Jeffrey’s Gleason Score 7 Prostate Cancer Story
The Patient-Doctor Story:
A Shared Decision-Making Conversation Between Patient & His Doctor

Jeffrey P., Diagnosed with early stage prostate cancer (Grade 2) at 59 years old.

Dr. Christopher Weight, Cleveland Clinic, Center Director for Urological Oncology
Full Transcript
- Introduction
- Getting Diagnosed
- Treatment Decisions
- First conversation on prostate cancer treatment
- How did you decide to pursue surgery?
- Breaking the news to loved ones
- Knowing other people’s prostate cancer experience was helpful
- Patient POV on treatment options
- Oncologist POV on treatment options
- Early stage prostate cancer treatment options
- Advanced prostate cancer treatment options
- Radiation
- Surgery
- Focal therapy
- Understanding the Prostate Cancer Scoring System (Gleason)
- Being an Empowered Patient
- Patient self-advocacy
- The impact of a doctor’s personal approach
- Dr. Weight’s POV on empowered patients
- Seek a second opinion!
- Treating patients as individuals in medicine
- Family discussions on risk of prostate cancer
- The importance of diverse patient voices
- The importance of patient stories
- Healthcare disparities
- NEXT: Al Roker's Prostate Cancer Story
- Prostate Cancer Patient Stories
The interview has been edited lightly for clarity. Thank you, Jeffrey and Dr. Weight, for sharing your voices!
This is not medical advice. Please consult with your healthcare provider for treatment decisions.
Introduction
Stephanie Chuang, The Patient Story: Hi, everyone, it’s Stephanie with The Patient Story, and I am thrilled to be able to have this conversation that we’re going to have today with two wonderful gentlemen.
First, Dr. Chris Weight, the director at the Center for Urologic Oncology at Cleveland Clinic, someone we’ve had the pleasure of speaking with before. And one of his patients, Jeff, who’s here to share his prostate cancer story.
Welcome to the both of you. I thought we would kick it off with an introduction. First of all, we’ll talk to Dr. Weight, if you could just tell us a little bit about yourself and your work.
Dr. Christopher Weight, Cleveland Clinic: Thank you, Stephanie, very happy. I’m happy to be here and happy that Jeff joined us. I think patient stories are a really important part of understanding cancer care. Today we’re talking about prostate cancer.
As Stephanie said, I’m the center director for urological oncology at Cleveland Clinic, and I take care of patients with prostate cancer, bladder cancer, kidney cancer are the three primary cancers and also some other, more rare cancers.
I have a personal connection to prostate cancer in particular because my dad had prostate cancer while I was in the midst of my surgical training.
That really influenced the way I think about taking care of patients and understanding what, maybe more, what it feels like to be on the family side of a cancer experience.

The Patient Story: Wow, thank you so much for sharing that. That’s incredibly powerful, that you’re driven not just by your intellectual curiosities and ambitions, but that you have such a personal tie.
Thank you for sharing that, Dr. Weight. We’re going to now get introduced to Jeff, one of Dr. Weight’s patients. Jeff, we would love to learn more about you.
Jeffrey P.: Hello, everyone. Thanks again to Stephanie for the invitation. My name is Jeffrey P. I’m a retired federal government employee. I retired from the federal government from 38.5 years of service.
I worked with the agency of Defense, Finance and Accounting Service, where I was working in the finance arena paying people, civilian and military people. I’ve been in Cleveland for about 13 years. Thank you, Dr. Weight, for your assistance in this process here.
Getting Diagnosed
The Patient Story: Wonderful. Today’s conversation is going to be about the decision-making process and the patient-doctor relationship. So really excited to have that. I’d love to start with you, Jeff.
I know that you got your first PSA test many years ago, and then at some point it got to go from your primary care doctor to a urologist, and then shifted over to Dr. Weight. Can you talk about the shift from your urologist to Dr. Weight and how you were able to find him?
The first tests and scans
Jeffrey P.: First, it started out with my primary care physician back in 2007 or 2008, when I first began with him. My numbers began to inch up little by little.
When it started to go over 1 or 2, I sent him a message and said, “Hey, should I be concerned about my numbers increasing?” He says, “No, no, don’t worry about it just yet. We will continue to look at it a year from now and if it continues.” And it did.
Finally, they referred me over to a urologist. At that particular point in time, we did a PSA test, and then from there we went to a biopsy and that type of thing. Then from that, the biopsy revealed — I think there were 2 or 3 of those — that each test came back negative.
Then finally he called and said, “We’ve done a PSA test. I think we need to move forward to see if we can take a more aggressive testing: IsoPSA.” He said that test will usually determine if you have cancer or not. And so we did.
We got the results back, and he says, “Hey, we’ve seen something in there that maybe we need to have a closer look, and so I want to refer you over to Dr. Christopher Weight and have him do an MRI PSA.” We did the MRI, and then we did the MRI biopsy. Then Dr. Weight revealed what I have today, prostate cancer.
When should people move to specialists?
The Patient Story: Thank you for walking us through that. That was really great; that was very succinct. I hear that you had a lot of monitoring go on for many years. Dr. Weight, I actually want to jump in and ask you this question. How important?
We know primary care is the first point of contact for a lot of patients. How important is it, and at what point should people be considering going to a specialist first, maybe a urologist? And then to someone like you who specializes in oncology?
Dr. Christopher Weight: Prostate cancer screening has taken a little bit of a battering over the years. You know, 10 years ago, I think maybe we were overdoing the screening and doing it too often, too frequently, getting too excited about the results.
That led to a period of time where we certainly reduced the risk of dying from prostate cancer nationwide. But at the same time, we diagnosed and overdiagnosed a lot of people.
Now there has been some revision in the way we do screening. There may be a lot of confusion among the primary care doctors who have to focus on a lot, and I don’t envy them one bit. They have a lot to focus on, and cancer screening is one portion of what they’re focused on.
But they may not be apprised of the most current guidelines and the nuances of how to appropriately screen. In an ideal screening situation, we identify those who are at risk and send them on to get further testing, but leave those who are not at risk alone and don’t get into a situation where you have a lot of people being over-tested and over-diagnosed. So it’s a tricky balance.
Factors for whether to test for prostate cancer
- PSA level (blood test)
- Exam
- Family history
- Ethnicity
It’s based somewhat on your PSA level, which is a blood test that many men know about and have had drawn. But it’s also based a little bit on your exam, on your family history, on your ethnicity.
I would recommend that you have a conversation with your primary care doctor if they start to be unable to answer some of these questions, you know, should I do it more often because of this family history?
Then that might be a good trigger to at least go to a urologist who has a little bit more experience with this and finding the appropriate trigger point for getting additional testing.
Biopsy test
Jeff’s story’s really interesting because he got sort of a multifaceted screening program. He was biopsied before and did not find it. Is that right?
Jeffrey P.: That’s correct.
Dr. Christopher Weight: That’s not unusual. Biopsy is the gold standard, so to speak. It’s the test that we make the treatment decisions based on. But it’s also not perfect.
You’re taking a sampling of the prostate, 12 little hair-size samples of a prostate, and you may or may not get the right answer. I think this is a good case of that, where there was a previous PSA testing, previous biopsies, and those did not reveal the cancer.
The good news is usually that means that cancer is small, but I think it’s good to know that there are additional tests that are available that can help lead us down the pathway to hopefully finding a cancer that may become a problem down the road while, for the most part, leaving most men alone that have very low risk of having an occult cancer.
What is the PSA test?
The Patient Story: Got it. I want a quick follow-up, Dr. Weight, on that. Jeff shared his PSA levels, and they ranged over a period of over a decade, going from 2-something to finally with the IsoPSA test 10-point-something.
What do those numbers mean? I understand that it’s also about the pattern, how quickly the numbers are escalating. Is that right?
Dr. Christopher Weight: Yes. The PSA is a portion of a protein made only in the prostate. This peptide gets into the bloodstream and can be identified on blood tests. The quote-unquote normal level was 0 to 4. So anything under 4 historically has been considered normal.
Part of what we understand now, as time has gone on, is that doesn’t really make sense. You can have prostate cancer and have a PSA under 4. I’ve had patients with PSAs under 1, but that’s quite rare.
Also, it’s important to know that most men with a PSA from 4 to 10 don’t have prostate cancer. But as that PSA level goes up for the average man, the risk of prostate cancer goes up.
Benign causes of increasing PSA levels
- urinary tract infection
- urinary retention
- having sex
But this is confounded by age and some ethnicity issues and differences. There are some genetic alterations that increase your PSA, as well as many benign things that make your PSA go up. For example, a urinary tract infection or urinary retention, even something like having sex can temporarily make your PSA go up.
So it’s always important not to get too excited about one PSA. Really more important [is] the trend, especially if there’s a sudden change in that trend that’s not proportionate to the normal rise that we see as all men age.
The Patient Story: Perfect. Thank you, Dr. Weight. Jeff, I want to go back to you now. We’ve come up to this point. You meet Dr. Weight. You go through more tests and scans, and then you get the news. What do you remember about the diagnosis from that day?
Recalling the moment of diagnosis
Jeffrey P.: Because I’m a big user of the MyChart, and so once the results were out on MyChart, I saw them and began to Google certain words, and the results out there are malignant this and that.
Okay, so that’s what this word means. So this is what I’m looking forward to. When Dr. Weight came into the room, he had the results in his hand, and I already had an inkling what he was getting ready to tell me.
So when he showed the results, I wasn’t shocked. I guess I was shocked. But then again, I wasn’t because I’d seen the results in the MyChart record. So when he told me, I was numb for a second. Then he began to go through the recommendations of fixing it, what have you.
Treatment Decisions
First conversation on prostate cancer treatment
He said surgery was one. Radiation was another one. The seeds (implants) was another one. And then I think it was something, I think if I remember correctly, the focal (therapy) was another example of treatment.
Just sitting there, if I had to make a decision right now, we would just take out the prostate and be done with and move on with life.
He said, “Well, just take a few days and take some time to think about it, and then when you make a decision, call me back and we’ll set up whatever your choices are, whatever you decide to do.”
How did you decide to pursue surgery?
That was in February. I think maybe two weeks later, two to three weeks later, I had broken the news to my family. One of the questions that came up from my family was, “Would you need to have radiation treatment?”
I said, “The doctor didn’t say anything about that, but I will go back to him and check.” So I began sending Dr. Weight and Dr. Modlin both similar messages. Will I have to have radiation treatment after this and another?
Both of them came back and said, “At this point, you will not. But we have to find out what happened after the pathology comes back.” When I came to them and I said, “You know what? I’m ready for it.” I told Dr. Weight I’m ready for the surgery. Let’s schedule it so I can get this behind me, and we can move on with life.
The Patient Story: Great. And that was how you came to the decision. Actually, Jeff, really quickly, what I’m hearing from you is that you were like, “I just want to move forward.” Anything else you want to say about what went into the decision? And it sounds like your family had an impact, too, in terms of what they were concerned about for you?
Breaking the news to loved ones
Jeffrey P.: Well, they were because of all of our family’s in Alabama — my mother, sisters, everybody’s there. I’m the only one who’s out of state. And so breaking that, having that conversation, it was a tough one.
I started out with my sister, who is a breast cancer survivor. We share similar stories. She told me about her story, and I said, “At this point, we’re going to remove it.” And she said, “You’re going to be fine.” She says, “Well, I’m not sure how you’re going to tell the rest of the family.”
I began slowly but surely breaking the news to my brother and told my older sister. And then finally, I told my mother. She was the most difficult one to tell.
But in the meantime, when all of that was happening, I was looking online to see how this procedure was going to be done as such.

Knowing other people’s prostate cancer experience was helpful
I’m not sure if I told you this, but I have a fraternity brother who had a similar case like this nine years ago, and he was telling me about his story. That he has a huge scar in his stomach So I began to, like, “Oh my God, I’m going to have this huge scar on my stomach.”
But then when I began looking at online and saw how the robotic surgery was being done, it’s like only five little scars, two little inches maybe. That helped me a lot, just to see how it was going to be done.
I think there was an article from the Mayo Clinic that said you’ll be down for maybe two to three weeks. If you’re just doing sedentary-type work, maybe you’ll be up and operational within a week and a half. If not, four weeks at most.
You may go back in to have staples removed or whatever, and the stapler wasn’t there. You may have to wear towels for seven to 10 days. And even Dr. Weight told me about that as well.
That sort of put me at ease as to the process and the recovery time. So that helped me and my decision. I did not like the radiation treatment. I did not like the seeds, because I think — the doctor may have said or I may have read it — that there may be a chance, with the seeds, it may come back again. And I do not want to go through that cycle twice. That’s why I said, “Go to the surgery.”
When I mentioned it to my primary care, he said, “You know, at your age, surgery probably is the best thing. Just take it out and be done with it. Get the healing process started.”
The Patient Story: So you had a lot of different input. That’s great, and you landed on the surgery. Dr. Weight, I would love to hear from the medical perspective.
What were the treatment options? It sounds like with prostate cancer, it was localized for Jeff, so it wasn’t advanced. It hadn’t spread. What are the typical treatment options there, and how do you like to characterize it to your patients?
Dr. Christopher Weight: I think this is always a really challenging discussion. I’m amazed actually at how much Jeff understood because you have to transfer a lot of information across to this patient, and I would be interested to hear from you, Jeff, as well.
On top of the shock of being diagnosed with cancer, now suddenly you’re given four or five options, of which many you don’t have any experience in. I always imagine it must feel overwhelming, and I would just be anxious to hear.
I’ll go through kind of my algorithm, but I’d be anxious to hear, Jeff, how that felt for you. And if it was made a little bit easier by getting a little peek ahead of time with my chart.
Patient POV on treatment options
Jeffrey P.: Yes, it was overwhelming, but the MyChart has sort of lessened the blow, if you will, because I had a chance to Google some things in the results there. It sort of eased my mind as opposed to not looking at it, not having an advanced knowledge of that.
So it was overwhelming, but then again, it wasn’t. The way you were explaining it to me that day is sort of, “These are your options, and if I was you, I would do this,” or whatever. But you left the decision up to me to make the final decision.
I relied heavily on your decision, but I know the ultimate decision was mine to make it, and so it was overwhelming.
But again, the peeking of MyChart sort of lessened the blow. I think the second time I visited with you, it really settled in with me, and I was getting ready to have a meltdown in your office. But you let me have my way.
Because at that point, the reality was setting in there because I really do have it, and I was getting ready to have the surgery. The reality was going to happen. I began to have a meltdown in your office, a mini meltdown. But you let me have my way. You said, “Again, if you have any questions, feel free to give me a call back.”
Oncologist POV on treatment options
Dr. Christopher Weight: Well, great. Thank you for sharing that. I think that the first thing I always try to communicate is just to take a breath. Sometimes it may feel like life will never be the same. Or you’ll never be happier, and you’ll never smile. You never do the stuff you love to do again.
And you take a breath. And then let’s talk about the options now.
Early stage prostate cancer treatment options
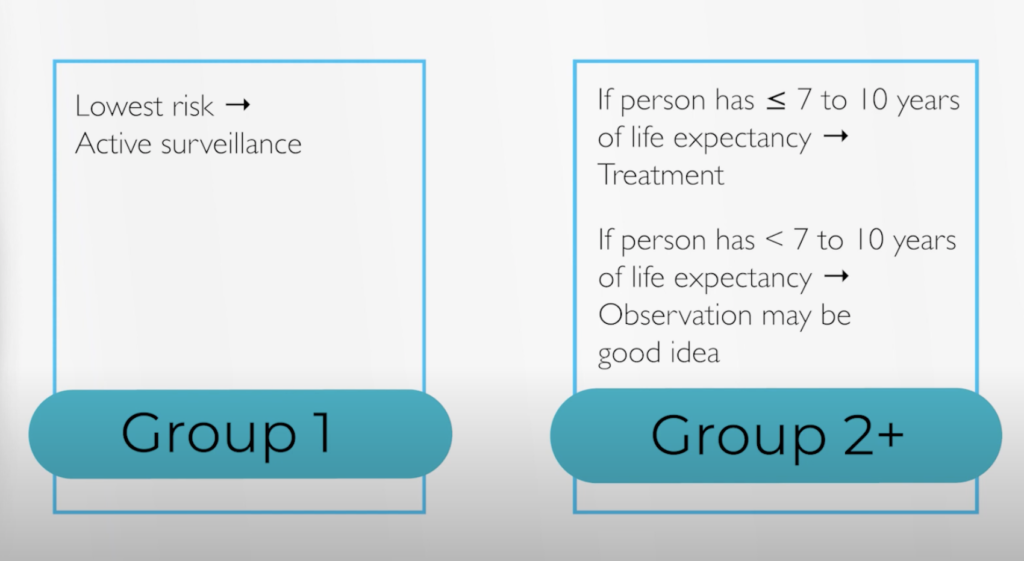
When I talk with my patients, I always like to generally say there are four general categories. One is the observation, and for actually a lot of prostate cancer, you can closely watch it, and that’s a safe treatment option.
It feels weird to patients, where you say, “What? I have cancer, and we’re just going to not do anything about it?” But we know early stage, small-volume prostate cancer is very treatable by what we call active surveillance.
It’s close monitoring, and we know that 15 years later, almost all those men are still alive, and at least half of them or more never got any treatment in those entire 15 years and are still doing okay.
Advanced prostate cancer treatment options
But as you move up in the stages of and the grades of prostate cancer, that becomes a less appropriate option unless you have really other competing comorbidities. So the first question always to be asked in my mind is, should we treat this or not?
If the patient is young and healthy and if the cancer is at least a grade Group Two or higher, generally, the answer is yes. Then you move into the treatment options, and there are kind of, in my mind, three categories of treatments.
Radiation
- External beam radiation therapy (EBRT)
- Radioactive seed implants (brachytherapy)
One is radiation treatments, which Jeff referred to, and the common one is an external beam radiation, where you lie on a table and get hit with an X-ray of some sort or some sort of energy force that delivers radiation to the prostate.
The other type is seeds. This is done in the operating room. You have small, little rice-sized pieces of brachytherapy seeds that are placed into the prostate, and those give off the radiation locally. But many of the side effects and many of the pros and the cons are similar between those two types of treatments.
Surgery
- Open radical prostatectomy or perineal prostatectomy (older, more traditional)
- Laparoscopic prostatectomy (robotic surgery)
Then you have surgical treatments. Historically, for 70 or 80 years, that was an open radical prostatectomy or a perineal prostatectomy, but where you made the bigger incision, which sounds like that’s the one you’d heard about.
In the United States now, though, most surgery for prostate cancer is done robotically because the incisions are smaller and the total recovery is faster. The risk of needing a blood transfusion and a few other complications are lower. That’s where you remove the prostate and usually the nearby lymph nodes.
Focal therapy
Then the last category, which is an emerging category, is focal therapy. The idea behind focal therapy is that if you catch it early enough, you may be able to treat just one part of the prostate instead of the entire gland, which historically radiation and clearly removing it does.
This is a much smaller group of people that are eligible for this kind of treatment, and as our imaging gets a little better, as our biopsy techniques get better and we get a little bit more confidence that we have identified the part of the prostate that’s affected only, there may be some eligibility for focal therapy.
There are different types of focal therapy for prostate cancer. Those are kind of the general categories that I introduce to the patient. Then as we consider their specific details, we kind of go down one pathway or another, or as we also consider their priorities and what makes sense to them.
Understanding the Prostate Cancer Scoring System (Gleason)
The Patient Story: Thank you both for sharing. I also thought that tidbit about finding out on MyChart was really interesting, Jeff, how that lessened the blow for you. Dr. Weight, going back to what you were just describing, though, Jeff described his situation as a Gleason score seven.
Does that dictate the grading, and do those numbers really inform which path is the best way? I know it has to do with the individual as well. I also wanted to ask about how people are worried about the order in which you might receive these treatments. One of the conceptions is if you get radiation, then surgery is off the table for later. These kinds of things.
Old scoring system
Dr. Christopher Weight: Yeah. Great, great question. The old scoring system for prostate cancer was a little bit confusing, and that was the sum of the two most common patterns seen in the prostate.
You could have a Gleason seven that could be either a 3 + 4 or a 4 + 3.
In addition, to add to the confusion, those actually behave differently. So the 4 + 3 behaves a little bit more aggressively than the 3 + 4 in general.
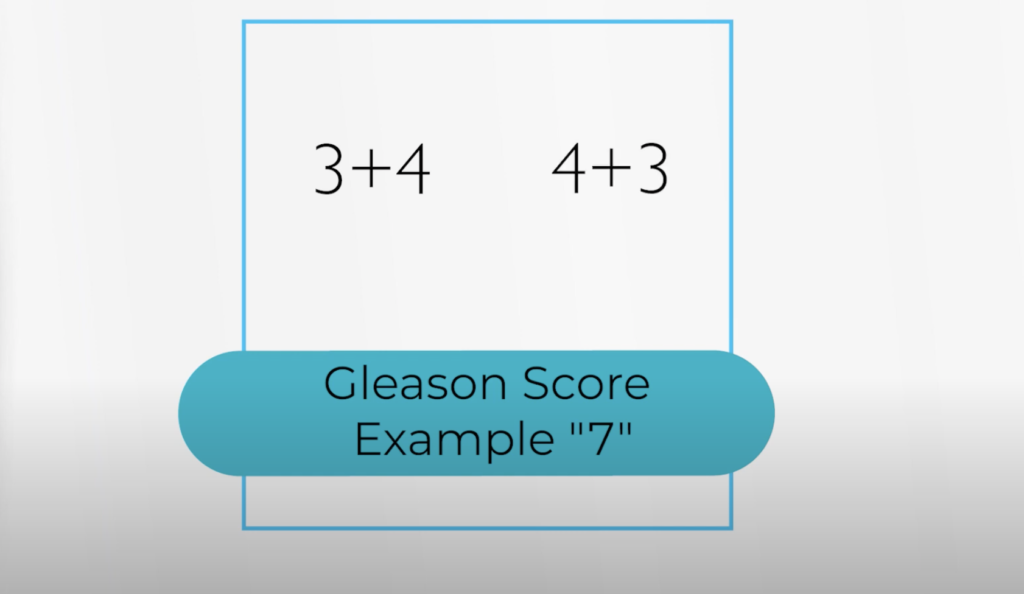
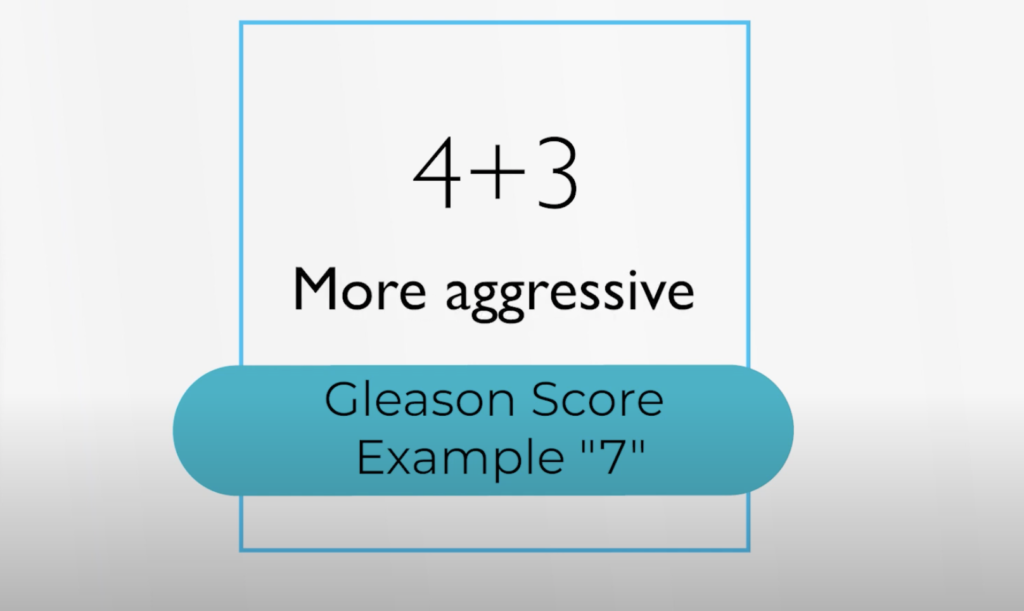
The other thing that was confusing to a lot of patients is the lowest grade prostate cancer was a 6, but it doesn’t feel like 6 is the lowest, right?
It feels like it’s on a scale of 1 to 10, and you’re a 6. You’re almost to the top, it feels like. So we had a little bit harder time convincing patients, “Yeah, I know it’s a 6, but it’s not that risky.”
New scoring system
The new scoring system has shifted that kind of 6 to 10 system to a 1 to 5 system. It’s based on the same underlying patterns. But it’s just, I think, a little bit more intuitive, and it’s easier to communicate to the patient.
On the old scoring system, it was a 7, but it was a 3 + 4. On the new scoring system, that becomes a 2. So that’s where Jeff’s cancer fell.
Treatment decisions based on score
We generally like to leave 1’s alone and watch those closely. If there’s a high volume, we may consider some additional testing like genomics, which we take the biopsy that was already done, and we do some additional testing on that to see which genes are expressed or suppressed. That pattern of expression has been associated with prostate cancer outcomes.
In general, we like to use active surveillance for the lowest risk group. Then in the group 2 or higher, generally, for the average person that has at least 7 to 10 years of life expectancy, on average, that patient will benefit from treatment.
If they have less than 7 to 10 years, then it’s very unlikely the average patient, except for the most aggressive kinds of prostate cancer, will benefit from treatment. Observation may continue to be a good idea in that situation.
Sometimes in people who are older, who are sicker, we may extend the watching criteria to people who are even in grade Group 2 or 3. And you had another question.
The Patient Story: Yes, it’s OK. Yeah, I asked you a lot. The order in which you might undergo a particular treatment.
Surgery before radiation vs. radiation before surgery
Dr. Christopher Weight: So this one, this is a contentious topic sometimes among prostate cancer specialists, but it’s easier to sequence surgery, followed by radiation.
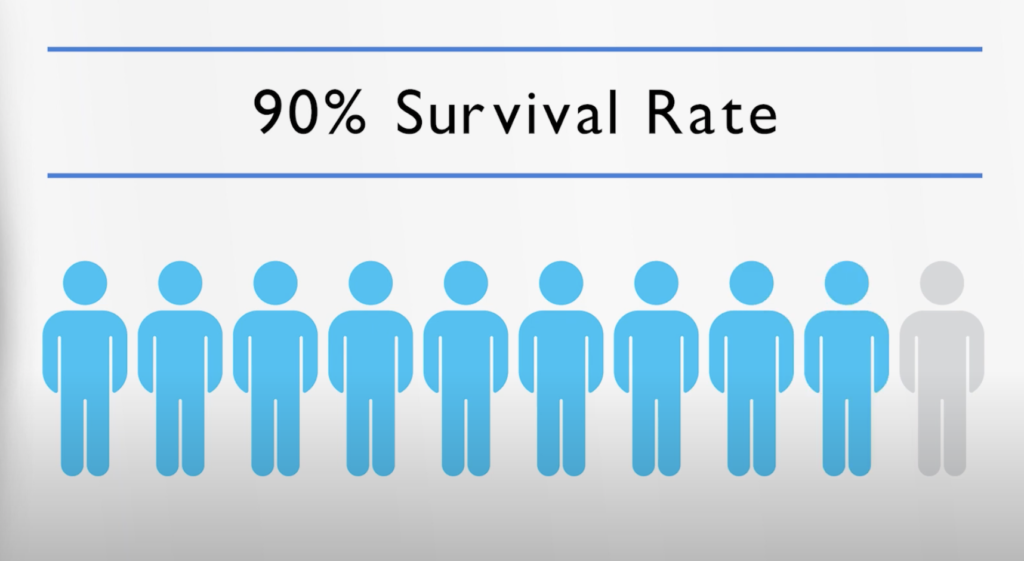
The good news is for tumors like Jeff’s, most of the time one treatment is more than adequate, and one treatment has a very high chance with a cancer-specific survival on average usually in the 90% range.
Meaning if you take 100 people, 90 of them will still be alive from their cancer standpoint 10 years later. So that’s good news.
But in the more aggressive tumors, you may need multiple treatments. You may need surgery and radiation and hormone therapy. The sequencing is a little bit easier, a little bit lower risk — surgery, followed by radiation. You can do surgery after radiation, but it’s a much higher risk proposition. Not very many surgeons do it because of the riskiness of it.
I always like to compare it to making a grilled cheese sandwich. It’s way easier to take the cheese out before you grill the sandwich than to take it out after you’ve grilled it.
So surgery just is a simpler, lower-risk option if there has not been any radiation.
The Patient Story: Thank you for laying that out. I think it’s interesting that even among specialists, there are some areas still where there’s debate, still a lot of medical different opinions, right?
Jeff, I’m curious after, at this point, you know, Dr. Weight’s presented all the options. I know you did a lot of your own research. Dr. Google pops up quite often nowadays. But how much did you feel like you wanted to rely on Dr. Weight’s opinion versus your own? Were you confident in being able to make the decision more on your own after getting this information?
Real doctor vs. Dr. Google (research)
Jeffrey P.: I guess it was a combination. As I said, Dr. Weight gave me the diagnosis that day. He told me about his story. His dad was my age when he was diagnosed, and he lived a very productive life after that. And considering your age, you live a similar lifestyle as well. Between that and my research online, and that helped me make the decision, so it may be a combination of the two.
The Patient Story: On that note, Jeff, we talked a little bit about this earlier before we started recording. Oftentimes patients feel the need to be, say, “a good patient.” And I think you gave a great example that showed the relationship that you and Dr. Weight would have. Can you talk about that?
Being an Empowered Patient
Patient self-advocacy
Jeffrey P.: After I broke the news to my sister, who is a breast cancer survivor, she was asking me, “Do I need radiation treatment?” Then I began reaching out to both Dr. Weight and Dr. Modlin and asking them the same questions.
In my mind, if they weren’t responding within the two days or three days that they were saying, I was getting nervous and getting nervous. Finally, I reached out to one of his nurses in the triage area. She said, “You know what? It’s probably best to come in to see Dr. Weight and ask those questions.”
When I got in there and I talked about it, he answered my question. I said, ‘Again, I feel like I’ve been a pest. I do apologize.’
He says, ‘You’re not being a pest.’ He said, ‘Just feel free to ask any questions you may have. Just feel comfortable asking me a question.’
But I felt like because I was going in two different directions that I was bothering both him and Dr. Modlin by my question, but he gave me some reassurance. He said, “You’re not being a pest.” He says, “Just feel free to ask any questions that you may have. After today, if you’ve got any more questions, just reach back out to me, and we’ll be more than happy to answer your questions.”
In fact, [my primary care doctor] said Dr. Weight has the highest bedside manner that he can recommend to me in this area. That sort of eased me down, and that sort of settled me down some as well.
The Patient Story: I love that you shared that because, of course, we know Dr. Weight’s credentials and at Cleveland Clinic, and it’s really important to find someone you feel comfortable with [who has] the medical expertise.
The impact of a doctor’s personal approach
Jeff, how did that make you feel in terms of being more of an empowered patient, perhaps, when you finally heard this directly from him — hey, you’re not being a bother. Go ahead and ask me whatever questions you need.
Jeffrey P.: Like I said, that sort of settled me down because I was already nervous. I was about to have that little mini meltdown in his office. But that sort of settled me down. He was like, “You’re not being a pest. This is something that you were going to go through. If you have any questions that you may have, feel free to reach out.”
After he said that, it was like, okay, I’m not bothering him. Just ask the question. If you have something tonight or tomorrow or whatever, just feel free to ask any questions you may have. And I felt comfortable with him that day. That just really put me at ease.
The Patient Story: One more thing about that. When Dr. Weight shared with you such a personal tidbit, that his father had been diagnosed with prostate cancer, and gave you more of that personal bit of information, how did that impact you? How did that help you?
Jeffrey P.: I may have told you before, but I’m a man of faith. I believe in God. With that, his father lived a very productive life. Then speaking to my fraternity brother, who was my age eight years ago, had a similar surgery. Hearing that news made me feel, hey, this is not the end of the world. There’s still time left to go forward.
That sort of helped me make the decision to say things are going to be okay. I talked to my sister, who’s in ministry. She also said, “Hey, you know God. God knows you. You’re going to make it; you’re going to survive through this whole process.” That, too, sort of settled me down a bit because it was after I got that initial news.
Subconsciously, I think I was still on the edge, but I guess that’s to be expected. But subconsciously, I was still on edge. I didn’t sleep very well for a couple of days after that. Then the closer I got to the surgery, it was even more sleepless nights and what have you. I guess that’s to be expected.
The Patient Story: Definitely. You just get so overwhelmed with this news. I don’t expect anything otherwise. Thank you for sharing that, Jeff. Dr. Weight, speaking about the questions, you know, and I know you gave Jeff that reassurance, “Ask whatever you need.”
I know it depends on the person. What are some of the most important questions you think patients should be asking? At this point, whether it’s about treatment or what have you.
Dr. Weight’s POV on empowered patients
Dr. Christopher Weight: I think it’s important. It’s actually a hard process to become an empowered patient. I think we’re not used to it. We’re not good at it. We don’t have the experience generally, especially if this is your first, so to speak, rodeo in the medical specialty or in the medical field.
I’ve thought a lot, “How do we help patients get there?” I think the patient should really feel like they are in the driver’s seat. That’s hard to do because when you get diagnosed with cancer, it feels like everything’s out of control. Everything’s happening to you, people are making predictions about your life, and you feel like you don’t have any control.
Seek a second opinion!
But I think it’s important to remember that you do. I really like what Jeff did. He got multiple opinions, and he sought multiple sources. I think that helps you to start to feel some degree of control when you start to hear similar stories from your primary care doctor, from one or two specialists, which I think is a good idea to visit with.
I usually encourage my patients to get another opinion, at least with a radiation doctor so you really start to hear a lot of opinions, and you start to feel empowered that you’re the one that’s going to make the decision that meets your goals and your needs the most.
I think that’s one of the hardest hurdles to get over. But as a patient recently diagnosed with cancer, you should feel empowered to say, “Hey, I am the one that’s driving. My priorities are the ones that matter. I’m going to try to get all the information I can so I can make the decision that helps me meet my priorities and goals,” because they may be different from your doctor’s. I think that’s important to realize.
The Patient Story: Yeah, no, absolutely. Those are great points to consider. Dr. Weight, one more follow-up here. Speaking of questions and the patient, I know with prostate cancer it’s really about the individual. Jeff — 59 at diagnosis, young, healthy, a Black man.
So I wanted to ask you about what factors to consider for people, too. I know with genomics and mutations, we don’t know if his sister with breast cancer had BRCA 1 or 2 or anything like that. But how important is it to have this kind of information and for patients to be able to ask the right questions?
Treating patients as individuals in medicine
Dr. Christopher Weight: I think we’re still learning how to apply all of these other details, and I think it’s an exciting time. I think we’re going to get to the point where we can really approach individualized medicine.
We still do a lot of population-based medicine, where we take people and we try to put them into the smallest groups possible, but we still make these determinations based on the average Black man or the average white man or the average guy who’s 59 or the average genomic score, for example.
I think we’re still trying to learn and I think there are lots of opportunities, both with genomics, but also with the aid of artificial intelligence and decision trees and prognostic models, where we are going to get even better at helping give patients information that will be more specific to them.
I think that’s exciting, but it’s also frustrating because right now it may feel like a smorgasbord of information that’s just swirling around, and you’re like, “How do I make sense of this? I’ve got to make some decision and move forward.”
I think we’re making progress here, and we continue to get little pieces here and there that give us more information on how to make better decisions for patients as they face this cancer.
Family discussions on risk of prostate cancer
The Patient Story: Absolutely, thank you for that. Jeff, on that note, I know you’ve mentioned you have a younger brother a couple of years younger than you. We know from some statistics that if you have a father or a brother with prostate cancer, you’re more likely to get prostate cancer, to have it.
I would love to hear from you. You said you were going to talk to him. Can you tell us a little bit more about the conversation that you think is important to have?
Jeffrey P.: Probably the most important one is get yourself checked, the quicker the better. But the sooner, the better off you would be.
So if there is presence of cancer, you can get treated quickly and get it taken care of versus waiting till later, because men of color tend not to go to the doctors a lot. And if they do so, it’s always at the ninth hour.
The sooner you can get it checked and get tested or what have you, the better off you will be. That would be my conversation with him or any man of color, to get checked and get checked quicker and timely and more frequently.
The importance of diverse patient voices
The Patient Story: Wonderful. It’s such an important conversation to have.
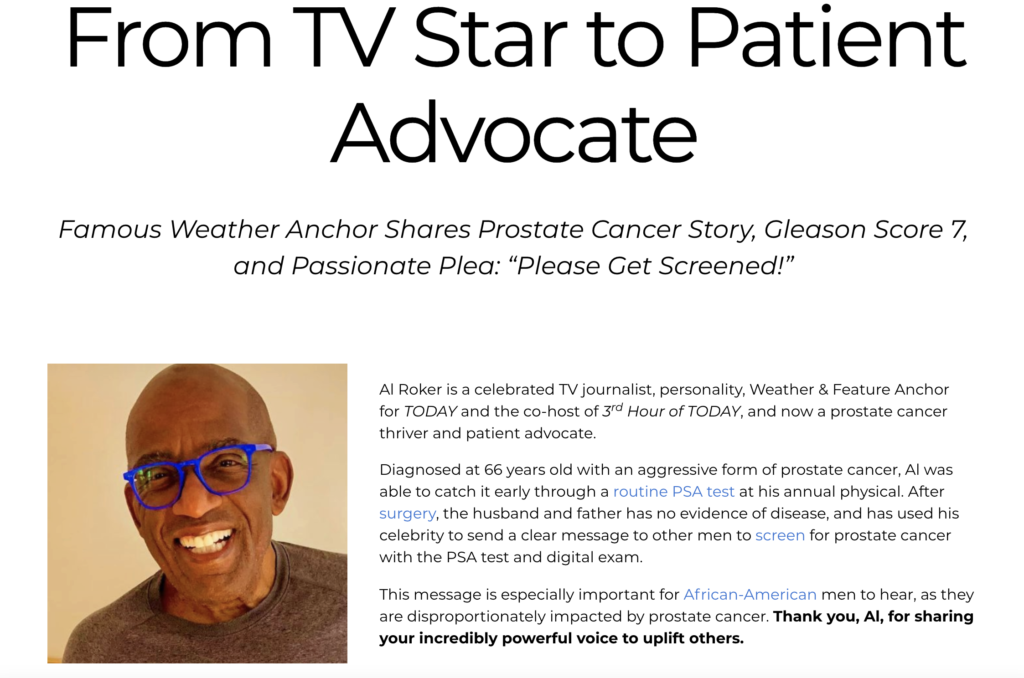
Jeff, just to follow up, my last question to you is — I know you talked about the Al Roker story. I was fortunate enough to talk to him. The importance of seeing people like yourself, especially those maybe in the public eye, but just to get that presence out there.
What’s the importance of having people share their stories, people like you, to make sure that other people are hearing that message of what you were talking about — getting screened earlier and just taking better care of their health?
Jeffrey P.: The awareness, because a lot of times we don’t know what we don’t know. If you have a situation going on inside your body, the more you know about it, the better off you are.
Case in point: a few years ago, when I was going to the Minority Men’s Health Fair, I felt a little guilty because I have health insurance, and I’ve taken up a space for someone who does not have health insurance.
Then after speaking to the director of that, he says, “No, don’t ever feel that way. If they see you are more interested in your health conditions, that would probably inspire others to do the same thing.”
And so I sort of changed my thought process on and off. Now that I’ve been diagnosed with this prostate cancer, more people need to become more aware of their bodies and take an interest in caring for themselves.
I feel like I’ve lived at Cleveland Clinic now, between my primary care physician, my urologist, my cardiologist, this and this and this.
I feel like I’ve got the whole body covered now because of everything that’s happening. But again, the more I know about my body and what’s happening with it, the better I am.
The importance of patient stories
The Patient Story: Oh, I love that. Dr. Weight, I’ll give you the last question. What’s your last message to patients and maybe the doctors, too, about the importance of people sharing their stories and also people listening?
Dr. Christopher Weight: I’m really grateful to Jeff for coming on and sharing your story because it’s not easy to do sometimes, and especially sometimes with prostate cancer, people have sometimes some funny ideas about prostate cancer.
But I think it is so valuable to share stories. I think we’re good at sharing the numbers and sharing the mechanism of treatment and how to navigate through it, but that’s the whole reason we do that is so we can have life.
I think that when people can see Jeff now — he’s gone through his treatment. He’s still smiling. He’s still doing stuff with his dog. He’s still living life. I think that’s really valuable.
Knowing how to negotiate that, it helps people see that there is something up there ahead when maybe all you can see is that diagnosis initially. I’m really grateful, Jeff, for you to be doing this with us and sharing your story.
My message, I think, to doctors would be we need to listen to this aspect of the story because this helps us to understand. This helps us to select which treatment maybe is the best, and we need to really listen to what do our patients value? What do they care about most?
One of the questions I ask is, sometimes as doctors, we get stuck on thinking about how to improve the survival of the patient. We get focused on the survival, especially cancer-specific survival. That’s our wheelhouse. And sometimes we forget. We think about the cancer, and we forget about the patient who has the cancer.
I would just encourage doctors to listen to what the patient is saying, what they value, what they care about, where they want to go. Then we can help choose and help them choose the treatments that help them to meet those goals.
Healthcare disparities
I really also appreciate what Jeff said about some of the disparities in prostate cancer, because they’re marked in the United States, and it’s interesting. We’re beginning to dig into why this is.
We know that African-American men are more likely to get prostate cancer, and when they get it, they’re almost twice as likely to die from it.
There’s been a lot of proposed theories as to why that is, but most of the recent data suggests it’s largely due to non-biological-related things. A lot of people have thought maybe it was all due to different genetics between African-Americans and Caucasians, but the genetics seem to play actually a fairly slim role overall.
It’s more likely due to:
- lower insurance rates among African-Americans
- lower access to care
- lower education about these topics.
I think these kinds of things are really helpful to help us begin to overcome these things. Because if people listen to Jeff and go out and get screened and be active participants in their healthcare, I think we will be able to shrink those discrepancies.
If we do things on a society level, like improve the number of people insured and improve educational outreach, then I think we can start to narrow these discrepancies.
The Patient Story: That is so powerful. Thank you so much, Dr. Weight, for sharing that. I couldn’t agree with you more, as a former patient.
Jeff, I second what Dr. Weight said. You coming on here, sharing your story, so powerful, and I know will make such a big impact. I appreciate that Dr. Weight helped connect us. Thank you both.
NEXT: Al Roker’s Prostate Cancer Story
Prostate Cancer Patient Stories
Jamel Martin, Son of Prostate Cancer Patient
“Take your time. Be patient with the loved one that you are caregiving for and help them embrace life.”
Joseph M., Prostate Cancer
When Joseph was diagnosed with prostate cancer, the news came as a shock and forced him to face questions about his health, future, and faith. He shares how he navigated his diagnosis, chose robotic surgery, and learned to open up to his loved ones about his health.
Rob M., Prostate Cancer, Stage 4
Symptoms: Burning sensation while urinating, erectile dysfunction
Treatments: Surgeries (radical prostatectomy, artificial urinary sphincter to address incontinence, penile prosthesis), radiation therapy (EBRT), hormone therapy (androgen deprivation therapy or ADT)
John B., Prostate Cancer, Gleason 9, Stage 4A
Symptoms: Nocturia (frequent urination at night), weak stream of urine
Treatments: Surgery (prostatectomy), hormone therapy (androgen deprivation therapy), radiation
Eve G., Prostate Cancer, Gleason 9
Symptom: None; elevated PSA levels detected during annual physicals
Treatments: Surgeries (robot-assisted laparoscopic prostatectomy & bilateral orchiectomy), radiation, hormone therapy
Lonnie V., Prostate Cancer, Stage 4
Symptoms: Urination issues, general body pain, severe lower body pain
Treatments: Hormone therapy, targeted therapy (through clinical trial), radiation
Paul G., Prostate Cancer, Gleason 7
Symptom: None; elevated PSA levels
Treatments: Prostatectomy (surgery), radiation, hormone therapy
Tim J., Prostate Cancer, Stage 1
Symptom: None; elevated PSA levels
Treatments: Prostatectomy (surgery)
Mark K., Prostate Cancer, Stage 4
Symptom: Inability to walk
Treatments: Chemotherapy, monthly injection for lungs
Mical R., Prostate Cancer, Stage 2
Symptom: None; elevated PSA level detected at routine physical
Treatment: Radical prostatectomy (surgery)
Jeffrey P., Prostate Cancer, Gleason 7
Symptom: None; routine PSA test, then IsoPSA test
Treatment: Laparoscopic prostatectomy
Theo W., Prostate Cancer, Gleason 7
Symptom: None; elevated PSA level of 72
Treatments: Surgery, radiation
Dennis G., Prostate Cancer, Gleason 9 (Contained)
Symptoms: Urinating more frequently middle of night, slower urine flow
Treatments: Radical prostatectomy (surgery), salvage radiation, hormone therapy (Lupron)
Bruce M., Prostate Cancer, Stage 4A, Gleason 8/9
Symptom: Urination changes
Treatments: Radical prostatectomy (surgery), salvage radiation, hormone therapy (Casodex & Lupron)
Al Roker, Prostate Cancer, Gleason 7+, Aggressive
Symptom: None; elevated PSA level caught at routine physical
Treatment: Radical prostatectomy (surgery)
Steve R., Prostate Cancer, Stage 4, Gleason 6
Symptom: Rising PSA level
Treatments: IMRT (radiation therapy), brachytherapy, surgery, and lutetium-177
Clarence S., Prostate Cancer, Low Gleason Score
Symptom: None; fluctuating PSA levels
Treatment: Radical prostatectomy (surgery)