Brandie’s Stage 4 Leiomyosarcoma Story
Interviewed by: Alexis Moberger
Edited by: Katrina Villareal

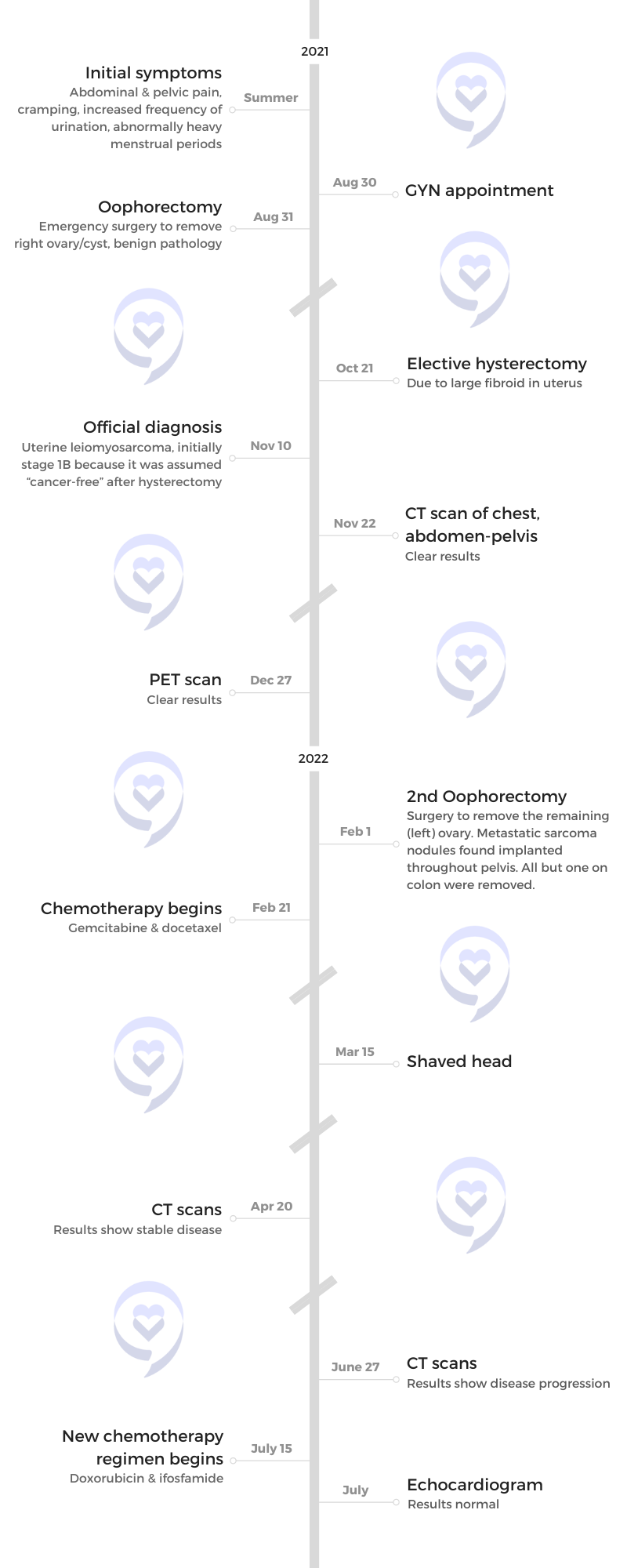
Brandie shares her journey with stage 4 leiomyosarcoma. She had a history of painful menstrual periods and a family history of fibroids and endometriosis, but in the summer of 2021, Brandie experienced worsening symptoms, including severe urinary urgency. Assuming it was related to fibroids, she underwent ovary removal surgery and an elective hysterectomy.
Unexpectedly, the pathology report revealed leiomyosarcoma, a rare cancer of the smooth muscle. Further surgeries were performed to remove metastatic implants. She also underwent chemotherapy regimens, which proved ineffective.
Seeking a second opinion at MD Anderson, she was recommended radiation. Despite its damaging effects on her bladder and colon, Brandie remained hopeful. However, the tumor continued to grow, leading to a failed surgery attempt. Desperate for options, she sought opinions from other specialists and found a sarcoma surgeon at City of Hope.
In April 2023, Brandie underwent a 14-hour surgery. The tumor was successfully removed, but her medical oncologist warned about the risk of microscopic cells in her bloodstream. A follow-up scan in September revealed a lung nodule, leading to a pulmonary wedge resection in October.
Throughout her leiomyosarcoma treatment, Brandie faced significant side effects, including neuropathy, muscle loss, and urinary incontinence. She maintained a positive outlook and her most recent scans in January 2024 showed no evidence of disease.
Despite the challenges, Brandie emphasizes the importance of seeing a specialist, getting multiple opinions, and continuing support for cancer survivors. She also shares her experience with having an ostomy, expressing gratitude for the improved quality of life it brought. Brandie encourages others to openly discuss their cancer journey and seek help when needed.
In addition to Brandie’s narrative, The Patient Story offers a diverse collection of sarcoma stories. These empowering stories provide real-life experiences, valuable insights, and perspectives on symptoms, diagnosis, and treatment options for cancer.
- Name: Brandie B.
- Diagnosis:
- Leiomyosarcoma
- Staging:
- 4
- Initial Symptoms:
- Abdominal & pelvic pain
- Cramping
- Increased frequency of urination
- Abnormally heavy menstrual periods
- Treatment:
- Chemotherapy: gemcitabine, docetaxel, doxorubicin, ifosfamide
- Radiation
- Surgeries: oophorectomy, elective hysterectomy, pulmonary wedge resection

This interview has been edited for clarity and length. This is not medical advice. Please consult with your healthcare provider to make informed treatment decisions.
The views and opinions expressed in this interview do not necessarily reflect those of The Patient Story.
- Introduction
- Pre-diagnosis
- Diagnosis
- Treatment for Stage 4 Leiomyosarcoma
- Chemotherapy (Gemcitabine & Docetaxel)
- Chemotherapy (Doxorubicin & Ifosfamide)
- Tumor Not Responding to Chemo
- Getting a Second Opinion
- Radiation
- Tumor Grew
- Follow-up Appointment with Oncologist
- Getting Additional Opinions
- Surgery to Remove the Tumor
- Recovering from Surgery
- Status Post-Surgery
- Post-Surgery Scan
- Pulmonary Wedge Resection
- Side Effects of Treatment
- Follow-up Scans
- Sharing My Cancer Story
- Having a Colostomy Bag
- Words of Advice
I have a bit of a medical background so I’m running the different possible scenarios through my head. It never crossed my mind that it could be cancer.
Introduction
I live in Northern California. I’m a registered nurse and work as an educator for a medical device company.
I love to travel. Before my diagnosis, I was into fitness. I did CrossFit and was a Peloton enthusiast.
I have a 6-year-old big, fat orange tabby cat named Toby and a wonderful boyfriend named Brad, who is a high school math teacher.
Pre-diagnosis
Initial Symptoms
I’ve always had painful menstrual periods since I was a teenager and a family history of fibroids and endometriosis. I always suspected that there was something unusual going on.
Doctors weren’t concerned over the years. There wasn’t ever any evidence of anything wrong. They told me, “You probably do have endometriosis, but we have to do surgery to confirm that so we’re just going to assume you do. If it gets to the point where you need to have surgery, then we can confirm it that way.”


Symptoms Worsen
Fast forward to the summer of 2021, I started having heavier, more painful menstrual periods, which was unusual. I also had a sensation of fullness or bloating in my pelvis. What spurred me to see a doctor emergently was having severe urinary urgency.
I have a bit of a medical background so I’m running the different possible scenarios through my head. It never crossed my mind that it could be cancer. I assumed I had a fibroid. I’d been told years ago that I had a teeny tiny one so I assumed that it was related to that.
Oophorectomy (Ovary Removal Surgery)
I ended up getting rushed into surgery. At this point, cancer’s still not on my radar. I had a large cyst on my ovary, which was funny that it didn’t raise alarm bells for me. It didn’t even occur to me that it could be malignant. They ended up having to remove my ovary because the cyst was solid.
Everything came back benign. But the doctor said, “What do you want to do about this large fibroid in your uterus?” I had turned 38 at the time and wasn’t interested in having children so I told the doctor, “Let’s do a hysterectomy. I know fibroids can come back. I want to do a one-and-done.”
The surgeon gets on the call and tells me, ‘I’m sorry, but your pathology report came back and it was not a fibroid. It was a sarcoma.’
Elective Hysterectomy
I had an elective hysterectomy and a couple of weeks later, I got a phone call from the clinic and they said, “Do you have time this afternoon for a video visit with your surgeon?” I knew something was up.
Diagnosis
Getting the Diagnosis of Stage 4 Leiomyosarcoma
The surgeon gets on the call and tells me, “I’m sorry, but your pathology report came back and it was not a fibroid. It was a sarcoma.” He kept saying, “Wow,” and added, “I haven’t seen this in decades.” He told me that he would be referring me to an oncologist and that’s where it all began.
We were hopeful that this sarcoma was confined to my uterus and since my uterus was gone, maybe this was it. Maybe this was my whole cancer story.


Secondary Oophorectomy
A couple of months later, the oncologist decided that she wanted to remove my remaining ovary because the tumor had estrogen receptors. When she went in, she found metastatic implants throughout my pelvis, which were confirmed to be sarcoma.
There were about six tiny nodules throughout my pelvis. They were attached to my peritoneum, bowel, and diaphragm, and they removed them all.
There was one small piece on my colon that they left behind. The surgeon, who was a gynecologic oncologist, told me that she was concerned about damaging my colon so she didn’t want to mess with it.
When I woke up from surgery, the fellow talked to me and said, “I’m so sorry.” I was still hazy coming out of anesthesia. She put her hand on my arm and said, “I’m so sorry, nobody deserves this.” I said, “What are you talking about?” I still was not fully with what was going on and she said, “We found more cancer in your pelvis so we’re going to have you start chemo in three weeks.”
At that point, I thought, “All right, we got this. I’m going to do chemo and it’s going to be what it is.” It turns out, I have leiomyosarcoma, a cancer of the smooth muscle, and it’s pretty much resistant to treatment.
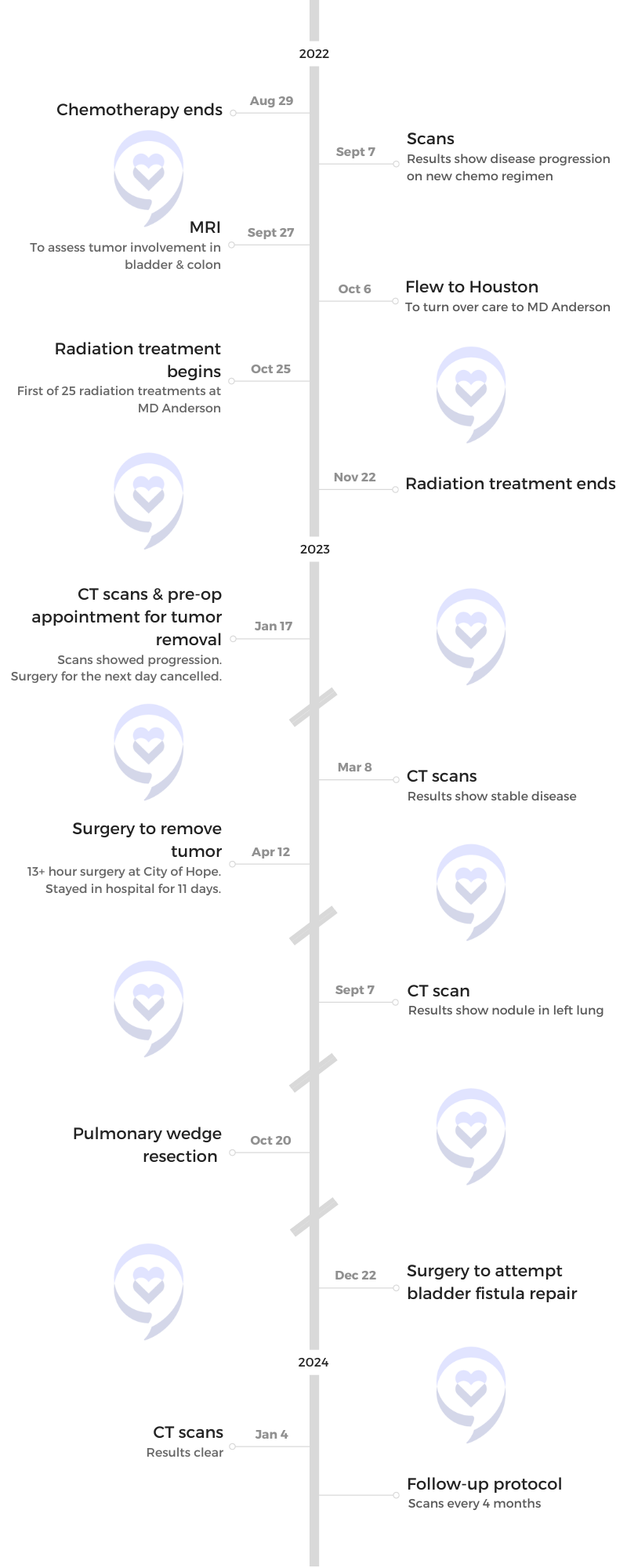
I did 12 infusions, but the tumor doubled in size.
Treatment for Stage 4 Leiomyosarcoma
Chemotherapy (Gemcitabine & Docetaxel)
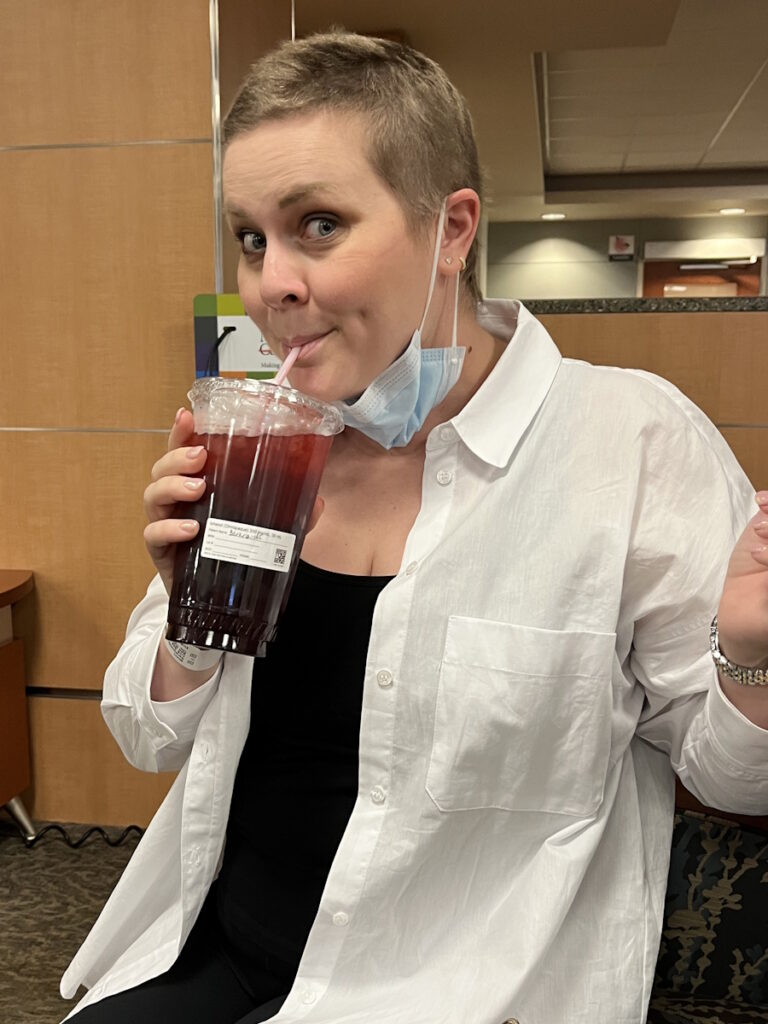
I did about six rounds of gemcitabine and docetaxel for four months, which I had an allergic reaction to. I did 12 infusions, but the tumor doubled in size so it did nothing.
Chemotherapy (Doxorubicin & Ifosfamide)
They decided to start me on a more aggressive chemotherapy that required me to be hospitalized for five days every three weeks. I started doxorubicin, or what they call the Red Devil, and ifosfamide, which can cause damage to your bladder, which is part of the reason why I had to be hospitalized and monitored closely while undergoing chemotherapy.
I did three rounds of that in about nine weeks and stayed 15 days or so in the hospital for those chemo infusions. They sent me for a scan and it doubled in size again so the tumor was not having it.

Tumor Not Responding to Chemo
They started weighing the different options. “It’s starting to invade your bladder and your sigmoid colon. We need to see if we can go in and remove this. If this looks like a surgery that’s not going to cause a ton of damage to your insides, we want to get it done and get you back on another chemo.”
The MRI showed that there’s too much invasion into my internal organs that if they do a surgery, it’s not going to be straightforward. It’s going to be a long recovery. It’s going to delay getting on to another systemic therapy so they decided that they didn’t want to operate.
I was pretty freaked out. Two chemo regimens had already failed me and they wanted to put me on a third. I’m thinking, What are the chances of that doing anything at this point?
Sometimes I wonder if things would have played out differently if I had been with a sarcoma specialist from the beginning.
Getting a Second Opinion
I got on a plane and went to MD Anderson to see a team of specialists who only treated sarcoma. I guess that was my first mistake as the doctor I had been seeing was not a sarcoma specialist. Sometimes I wonder if things would have played out differently if I had been with a sarcoma specialist from the beginning.
The team at MD Anderson said, “We’re going to get some more scans. We’re going to bring this to the tumor board then we’re going to call you and let you know what we think we should do next.”
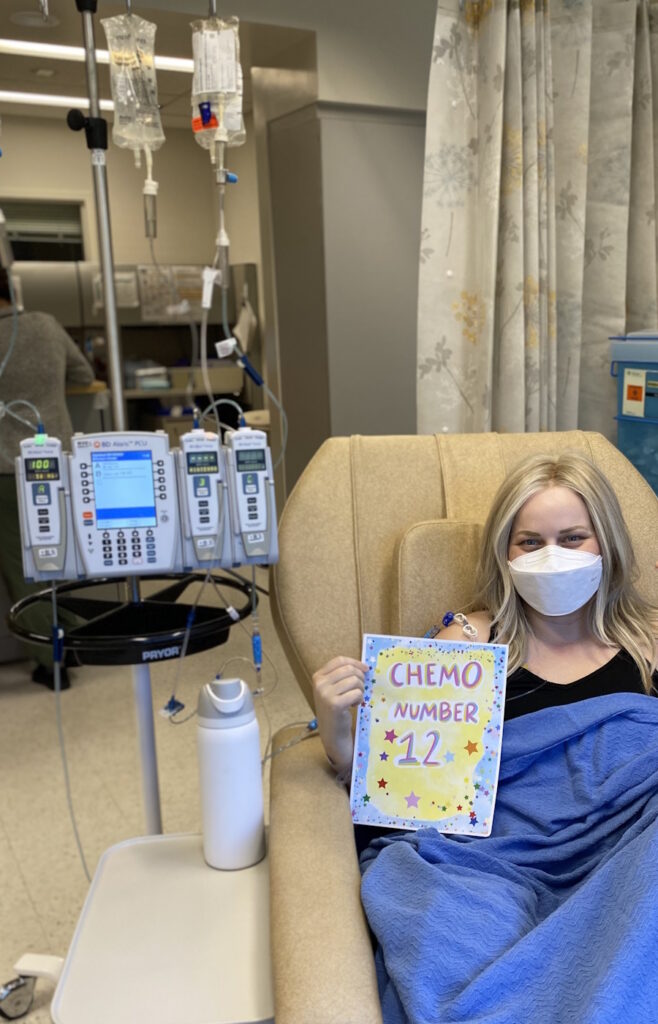
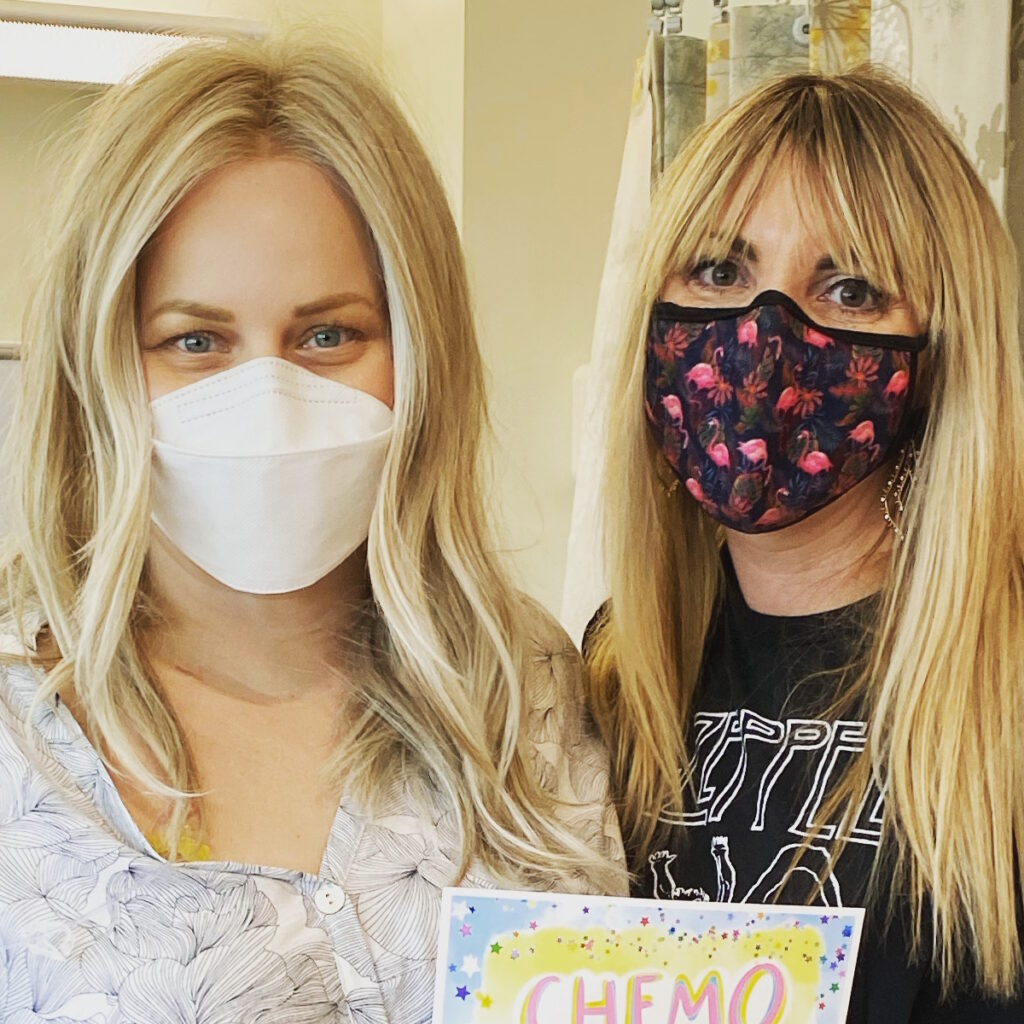
A few days later, they called me and said they thought radiation was the best way to go. I temporarily relocated to Houston for about six weeks. Luckily, I have an amazing friend who let me stay with her and her husband. It was nice and comfortable. I had my own room. It was a good experience despite the reason why I was there.

Radiation
I went through 25 fractions of radiation. I went every single day. It was the first time that anybody had given me any hope. She told me, “I’ve seen your type of tumor respond to radiation before.” She explained how they dosed it in a way that it was going to cover a margin around the tumor that would reduce the risk of it recurring by 50%. I was on cloud nine, thinking I finally figured out something that was going to work.
But even as a nurse, I didn’t realize how devastating radiation can be to your body. I tolerated it pretty well while I was going through it, but it damaged my bladder severely and my colon. I start having bowel issues and urinary incontinence. I thought, This is a means to an end.
I finished radiation the day before Thanksgiving 2022. I packed all my things, went back home, and spent the holidays with my family. That was the order from my doctors. “Go home, spend the holidays with your family, rest, recover from radiation, and we’re going to see you back at the beginning of January for your surgery. We’re going to remove this tumor.”
I thought, If these surgeons at this top hospital are not comfortable operating on me, then I’m a goner. This is it.
Tumor Grew
They scheduled me for surgery. I went out a few days early and my mom flew out with me. They did scans and a bunch of tests. I showed up on the morning of my pre-op, the day before the surgery was supposed to take place, and the surgeon told me, “I’m sorry. It looks like your tumor has grown and I can’t operate on you.”
That was probably the lowest point for me right there. I felt pretty hopeless. I went through all of this to get this thing out of me. It was 12 cm. It was huge and uncomfortable. It was crushing my bladder. I was having bowel issues. I was getting obstructed and I was miserable. I thought, If these surgeons at this top hospital are not comfortable operating on me, then I’m a goner. This is it.

Follow-up Appointment with Oncologist
They decided that they were going to have me follow up with my medical oncologist before I flew back home to California. I moped around for a couple of days then I got in to see him.
He said, “You know what? It might still be inflamed from the radiation. It’s negligibly larger. I’m going to run this by the tumor board, but we’re going to send you home for six more weeks. We’re going to scan you again and then make a decision. If it is larger, we’re going to consider systemic therapy again. But if it’s not, then we’ll talk about what we can do.”
I had this sense of relief. I’m going to go back to living my life for six more weeks.
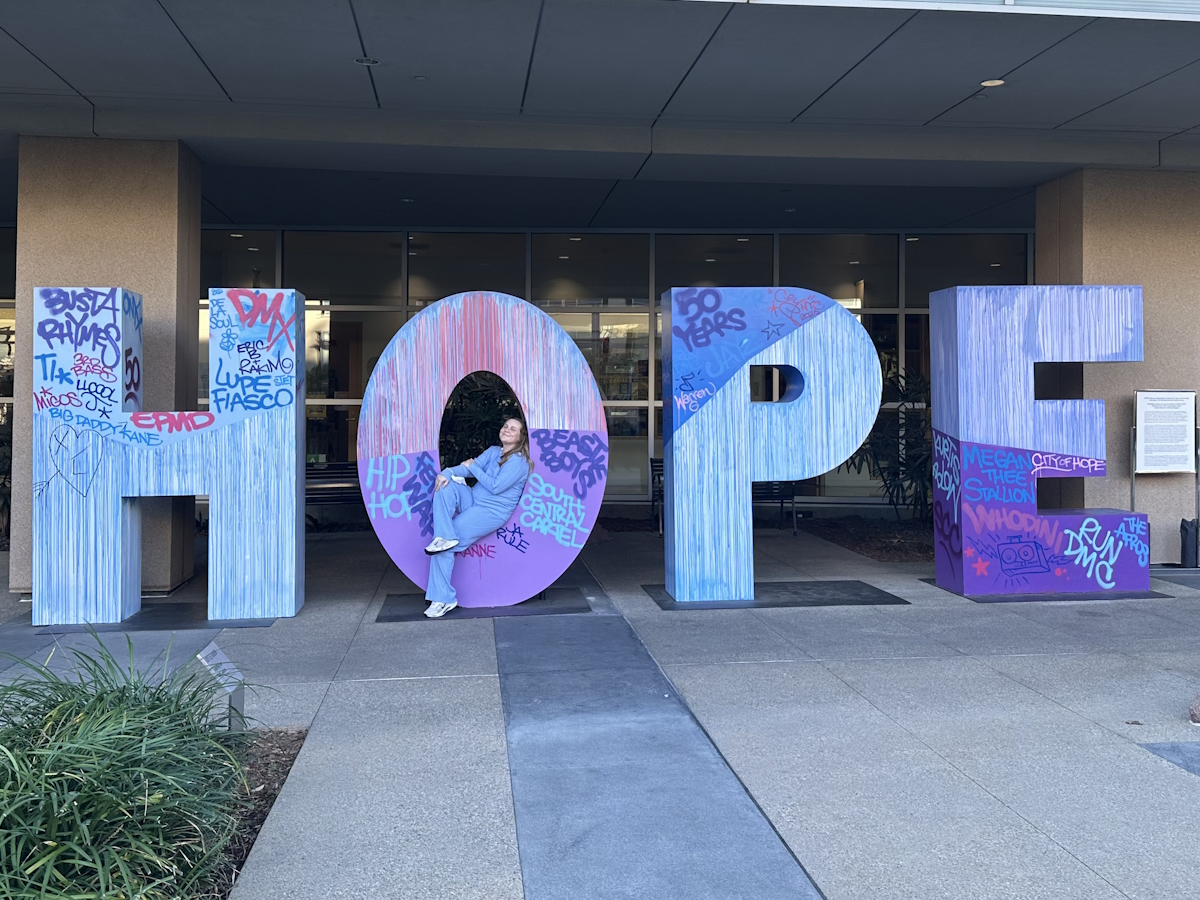
The team at City of Hope brought my case to the tumor board and found out that there was a surgeon there who did nothing but operate on soft tissue sarcoma.
Getting Additional Opinions
During those six weeks, I got more opinions. I saw a doctor at Memorial Sloan-Kettering and a doctor at City of Hope. The team at City of Hope brought my case to the tumor board and found out that there was a surgeon there who did nothing but operate on soft tissue sarcoma.
I felt like it was all serendipitous. When I was first diagnosed, I looked for other sarcoma patients and their stories on social media to help guide me through what I was going through. I came across a surgeon whose Instagram name was @sarcomasurgeon. He turned out to be the surgeon who said that he would be able to help me. I thought, Everything’s aligning. This is meant to be. This guy’s going to save my life.


Surgery to Remove the Tumor
I went for my pre-op and saw the surgeon. I said, “Things are not moving.” He admitted me to the hospital right then and there, and I had surgery the next day.
The surgery was supposed to be on April 20th and it ended up happening earlier on April 12, 2023. I was brought in emergently. I had an almost 14-hour surgery.
There were five different surgeons involved. Dr. Tseng, a sarcoma oncologist at City of Hope, led the team, which included 1 or 2 urologists and a gynecologic surgeon. They had to do a diverting colostomy so there was a colorectal surgeon involved.
They ended up having to call on vascular surgery because the tumor was fused to the neurovascular bundle in the left side of my pelvis so the major artery in my pelvis was severed. They had to graft it and repair it because the tumor was fused to it. The tumor was stuck to my sigmoid colon. It had not grown into my colon, but it was smashing it so severely that nothing could pass through.
They had to remove a piece of my sigmoid colon and half of my bladder. The tumor was attached to my left distal ureter, which is the tube that goes from your kidney to your bladder, so they had to remove part of that.
I didn’t care what morbidities or complications I was left with. I wanted the tumor out and I didn’t care what they had to do.
My ureter wasn’t long enough to reach my bladder anymore so they had to reroute my ureters so that they funneled into one. My insides have been MacGyver-ed. They grafted the arterial damage to the artery in my pelvis.
When I went in for the surgery, there was some discrepancy because the radiologist said they were concerned that the cancer had implanted in my peritoneum so they were calling it sarcomatosis, which would pretty much be there’s nothing we can do at this point.
He told me that he did not see that. He did not agree with that radiologist and that we were going to proceed with the surgery, but I needed to be aware that if he opened me up and saw that, then he would have to abort the surgery. That was a big thing going in because I didn’t know if it was going to be successful. I didn’t know if they would be able to get the tumor out at all.
After a few hours, my mom was under the impression that they must be proceeding with the surgery because I’d been in there that long. That was a little bit nerve-wracking. I didn’t care what morbidities or complications I was left with. I wanted the tumor out and I didn’t care what they had to do.


Recovering from Surgery
I spent two days in the ICU and about 10 days total in the hospital. They wouldn’t let me go home to Northern California for another month because they wanted me to be close by. I stayed with a friend in the LA area who was a nurse and took great care of me. I have been fortunate to have so many good friends through all of this who have been willing to step up and help out.
I had a nephrostomy tube in my back to drain my kidney, a drain in my abdomen, and a catheter in my bladder. I had all these tubes coming out of me and they sent me home that way for about a month before they finally let me go home to Northern California.
I come back for my first scans and there is a nodule in my lung.
He said, ‘We’re not going to mess around. We’re not going to wait and see what this turns into. I’m sending you to a thoracic surgeon and having that piece of your lung removed.’
Status Post-Surgery
After the surgery, the surgeon came to talk to me and said, “We got the whole tumor out with clear margins, but with sarcoma, that doesn’t mean a whole lot. There could be microscopic cells floating throughout your bloodstream that are waiting to re-implant somewhere else. I’m not telling you that to scare you, but that’s the reality and I want you to be aware.”
I followed up a few weeks later with my medical oncologist and he said, “I consider you to be cured.” I was elated at this point. This was June 2023 and I’m being told that I’m cured of stage 4 sarcoma. This made me laugh. I told him, “Okay. I know we’re going to continue with the scans every four months. I’m going to be cautiously optimistic because I understand the risks of this returning,” and he said, “No, no, no, you should be grotesquely optimistic.” There was a big celebration at this point.


Post-Surgery Scan
Fast forward to September, I come back for my first scans and there is a nodule in my lung. My doctor is still very optimistic. He said, “Look, it looks like that nodule has been there for a long time. I went back and looked at your old scans. It decided to grow a little bit and it was still less than a centimeter. It was tiny.”
He said, “We’re not going to mess around. We’re not going to wait and see what this turns into. I’m sending you to a thoracic surgeon and having that piece of your lung removed.”
Pulmonary Wedge Resection
In October, I had a pulmonary wedge resection. They removed the top part of my left lung with the tumor. It was confirmed to be metastatic sarcoma, but they got it all out. Turns out that’s the best-case scenario for me. If something pops up and it is operable, then that’s the plan because we know that I don’t respond to chemo.
When you get diagnosed with cancer, your whole life changes.
Side Effects of Treatment
All of the treatments that I’ve been through have left me with some pretty significant impairments. I have pretty severe neuropathy in both feet and damage to a nerve in my left thigh. I have a lot of muscle loss. I have been able to regain a lot of strength months after surgery, but for a while, I was falling a lot. I even fell and broke my wrist at one point.
I had a lot of instability, like the feeling of not being able to feel your feet. Your feet feel like they’re asleep, like pins and needles 24/7 so that’s pretty uncomfortable. But like I said, I’m alive.
Follow-up Scans
My most recent scans were on January 4, 2024, and they were perfectly clear for the first time since I started this whole journey.

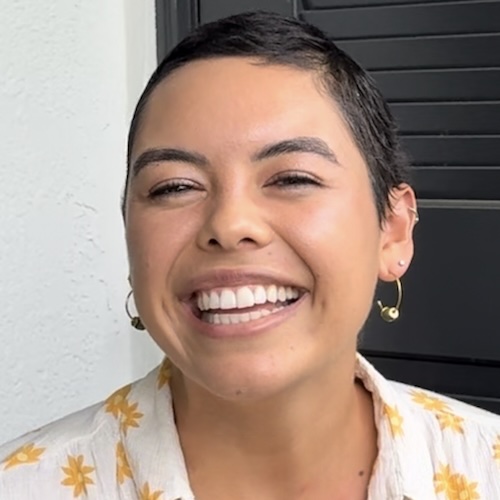
Sharing My Cancer Story
Part of the reason why I like to be so open about what I’ve been going through is sarcoma is a rare cancer and a lot of people don’t know what it is. When they hear the word sarcoma, they don’t necessarily know that it’s cancer or what it affects. It makes up less than 1% of all diagnosed cancers and there are over 80 subtypes. There’s not a lot of research. There aren’t a lot of treatment options.
When you get diagnosed with cancer, your whole life changes. It’s not as simple as, “I’m going to do chemo or have this surgery and then I’m going to go on my merry way and put this behind me.” For most people, that’s not the case.
The very first time my care team said that a colostomy was a possibility, I did everything I could to mentally prepare myself.
Having a Colostomy Bag
The colostomy has not been an issue at all. They told me that it would potentially be reversible. I don’t even care. It’s honestly improved my quality of life. I don’t mind it at all. It’s not hard to manage.
Most people wouldn’t know it was there if I didn’t tell them and the people who do know are people who know what to look for because they’re medical professionals that I encounter in my day-to-day life. Nobody needs to know it’s there if I don’t tell them.
I’ve had a pretty significant injury to my bladder so after all of the radiation and the surgery, I was left with a fistula. A hole that developed in my bladder has left me with pretty severe urinary incontinence, which is difficult for a woman in her late 30s who likes to travel and do things.
I’ve been confined to managing that. I spent about four months with a catheter in my bladder in 2023. We’ve tried a lot of things to get it to heal. I saw a specialist who attempted to repair it but my bladder and vaginal tissue were so severely damaged from all the radiation and the surgery that the repair did not work.


I’m getting ready to have an ileal conduit surgery, which is a urostomy so I’m going to have two ostomies. We decided that this was the quickest way to get my quality of life back so I could get back to traveling, going on girls’ trips, getting in a swimsuit, and not having to worry about urinary incontinence or having a catheter.
The very first time my care team said that a colostomy was a possibility, I did everything I could to mentally prepare myself. I went on Instagram and started following people who have colostomies, watching their day-to-day lives, how they dress, how they manage it, and how they maintain it. It helped me wrap my head around these women living these lives. They’re in swimsuits, wearing cute clothes, doing this and that, and nobody has to know that they have a colostomy. I can do this.
When I went in for the surgery, they still didn’t know if I would need it or not. It was going to be a surprise when I woke up. But when they told me, I wasn’t upset, not even a little bit. I said, “You guys did what you had to do to save my life and this is my new normal.”
For the most part, it doesn’t affect me. It’s not a problem. It’s only improved my quality of life.
When I came out of surgery, there were so many things going on that I didn’t pay any attention to it. The ostomy nurse saw me several times before I was discharged from the hospital and made sure I was comfortable changing it. She taught me how to do it and then she had me do it with her there so that she could watch, critique, and offer suggestions. We talked about the different products that were available and what I should try. She set me up with my first order of supplies and then I went from there.
I do think that I have a little bit of an unfair advantage being a nurse. Things that might be a little weird or gross to a regular person don’t necessarily gross me out, but it hasn’t been trouble. I haven’t had any horror stories, like a leakage accident, happen.
There have been times when the bag starts to detach from my abdomen, but I usually can tell that something’s going awry and I can intervene pretty quickly. For the most part, it doesn’t affect me. It’s not a problem. It’s only improved my quality of life.


Words of Advice
If you were to ever be diagnosed with sarcoma, the very first thing you need to do is search for a sarcoma center at a hospital with a cancer center. Sarcoma does not behave the same way as solid tumor cancers. It’s its own beast and requires somebody who knows exactly how it behaves and how to treat it.
I do wonder what if. What if I had been seeing a sarcoma specialist from the get-go? Not only should you see a sarcoma specialist right off the bat, but you should also get multiple opinions. I know that can seem daunting when you’re faced with a new diagnosis. You feel overwhelmed and don’t know what to do first.
I very much remember being in that situation where somebody like me, who is a nurse, who wants to understand everything about what’s going on, shut down. I wanted to curl up in a fetal position and let somebody else deal with it. It was too much for me to handle.
Once somebody is treated for cancer and receives clear scans or told that they have no evidence of disease, they still need support. It doesn’t end right there.
Fortunately, I have a really good friend who helped her mom navigate through a colon cancer diagnosis and she knew how to be that advocate. She stepped in and made phone calls for me. She handled what I was not capable of handling at the moment. I’m really grateful to her for that.
She set up multiple opinions for me because it’s overwhelming. You just want to go with what the first doctor says, get started with treatment, and get going, but it’s important to get multiple opinions from places that specialize in sarcoma.
Once somebody is treated for cancer and receives clear scans or told that they have no evidence of disease, they still need support. It doesn’t end right there. I’m going to continue to be scanned every four months, probably for the rest of my life, and I have to deal with that paralyzing fear every time.
I have all of these disabilities and complications to deal with now. This is the price that I had to pay to have more time on this earth and I would do it again if I had to.
Continue to support your friends who have been through cancer because it doesn’t go away once they get that all clear.


Honestly, if you’re comfortable, ask your doctor for medications that can help. It’s okay to not be able to deal with it all on your own. I take medication for anxiety when I go in for scans and usually, I have to start taking it a few days before.
This might be different for other people, but I can show up to surgery alone; it doesn’t scare me. I can go sit in a chemo chair alone; that’s fine. But when I’m going to have the doctor deliver my scan results, I need to have somebody close to me with me. I do my best to remind myself that whatever the result is, we will take the next steps and deal with it.

Inspired by Brandie's story?
Share your story, too!
More Soft Tissue Sarcoma Stories
Kara L., Synovial Sarcoma, Stage 1B
Symptoms: Pain behind left knee, needle-like sensation in left foot
Treatments: Surgery to remove what was thought to be benign tumor, chemotherapy, final surgery, radiation (36 sessions)
...
Jillian J., Synovial Sarcoma, Stage 3
Symptom: Pain in leg for over 15 years
Treatments: Surgeries (tumor resection, thoracotomy)
...
Marisa C., Synovial Sarcoma, Stage 4
Symptom: Small bump on the foot (stable for years, then grew during pregnancy), pain when pressed
Treatments: Surgeries (below-knee amputation, pulmonary wedge resections, segmentectomy), chemotherapy, radiation (lungs & hip)
...
Julie K., High-Grade Poorly Differentiated Spindle Cell Synovial Sarcoma, Stage 4
Symptoms: Chest and back pain after car accident, trouble breathing
Treatments: Chemotherapy, surgeries (lung resection, video-assisted thoracoscopic surgery or VATS, neurectomy, rib removal), radiation therapy (CyberKnife)
...
McKenna A., Synovial Sarcoma, Stage 3 Grade 3B
Symptoms: Insomnia, weak immune system resulting in persistent illnesses such as UTIs and strep throat, severe swelling in left leg
Treatments: Surgery (tumor excision), chemotherapy, radiation therapy (proton radiation), integrative therapies
...
Monica H., IDC, Stage 2B & Undifferentiated Pleomorphic Sarcoma
Symptoms: Tightness and lump in left breast
Treatments: Chemotherapy, radiation, surgery
Nicole B., Undifferentiated Pleomorphic Sarcoma, Stage 3
Symptoms: Severe intolerance to food, nausea
Treatments: Surgeries (cholecystectomy, Whipple), chemotherapy (Gemcitabine and Taxotere)
Ashley W., Desmoid Tumor
Symptoms: Leg tightness, increased swelling in leg
Treatments: Chemotherapy infusion (Methotrexate, Navelbene), oral chemotherapy (Nexovar)
...
Demi D., Desmoid Tumor
Symptoms: Fatigue, lump in hip
Treatments: Surgery, radiation, chemotherapy
...
Alicia B., Desmoid Tumor, Stage 4
Symptom: Lump in right armpit
Treatments: Chemotherapy, radiation, targeted therapy, clinical trials, surgery, including forequarter amputation
...









One reply on “Brandie’s Stage 4 Leiomyosarcoma Story”
Thank you for your story!
Leiomyosarcoma Support & Direct Research Foundation (LMSDR) offers support and education for LMS patients, and we raise money for LMS specific research. Join our support group! http://www.LMSDR.org