they weren’t able to tell if it was cancerous or not, but I was okay to go forward with the trial.
I had a procedure to place the port in my abdomen and a few weeks after, I began the chemo to my peritoneum. I received three rounds of chemo. Everything was good. Then we started preparing for surgery.
They removed my stomach and attached my intestines to my esophagus.
Gastrectomy & Oophorectomy
I had a break and during that break, we did more blood work. We did the pre-ops. We did one final CT scan six days before the procedure. But also during that time, I had to meet with another surgeon who was supposed to remove my ovaries.
She told me, “Do you know that this is going to put you into menopause? Do you know that you will not be able to have kids anymore? You’re very young to be going through menopause.” I told her, “I completely understand. This is not a decision that we are making lightly. We know how big this is going to impact us and we want to continue having children, so it’s not an easy decision.”
She was upset with my decision. She wasn’t in agreement. We knew my type of cancer has a tendency to spread to the ovaries and they’re not able to tell us for sure if it’s cancerous or not. My surgical oncologist also feels like this is the best plan. He looked at my ovaries when he did the laparoscopy and said they didn’t look completely normal.


The day before surgery, I met with her again and she told me, “What are we doing?” I said, “We’re removing the ovaries.” I went in to have my surgery, which was a 7- to 8-hour procedure. They removed my stomach and attached my intestines to my esophagus. They also removed my ovaries.
I was supposed to be in the hospital for a week, but I was very determined to not have any complications. I knew the surgery had a tendency to have complications and it’s not 100% in my control, but I wanted to do everything that they wanted me to do to help with that.
They wanted me to walk around, so I walked around. They wanted to make sure that I was sitting up most of the day, so I sat up and hardly laid down. I ate the protein that they asked me to eat. I did everything that they asked me to do. Because of that and the way everything was looking, I was able to leave the hospital in four days versus a week.
‘The cancer is being very aggressive… we’re looking at distant spread. We didn’t get the results that we wanted.’
Post-Op Follow-up
I had a follow-up one week later with my surgical oncologist. He went over the pathology and that was a shocker for us because we had hopes that the trial was going to get me to no evidence of disease. Unfortunately, he wasn’t able to get clear margins. The cancer had gone further up my esophagus than it had before. He went as high as he could, that was safe to do so, but it was very high.
He also shared that the tumor had taken up half of my stomach and it wasn’t like that before. He removed 53 lymph nodes and 27 came back as cancerous. He said, “What this means is that the cancer is being very aggressive. It also signals distant metastasis, so we’re looking at distant spread. We didn’t get the results that we wanted to get. Even with the chemo that you did before the trial, it looks like you had a zero response to it.”


I was shocked. I didn’t know what to think and how to feel. He told me, “We still have you on the schedule to have three more rounds of chemo to your peritoneum, but I’m concerned with the results of the pathology. I don’t know if we can wait until you finish that to put you back on systemic chemo or if we need to jump right into systemic chemo to address anything in your body versus focusing on the peritoneum.”
We brought back in my oncologist and she shared that it’d be best to go ahead and finish the trial. After that, maybe we should move to observation.
That brings me to the present. I’m waiting it out. I have another scan to review what’s going on and if there’s anything else concerning anywhere.
My faith is very important to me. When I’m struggling, I put on my worship music, pray, and ask for guidance.
Having a Support System
I have a great support system. I have great family and friends who check in on me and make sure that I’m okay. I rely heavily on the support group. I bounce ideas off of them. They told me about the Signatera™ test that I wouldn’t have known about if it hadn’t been for that group.
My faith is very important to me. When I’m struggling, I put on my worship music, pray, and ask for guidance because some days are harder than others.
I also undergo therapy. Therapy is so important. I always felt like I was dealing with most of this relatively well, but I didn’t want to have too much confidence in myself, so I wanted to have someone I could talk to to make sure that I was dealing with everything okay.
For the most part, I feel okay, but there are times when things rock me and I want to make sure that I’m coping healthily. I don’t want to brush it off and think I’m being strong when I’m hurting myself more.


Importance of Self-Advocacy
Focus on your why. Why do you want answers? Why is it important? For me, it’s my family. I want to be here for my family. I have a son and want to be there for him and see him grow up. I want to be the cool, tatted grandma and witness my child grow up and be a husband and a father. I want to see all his big life moments and be there to support him. I want to spend the rest of my life with my spouse. We have so much more time and so many more memories to make.
Advocating for yourself is the most important thing when it comes to your health.
Feeling Different
My body is so exhausted. It’s not the body that I used to have. I always joke with my spouse and say I’m an old woman now because I get fatigued so easily. After doing one task, I feel like I did a whole day’s worth of running errands.
I have a lot of things that are going against my energy. Without a stomach, I’m not able to absorb B12, so I have to do B12 injections once a month, but those wear off. I’m not getting the maximum absorption of iron, so I’m anemic and struggling to absorb iron. That’s also making me exhausted. With my ovaries gone, I’m going through menopause and my hormones are going crazy.
Because of the after-effects of chemotherapy and immunotherapy, my body is tired and I can feel that. It’s a bit frustrating because I’m a very independent person and I like to take care of things.


Words of Advice
Self-advocacy is so vital. You have to make sure that you’re advocating for yourself at each appointment. You know your body. Unfortunately, doctors get a lot of patients and they’re very busy. It’s not all on them. Sometimes, we have to reiterate, “This symptom is concerning because of this. This is what I need from you.” We forget that we have that power.
We go into the doctor’s office wanting them to give us answers, but they don’t have all the information and that’s not their fault. Sometimes, we don’t have all the information but make sure that we are pushing for more.
If they can’t do something for you, then get a second opinion or ask them to put you in touch with someone who can do that for you. Advocating for yourself is the most important thing when it comes to your health to make sure that you are getting the right treatment that’s specific to you and your needs.

Inspired by Alyssa's story?
Share your story, too!
More Stomach Cancer Stories
Andy G., Stomach Cancer, Stage 4 (Metastatic)
Symptoms: Stomach pain, back pain, chest pain, extreme exhaustion, shortness of breath after short walks
Treatments: Chemotherapy, immunotherapy
...
Alyssa B., Stomach Cancer, Stage 4 (Metastatic)
Symptoms: Fatigue, elevated resting heart rate, heartburn, difficulty swallowing, weight loss
Treatments: Chemotherapy, immunotherapy, surgeries (total gastrectomy; partial esophagus removal; bilateral oophorectomy and fallopian tube removal), clinical trial
...
Brittany D., Stomach Cancer, Stage T1b
Symptoms: Choking suddenly while eating and attempting to speak, neck and right shoulder pain, neck tightness, trouble swallowing certain food items
Treatments: Surgeries (subtotal gastrectomy, D1 lymphadenectomy, gastric bypass)
...
Camilla C., Stomach Cancer, Stage 4 (Metastatic)
Symptoms: Issues swallowing, swollen gland in the neck
Treatments: Palliative chemotherapy was offered but declined, nutritional changes to support her comfort and energy, meditation and mindfulness practices, self-directed healing methods
...
Emily D., Stomach Cancer (Gastric Adenocarcinoma), Stage 4 (Metastatic)
Symptoms: Persistent postpartum stomachache, early satiety, difficulty swallowing, vomiting
Treatments: Chemotherapy, immunotherapy
...
Alyssa B., Stomach Cancer, Stage 4 (Metastatic) (Hospice Update)
Symptoms: Fatigue, elevated resting heart rate, heartburn, difficulty swallowing, weight loss
Treatments: Chemotherapy, immunotherapy, surgeries (total gastrectomy; partial esophagus removal; bilateral oophorectomy and fallopian tube removal), clinical trial
...





2 replies on “Alyssa’s Stage 4 Stomach Cancer Story”
Alyssa, I’m an ovarian and luekemia survivor. Will be on meds forever for the luekemia.
God bless you sweetheart. I wanted to reach through the television and hug you. Please remember that God is in control and I’ve heard of so many miracles. He is the great physician. I am going to be praying for you beautiful girl. I pray that God takes the gut wrenching fear from you. I had a pretty bad prognosis in 2002. I had two sons, and was scared to death. Since then, so many new treatments gave come out. Sone in just the past years. There is always hope! No one can take that away.
Alyssa you are a true inspiration. I am going through some similar symptoms and am getting a second opinion. Thank you for all your advise. And may God bless you!