Chris’s Stage 4 Pancreatic Cancer Story
Interviewed by: Taylor Scheib
Edited by: Chris Sanchez

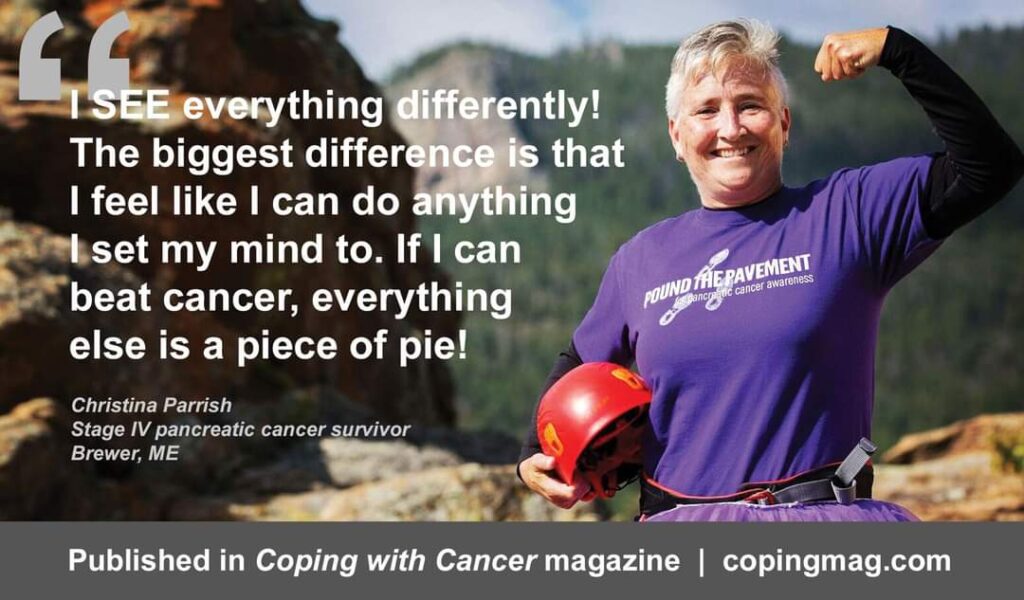
Christina P., or Chris, was diagnosed with stage 4 pancreatic cancer and given 6 months to live. That was 16 years ago.
No less than 5 years prior to her cancer diagnosis, Chris had already been struggling with its initial symptoms — weight loss of as much as 100 lbs and bad stomach issues. Her diagnosis stunned her, especially when she found out that the affected parts of her pancreas and liver could not simply be removed, and when she was told she had just a few months left to live. Additionally, she was dissatisfied with the doctors she initially saw and the treatment options they discussed with her.
But after Chris found the right team for her at the Cancer Treatment Centers of America (which now operates as a nonprofit called City of Hope), she worked with them on her treatment plan and prepared to fight.
Chris’s treatments proved to be intense, especially her intra-arterial chemotherapy regimen. But they were effective. Although she has not been declared NED, she had her last chemotherapy session in December 2011 and was placed on a “chemo holiday” in January 2012 — which is still ongoing.
Chris now helps make sure that other cancer patients, including those who have pancreatic cancer, get not only support but also reassurance, advice, and hope. She sits on the board of the National Pancreatic Cancer Foundation and also founded her own nonprofit, the Purple Iris Foundation. Her foundation works to raise awareness regarding cancer, provide support, and give hope to individuals and families affected by cancer in Maine. She also tells her story to help others like her learn about the importance of faith and hope, even when facing the most dire of situations.
- Name: Chris P.
- Diagnosis:
- Pancreatic Cancer
- Staging:
- Stage 4
- Symptoms:
- Significant weight loss (at least 100 lbs.)
- Stomach and digestive problems
- Treatments:
- Intra-arterial chemotherapy to liver and pancreas (cisplatin, mitomycin, oxaliplatin)
- Intravenous chemotherapy (FUDR, leucovorin)

This interview has been edited for clarity and length. This is not medical advice. Please consult with your healthcare provider to make informed treatment decisions.
The views and opinions expressed in this interview do not necessarily reflect those of The Patient Story.
I pinch myself every day, grateful for every breath I get to take.
I really do not waste my 2nd chances.
Introduction

My name is Christina or Chris.
I am 56 years old, and I am a 16-year stage 4 pancreatic cancer survivor.
Pre-diagnosis
My story started approximately 5 years before I was diagnosed; approximately 2003 to 2008.
I had significant weight loss of I would say at least 70 pounds. I went from 160-170 pounds down to 100 pounds soaking wet.
At that time, the doctors I saw did not see anything wrong with the weight loss, and neither did I. I ran a daycare, so I was always running around after kids.
It was the first time I was skinny, and people were asking me, “Are you okay? You’ve lost a lot of weight. Your clothes are hanging off you!”

I also had a lot of digestive issues; I was popping Tums all the time.
I got tired of having to deal with all that, so I went to my doctor, and they threw me on some Nexium and Prilosec; they did neither scans nor an MRI. They just thought that those medicines would suffice.
Well, fast forward a year, and they had not worked, and I got tired of going to my doctor, so I stopped seeing them, and just started taking Tums again.
A couple years later, I had changed careers, and worked at a call center for a major bank.
At work one day, I felt like I was dying, and when I say that, I mean I could not eat, I could not urinate, I could not poop, and I literally felt like everything was stopping in my body and it got so bad that I started crying to my boss saying, “I have to leave.”
I went and called my doctor and got in the next day and they ordered scans. They said, “Chris, you are never sick.” I replied, “Well, I was, but I just got tired of coming to you because you did not take what was going on seriously.”
Discovery and Diagnosis

My cancer was finally diagnosed in 2008.
I think that was a Thursday or a Friday, and I got the scans. They got me in quick to get them.
The MRI was on a Monday or Tuesday. I had gotten the call to come in, and I said, “Well, can you just give me the results over the phone.”
They told me that I was not going back to work at this point because I just was not feeling good, and when I went in, I did not bring anybody with me because I thought it was just another appointment.
That is when they told me I had a 5-and-a-half-centimeter mass in my pancreas and numerous lesions in the right lobe of my liver.
They did not call it cancer because it was just my PA, but she was crying when we were talking, so she knew the significance of it.
My life flashed before my eyes.
When I asked her if they could just remove it all, she just shook her head and said no. I was like, “Oh. Oh!”
She also mentioned an oncologist, and I said, “Wait a minute, what!” Then I just lost it.
After that, I was in denial until I met with the oncologist. I kept thinking they had the wrong person; it was something stupid, an old sports injury, but reality set in when I saw the oncologist.
Consultation with the Oncologist
Oncology came about 2 weeks later with me advocating.
My appointment was set out a month later, and all the reading I did said that I had 6 months to live if it was a late stage. I did not know the staging at the time, so I had no idea.
When I got there, I went in and met my nurse, and I called her Nurse Ratched. She was not very nice. She asked me if I needed any Ativan, and I told her I was fine. I guess she was trying to prepare me, but I am not sure.
The oncologist comes in, and he was a nice guy. He told me I had stage IV pancreatic cancer. I said, “Oh, ok.”
I just sat there wrapping my head around it, and I did not ask him for my time frame to be alive, but I was told I had 6 months with treatment.
“Woah! I am 40 years old; how can that be? That cannot be. There must be something I can do!”

I was numb at that point, and I said, “Okay, well, I would like to have a second opinion and would like to go to Boston.” I live in Maine, so Boston is the next place down, so to speak.
That is what got “Nurse Ratched” started up. She said that they could do just as well up here, and I said, “I do not feel that this is the place that I need to be to beat this. No offense to you, but we are rural, and I would like to go and get a second opinion.”
With a little convincing, more from me, I successfully got them to schedule me a second opinion. That took me roughly 2 weeks to get into.
I went down to Boston, and I talked to the oncologist via email. She had a clinical trial, but she said I had the wrong type of pancreatic cancer for the clinical trial. I went down anyway for the appointment.
They kept changing where it was and who I was to see, but I finally got in to see my oncologist, just to be told to go home and to do what they told me to do and get my affairs in order. I asked them, “What are you guys not understanding? All you have to do is get me in the ring, and I will fight.”
I went home after that. It was laughable. I had to laugh because I did not want to cry.
Cancer Treatment Centers of America

At that point, I had a list of the top ten cancer facilities in the United States. I had been seeing a commercial for Cancer Treatment Centers of America, and it featured a long-term survivor of stage 4 pancreatic cancer named Peggy Kesler.
I did have some insurance issues which had to be addressed to get out there. Changing insurance is like an act of Congress, literally. You must apply federally to get that changed. The major bank I had worked for, I had some great advocates there, and through them, they found a loophole that I could change my insurance through a life-changing event. That is either getting married, having a child, or moving. My boss said that he would marry me, and I replied, “I love you for that, but no.” I did appreciate him wanting to do that. I just did not feel that somebody else needed to go on this journey; I just could not do it.
My other big boss found a loophole with changing address, so the facility I went to is in northern Chicago, and I took out a P.O. Box there, which changed my address. That gave me the change of insurance that I needed to get to the facility of the Cancer Treatment Centers of America.
That was a whole story in and of itself. They flew me and my mom in, and we got to have our first consult, a 7-day consult. They run you through everything, and everything is under the same roof, so you do not have to go anywhere.
We were treated like rock stars as soon as we walked in. I was not full of faith until I stepped through those doors, and I felt God had His hand on me. I did not speak about faith a whole lot prior to cancer, but I must say that they gave me my faith back, and they gave me a lot of hope.
They did not tell me that I was going to die. They said, “Well, you are young. This is what we are going to do for you. Just let us know.” I replied, “I am here–let’s do it. Let’s start treatment.”
Treatment
Intra-Arterial Chemotherapy
The treatment regimen I had was a clinical trial that was called intra-arterial therapy. It was a clinical trial between MD Anderson and Cancer Treatment Centers of America, and two oncologists worked on it.
My brilliant oncologist was Dr. Robert Levin. I was a good candidate because I was young, and I had not had chemo.
Basically, it is like a health catheter. Only it goes directly to the organs that are impacted by cancer and, for 15 hours, circulates 40 times the amount of chemo through those organs. So, in my case, through my pancreas and liver.
I was strapped down and had sandbags so I could not move and even some morphine. I was able to do one of those treatments each month.

My intra-arterial was cisplatin, mitomycin, and I want to say the third was oxaliplatin or something like that. They were 3 old-school drugs.
With the intra-arterial, I went through at least 8 to 10 blood platelet transfusions. I missed a little bit of chemo. I may have taken 6 weeks off when that happened, but every 3 to 4 weeks, I was out there getting it, and my job was to make sure my body was ready for whatever they did.
My intra-arterial treatment was one of the hardest things I have ever experienced medically before pancreatitis. I knew it was going to be hard, but I did not realize how hard it was.
Now that I look back on it, I think I just did what I had to do to survive, but when I look back on it now, I think, “Wow, just wow!”
They do not even do the intra-arterial anymore because of the toxicity that it can cause, and people can bleed out if they move. You are just as good as dead because the chemo will go into your body, the full dose of it, and that would probably kill you right off the bat.
I did a total of 4; I did one in August, September, October, and November. Then my blood work plummeted: platelets, red blood cells, white blood cells. Everything just tanked.
Intravenous Chemotherapy

So I ended up having to stop the intra-arterial treatment. But I was also doing a drug combo called FUDR, which has leucovorin mixed in with it. That was my regular chemo that I continued with for 3 and a half years.
I started to get neuropathy, and we did not know if it was from residual stuff from the intra-arterial therapy, so they dialed back my FUDR so that I had a better quality of life as well, and the neuropathy came to an end.
I am very grateful for that.
Really, it was just learning to live with the fact that I might have to do chemo for the rest of my life, and it was just preparing myself for that and the chemo; they dialed it back enough that I had 2 to 4 days of being down and then the rest of the month I was out learning to live again.
I would go to concerts. I would go to ball games. People were buying me tickets to things left and right and I was saying, “Let’s do it!”
I would get back from something, and the next morning, I would have to catch a flight out, and I knew I could sleep on the plane.
I knew if I only had a certain amount of time, then I wanted to make sure I utilized my time doing what I really wanted to do and what I loved.
Chemo Holiday
I was put on a chemo holiday in January 2012.
I had my last chemo in December 2011, and when I got in, my oncologist, Dr. Levin, said, “We are not doing chemo this month. We are going to have you go on a chemo holiday.”
They wanted me to “go on holiday” because it would allow my body to kick back in and see what it can do.
Like I said before, I had 4 intra-arterials that were 40 times the amount of chemo, and then I had already had 3 and a half years of chemo every 3 to 4 weeks. I have not ever been able to figure out how much chemo I had, but it was a lot.

I did not want to go on a chemo holiday. They had to talk me into it. I was scared, thinking that the chemo was what was keeping me alive. But in the end I agreed to it.
December 2011 was the last day of my chemotherapy, and I have been on a chemo holiday ever since.
I go back every 3 months for scans. Between my 1st 3-month check and my 2nd one, I started with what I thought was a gallbladder attack. Once, I had to go in locally here in Maine, and what they realized was that my pancreas was shriveled up because of the chemo, and all I had left was the head that they could see.
My liver is doing great because that regenerates, but the pancreas does what it wants when it wants to, and it can’t be forced to do otherwise.
We just work symbiotically together and find the best way through each day.
Uncharted Territory

As I have been getting into treatment, I started looking into what to do if your pancreas stops working.
You cannot live without a pancreas, and I am thinking, what happens if it stops working? What do you do? Nobody can really tell me that, even an endocrinologist.
I am in uncharted territory right now. I have gone to Johns Hopkins and NYU, and had a great gastro doctor at what is now the City of Hope. Basically, they told me that we are in uncharted territory.
I said to them, “Okay, great, how about you study me.”
My whole goal is to get somebody to study why I survived and how my body is acclimating well, where most people would be in bed most days.
Being Positive–Giving Hope
I wanted to share how important it is to be positive.
You have to be positive. You really do. People say it is kind of toxic positivity, but I tell them those are your words; you can be whatever you want.
For me, being positive is how I get through my life, and that is just how I have to be because you do not get second chances. I have lost a lot of friends to pancreatic cancer at all stages.

So, I am going to be that positive person. I am always going to remind you that there is light at the end of the tunnel.
I talk to people all over the world with pancreatic cancer, and I leave them better than when I found them because they are scared and crying, and by the end of the conversation, we are laughing, and they have the tools and the positivity and the hope that they need to face it head-on.
If anybody wants to hear the whole story, I am writing a book. It is just that I have to process things as I write it and a lot of that stuff is pretty heavy, and it is a good way to let it go. I am hopeful that by the middle of next year, I can have it done.
Resources that Helped Her and Which Can Help Others

I used a non-profit called Patient Airlift Services to help get me out there for treatment every time I had an appointment. They did not miss once. Occasionally, they still provide me with vouchers to get out for my checkups.
It is a wonderful organization that helps people and kids with cancer get to where they need to go. I still go out for my checkups out there.
I do have my own non-profit here in Maine, the Purple Iris Foundation, and we can help if you are from there. It was started because of my battle, and it started with me planting hope gardens and Purple Iris because it means faith, hope, courage and wisdom and all of these things I am still gaining today.
So, we wanted a soft name for a not-so-nice thing like cancer, and we have grown to where we now do patient assistance grants, monthly grocery cards, and gas cards for low-income “Mainers.” That way, they can have a leg up on getting to their treatments and eating nutritious food and things of that nature.We do all cancers, but pancreatic cancer is my baby, and I will always be an advocate for that.
Pancreatic cancer has some great financial assistance elsewhere too, like the National Pancreatic Cancer Foundation Project Purple, there is one in Connecticut, and there is the Dawn Hill Fight Foundation.
So, anybody that is out there facing this, there are so many places that you can call with pancreatic cancer, and they can get you in for clinical trials.
I am going to be that positive person.
I am always going to remind you that there is light at the end of the tunnel.
Final Thoughts
Seek out and get yourself second and third opinions. Do not wait until you start treatment to find a second opinion. You need to do it before you start treatment because your first line of treatment is your most important. After all, that is your first line of defense. Always just do your due diligence before actually starting a treatment.
Do not settle. Just do not settle. People do not settle on buying cars; they go to find the best deal. Why not find the best possible treatment facility for your pancreatic cancer?
Find good facilities. Reach out to doctors. You want to have that good team. Treatment needs to be a team approach. And it is also crucial to find a place where you just feel comfortable and where they have your back.

Have backup plans just in case your main plan does not work. Create that game plan, so you know in your head, ok, well, if this does not work, then we have this, this, and that.
Clinical trials are so very vital. I would not be here without a clinical trial.
Nutrition is huge. Keeping your body fueled is such a key to survival.
We are all scared. Cancer is a scary thing. I had to put on my big girl pants and just have faith that I was getting to the right place and that faith has stayed with me for the past 16 years. It took me 1200 miles from my home, but I found a way to make it happen.

Inspired by Chris's story?
Share your story, too!
More Pancreatic Cancer Stories
Roger R., Pancreatic Cancer, Stage 2
Symptom: None
Treatments: 5FU (folfirinox), Gemzar, NK cell expansion therapy, Dendritic cell expansion therapy, Neoantigen peptide vaccine
Matthew R., Pancreatic Cancer, Stage 4
Symptoms: Dark urine, bone white stool, itching on palms and soles
Treatments: Chemotherapy, surgery
Chris P., Pancreatic Cancer, Stage 4
Symptoms: Significant weight loss, stomach and digestive problems
Treatment: Chemotherapy
Jessica B., Pancreatic Cancer, Stage 1B
Symptoms: Upper abdominal pain, nausea, vomiting
Treatment: Surgery (Pancreaticoduodenectomy or Whipple procedure)
Elise T., Pancreatic Cancer, Stage 4
Symptoms: Severe and persistent back and stomach pain, weight loss, indigestion
Treatments: Chemotherapy, surgery (irreversible electroporation), radiation therapy




2 replies on “Chris’s Stage 4 Pancreatic Cancer Story”
Chris, thanks for sharing your remarkable hard journey. I am looking forward to see you publishing your book. Your story gives me the strength and encouragement to fight the late stage pancreatic cancer.
Hey chris, I wanna know about your treatment options . I’m crom India , could you please connect me through e mail if possible . One of my loved ones is struggling now . I just wanna know our options