Learning What I Can Control as a Control Freak: Kim’s Pancreatic Cancer
Kim was fully immersed in family life and in the work she loved as a special education teacher and therapeutic riding instructor when subtle changes in her health began to surface. Abdominal pain, bathroom changes, and a sudden 30-pound weight loss appeared in late 2024. Believing they were related to old ulcer issues, she tried to push through. When the pain became too intense, an ER visit finally revealed something far more serious. Imaging showed a mass in her pancreas, and follow-up tests confirmed it was pancreatic cancer.
Interviewed by: Nikki Murphy
Edited by: Chris Sanchez
Throughout the shock and grief, Kim’s response to her pancreatic cancer diagnosis was shaped by faith, resilience, and a proactive mindset. Treatment began swiftly. Her oncologist recommended an aggressive chemotherapy regimen starting in June 2025, after installing a port for the infusions.

Chemo impacted Kim significantly. She experienced side effects ranging from stomach problems and severe diarrhea to cold sensitivity and platelet fluctuations. Her medical team offered tips to help her manage the symptoms and side effects, like using Imodium or adjusting dietary choices. Emotional support was equally crucial, with family and friends providing strength, especially during the loss of her father shortly after starting chemo.
Kim’s greatest challenge was relinquishing her sense of control and leaning into acceptance. She found joy even in adversity, actively choosing to participate in life and encouraging others to do the same. Kim’s hope has grown as her tumor marker, CA19-9, has dropped from 359.6 to 17. While her tumor is not yet operable, continued therapy aims to shrink it enough for surgical intervention.
Through faith and a community of support, Kim B. continues her pancreatic cancer experience. She says, “Perspective is everything,” and urges other patients to realize that every moment is worth the effort to live and improve, and to look for and focus on what brings joy.
Watch Kim’s video to learn how:
- The right mindset can make a crucial difference when facing a pancreatic cancer diagnosis
- Support from family, medical teams, and faith is vital in navigating cancer and treatment side effects
- Accepting loss of control and finding intentional joy, rather than fleeting happiness, is essential during illness
- Every patient’s path is different; there’s no single way to handle cancer; solutions are personal
- This key truth can help cancer patients: “You don’t have the luxury of being defeated; many people are counting on you to persist and find hope.”
- Name: Kim B.
- Diagnosis:
- Pancreatic Cancer
- Age at Diagnosis:
- 58
- Symptoms:
- Persistent stomach pain
- Abnormal bathroom habits
- Loss of over 30 lbs over a few months
- Treatments:
- Surgery: installation of chemotherapy port
- Chemotherapy
This interview has been edited for clarity and length. This is not medical advice. Please consult with your healthcare provider to make informed treatment decisions.
The views and opinions expressed in this interview do not necessarily reflect those of The Patient Story.
- My name is Kim
- When I first noticed something was wrong
- What happened next
- The moment everything changed
- My treatment plan
- How I’m navigating the side effects of treatment
- I hope surgery will be an option
- The biggest challenge of my diagnosis
- Dealing with my father’s passing in the middle of cancer treatment
- What I want others to know
My name is Kim
I was diagnosed on May 27th, 2025, with pancreatic cancer. I live in Florida.
I am a special education teacher, though not currently. However, I am fighting a different battle at this moment.
I am also a therapeutic riding instructor. I teach individuals with special needs, whether cognitive or physical, how to ride horses, and I absolutely love it.
I would take an arena over a classroom any day for all that it offers. It is a level playing field, and it does not matter how many years it takes a skill to develop. In general education, kids might learn it in a week; individuals with special needs might take six months, but it is just as victorious. That is a big passion of mine.
I love to encourage as best I can, and that is what I have done with this whole opportunity of having cancer. I have just taken it and tried to encourage others, no matter what they are facing. It is your mindset that is going to make the difference.
When I first noticed something was wrong
I started to have pain right next to my belly button, and I thought, “It has got to be an ulcer again,” because I have had them before. Between taking the grandkids to school, bringing them home after school, helping my daughter with various things, keeping up with Craig and his diabetes and insulin… life just keeps going. As the mom, wife, and grandparent, you push yourself. You think, “It will be fine. I’ll just take whatever we have in the medicine chest.”
So it just kept going. The pain just kept going. Of course, I kept saying, “Well, I’ll just do this, or I’ll do that, or I’ll stop eating this, or I’ll start eating that.” Nothing remotely cancer-related entered my mind.
As a side note, I lost 30 pounds with no explanation from about September to December. That plays a part in this as well.
Eventually, on May 14th, after being at my dad’s house (he had broken his hip in March and came out of rehab on the weekend of Mother’s Day), I was helping him and his wife settle in. But my stomach felt off. Everything, including my bathroom habits, changed, and I wondered what the heck was going on. During my weight loss, I said to my mom, “I do not think this is right,” because I was not doing anything out of the ordinary. I was not going to the gym. I changed how I ate, but not enough to lose 30 pounds like it was nothing. I had quit drinking on July 10th, 2024. I just woke up one day and knew I was done; I could not feel that way any longer. I believe fully that was a still, small voice preparing me for what was coming, because this was coming regardless. Quitting drinking at that time helped a lot, because there’s no telling where I would be if I had continued.
I finally came home from my dad’s on May 14th, a Wednesday, it was late, probably about 10:45 p.m. I could not get comfortable, and the pain was near where I think my appendix is. I am not medical; ask me a special ed question, and I am all about it, but medically, I am not the person to ask. I said, “I need to go to the ER.” After nearly 34 years of marriage, of course, we argued about my going. Eventually, my husband drove me to the ER.
They gave me pain medication, and I explained what was going on. Everyone thought it was my appendix, even the doctor. I was not allowed even ice chips because they thought surgery was likely. They did a CT scan, and when the doctor came in to discharge me, she got a chair. I thought, “Oh, please don’t get a chair. That’s not good.” She not only got a chair, she leaned on the bed. I immediately felt uneasy. Then she said, “Your appendix is fine, but we saw a mass on your pancreas.”
I sat for a brief moment. A single tear went down my left cheek; I can feel it even now. I looked at my husband and said, “Alright, what do we do? What’s next?” That was the day I heard the words “mass” and “pancreas” in the same sentence.
What happened next
The day after I was at the ER, I called my primary doctor, who I was not supposed to see until July (just as a new patient for prescription refills and routine things). I spoke to the person answering the phone and explained, “Here’s the deal: I am not due to see the doctor until July, I’m a new patient, but let me tell you what happened last night.” She typed everything in as I told her. A couple of hours later, I received a call from the office asking if I could be there on May 21st. I said, “Absolutely.”
When we went in, the very kind doctor asked what brought me in. I said, “There’s a mass on my pancreas. Honestly, I’m just supposed to be a new patient.” I added, “This is not supposed to be part of the plan.” He replied, “The first thing we’re going to do is order a CA19-9 cancer blood test.” I agreed.
The blood test was done, and everything started moving very quickly. He ordered both a CEA and a CA19-9 test. My CEA result was just about normal, which seemed like good news. The purpose, though, was to determine if cancer was present. Hours later, I received results for the CA19-9; the normal range is 34 or lower. Mine was 359.6. Now we knew cancer was present.
Before I left the doctor’s office on the afternoon of the 21st, he said, “I’m going to have you see an oncologist. Walk up to the front with me; we’re doing a STAT referral.” I said, “Okay.”
During this time, I noticed myself leaning over a lot, putting my hands on my knees. It turns out that was because of the location of my tumor. It was on the superior mesenteric artery, which sits behind the pancreas and supplies the small intestine. I only found this out after a PET scan the surgeon ordered, which clarified everything. The PET scan completely cleared things up for me; now I understood this could really be a big deal.
The moment everything changed
When the doctor was standing at the foot of my bed, I asked him, “Is it cancer?” He answered, “Yes.” My husband was sitting to my right, and I was lying in the bed. I never in a million years thought I would hear the words: “It is cancer.” And it was my cancer. I had never given my pancreas a second thought. In fact, my husband’s pancreas does not even work, and that was the only introduction I ever had to that organ. He is insulin-dependent and deals with everything that comes with that diagnosis.
Before this happened, I went through a period when I learned the difference between gratitude and pride. I used to say, “Oh, I’m so grateful. All I take is a thyroid pill and a water pill.” But that wasn’t gratitude; it was pride. I looked at the handful of medications my husband would take, morning and afternoon, and thought I was fortunate. Then, I heard, “You have cancer.” Honestly, my first response was, “Buckle down. Okay, God. This is uncharted territory. I am going on blind faith. Let’s do it. Whatever comes, I am going to trust it is put in place by You, and that is the route I take.”
I have not looked back. I have never asked, “Why me?” I had only one defeated moment throughout this entire journey I have been on.
My treatment plan
On May 29th, when I sat with my oncologist and he was explaining the plan, he said, “You will start on June 10th. Every other Tuesday after that, you will have chemotherapy, and it is going to be rough. Then you will take home a pump.” I could not wrap my mind around what he meant. “What do you mean, a pump? How does that work? What does it look like?” I found out soon enough that the pump was a shadow I would have with me for 46 hours after treatment. You have to navigate it; you cannot shower with it, but we figured out how to make the tub work.
I sat and listened to my oncologist, who has lots of initials after his name. I realized I was in no position to take over my care. Doing so would have been the biggest mistake I could make. For me, I was in completely uncharted territory; I knew I was in God’s hands. All I could do was trust Him to put the right people in place throughout my treatment plan.
My medical team, I believe, has been handpicked; they have been amazing. I walk into the treatment room, and they tell me where to sit. I sit, they access the port, and I spray it with a ton of lidocaine beforehand because it hurts if you do not.
How I’m navigating the side effects of treatment
The first round of chemotherapy was rough, but I fully believe it was because of everything else I had in my system. I have not thrown up once, and I have mastered how to navigate stomach issues. My medical team told me I could take up to eight Imodium a day; it makes all the difference. It helps me feel much more in control, because when you aren’t, you know it, and it is humbling.
Dealing with stomach issues, there is no way around it. When I heard that eight Imodium a day was allowed due to the diarrhea, I realized I was not alone in this challenge. There was also a cold sensitivity. After treatment, I keep winter gloves by the fridge for when I need to grab something cold.
You simply figure out what works for you. People support and surround you, constantly asking what you need, but honestly, I do not know what I need until the moment arrives. If I feel well enough to do something myself, I do it, because it feels normal. Last week, I said to my husband, “I feel like a science experiment.” Between the head, the pump, and everything else, sometimes you feel like a transformer hooked up to a power station.
Whenever my blood work shows something is low, I research what food I should eat or what I should drink. Pomegranate juice, for the record, is disgusting. Fruit, vegetables, and protein are extremely important right now. I can’t stand the thought of red meat, so I avoid it entirely. If even the thought of something makes my symptoms worse, I do not push it; someday, I might want it again.
Of all the side effects, diarrhea is the worst. There were days—total transparency—when I made it to the tub, started the water, and just let things happen, because nothing else could be done. Sometimes your mind wants one thing, but your body insists on something else.
You adjust, and at some point accept, “This is my life right now.” In this life, there will be trouble. How you handle it matters; it is just a hiccup. These moments of making a mess, of not being able to eat, of being unable to go out, shop, or attend church… the risk is simply too great. Mindset, I cannot tell you, makes all the difference.
I hope surgery will be an option
Recently, I discovered that after a PET scan, my tumor is no longer malignant. However, it is still not small enough to be taken out surgically. Treatment continues in hopes that it will shrink to a size where my surgeon can simply go in and scoop it out, like using a Baskin-Robbins scoop. That is the goal.
I have had seven rounds of chemotherapy. I started in May with a CA19-9 level of 359.6. In July, my level was 17, which is in the normal range. Because of where the tumor is, it could return at any moment. What I have learned is that the tumor is no longer malignant and has been fragmented, much like the asteroids in that old video game where you shoot lasers at flying objects. There is a piece of the tumor lying on the superior mesenteric artery, with other pieces scattered, but nothing is active. My PET scan showed nothing glowing, which I imagine as a fluorescent orange vest, so nothing lit up.
However, stopping treatment now would be a mistake; malignancy could return at any moment. Until my surgeon tells me the tumor is small enough to remove, I will keep going.
The biggest challenge of my diagnosis
The biggest challenges for me have been coming to terms with how much of a control freak I was, how much I needed to be involved, and how much I thought I could do things better. All of that was taken away.
My daughter, who lives down the street, found herself at the receiving end of my constant offers to help: “Well, I’ll do this, I’ll take the kids, I can do that, I can do the other.” The same was true for my husband; I had everyone’s life, even the grandkids’ retirement, all planned out. It was ridiculous.
Apparently, smaller lessons in my life had not taught me that I am not in control. This diagnosis did. I embraced that reality. I have never complained that I have cancer or asked, “Why me?” because those questions do not help; they cannot make it go away.
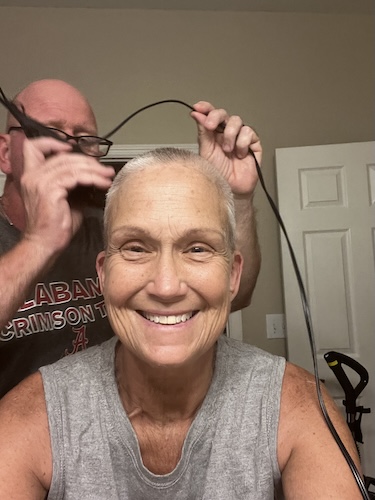
Mentally, I have created videos to keep people updated, and I make sure to laugh in each one. You have to laugh. Laughter releases whatever is going on. I choose joy every day.
Dealing with my father’s passing in the middle of cancer treatment
On March 12th, I got the call that my father had broken his hip. The challenges of his hospitalization and rehab were immense, especially as he expressed his desire to stop treatment and go meet Jesus.
His passing occurred three days after my first chemotherapy session, making it difficult to be present due to my side effects and immune suppression.
My family organized a meaningful graveside funeral, honoring him with cherished keepsakes.
What I want others to know
If I could leave you with one thing, it would be: Go outside as much as you can. Go see the ocean, a lake, watch the sky, notice the colors change. Watching these things reminds you that there are things much bigger than what we are going through.
Perspective is everything. In this great scheme of life, this is just something I have, but I also know I am going to get through it. How I will get through it is not yet written.
I encourage everyone to go see anything big, listen to music, all your favorite tunes. I have even looked up dance lessons on YouTube for movement and activity. I tried line dancing, since when I was a teacher, we would do the Cupid Shuffle with the kids; it teaches left and right, counting, and following directions. We did all kinds of dances like that. Yoga is also possible, even while watching TV. There are so many things you can do.
Just because you have the “C word” in your body does not mean any certificate has been signed. Every moment is worth living, worth making yourself better; physically, spiritually, mentally, emotionally. Do not sell yourself short.

Inspired by Kim's story?
Share your story, too!
More Pancreatic Cancer Stories
Roger R., Pancreatic Cancer, Stage 2
Symptom: None
Treatments: 5FU (folfirinox), Gemzar, NK cell expansion therapy, Dendritic cell expansion therapy, Neoantigen peptide vaccine
Matthew R., Pancreatic Cancer, Stage 4
Symptoms: Dark urine, bone white stool, itching on palms and soles
Treatments: Chemotherapy, surgery
Chris P., Pancreatic Cancer, Stage 4
Symptoms: Significant weight loss, stomach and digestive problems
Treatment: Chemotherapy
Jessica B., Pancreatic Cancer, Stage 1B
Symptoms: Upper abdominal pain, nausea, vomiting
Treatment: Surgery (Pancreaticoduodenectomy or Whipple procedure)
Elise T., Pancreatic Cancer, Stage 4
Symptoms: Severe and persistent back and stomach pain, weight loss, indigestion
Treatments: Chemotherapy, surgery (irreversible electroporation), radiation therapy