Cheyann’s Stage 4B Low-Grade Serous Carcinoma Ovarian Cancer Story
Cheyann Shaw became an inspiration for countless people, including ovarian cancer patients and caregivers, after sharing her story of a stage 4B ovarian cancer diagnosis.
In her story, Cheyann details undergoing surgery, chemotherapy, and targeted therapy. She also highlights the importance of patient self-advocacy, how cancer impacted her relationships, including her marriage, and how she approached the issue of fertility preservation.

- Name: Cheyann S.
- Diagnosis:
- Ovarian cancer
- Low-grade serous carcinoma
- Staging: 4B
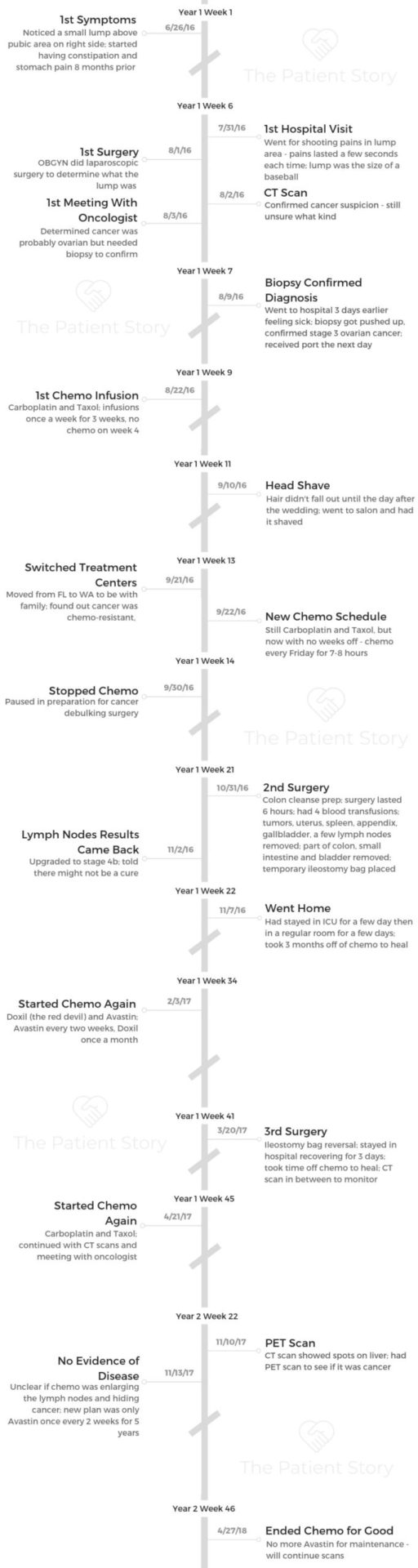
- 1st Symptoms:
- Stomach pain
- Constipation
- Small lump above pubic area on right side
- Treatment:
- Surgery
- Laparoscopic exploratory surgery & biopsy
- Cancer debulking surgery
- Ileostomy bag reversal
- Chemotherapy & Targeted Therapy
- Carboplatin & Taxol: Once a week for 3 weeks, off on week 4
- Doxil & Avastin: Doxil once a month. Avastin once every two weeks
- Surgery
Swing harder, punch harder, and don’t give up. Find the good in this horrible situation. Cancer is crappy. It’s horrible. It’s negative. Why focus on that?
Choose to find something positive and bring joy to your life. At the end of the day, it’s a cancer diagnosis, but it doesn’t take up enough space that it takes away who you are as a person.
Cancer did not take away Cheyann Shaw. I was not going to let it do that. You have a choice. In a world of not having choices, this is one you do have. It’s up to you.
Cheyann Shaw

- Diagnosis
- Treatment Decisions
- 1st-Line Chemotherapy & Surgery
- What were the side effects you experienced from chemo?
- What were the chemotherapy side effects?
- How did you deal with the loss of appetite and weight loss?
- What was the preparation for the cancer debulking surgery?
- How did you feel going into surgery?
- How did the surgery go?
- You woke up in the ICU. What do you remember?
- You got your lymph nodes results back after surgery?
- Did you have any complications in recovery?
- Did you get your ileostomy bag removed, or was it permanent?
- 2nd-Line Chemotherapy & No Evidence of Disease (NED)
- Emotions & Quality of Life
- How did you hair loss affect you emotionally?
- Did you ever wear wigs or hats?
- What was the lowest point you experienced?
- What helped you through the hardest times?
- Can you explain your experience with self-advocacy?
- Do you have advice for anyone who’s nervous about standing up for themselves?
- Was there a talk about fertility?
- How did your cancer affect your relationship with your husband?
- Do you have any advice for other couples going through cancer?
- How was the financial aspect of treatment?
- How important was it for you to have outside help?
- What is your “new normal” after cancer?
- What advice do you have for someone who has just been diagnosed?
This interview has been edited for clarity. This is not medical advice. Please consult with your healthcare provider for treatment decisions.
Diagnosis
What were your first symptoms?
My first symptoms actually started a year before I was diagnosed. I was in and out of the ER about six times with horrible constipation that would lead to stomach cramping.
I would just throw up constantly, I was peeing every 20 minutes, and my husband and I actually thought I was pregnant for a while because every month, my period was missing or irregular.
Finally, in July, a bump appeared on my right side. It was the size of a golf ball on my stomach. I was lying down and noticed it. A few weeks later, it was still there. We had given it until then because we thought it might be a cyst or something since I hadn’t had my period.
A few more weeks later, I started getting shooting pains where that lump was, and it was so bad that I couldn’t walk. It would last for five or six seconds, and then it would go away. From October to July, I was in and out of the hospital with constipation, throwing up, feeling like my appendix burst at one point.
They kept telling me I was just constipated. They did CT scans, but they didn’t see anything, and they weren’t really pushing for more tests because I was 22 or 23 during that time.

How did you get diagnosed?
Finally, I went to the ER again and said, “Listen, something is wrong,” so they did a transvaginal ultrasound. The lump had gotten bigger at this point. It started out about the size of a golf ball, and it was now the size of a baseball.
The ER doctor came back into the room about an hour or two later, and he was smiling from ear to ear. He was like, “You’re fine. It’s probably a non-cancerous tumor or a cyst.” He told me to just see my OB-GYN to be safe.
I knew there was no way this way nothing. I called my doctor that Monday, because I went to the ER on Saturday. I said, “I’m getting married in 30 days or so. If I need surgery, could we schedule that right away?”
She already had all the ER notes and said, ‘Let me call you back in a couple of hours and see what I can do.’
She called back within the hour and asked if I could be at the hospital at 5 o’clock tonight, and we’ll do a laparoscopy and go from there. My OB-GYN was always very quick any time I’ve had an issue, and this was no different.
She wasn’t sure if it was a cyst that needed to be ruptured surgically or a torn muscle. I was huge into fitness at this point, so that was pretty likely.
However, not even five minutes into the surgery, they saw cancer everywhere. She sewed me back up, and they rolled me in for a CT scan. I still had no idea what was going on.
I spent the night in the hospital that night, and the next morning is when I found out I had cancer. My doctor came into the room and told me. They weren’t 100% sure if it was ovarian cancer or if was cancer from somewhere else that had metastasized.

What were the next steps after diagnosis?
The day after that, I met with my oncologist. That’s when everything just started going super quickly. I had a biopsy a few days later because I actually wound up back in the hospital. I was throwing up constantly and couldn’t even keep liquids down, so we called my new oncologist. She said to get me up to the ER so they could get fluids in me.
That was kind of a blessing because I stayed in the hospital for about a week because of that, and they did the biopsy during that time. The biopsy wasn’t supposed to happen until a few weeks later, but it got bumped up, so that’s how we found out it was ovarian cancer.
There is no test to determine if something is ovarian cancer. A Pap smear doesn’t detect it, and it’s not like there’s a mammogram for your ovaries. To know 100% that it’s ovarian cancer, you have to get a biopsy.
Once that came back, my oncologist had a plan, and that was to do chemo every Friday for three weeks, take a week off, and do that for three months.
After those three months, the plan was to do a CT and a PET scan to see if the cancer had shrunk at all. If it hadn’t, then we would continue chemo.
»MORE: Read different experiences of a cancer diagnosis and treatment
The plan for starting chemotherapy
We started chemo right away. My first round was August 22nd because in that week I got my biopsy, they put in my port, too. Then we started chemo.
I was getting married on September 9th, and that was the day I was scheduled for my last infusion for that cycle, but they bumped it up a few days for me.
I had chemo on Tuesday and got married on Friday. I was told that after three weeks, you start to lose your hair, so I was very nervous that I was going to be bald on our wedding day. Thankfully, my hair did not fall out until the next day. The day after the wedding, I was brushing my hair and a clump came out, so I shaved it.
My family and I just didn’t feel comfortable with my doctor in Florida, so 11 days after we got married, I flew back to Seattle, where me, my husband, and all of our family are originally from.
I started getting treatment at University of Washington. I got there on the 20th, saw my new oncologist on the 21st, and started chemo again on the 22nd. It was all just so quick.
What was the biopsy like? How long did the results take?
The biopsy was another surgery. They knocked me out thankfully, but it was really quick. Right where that lump was, they went in with a needle and grabbed some of the tumor tissue.
I think they said it was a 30- to 45-minute surgery. I woke up and had a tiny little patch where they had bandaged me up. I was sore for about a week.
They got those results within a few days. I was supposed to be able to leave fairly soon after that, but my doctor’s fellow or colleague came in and said, “I know you’ve been here for a few days, and you’re ready to go home, but would you be okay staying a couple more hours and getting your port put in?”
I said yes, because otherwise I would’ve had to wait a week, and I was already there.
How long did it take to put the port in?
They put the port in around 3:00 p.m., and we were home by around 8:30 p.m., so it was really quick. I was really sore for a week. I was black and blue all around the port.
I couldn’t work out for a week, so that sucked. In a snap of the finger, my life was getting flipped upside down. It was a lot to process.
Treatment Decisions
Why did you move across the country for treatment?
At the time, it was just my husband and I down here in Florida. His dad and stepmom are here now, but they weren’t yet. His brother and sister-in-law lived down here, but we were all young and in our 20s. We didn’t really have support down here, and my husband works full time.
He’s a real estate agent and is always on the go. I didn’t want to slow down his life because my life was getting slowed down. Even though we’re married, I didn’t want him to put all of his focus on me. We’re young. I wanted him to focus on work.
Not having support down here was a big thing, but the way my doctor made me feel uneasy was the main reason. She made me feel like a dollar sign. Also, I asked her about surgery. I said, “What about doing surgery right away? Wouldn’t that make it easier for the chemo to get anything that’s left?”
I’ll never forget it. She looked at me and said, “That would be a disservice to you.” When she said that, it just sent this chill down my spine, and I was just not comfortable.
After talking to all my family in Washington, we decided that it would be better for all of us to get me to Washington.
My husband couldn’t come for another four or five months because we had a lease we couldn’t break, and all his work was in Florida. I didn’t want him to just stop his life and restart his career.
»MORE: How to be a self-advocate as a patient
What was your first meeting with the new oncologist like?
I met my new doctor, and we sat down for an hour and a half. That’s something I didn’t do with my oncologist in Florida. I instantly felt so much better and more comfortable with her.
She didn’t see me as a dollar sign, a number, or even really a patient. She almost saw me like her own child. I was the youngest patient on the floor for the whole time I was there.
We sat down, and she told me her entire game plan. In that first meeting, she told me more about the cancer than I had heard the entire month I was in Florida.
We found out I was misdiagnosed. I was told I had stage 3, high-grade ovarian cancer when I was in Florida. It’s the more common, easier-to-treat type.
When I was in that meeting, we found out that I actually had low-grade. That’s the more rare type, and it’s completely resistant to chemo.
That was a punch in the gut. I didn’t understand how that was possible because I’m only 23 years old at the time.
She told me if I had come to her first, she would’ve done surgery right away. I told her what the doctor in Florida told me, and she goes, “No. Doing surgery would help with the chemo. It’ll help us centralize the treatment.”

What was your new treatment plan?
Her plan going forward was to keep me on Taxol and carboplatin for about a month to see how the cancer was responding. I was getting infusions every Friday with no weeks off.
Around the beginning of October, the tumor was the size of a cantaloupe. I looked pregnant on the right side. I had excruciating pain in my back, and I had to stay drugged up on painkillers because just one wouldn’t cut it, and I didn’t like that at all.
My doctor then said, “This chemo is not working. We need to do surgery to get as much of this out as we possibly can.” She sat me down and asked me if I was superstitious at all.
I was like, “That’s a weird question, but no. Why?” She told me she had an opening for surgery on Halloween and asked if I would be okay with that. I said, “Uh, yeah! Get this crap out of me as soon as you can!”
I stopped chemo right away because the chemo could make me bleed out or make my body not heal properly from surgery, so I stopped for three weeks. Then, on Halloween, that’s when we did the major cancer debulking surgery.
1st-Line Chemotherapy & Surgery
What were the side effects you experienced from chemo?
I was really lucky. I was super nervous about chemotherapy. On the first day of chemo, I sat in the waiting room and just cried because I was thinking about all the horror stories I’d heard. I had no idea what to expect.
For some reason, I thought I’d be in this chair that looked like a spaceship. Once I had my first round, I was like, “Oh. This isn’t too bad.
»MORE: Read other cancer patient experiences with chemotherapy
What were the chemotherapy side effects?
I have a few family members and family friends who have been through cancer and heard their stories, but I was very fortunate. I never once got sick from chemo, I never threw up from chemo, and I never felt nauseous.
The only side effects I experienced were hair loss and extreme weight loss. Before treatment, I weighed a healthy 130lbs. I had maybe 13% body fat. I was almost all muscle.
After my cancer debulking surgery, I dropped down to 97 pounds. I lost 15 of that during chemo. I had no appetite. I didn’t want to eat. When I did, I would usually have diarrhea. That’s about it, though.

How did you deal with the loss of appetite and weight loss?
I ate pretty much whatever I craved. I did not change my diet for the first five months after being diagnosed until my doctor told me I needed to cool it on the sugar.
I was craving sugar. I was drinking Mountain Dew like crazy, and I hadn’t drunk that in forever. I was eating so many Reese’s Peanut Butter Cups.
My doctor finally said I needed to reel that in. She said the foods I was eating could really deter my treatment or make the cancer grow.
I ended up going vegan for the duration of my treatment, and I’m plant-based now.
I ate a ton of tofu and sweets that didn’t have a ton of sugar and didn’t have dairy. Vegan macaroni and cheese was my jam for a while. Veganism is huge in Seattle, so I would get vegan donuts from a donut shop called Mighty-O.
Every day after treatment, we’d go get donuts. I ate a lot of fish before I went full vegan. One food that never sounded good that I used to love was lasagna. It just never sounded good. It would make my stomach churn to think about it.
In Seattle at the time, marijuana is medical and recreational. My doctor prescribed me my medical card. She said it would help with my appetite. When I got down to 97 pounds, it was really hard to put on any weight. I started taking THC and CBD, and I think that’s what was making me able to eat.
When I would take the pills or smoke, I would eat the whole house. If I had dropped to 95 pounds, I would’ve had to get a feeding tube, so I was willing to try anything. I think that’s why my doctor pushed for it so hard. She didn’t want me to get the tube.
»MORE: CBD, Cancer & Treatment Side Effects
What was the preparation for the cancer debulking surgery?
My surgery was scheduled on Halloween. A few days before the surgery, I had to go get my blood drawn so they could determine my blood type.
With this surgery, there was a chance I’d need to get blood transfusions. There’s a slim chance of that, but they still want to have the blood in the room and ready just in case. They checked all my levels and made sure my body was ready for surgery.
The weekend before surgery, I had to do a full colon cleanse. That was not fun. Every hour, I had to take sips of this nasty substance. I was on a strict liquid diet for the first day.
The second day, I could only drink the cleanse until the afternoon, and then I could also have water. The third day was the same. That’s all I had to do for the surgery prep really.
When I got up to the hospital, they took me back to the operating room and hooked me up to my port, they checked my labs again, and that’s when everyone started coming in.
There was an anesthesiologist that came in to talk to me, my doctor came in, and I had about 20 family members in the waiting room. They all cycled through to say hi before surgery.
The last thing I remember before surgery was getting the cocktail to make me loopy, I could see the lights in the hallway going by, and then I was in the operating room, and they put the mask on me.
How did you feel going into surgery?
Since I was 12, I’ve had around 10 surgeries because I’m an athlete. I wasn’t nervous about going under. I was more nervous about the outcome.
I didn’t know if they were going to be able to get it all or what would happen next. Yes, it was surgery and a big deal, but I was kind of a pro at it at this point.
I just wanted them to be able to save my life more than anything else. I was bubbly, happy, and ready to go.
To cope with things, I laugh and dance and tell jokes. I used my humor to cope with my nervousness.
How did the surgery go?
Apparently, what happened was when they got into the operating room and opened me up, the cancer was worse than they thought. On my CT scans, it looked like I just had one massive tumor, but I had five tumors. The big one was hiding the four others behind it. One was so far pushed into my back, they didn’t know if they were going to get that out without severe nerve damage.
The doctor had to call out to my husband in the waiting room because it was an emergency. I was bleeding out a lot. I had four blood transfusions. The big problem was that they were going to have to insert an ileostomy bag because the big tumor was connected to my colon and my small intestine. They weren’t sure if it was going to be permanent or not, but it had to be done.
She told my husband, ‘I’m not really asking your permission. I’m telling you what we’re doing.’
I had no idea that was a possibility.
I ended up having a full hysterectomy, I had part of my bladder removed, part of my colon and small intestine were removed, and I had some lymph nodes removed so they could test them. My spleen, appendix, and gallbladder came out. The five tumors were removed. The biggest one was actually the size of a beach ball.
My doctor said the tumor sat in my pelvis. The pelvis acts like a fish bowl, so the tumor just sat there and started spilling out over the top. She said my bladder was up under my ribcage.
I had organs all over the place. That’s why I had been so constipated. That tumor was pinching my intestines and colon.

You woke up in the ICU. What do you remember?
I remember seeing about 20 different white coats. At University of Washington, they have students because they’re a teaching hospital. I was still pretty high from the anesthesia, but I heard bits and pieces.
I heard something about the ileostomy bag, so I looked down, and I was like, “What is that?” They said, “Well, that’s how you’re going to use the bathroom.”
It looked like a brain because my small intestine was on the outside of my skin. That’s how I would go to the bathroom, so I’d literally just be pooping in a bag. The intestine would move. It was kind of fascinating to watch, but it was really shocking.
My doctor said, ‘We got all the cancer we could physically see.’
I threw my arms up in the air, and I kept saying, ‘Woohoo!’
She also said they sent a few lymph nodes off to be tested. I was in the ICU for four or five days. I have a 13-inch scar because they literally had to split me wide open to get everything. They almost had to bring the scar right in between my boobs because that’s how big the tumor was.
You got your lymph nodes results back after surgery?
The third day after surgery is when I had to learn how to walk and sit in a chair again. I was sitting in this chair, and my doctor walked in. I knew something wasn’t right. She’s usually super bubbly, but this time, she walked in with a straight face and her head down a little.
She sat next to me and said, “We got your lymph nodes results back, and unfortunately you’re now stage 4. You have cancer in some of your lymph nodes, and we can’t surgically remove them. Thankfully, it’s not in your bloodstream.”
That’s when she told me basically that I was terminal. She didn’t say those words, but she said there might not be a chance of a cure. She did say that she would fight it with everything she could, though.
I looked at her. I was kind of shocked, but I asked her, ‘Do you believe in God?’ She said, ‘Well, I believe in science.’ I said, ‘That’s okay, but I believe in God, and I’m going to be okay. We’re going to beat this thing.’
She rubbed my back and said, ‘I love your optimism, but I need you to know the severity.’ I told her I knew there might be a chance I wouldn’t make it, but I was going to beat it anyway.
She left, and I was tired, so I laid back down. My husband had flown back to Florida. He came in town for my surgery, but he had to leave the next day. My mom was with me the whole time.
When I was sleeping, my doctor walked her down the hall and told her, “You should prepare yourself because we don’t know if she’ll be here after Christmas.” I never knew that until I was done with chemo.
Did you have any complications in recovery?
After four or five days post-op in the ICU, I was moved up to the regular floor and being watched and monitored and all that. They gave me the go-ahead to go home, and I was off chemo for about three months just to give my body time to heal.
During those three months, I was admitted to the hospital for a week. I had a block in my stomach because of the ileostomy bag. Sometimes, if a block like that is severe enough, you have to get surgery.
Luckily, I didn’t have to, but it took about a week for it to work itself out. I couldn’t eat without it coming right back up, so I was on fluids constantly and peeing like a crazy person.
Once I was released, I didn’t have any issues until a few months after that, right before I was about to start chemo again. That’s when I was dealing with all the weight loss.
I was 97 pounds, and my doctor told me I had to get a feeding tube if I lost two more pounds. That’s when I started the medical marijuana, and I wasn’t able to put on much weight at all, but I wasn’t losing weight either.
Did you get your ileostomy bag removed, or was it permanent?
My ileostomy bag was leaking stomach acid underneath the sticker that was supposed to keep it in place, and it was eating my skin. It was raw and it hurt, so my doctor scheduled a colon check to make sure I could get my ileostomy bag reversed.
That was some type of test. I will never forget that. I had to go to the X-ray machine, and they put a tube in my rear. They flushed a saline solution up there that would light up. I had to stay in all these awkward positions for twenty minutes while I was getting pictures taken.
There was a live feed that I was watching, and I could see the solution working its way through my insides. They did that to make sure that where they fused everything together was completely healed, because if not, they couldn’t reverse it.
If liquid went through it, that meant that poop would also be able to go through it, and I could die from being septic. We did the ileostomy bag reversal on March 20th..
2nd-Line Chemotherapy & No Evidence of Disease (NED)
What was the 2nd chemotherapy regimen?
I started a whole new regimen because the Taxol and carboplatin was not working. My doctor said, “We’re going to give you the most intense chemo we can think of.” Its nickname is “The Red Devil” because it’s actually red. It looks like Gatorade. It can change your pee.
Doxil and Avastin were gonna be my new drugs. Doxil was once a month, and Avastin was every week. I did Doxil and Avastin for about six months.
This regimen was really intense. There was a whole new ruleset with Doxil. I would get that once a month. The first week of the month, I would get both drugs, so we would be there for seven hours at the hospital from start to finish.
It was a long chemo day, but then the week after that, it would just be Avastin for three weeks. When the new month started, I would get both again.
They don’t call Doxil ‘The Red Devil’ for nothing.

What were the Doxil and Avastin side effects?
You can get hand and foot blisters, so for five days after the infusion, you can’t get too hot, you have to take lukewarm showers, and you can’t put your hands or feet in hot water. You have to wear loose-fitting clothes, and you don’t want to sweat. It can destroy your skin.
There was one time I was setting my elbow down on a leather couch, and my skin was just gone. My skin was really fragile. That was rough. I never got hand and foot blisters, but I did get blisters in my mouth, and specifically I had a blister the length of my tongue.
For a week, I couldn’t talk, and I could barely eat. The acid from citrus fruits would kill my mouth, so I couldn’t have anything like that. That was the worst side effect I had from that besides the weight loss.
It also made me tired, but not as tired as the Taxol or carboplatin. At chemo, I had to put ice bags on my hands and feet, so it was freezing. Not to mention that this was in winter in Seattle, where it’s already cold.
Avastin was super simple. I had no side effects from that. The infusions lasted around 30 minutes. It’s actually a maintenance chemo, so it’s supposed to stop the growth and spread of any tumors and keep the tumors away.
Those days, I was there maybe two hours because I would meet with my doctor or her fellow, get my blood drawn, and then get chemo for 30 minutes.
What this new regimen effective?
For every scan, they noticed that it wasn’t necessarily shrinking the lymph nodes. I only had cancer isolated to three or four lymph nodes at this point.
They weren’t shrinking, but they were stable. After month six of being on this regimen, I had a scan, and that’s when they saw some stuff appear on my liver. There were two or three black spots.
My doctor came in and had the same look she did when she told me I was terminal. My mom, dad ,and husband were all there. She said, “The lymph nodes are stable. Your CA 125 is doing really well. You do have some new spots on your liver, though, and we’re not sure if it’s cancer or if it metastasized, but we need to move quickly.”

I instantly started crying. I was finally putting on a little bit of weight, and I had been doing so well. I felt like myself other than not being the weight I need to be.
I didn’t understand. Two months before this, everything had been fine. I just didn’t understand.
She gave my family and I a few minutes to process, and when she came back in, she scheduled a PET scan. She said, “You’ll get basically a radioactive sugar injected into you, and if there’s cancer in your body, it’ll light up.”
How was the PET scan?
Three days later or so, I had the PET scan. I was so nervous. We lived about 45 minutes from Seattle, and the car rides were usually fun.
We would listen to music and talk. This time, it was just silent and somber. I was preparing myself for the worst.
When we got there, I felt some peace. I told myself I was going to be okay.
They hooked me up to my port and put the radioactive sugar in me. When you get it, you have to lay on the bed completely still for like 45 minutes.
I asked them to play some Christian music because it calms me down, and that was the most peaceful I had felt in a long time. I went through the machine a couple of times, and that was it. My doctor called me to set up the appointment to talk about the results a few days later.
What were the results of your PET scan?
During that appointment, my doctor sat my husband and I down and said, “Well, the good news is it’s not cancer on your liver. It hasn’t metastasized. It looks like it’s scarring and fatty tissue on the liver. We’ll monitor it. We know about it now, and we know it’s not cancer. We also know you don’t have any more cancer in your lymph nodes.”
We were shocked. She said, “Your lymph nodes did not light up whatsoever.” At this time, they had been stable, but they weren’t shrinking, so she said I was in a gray area.
The plan going forward was to take me off of Doxil and keep me on Avastin for pretty much the rest of my life, with getting scans every month for the first three months.
When did you find out you had no evidence of disease (NED)?
I got a call from my doctor on November 13th the next year. She said they had looked over everything. They looked over all my scans, CA125, and everything.
She said, ‘You have no evidence of disease. There is no cancer in your body.’
I was like, ‘What?! Woohoo!’ I was so excited that I hung up the phone, and we started jumping up and down and dancing.
We ended up going to dinner that night. It was a great day and great feeling. I remember seeing all my friends on social media celebrate their no evidence of disease.
One friend celebrated hers, and I was so happy for her, but I was also immensely jealous of her. I thought, “I’ve been fighting longer than her, and I was diagnosed before her, so how is this fair?” I was really upset, but I knew I was going to be there one day.
When my doctor told me, I looked back to me laying in my bed wondering when my time was going to come, and I was just so happy. It was super cool. I’ll never forget what I was doing, where I was, what I was wearing, or any of that when I got the call. It was just a great day.
What’s your ongoing treatment look like now?
I’m no longer on chemo. I ended the Avastin on April 27, 2018, because I didn’t feel like I needed it.
I had six scans and CA 125s in a row that were all really good. The lymph nodes were actually starting to shrink back to normal size over time.
I asked if I could be done with chemo, and my doctor said, “You don’t have to be on Avastin if you don’t want to,” so I stopped that.
Now, I meet with my doctor here out in Tampa, where we moved. I meet with her every three months, and I get CT scans every six months.
Emotions & Quality of Life
How did you hair loss affect you emotionally?
It was kind of like a bit of relief. I thought, “Well, at least it didn’t happen yesterday when I was getting my hair done.”
When I was told I might lose my hair for my wedding, I went and bought some wigs. I didn’t want to be bald on my wedding day, so I had mentally prepared for needing to wear a wig.
Looking back, had my hair fallen out before the wedding, I don’t think I actually would’ve worn the wig. I think I would’ve gone bald because once I was bald, it was kind of nice.
When it came out, I just felt like I wanted to shave it. I didn’t want to sit around and wait for my hair to fall out. I wanted to have control in a situation where I had zero control. This was the one area I could have some sort of control.
We went to a hair salon that day, and it was super emotional. I cried in the chair the whole time. I was terrified to see what my head looks like bald. I didn’t know if it was going to be misshapen or not. I also have a mole on my head that I’ve always been really self-conscious about. I wasn’t excited about the idea of everyone seeing that.

Once I got home, I realized my head is extremely round and the mole wasn’t that noticeable. The way I coped with everything was I named my mole. I had done the same with my port and my tumor. It made me feel more comfortable and confident.
Over time, I actually enjoyed being bald. I never had to do my hair. Getting ready was super quick and easy. I just knew it was something I couldn’t control, and I needed to accept it and learn to love myself in a new way.
Even when I was first diagnosed, there was no way I was going to sit there and feel sorry for myself. I told myself, ‘I’m gonna get up. I’m gonna fight this thing. I’m not going to lose.’ I always said I would win.
Looking at things in a positive way really helped me, so that’s what I did with my bald head. I would say, ‘Yeah, this sucks, but at least I don’t have to wash my hair. At least I don’t have to blow dry it. At least I can get ready in five minutes.’ I always tried to put a positive spin on it.
»MORE: Dealing with hair loss during cancer treatment
Did you ever wear wigs or hats?
I had a few wigs. One was super long and brown. My natural hair color is platinum blonde, and I’ve always had platinum blonde hair, so I wanted to try something different. I had another one that was about shoulder length. I wore each wig once, but I just felt comfortable with my bald head.
I always wore beanies, too, because Washington is really pretty cold. You don’t know how warm your hair is until it’s not there anymore. But I actually loved being bald. I don’t know why, but maybe because it made me look at me.
I didn’t see my long, beautiful blonde hair or my muscles I had from working out when I looked in the mirror anymore.
I saw me. I saw me stripped of everything I had worked for. I saw me at my most vulnerable, and that’s where I learned to love myself the most.

What was the lowest point you experienced?
That would be November, about a month after my cancer debulking surgery. I was 97 pounds, no hair, and I had an ileostomy bag.
I took a picture of me standing to the side. I had nothing. I sent it to my husband alongside a picture of me at my fittest. I said, “I can’t believe I lost everything I’ve worked for.”
I remember not recognizing myself in the mirror. That same night after beating myself down, that’s when I realized it wasn’t healthy for me to rip myself apart because I had no control over the situation. What I did have control over was how I thought of myself and my situation.
My weakest point was also when I found my strength.

What helped you through the hardest times?
It was a combination of a lot of stuff. After I posted that picture that I sent my husband on Instagram, overnight my story went viral. I woke up the next morning with like 10 times the followers. My picture had thousands of likes and comments. The support from people all over the world I’ve never met, from my friends and from my family — that was crucial.
My husband always told me how beautiful I was. He never acted like I had lost anything. He was so supportive.
My faith had the biggest impact on me. I was always kind of a religious person, but I was never super into it. My faith gave me a ton of the strength that I needed.
I also have just been a tougher person. I haven’t had the easiest life and the easiest upbringing, but I feel like everything I’ve gone through shaped me to be the person I was when I was battling [cancer]. I’ve always been the type of person who finds the good and the humor in everything.
I had a medical team that cared so deeply about me. My doctor had two days off in a row when I was in the ICU, but she came to check on me every day to see how I was doing. When you have an oncology team that’s that devoted to you, it really makes you feel like you can beat anything. I truly believe it was a combination of everything.
Can you explain your experience with self-advocacy?
When I was first diagnosed and even prior to being diagnosed, I had to push for myself.
Each time I went to the ER, I would fight. Come to find out, I did have images on my CT scan that showed I had cancer, but because of my age, it was so rare.
When I was in Florida, I really had to push for myself. That’s the main reason I went to Washington. We just didn’t feel comfortable with my first oncologist.
Her treatment plan didn’t make sense to me. I even thought surgery first made more sense, and I said so, and that’s when she told me that would be a disservice to me. That was it for me.
When I got to Washington, I never had to advocate for myself. My doctor would sit down with me and answer questions and tell me the truth. She told me everything I needed to know and more.
Do you have advice for anyone who’s nervous about standing up for themselves?
Just stand up for yourself. I don’t like confrontation, but at the end of the day, you’re the only one who knows 100% when something is off in your body. Doctors can go to all the school they want to, but they don’t know how you’re feeling. You have to tell them if something is up.
If you’re nervous to push, you can always send your concerns in an email or leave a message at the desk for them. Always get second, third, and fourth opinions. You know your body better than anyone else.
If any symptom lasts longer than two weeks, you need to go get checked. Do not be afraid to get checked. It literally could save your life. That could be the difference between you being here or not.
»MORE: How to be a self-advocate as a patient
Was there a talk about fertility?
Before I was diagnosed, my husband and I were planning on starting a family right after we got married. Unfortunately, with ovarian cancer, I couldn’t. Before I had my huge debulking surgery, I expressed to my doctor that we wanted to have kids. I asked what the chances were.
She said she could see how bad the cancer was when she got in there and maybe try to save an ovary, but there was a high chance of it spreading if we did that. I told her I just wanted to get rid of the cancer and both ovaries, but then asked if we could save eggs before we do the surgery.
We scheduled with a fertility specialist, and she said the chances of me being able to save eggs were very slim, but they would try. During the cancer debulking surgery, my doctor retrieved some eggs and gave them to her, but both ovaries were saturated with cancer, and all the eggs were covered.
I can’t have kids. It’s still a very hard subject, but now I can at least talk about it. It took me about two years to grieve the process. My counselor told me it was important that I grieve because it’s like I lost kids in a sense.
We can’t have kids in the way that a lot of people can. We looked into adoption, but with that, you have to be five years cancer-free. I totally get that, but it still sucks. We want to do an egg donor and surrogate first. We’re in the process of looking for an egg bank very soon. We’ll eventually have kids — just not the normal way.
In the beginning, the surrogacy thing kind of bothered me because I thought, “Well, is this child even going to be mine?” After speaking with some people about it, I felt so much better. They said, “When you see that baby, you feel like that child is absolutely yours.”
I get super emotional when it comes to this because as a woman, my job is to help create a life. That was just ripped from me. I had to come to terms with it, though, because it’s not something I can change.
Talking to other people about their experiences really helped. My biggest advice is to seek help. Talk to somebody. When I started going to a counselor, I started feeling so much better.
You need to talk about it. I lost the ability to have a child, so I needed to grieve. For a long time, I felt like it was my fault, and I know it’s not now.
»MORE: Fertility preservation and cancer treatment
How did your cancer affect your relationship with your husband?
It was tough. We were apart for the first five or six months. He came down in March of 2017, right before my bag reversal. We had a ton of FaceTime dates and a ton of phone calls. At the same time, I think it made our relationship stronger.
I know I wanted my husband to be there for me and next to me. He wasn’t physically there, but he was always there for me. I would call him at all hours of the night, and he would let me talk or cry or do whatever I needed to do.
Once he got to Washington, that’s when our relationship got so much stronger. At one point, I was in a pull-up after the ileostomy bag reversal because I couldn’t hold my own fluids. I had a baby explosion like when kids have the diarrhea up their back. He had to help me clean myself.
Going through some of those crazy scenarios, like being so young and needing my husband to clean poop off my back, that brought us so much closer.
There were times it was so tough. Being apart and not seeing each other was really hard. We’re with each other pretty much 24/7 because we work together. He’s a real estate agent, and I help him with all that. I’m the photographer for all his listings.
We were together 24/7, so then not seeing each other except in a phone screen for six months was tough. It was our new normal for the moment, and we did the best we could with what we had.
»MORE: 3 Things To Remember If Your Spouse Is Diagnosed With Cancer


Do you have any advice for other couples going through cancer?
We talked a lot. We were very open and honest with each other. There were times I wouldn’t necessarily talk to him all that much for a week. There were times I just wasn’t able to get on the phone.
We would text, but sometimes I just couldn’t make it to the phone. He would say, “It sucks we haven’t talked all week. Did I do something wrong? What’s going on?”
He was very honest with me when he felt like I was pulling away. That’s when I’d tell him I had just been really tired or in a weird mood and didn’t feel like talking.
That’s when our communication got extremely strong. My advice is to be patient with each other. Don’t push each other away.
At times, I would push him away because I didn’t know what was going to happen to me.
I didn’t want him to not have me, so I would push him away to prepare him, but that did more harm. It caused more tension, and that’s one thing you don’t need when you’re going through cancer.
Just be there for each other. Be honest with each other. Realize that your life is going to change, and you have to be open to the changes and find your new normal.
That’s exactly what we had to do. We had to find a new daily routine. There were times I couldn’t leave the house, and that was our life, so we went with it until it wasn’t anymore.
You have to go with the flow and not stress too much when things aren’t going the way you want them to.
How was the financial aspect of treatment?
Before we got married, I had insurance through my dad. He’s a government worker. My mom works with insurance, so she was able to get it to where I still had my dad’s coverage even after we were married.
My husband and I also had insurance. When I got to Washington, my dad’s insurance dropped and we just had ours. It covered pretty decent bills, but being a young couple, those bills come in pretty quickly.
I was very fortunate to have a really big support system on social media and through family and friends. What we did was create [a] “#CheyStrong” shirt. That was my slogan. We sold the shirts for $20.
We raised a lot of money. It helped with paying the bills and getting us to and from chemo. We had a lot of support.
How important was it for you to have outside help?
When I moved to Washington, I moved in with my mom and her husband. Her job was super cool and let her work from home so she could take care of me. For about five months, I lived with my mom.
After my husband moved, we stayed about three more weeks, and then we moved into our own apartment. My dad would take me to chemo when he didn’t have to work. He’s a corrections officer, so his hours were really crazy. We had so much family support.
It was extremely important for me to have that. That was really why I moved to Seattle. My husband and I had no idea how to deal with something like an ileostomy bag. My mom works with insurance but also with assisted living, so she knew her way around some of that stuff a lot better than we did.
It was important for me, but it was even more important for my husband to know that I was taken care of because he couldn’t be there for the first several months.
What is your “new normal” after cancer?
My new normal is living every single day to the fullest. That doesn’t mean I don’t have bad days. I do still, but when I have a bad day, I don’t wallow in it too long. I don’t set up camp in a bad day like I used to.
Other than after effects of cancer, my life has gone back to normal. I still have some stomach issues, so I’ve had to change the way I eat. I have to be very particular with what I put in my body.
I don’t eat a ton of sugar like I used to anymore. I’ll still have it sometimes because I believe in moderation, but I’m not downing it like I used to.
It’s just about being more aware of my own body. When I feel like something is off, I’m instantly paying attention to it and calling a doctor if I need to.
I live in the moment more. I used to live every single day and let it go by. Now, I’m living life and taking time to smell the roses, no matter how corny that sounds.
I’m stopping to enjoy the sunset and slowing down. I’m noticing the beauty all around me and focusing on the light.

There’s a lot of darkness in this world. Why look for it? Why not look for the good things in life? When you look for the light, your world becomes so much brighter.
I don’t let the bumps in the road get me down. I’m just living every day, as well as dealing with post-cancer stuff like the stomach issues and not being able to have kids.
What advice do you have for someone who has just been diagnosed?
Your life may be flipped upside down, but you have a choice in all of this. You can either choose to look at this as a negative and let it destroy your life, or you can look at this from a different perspective and say, “This sucks, but I can do this. I’m not going to lay down. If I get knocked down, I’m going to get up every time.”
Swing harder, punch harder, and don’t give up. Find the good in this horrible situation. Cancer is crappy. It’s horrible. It’s negative. Why focus on that? Choose to find something positive and bring joy to your life.
At the end of the day, it’s a cancer diagnosis, but it doesn’t take up enough space that it takes away who you are as a person.
Cancer did not take away Cheyann Shaw. I was not going to let it do that. You have a choice. In a world of not having choices, this is one you do have. It’s up to you.

Inspired by Cheyann's story?
Share your story, too!
Ovarian Cancer, Low Grade Serous Stories
Maurissa M., Low-Grade Serous Ovarian Cancer
Symptoms: Pressure on bladder, throbbing pain, could feel growth on right side of abdominal area
Treatments: 5 surgeries (official diagnosis after 3rd)
...
Alisa M., Low-Grade Serous Ovarian Cancer
Symptoms: Occasional rectal pain, acid reflux, bloating, night sweats
Treatments: Debulking surgeries, chemotherapy, immunotherapy
...
Cheyann S., Low-Grade Serous Ovarian Cancer, Stage 4B
Symptoms: Stomach pain, constipation, lump on the right side above pubic area
Treatments: Cancer debulking surgery, chemotherapy (carboplatin & Taxol, then Doxil & Avastin)
...
Kacie K., Low-Grade Serous Ovarian Cancer, Stage 3
Symptoms: Pelvic pain, sharp pains during menstrual periods, Inability to urinate normally, bleeding
Treatments: Surgeries (full hysterectomy, ostomy surgery, ostomy reversal surgery), chemotherapy
...




2 replies on “Cheyann’s Stage 4B Low-Grade Serous Carcinoma Ovarian Cancer Story”
My story is amazingly similar. Low grade 3C.
I’m on Avastin now. 9/2020 was my initial diagnosis.
I was originally diagnosed as high grade.
It was only with a second opinion that I learned about low grade cancer.
My new care team saved my life. They are amazing.
I keep positive. I love my life and look forward to one day retiring with my hubby.
Age 56
Unfortunately, Cheyann Shaw succumbed to her illness yesterday. The world today is a much lonelier place without her but we are grateful for having had the chance to see such an inspiration on social media. RIP Cheyann Shaw.