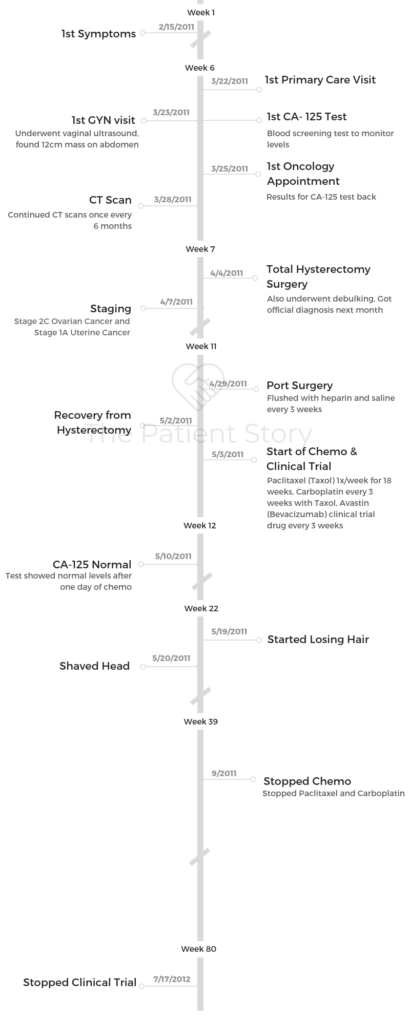
Heather’s Stage 2C Epithelial Ovarian Cancer & Stage 1A Uterine Cancer Story
Heather shares her story of stage 2C ovarian cancer, undergoing chemo, surgery, and a clinical trial with Avastin. She would eventually be diagnosed with stage 1A uterine cancer, which was removed by surgery.
As a former clinical trial program manager, she shares more on the process and what it entails. Heather also highlights important topics like how she paid for treatment, cancer’s impact on her sexual health, and how she parented with cancer. Thanks for sharing your story, Heather!

- Name: Heather M.
- Diagnosis:
- Epithelial ovarian cancer
- Stage 2
- Uterine cancer
- Stage 1A
- Epithelial ovarian cancer
- Age at Diagnosis: 40
- 1st Symptoms:
- Persistent bloating
- Pinching pain in right side of abdomen
- Pressure on bladder
- Pain during sexual intercourse
- How diagnosis happened:
- Went to doctor for separate issue (hand injury)
- Pelvic exam performed after telling doctor of symptoms
- Vaginal ultrasound shows 12-centimeter “complex” mass on right side of abdomen
- CT scan confirms mass
- Note: The official, full diagnosis with solid tumors cancer like ovarian require the surgical removal of the mass. Preliminary diagnoses are usually made before then.
- Treatment:
- Surgery (total hysterectomy and debulking)
- Chemotherapy
- Paclitaxel (Taxol) once a week for 18 weeks
- Carboplatin infused every 3 weeks (with the Taxol)
- Clinical trial
- Avastin (Bevacizumab) every 3 weeks
Those things that you beat into your brain as a mantra is extremely powerful medicine that you can do yourself. It’s setting you up to succeed, and that’s what we wanna do.
The doctors are fighting the fight with the medicines and all that, and you are fighting the good fight with your emotional medicines. Do try to do something like that, because I really felt that that helped me.
Heather M.

- Pre-Diagnosis
- What were your first symptoms?
- What was the catalyst that got you to go to the doctor?
- Describe the first doctor’s appointment
- What happened at the vaginal ultrasound?
- What procedures and tests came next?
- Describe the first visit to the oncologist
- You started having difficulty urinating
- What did they find at the ER?
- Tests & Scans
- Treatment Decisions
- How did you decide where to go for treatment?
- What did you like about going to a smaller treatment center?
- Did you get a second opinion?
- Did you research your cancer and treatment before starting?
- What’s your advice to patients and caregivers about to start treatment?
- Your doctor had great bedside manners
- Surgery
- How was the surgery prep?
- What do you remember about waking up from surgery?
- Describe the moment you heard that first official cancer diagnosis
- How was laparoscopic surgery described to you?
- How did you cope with the post-surgery pain?
- How long did it take to start recovering?
- Were there any post-surgery complications?
- The mental healing took longer than the physical recovery
- Do you recall the moment you got the staging?
- How did your loved ones react to your diagnosis?
- The debulking happened after. What is that?
- Chemotherapy & Clinical Trial (Concurrent)
- What was the decision-making to pursue chemotherapy?
- What was your first impression of the chemotherapy process?
- Describe getting the port(acath)
- Did you like the port?
- Describe your chemo regimen
- Describe what happened during and after the infusions
- You brought a “chemo buddy”
- You underwent your first clinical trial at the same time
- How long did it take to get the infusions?
- What helped you get through the infusions?
- Tip: tell your medical team about all side effects
- List of chemo side effects & what helped with them
- When did your hair start to fall?
- What helped most with styling your head?
- What helped with the hair loss?
- Were there side effects to the clinical trial (Avastin)?
- Getting into a Clinical Trial
- Work & Finances
- Support & Relationships
- Did you have to self-advocate through treatment?
- How did you talk to your kids about the cancer?
- You had to be more careful with germs
- Did you have to get outside help with the kids during this time?
- How did the cancer impact your relationship with your husband?
- Cancer's impact on the sexual relationship
- It’s important caregivers take care of themselves
- Ask people for support — they want to help
- Any last advice to people dealing with their own diagnosis?
This interview has been edited for clarity. This is not medical advice. Please consult with your healthcare provider for treatment decisions.

Pre-Diagnosis
What were your first symptoms?
- Bloating
- Pinching pain right side in abdomen
- Fatigue
I had just turned 40 years old. I have three kids; y kids were age 12, 10, and 4. I was very physically active. I was on a soccer team with my husband, a co-ed soccer team. I ran every day with my golden retriever. I felt like there wasn’t anything I was really, really concerned about.
I went for my annual checkups. As far as cancer in my family, my mother had had breast cancer and uterine cancer, but she was a survivor. I made sure to get my mammograms and things like that.
I noticed, though, that when I turned 40 in January, my pants started to feel snug. I knew that on certain days of the month, I would bloat like most women do, then I would de-bloat, and I could wear my skinny jeans then.
I remember thinking, “Oh my gosh, it’s snug down there.” I did more sit-ups. I tried to do more exercising. It still continued to be snug.
I also had a pinching pain on my right side in my abdomen, but I told myself it was just intestinal or something like that. It seemed to go away if I’d sit up, but if I sat down, I felt it.
As a busy mom of three, I just stood up more. I had this thing where I had the ‘three-strike rule.’
I was too busy to go to the doctor unless there were three things wrong with me. I hadn’t hit the three things yet.
What was the catalyst that got you to go to the doctor?
I noticed feeling always tired. What mom isn’t? What really spurred me to go to the doctor, though, was I was playing soccer, and this 200-pound guy kicked the ball as hard as he could at my face.
I got my hand up in time to block it, but we all thought my hand was broken. It was black and blue and this and that. I thought, “Oh my gosh, I really need to go to the doctor.”
Describe the first doctor’s appointment
I made an appointment the next day to go see my general practitioner, a woman who I had seen off and on for years. While she was looking at my arm, I said, “You know, I also think I’m gaining weight.”
At that point, I started to feel something may be pressing on my bladder. I had uterine tract infections before, bladder infections like that. I was going away to celebrate my 40th birthday with my girlfriends that coming weekend.
I asked if we could check to see if I had a bladder infection first because I didn’t want to get out to Asheville and then not have any fun.
She said, “Sure, we can do that.” While she was still looking at my wrist — my hand was fine by the way; it was just bruised — I said, “You know, I’m also gaining weight, I think. I’m bloated, and I’ve had this pinching pain on one side.”
She said, “Oh, well, that doesn’t sound right. Let me feel around.” She started to feel on the outside and said something didn’t feel exactly normal or right.
She wanted to do a pelvic exam, and I made fun. I said, “Oh, for a broken hand? That seems kind of a lot.” She said, “No, Heather, I really think that I should do that.”
I said, “Back in November, I had gone to the doctor for some spotting. They did a full pelvic exam in November. Said everything looked okay. Don’t know why I’m spotting. They said it was perimenopausal symptoms probably. I had never done that before in my life, and I just went home.”
I tried to talk her out of it. I said, “Well, I just had a pelvic exam several months ago, five months ago, and everything was fine.”
She said, “No, I really should do this.”
I let her do a pelvic exam. She said, “Heather, I can’t even get over to the right side of you. There is something blocking.”
Things started to happen very quickly then. She made an appointment for the next morning for me to have a vaginal ultrasound.
What happened at the vaginal ultrasound?
I had to drink a ton of water, which was not fun, so that they can see better on top of a full bladder. As I was trying not to go to the bathroom, the lady’s talking to me while she’s doing it. She was very sweet.
She was very chatty until she wasn’t anymore.
All of a sudden, she stopped and started to really take lots of recordings. Then she said, “Okay, I need you to sit here. Don’t go anywhere. I need to go talk to the radiologist.”
She disappeared, but she would come back in and call me sweetheart, offer me more blankets, offer me drinks, and all this stuff. It was starting to get to where I could tell there was something really not right.
My husband, luckily, had some sort of wisdom and foresight to have brought me. He was in the waiting room. Finally, they said I could get dressed, but not to leave.
We went and sat out there for another fifteen minutes until the radiologist came out and said, “There’s a mass, and it’s about 12 centimeters, which is about like this, on one side that looks like it’s your ovary, and it’s complex. You need to go right to your gynecologist and share these films with him.”
They had been trying to call the gynecologist for 15 minutes and could not get through. That’s what the holdup was.
What procedures and tests came next?
My husband basically took me and the films, loaded me in the truck, and drove me straight there. I don’t really remember much of that because you’re sort of like been slapped in the face.
He’s driving me there, and I know it’s a very busy practice. There’s tons of pregnant women everywhere. I just go up with my films to the receptionist, lay them down, and say, “Help. I have a complex, large mass, and I need to be seen right away.”
They got me back with somebody within five minutes. He’s looking at it. He did another exam. They took a blood test. He said, “Okay, it looks complex. I could remove this. This is a mass that should come out, but it’s complex.” I think that it had blood vessels in there.
He said, “I’m gonna send you to a gynecological oncology surgeon.” I found out later your number-one way of surviving ovarian cancer, which is what I had, is to have the right surgeon treat it like it’s cancer before they know that it’s cancer.
They took a blood test called CA 125, which I have had tons of since. It’s a marker test. There is no screening test for ovarian cancer. In the early stages, CA 125 can show a normal response even though you have cancer. They don’t like to use it, but it’s just another piece of evidence.
Luckily, they were able to get me into a really good gynecological oncology surgeon the next day, which was wonderful, except that I was supposed to be leaving with my girlfriends to go to the mountains.
I had to call them, and that was very, very emotional. It was very scary. You just don’t even know what to think, but I didn’t know anything at that point for sure.

Describe the first visit to the oncologist
The next morning, I went to the oncologist. She looked at it and she said, “Okay, it could be a benign mass, or it could be cancer. We will not know until we take it out, until we open you up.”
We scheduled the surgery for a week later. The CA 125 came back as slightly abnormal. The normal is below 35, and I was 42. I’ve known people who have had numbers up in the tens of thousands, so 42 was not something that would say yes, it’s cancer, so again, I was in limbo.
The whole weekend I was in limbo, but my girlfriends were all around me. The only advice I was given was, “Don’t rupture it. Whatever you do.”
Everyone made sure I didn’t run, I didn’t fall, [and] there was nothing that would cause it to rupture.
You started having difficulty urinating
I got back on Sunday, and on Monday, I ended up in the ER because I could not urinate. I drank a full chai latte. I’m a writer, so I went to write. I went to go to the bathroom, and nothing would come out.
About an hour into this, I’m in excruciating pain and being taken by my husband to the emergency room, where they drained almost two liters of urine out of me.
What did they find at the ER?
Come to find out that mass was pushing so hard on my bladder that it seized, and so it could not relax enough to allow me to pee. That was my first actual CT scan because they did that in the ER, and of course they came in and said, yes, it is a mass.
We said, “Well, can we cut it out now because we’re at the same hospital?” But they couldn’t fit me in, so I still had to wait until the next week.
We went to the hospital in the afternoon to have it out, and that was awful because I couldn’t eat or drink, so I was dehydrated and nauseous from hunger.
Tests & Scans
Describe the pelvic exam
With the pelvic exam they also do a rectal exam, and then they do palpitations around your abdomen. It’s like an annual pelvic exam where a woman is up in the stirrups, you have your heels in there, and they do need to enter the vagina.
They’re not doing a pap smear because pap smears don’t detect ovarian cancer (that’s cervical cancer), but what they did was push on one side and push on the other side.
Because I had a mass and they weren’t gonna rupture it, they pushed very gently to feel the edges, to feel it. It was really like a regular pelvic exam done at an annual gynecological physical.
They also then have to put a finger in your rectum because they can also feel it that way. They are very good about preparing you, telling you, making sure it’s not painful.
Usually what they do is they tell you to bear down like you’re having a bowel movement, and then they can go in there, you relax, and they can feel from that wall as well. Then just palpating on the abdomen is just like what regular doctors do, but they are gonna be real gentle if you have any type of a mass.
Describe the vaginal ultrasound
It sounds scary. It’s nothing worse than your pelvic exam except that you might have a full bladder because they tell you to drink a bunch of water usually so that they can contrast between whatever they’re looking for against the bladder.
The bladder is like a lit-up pillow or something, and they’re looking at things on top of it. That was the only uncomfortable part, and I told her.
I said, “I’m gonna pee on the table.” She goes, “You wouldn’t be the first.” She’s like, “It’s okay. Just try to hold on,” and then I put my feet in the stirrups again.
You’re in a shirt, you remove your bottom parts, and then you have a blanket or a sheet over you. You’re not just out there in the room. You’re covered, and they know what they’re doing. There’s a little flat paddle, and then they put lubrication stuff on it before putting it inside the vagina.
They’re going to take ultrasound pictures that way. It’s like getting the ultrasound on the belly, but with the transvaginal ultrasound they get a much better picture of your ovaries, uterus, and those parts of your body for a woman.
Describe the CT scan
I had the added difficulty of being allergic to CT dye. CT dye is put into your vein through an IV, and it helps light up whatever they’re looking at in the blood.
The first couple CT scans that I took, I had to drink a nasty-tasting something (as prep), and they would take some pictures.
It tasted terrible and I’m really bad about tastes, so I learned to ask to put it into my own drink.
I would bring a lemonade or something that I could drink because I didn’t like what they had, and they let me do that after a while.
Somewhere in there they stopped having me drink the stuff, but for that CT scan, I did have to drink this nasty stuff. In the scheme of things, it was okay. It didn’t make me sick; it just was really super sweet. I drank that down, then they took me back, and then they gave me an IV.
Because I was allergic to CT dye, which I knew from years ago, I had to take a bunch of prednisone (steroid) beforehand. When they had me at the ER and they did the CT scan, they did not do the contrast dye.
The contrast dye gives a better picture, but because I was allergic to it and they didn’t have time to prep me for it at the ER, they didn’t do it there.
Then they put you in this big, open donut. It’s not like an MRI where you’re enclosed; it’s just an open donut, and then they just lay you down and slide you in.
This machine tells you, ‘Breathe in. Hold your breath. Breathe out.’ Like that. That’s all you do. So you go in. You hold your breath.
If you don’t have any dye in you, you don’t even have to have an IV really. You can’t have anything wire on, so one tip if you’re getting a lot of CT scans done, wear a bra that does not have an underwire, and they’ll let you keep it on.
I learned to wear clothes that had no rivets in it, no snaps, nothing, and then I didn’t have to get into their little gowns or anything. So keep that in mind.
No jewelry, no underwire bras, and then you don’t have to undress. I keep my socks on because my feet always got cold. Then they just slide you in, you hold your breath, they take one or two pictures, and then that’s it.
How long did it take to get results for your tests and scans?
The CA 125 has to be sent off. The first one that I got, actually, they called me on my way driving to the mountains with my girlfriends. My girlfriends would not let them tell me what it was on the phone.
They made me ask them to call my husband and tell him. The nurse thought that was really odd, but they did not want me upset. They were really happy and this and that.
They took it on a Thursday, I saw the oncologist on a Friday, and then it was Friday afternoon when they were calling me, so it was only a day. It was 24 hours.
That time on, my nurse and I became really close. An oncologist nurse. She would track me down anywhere. She would tell me what my CA 125 is. It would go maybe a half a day to 24 hours at the most.
Once I started having them regularly, they wanted it done at the same lab all the time because it could fluctuate if I was changing labs a lot. I would always get the CA 125 drawn at the same laboratory after that.

How did you break the news to your loved ones?
From the ultrasound, we went directly to the GYN. Coming home from that, I remember pulling up in the driveway. My mother was watching my four-year-old. My neighbor was outside, and she came around. I was getting out of the truck, and she said, “What’s wrong?”
I just started bawling and just buried my head in her chest. I’m like, ‘There’s a mass. They think it could be cancer, and I have to see an oncologist tomorrow.’
I was just a mess. I don’t even remember how I got inside. Somehow I got inside, and my mother was there. She’s trying to take care of my four-year-old daughter, my other kids are there, and I can’t hide emotion.
That’s not something I ever will do with my kids necessarily. I mean, there’s some points where I did, but I never wanted to hide, and I couldn’t. I couldn’t hide being scared and worried and all that. It was my mom.
I gave her a quick rundown as quickly as I could. Then I remember my husband, he and I just went out and sat on the back deck by ourselves and just looked at the trees and the birds, and it was just really hard because we didn’t have anything to say.
We just held hands and said, “Wow, things can change like that.” One second you’re playing soccer, and the next second you’re in a doctor’s office and they’re telling you that it could be cancer.
I think they handled it really well. The doctors said, “Let’s talk about the elephant in the room. I don’t know if it’s cancer, but it could be.” It is a slap in the face, and it’s hard to breathe. It’s hard to just process it.
Then having to call my girlfriends, because some of them are flying in, to tell them, “Okay, I can’t pick you up from the airport because I’ll be with an oncologist,” and them trying to love on me over the phone as much as they can.
Of course people want to tell you that it’s fine. ‘It’s gonna be fine. It’s gonna be okay.’
That’s all great, and that’s what people do when they don’t know what to do, even though I knew that it could be not okay. You just stare, and you just breathe.
My husband was a trooper, and he fought as hard as I did. It could have gone the other way because his mother died of breast cancer when he was nine years old. He was now suddenly faced with a wife, with three kids, and he didn’t know what he was gonna have to deal with, which leads me into what he had to deal with when I was in surgery.
It just knocks the breath out of you. It really does because you don’t know, and it’s horrible for anybody, but when you’ve got a four-year-old who’s climbing on you, you get more scared about what’s gonna happen to them, your kids.
»MORE: Breaking the news of a diagnosis to loved ones
Treatment Decisions
How did you decide where to go for treatment?
It worked out to where my GYN said, “I want to send you to a gynecological oncology surgeon.” I live in North Carolina in the Triangle area, so University of North Carolina Medical School and Hospital is a really good one, and Duke University Hospital is another really good place.
It just so happened we thought my insurance might work better with Duke, and they had an oncologist available the next morning, Dr. Paula Lee, who was fabulous. I can’t say enough good things about her and her team.
I went there, and when I spoke with her the next day, she had me come to a small location. There’s a big Duke Medical Center with their Cancer Center, which is beautiful. There’s meditation rooms, all sorts of stuff.
I went to a small offshoot of that. She felt that I might like it better there. I think I did because it was smaller, more intimate. I didn’t have to pay for parking. She worked there half the time. She did her surgeries at big Duke, but she could do it at the smaller location.
What did you like about going to a smaller treatment center?
I’d seen people go to big Duke. I had gone to talk with people in chemo there, and that’s great. A big hospital is great. There are lots of things, but it’s also a really long distance to walk. They have wheelchairs and stuff, but it’s just huge, so I personally felt like I got very good service at a smaller branch.
I think I would probably recommend that over going to a huge hospital unless that’s really your only choice. There are perks for that, like the meditation room and things like. Music therapy. They had someone playing the grand piano in the foyer and things like that, but I personally liked the smaller campus.

Did you get a second opinion?
Because it was all happening so fast and because I agreed with her that whatever it was it needed to come out, I did not feel like I needed a second opinion.
I went under not knowing that I was going to have a total hysterectomy and my ovaries gone and everything. Dr. Lee spent a lot of time right before I went into surgery explaining [scenarios] to me.
“If this happens, this is what I’ll have to do, and if this happens, this is what I’ll have to do. I need you to sign off that you are okay with me doing all these different things if this happens.”
I went under fully understanding, but I didn’t know what was actually going to happen.
Did you research your cancer and treatment before starting?
The first part, I was just too engrossed in getting the surgery to go online. Actually, my husband wouldn’t let me go online. I think he went online, which was probably not good either.
But I know after I was diagnosed he spent a lot of time online, and the more he was on there the darker circles that were under his eyes, because you get doom and gloom on the internet. You get a lot of doom and gloom, and you don’t get a lot of the uplifting, hopeful stories.
Anybody who goes online to do their own medical research and stuff with diagnosis and stuff, just take that knowing that it tends to not show you an even good and bad.
It tends to show you bad, bad, bad, and so I was told that I shouldn’t do all of that, especially because we didn’t know what we were dealing with.
The nurse told me months later that Dr. Lee actually went in thinking that I did not have cancer and that she was very angry on my behalf when she realized that it was indeed cancer.
Again, she was a very experienced oncologist surgeon, and just looking at the CT scan and ultrasounds, she could not tell for sure that it was cancer until she went in.
What’s your advice to patients and caregivers about to start treatment?
Make sure whoever is going to be sitting in that waiting room while you’re in surgery has support, because you don’t know what’s going to happen.
My husband was all by himself and my surgery was only supposed to be an hour and a half. They said, “If it’s cancer, we’ll come out at an hour and a half and let you know things are going well, but it’ll be a little longer.”
At two hours, they came out and said, “Things are going well, but it’s going to be a little longer.” It was five hours. He lost his mom to cancer when he was nine, and he was by himself, so think about it.
Not to assume the worst, but if you have someone waiting in the waiting room, have them have some support or a friend if it is going to be bad.
Your doctor had great bedside manners
I love doctors and nurses, oncologists especially. I don’t know if you notice this as a patient, but they tend to walk into rooms and shut the door quietly. She would move quietly, she would move gently, and she would talk to me gently. Nothing was rushed or fast.
Now when I go visit her, she’s like, “Oh, how are you?” It was always calm and gentle. I even told her later, “Do they train you to do that? Because that was really good.”
Because you are in a state of shock. You are still in a state of shock. You just need this buffer around you, people to be kind, and people to smile, be helpful, not scare you, and not tell you their horror stories. But also not give you false hopes. Not too many false hopes, either.
Surgery
How was the surgery prep?
It’s hard. I know that they asked me how I was feeling, and I just said, “I’m nauseous because I’m so hungry and dehydrated.” Because they wouldn’t let me drink anything.
They said, “Well, we have to set up the IV, and we’ll give you fluids so you’ll feel better.” That was sort of a little carrot dangle. “You’ll feel better if you let us put the IV in.” [I’m scared of needles.] I gave birth to three babies, and the worst part was getting the IV.
My husband was back there with me and held my hand through getting the IV. I breathed and tried to think of happy thoughts. I learned later how to think of happy thoughts and come up with a happy thought.
It’s very, very important to have a happy place that you can retreat to in your mind. I did not, at that time, have one. But over the subsequent 15 months of chemo, I did come up with one.
That was the second of 108 sticks I had in one year. By the end, I no longer fear needles. I have a healthy respect for needles, but I don’t fear them anymore.

I remember going in and getting undressed. My blood pressure was up a little bit, but I was still going in there thinking that this was a cyst. It grew so fast. It had to be a cyst. It couldn’t be cancer. No one had ovarian cancer.
In the room, you get the little booties on, you get the gown on, and they did get the IV in. Luckily, I have been blessed with very nice, easy-to-get veins, so even though I don’t like getting stuck, they always get it on the first try. It’s always great.
I remember her coming in and talking to me and saying, “We’re gonna take out the mass, and then while you’re under, I’m going to look at it under a microscope. I’m going to be able to tell what type of cells we’re dealing with, what type of mass we’re dealing with. Depending on what it is, then I may have to take the other ovary. Okay?”
At that time, we weren’t sure. We thought it might just be that one side. I was like, “Okay,” but there were many other questions.
“Are you okay if I take the other ovary? Are you okay if I go through your whole body looking for some cancer cells if that’s what happens?” Ovarian cancer’s like a snow globe, so it sticks on cells everywhere.
A lot of ovarian cancer patients have growth all over their intestines, so they have to go through and look through on the outside of your intestines, your stomach, all of that.
I signed off saying, yes, that’s understandable. I’m done having my kids, too. I remember being wheeled down, and you see the lights and the view.
It’s like those emergency room doctor shows, and you can always hear the music in the background. The lights are going by, and you’re being wheeled down. It’s just surreal.
But at that point, I was just so hungry and exhausted from being hungry, dehydrated, and having an IV, which was very stressful at the time for me to get, that I was just really happy when they had me start counting backwards from ten.
That’s my favorite part of any surgery, counting backwards. Then you just drift away. It’s just the most peaceful, wonderful feeling.
»MORE: Read more patient experiences with surgery
What do you remember about waking up from surgery?
Waking up, not so wonderful. I woke up. I was supposed to be in an outpatient room, like a triage center. I woke up in a you’re-in-for-the-night room.
I think I was awake for a long time, it seems, with such pain in my back from laying down and such pain that I couldn’t communicate it. That was the worst part because I couldn’t say anything yet. I wasn’t awake enough yet to say, “I’m in pain.” I just had to wait and wait it out until I could finally speak.
My husband was there, and he got up and saw that my eyes were open. I said, “I’m in a room. This isn’t good.” He said, “No. It’s cancer.”
Describe the moment you heard that first official cancer diagnosis
Your whole life changes, like that. There will always be before cancer and after cancer. When I look at pictures, [I think,] “Is that before cancer or after cancer?”
My whole life has now been delineated. It’s been partitioned. Before you knew, then after you knew. Because it’s a complete game changer.
I was still so groggy and in pain. It’s so hard to think rationally when you’re in pain. That pain is something that I had to deal with for a long time because I had a lot of problems with the chemo. But you can’t think rationally.
All I can do is cry when I’m in pain. But I couldn’t even cry, and that was one of the worst parts because it hurt too much to cry.
When you have abdominal surgery like that, it ended up being that she not only had to take the mass. She had to take the other ovary, the uterus. They found out I had the start of uterine cancer, which was easy to fix. They just take out the uterus.
Then in four different places on the inside of pelvic wall, she had to scrape layers off to make sure she got everything that she could. Then they’d flood the region with saline, and they take the wash out because they did a look through the wash to see if there were already cells being split off.
Obviously there were some, because then you go on to the sides of the pelvis inside. She spent five hours searching all up and down my intestines and taking out all of that through tiny little slits because she did laparoscopic surgery.
»MORE: Patients share how they processed a cancer diagnosis
How was laparoscopic surgery described to you?
I think two holes, a little slit, and then she did stuff through the vagina, too. There were 18 stitches internally through the vagina, where she took out the cervix. So it was all gone.
That caused a lot of pain. I just remember laying there and the cuffs on my feet. They put these little blow-up cuffs. I really like them. They massage your calves; they keep the blood flowing so you don’t get blood clot. They would go pssh, pssh, and blow.
In my strange state, I would go, “Pssh, pssh,” as soon as they activated. The pssh, pssh, and I’d go, “Pssh, pssh.” We’d go back and forth. But I couldn’t breathe very well because of all of that trauma in my abdomen and the muscles being cut.
How did you cope with the post-surgery pain?
They ended up having to give me one of those tubes to blow into to help me concentrate on breathing in and out because I would start to hyperventilate, and then I couldn’t breathe.
I couldn’t cry because any time I started to cry, I would start to breathe fast, I would tense up, and then it was so much pain that I couldn’t breathe. I remember laying there, wanting to cry, and not being able to cry.
I also remember the pain in my back and finally being able to communicate and saying, “You’ve gotta get me off my back.” They set me up in the bed. Then I had to go to the bathroom because I’m laying on the catheter that was taking care of my urine.
The doctor came to talk to me, and she could tell, because I was shaking so badly, that I was in immense pain. She was very frustrated because at the time, the nurses were not responding very well. They did not know it was the surgeon who was asking them to bring in more pain killers for me, so they were taking their time a little bit.
She had to get a little bit severe and make sure they got in there. They were saying I couldn’t go home if they gave me more. The doctor said, “It doesn’t matter. Then she will stay, because she is in so much pain she cannot understand what I’m saying.”
They had to give me another full dose to get me to a level where I wasn’t shaking.
How long did it take to start recovering?
I did end up walking by that night in the hall, crazy enough. They were very wanting to try to get me mobile. They took the catheter out, so I was able to go to the bathroom, but I couldn’t sit down. I couldn’t bend. I couldn’t get out of bed. I couldn’t do anything on my own.
Either Braden would help me stand and take me there, or the nurse would. My girlfriends came with cookies, my older daughter, who was 12 at the time, and my mom.
I think Braden told them all they were not allowed to cry because nobody cried.
If they cry, then I’ll start to cry, and then I couldn’t breathe. Then the nurses were all worried because bells would go off or something. It was this terrible mess.
We went home that night or the next day. I can’t remember. It’s so foggy. I started slowly walking again about a week-and-a-half to two weeks later. I couldn’t walk with my dog. I got tired really easily. After a big surgery like that, you get tired very, very quickly.
I remember going to Target. I didn’t think I could get home, and the store was just around the corner. I managed to get there and walk to the aisles, leaning on the cart. I saw neighbors, and they wanted to chat.
Then I get out to the car, and I just had to sit there for 15 minutes before I had the energy to be able to drive home. I realized I was really pushing myself, and that was just two weeks after the surgery.
I had to sleep with seven pillows propped around me. I slept sitting up with pillows under my knees and around me, so I couldn’t move. I swore I would never ever be able to sleep on my stomach again. But I do. Now I sleep on my stomach, too.
I still had to have someone help me to sit down, go to the bathroom, and [be] with me for probably three weeks. Taking off the tape for the sutures was really scary. I remember Braden stood outside the shower, making sure I was okay.

Were there any post-surgery complications?
About three weeks later, I started bleeding vaginally. I’d bleed, I’d spot, and I’m like, “What is this?” So I wouldn’t move. Of course, I called them right away, and they said, “Okay, is it just the little spots?” It was just little spots, but it started getting bigger.
I remember I was going in to meet with my pastor that day, and I started to really hemorrhage. I called them, and they said, “Okay, you’ve gotta come in right away. Something’s going on. It’s not little spots. You’re soaking a pad, okay.” So I went in.
I had to leave my pastor, who gave me great advice: ‘All these things are happening to you, Heather, that you have no control over. All you can control is how you respond to them. What kind of woman do you want to be in response to this?’
I carried that with me. I carried that piece of advice almost like it was tangible. As my mother rushed me, I told my husband, “Stay home, you’re working.” He works from home, luckily, and the kids were at school.
My mom drove me to Dr. Lee. She got me right into the stirrups, and come to find out a couple of my sutures had opened up inside. She had to cauterize them closed with no anesthesia.
This is where I learned how to separate pain and suffering. There are two different things. Pain is a physical response to something happening in you. This is the neurons firing, saying, ‘Hey, hey, something’s happening.’
This here, the suffering, that’s the emotion behind it. That’s the, ‘I’m being attacked. Is this ever gonna end? Am I gonna be like this forever? Am I gonna die?’
Lying there with my feet in the stirrups, and she was so good. My mom was holding my hand. The doctor’s like, “Okay, you can’t move. I have to cauterize these shut.”
She had these long Q-tips that she was sticking in there. She kept pulling out these Q-tips with blood, because it was bleeding. It was just a suture, like if you had a cut and a suture. They just opened up.
It burned. It’s in a sensitive place, so I couldn’t move. Dr. Lee kept saying, “Don’t move, don’t move, don’t move, don’t move.” So I breathed in, and I thought, “Okay, this is the pain, and this is the suffering.”
I physically turned my eyes to the left and thought about the signal that was going to my brain that said that she was doing this, and I wasn’t gonna move. I didn’t move.
That was like a light switch went on, and I was like, ‘Okay, I can do this.’
The needles, the port that I got. Out of all that stuff, I could separate it. Pain and suffering. It’s really helpful, and it doesn’t work all the time. They’d like to go together. But if I could get rid of that, “Am I gonna die? Is this gonna end? Do I trust the person working on me? What is happening?”
If you can get rid of that, and you just go, “Okay, these are the facts. This is what’s happening to my body, and I’m gonna get through this.” That’s the type of woman I’m gonna be. I’m strong, and I’m not moving. I didn’t move.
I like to tell people if you’re going through that pain that’s critical, acute pain versus the long-term pain. That’s a different strategy that I’ve had to work with. But the acute pain, if you can separate it, it really does help.
The mental healing took longer than the physical recovery
You’re in so much pain and fear. The fear is as bad as the pain. The fear [is] crippling. That does not leave, even when the pain eventually went away. I’m eight years out and still have fear, and that’s normal.
But I’ll tell you, it gets better. It gets better, but boy, those first three weeks. That’s fear you can taste, like you’re going to throw up fear. That’s ugly-cry fear. It’s different for everybody. Some people can be very stoic, and that’s okay, too. But some people, like me, it’s just really hard.
It took me a week after the surgery to be able to cry before I could breathe when crying. That’s when the waterworks really started because then I was finally to the point where I could cry.
People would come visit, and they were told strictly that they could only smile in my house. My husband was like, “You can’t let her cry, because then she can’t breathe.”
Do you recall the moment you got the staging?
I remember the day that Dr. Lee called to tell me it was stage 2 because we weren’t supposed to see her for another weekend, and it was like a Thursday or Friday. She called, and I was upstairs and Braden was outside. I had a friend sitting with me. She called my mom, and she says, “The doctor’s on the phone.”
They got me on the phone. I am on heavy pain killers, on the Oxycodone, Percocet, whatever. I’m floating. We got a ton because it would wear off, and Braden knew exactly where I could have another pill. We kept it right there at the beginning because otherwise I couldn’t breathe. I was just in so much pain, so I was little loopy.
Dr. Lee: Heather, I’ve got your stage.
Heather: Wait. You’re not supposed to tell me now. I’m not ready to hear this now. Braden’s not even in the house. You’re supposed to tell us in person.
Dr. Lee: Heather, stop, it’s good news.
Heather: Okay, all right, you can tell me.
Dr. Lee: It’s stage 2. Stage 2C, but it’s stage 2.
Which means I had a fighting chance. Everybody has a fighting chance, let me tell you. I’ve met stage 4 people who have beaten it. They only had a 95% chance to live five years, and they’re like 15 years out. If you’re stage 4, I don’t mean to scare you. I really don’t.
When she said it was stage 2, Braden came running upstairs, and there are tears in his eyes. I didn’t realize at the time what a big deal stage 2 was.
He ended up having a stage 2 party, where people came over. We had like 20 people come over that night. They put me on the pillows on the couch.
I was still bloated, really bloated, from all the gas they put in there and all the trauma to the abdomen. I was just on the couch, kind of woozy but having a great time because everybody was so happy.
That was April 3rd. I was given until May 3rd to start chemo.

How did your loved ones react to your diagnosis?
I remember telling my girlfriends when they came, because we’d always go to the beach every year together. There’s 18 of us. There’s eight adults and 10 kids. And we always go to the beach together. We’ve been doing it for … at that point, 13 years, I guess.
The first thing I said to them when they came, I said, “Make sure they still go to the beach without me.” They were like, “We’re not going back. We’re not doing that. That’s not happening. We’re gonna get you through this.”
They had apparently been looking at the internet, which is really bad for ovarian cancer. The internet will say something like 46% survival rate. At the time, they did not have a stage for me, and that’s huge when it comes to survival rates with ovarian.
I ended up being stage 2C, which gave me about anywhere between a 57 to a 75% chance of surviving five years. If you go to stage 3, which I was very close to stage 3, that number would’ve dropped to 20% chance of living five years.
I was really lucky that I got hit with that soccer ball and really lucky that I said something when she was looking at my hand.
Women out there, if you have symptoms, don’t wait. Don’t wait until you have three things wrong with you. Don’t wait until your next GYN visit, because I had mine five months before all this happened.
»MORE: Breaking the news of a diagnosis to loved ones
The debulking happened after. What is that?
What she said was they did all the surgery that they could do to do a debulking. They call it “optimal debulking.” They took out everything they could, and they were going to give me until May 3rd to heal as much as I could before they started the chemo.
With ovarian cancer — and I think most cancers — they hit you really, really hard. If ovarian comes back, it’s really not good, so they want to hit it with everything they’ve got the very first time.
I went back to the doctor within a week. That was really hard because even though I’m stage 2, you still hear really bad things. I still didn’t know what my percentages were; I couldn’t even speak it.
I remember being in there and just breaking down and saying, “Do you ever have patients who become grandparents?” I didn’t feel like there was even a chance that I could live to be a grandma. She’s like, “Yes, yes. I do have patients who become grandparents.”
She was thinking that because of my age. I was young and healthy. Everything went well with the debulking, so I probably had a good 70% chance of living five years or more, I guess. She didn’t say that part.
She said, “You might be eligible for a clinical trial,” which was kind of ironic, because for 14 years, I helped manage clinical trials as a drug development coordinator. I remember thinking I would never go on a clinical trial, and here I was being talked to about a clinical trial.
My first thought was, “Absolutely. I’ve got three kids. I’ve got three young kids. I have to live, and we are going to do everything that we absolutely can to ensure that that happens.”
I was all about the clinical trial. She had to still find out if I was eligible, things like that. But it was giving me hope.
»MORE: Learn more about the process of clinical trials from one program director
Chemotherapy & Clinical Trial (Concurrent)
What was the decision-making to pursue chemotherapy?
Even for stage 1 ovarian cancer, they do a full round of chemo. It’s so deadly that they get in there as fast as they think your body can handle.
What was your first impression of the chemotherapy process?
Before I went into chemo, they gave me a tour of the chemo room so I could see how nice it was. It had a garden outside the windows. I guess it may have helped me, but don’t be shocked if you go on the tour or even your first day you go to chemo, and you look at those people and you’re just devastated.
I walked out of there and went into the parking lot with my husband and just sobbed. I said, “Honey, all those people in there look half dead, and I’m going to be one of them.”
I was so upset, so upset. I was still looking through those panic filters. Once I started going, I realized that those people are not ‘just dying.’
They are fighting, and they’re fighting harder than anyone I’ve ever known. They might be napping, they might look awful, or they might just be reading a book or whatever, but they are fighting.
And it actually is beautiful.
As a brand-new patient, that is not how I saw it, but I came around to that. If you are freaked out when you first see the chemo room, that is totally normal and okay. It doesn’t mean that that’s how it’s always gonna feel to you.
In fact, I went every Tuesday for 18 weeks and every third Tuesday for 10 more months. I liked those days, actually. I got to go, and I was treated like a queen. People brought me things. They wrapped me in warm blankets.
First, I just want to say it’s okay to totally be panicky about going there, looking at those people, and feeling like, “Oh my gosh, I’m going to be one of those people, and I don’t want to be one of those people.” You do. You wanna be fighting. You wanna be a fighter.
I really did not hate chemo at all. I came to look forward to the nurses. My husband always made them chocolate-dipped strawberries, which always helped. They all came to wait on my chemo.

Describe getting the port(acath)
I had to be put under for that, and that time, I did cry being put under. It was a surgery, and the last time I had gone under, I woke up with ovarian cancer, so I was so scared. They’re like, “We do this all the time.”
I wasn’t deep, deep under. But there’s a funny story about that. I’m claustrophobic, and when you’re getting a port put in, they’ve got your face kind of covered. They’ve got all of these TV monitors above you where they’re looking.
They’re scanning to see exactly where your veins are and everything so they put it in correctly. I started to wake up, and I still had the cover on my face.
They must have all realized I was waking up because I heard five different people going, “Don’t move, don’t move, don’t move.” I’m like, “I’m claustrophobic.” And they’re like, “Don’t move.”
Then I went back out. I remember that. Then I woke up in the recovery, and it was sore. I’d say my neck was stiff from having it to the side.
For two days, my neck was really stiff. Then I had this bulbous thing [on my chest], and I’m really squeamish about the sort of thing.
Did you like the port?
I loved my port. I did not have to risk my veins. They would just do it through there. It still pinches because they have to go through my skin, so it’s still a poke. But they can then tape over the port with the IV in it.
I had it hooked up so when I did these six-hour infusions, I could move my arm around. People who had it infused through their veins, they often had to put a warm blanket around their arms and just keep it floating.
I didn’t have to deal with any of that, so I highly recommend it. Because I was getting weekly chemo, they really wanted me to do that. I think to be part of the clinical trial, I needed to do it anyway.
I just went ahead and got the port before my first chemo. It still would pinch when I would get that in there. You can tell them, “Do it when I’m not thinking about it,” or, “A one, two, three, poke.”
You can let them know what you prefer. I was a one, two, three girl. So one, two, three, and I knew it was coming.
Describe your chemo regimen
I was going every week for 18 weeks to get paclitaxel (Taxol), so my nerves were being affected. Every three weeks, I would get carboplatin along with the paclitaxel.
The very first time you get chemo — and they don’t always talk about this — a lot of times your body can go into freak-out because it’s the first time you’re getting a poison put into your body.
Sometimes you’ll start to feel like you can’t breathe. If that’s happening and you’re starting to panic when you first are getting your chemo, please tell the nurse. They know all about this.
Describe what happened during and after the infusions
Different chemos do different things to you. I doubt it’s just for ovarian cancer. The nurses were right on it; they knew what to give me to help me calm down. They knew what to tell me. They’re just right on it. They’re so wonderful, and they’re trained so well.
They don’t like to scare you, because sometimes it doesn’t happen. But I think that I would’ve liked to have known that that could’ve happened, because it did. I was afraid to say anything because I thought it’s just in my head.
Come to find out, no. It is something that happens. They did come over and give me more steroid. They backed off on the chemo. They put more saline in and might’ve given me a second Benadryl. I don’t know. It was just through the IV to get my body to stop reacting.
All of that really tired me out. When I got to the car, I was just exhausted and fell asleep on the way home, mouth hanging open. My [chemo buddy] would help me in, and then I would nap on the couch. The kids would come in and cover me up, check on me, and bring me drinks.
I would wake up, and then I was on dexamethasone, which is a steroid to keep your body calm. I went one time 36 hours without even yawning after that. I would talk really, really fast.
I was just like that because that’s what that steroid would do, so they taper you off of it. I would take the full dose for the first day, and then they would slowly taper me off.
Each time I would get chemo, I’d have that reaction, especially if it was three drugs. For the three drugs, the nurses would give me even more steroids, because carboplatin is really nasty and can make you have neuropathy in your hands and feet, which is tingling, pain, and numbness.
I did get some of that in here, some of that. It can be permanent, so they want to know about it. Mine did go away. It took a long time because my nerves were damaged so much, and they had to grow back. They grow back about half an inch a year or something.
The first couple cycles were fine. The cycle was three weeks. I did six cycles of three weeks each of the really hard stuff.
By the sixth cycle, it was cumulative, so things were getting harder and harder with each one. The first cycle, the first three weeks was fine. I’m still gardening outside. The second cycle is when things started to change more.
You brought a “chemo buddy”
Their job was to hold my hand when I got the IV and then to get me out to the car at the end without letting me walk into any walls, because they would give me so much Benadryl and steroids to keep me calm and keep my body from reacting to the poison that’s being put into it.
You’re killing off fast-growing cells. That’s why your hair falls out, because they’re fast-growing cells. That’s why you lose taste buds, because they’re fast-growing cells. But they also kill cancer cells. You want all of that to happen because that means that that medicine is really affecting you, affecting those cells.
I always had a chemo buddy. They would drive me home. I would always fall asleep on the way home, then I’d wake up, and then I’d be getting hyper.

You underwent your first clinical trial at the same time
I would get my clinical trial material, which was Avastin. Bevacizumab was its technical name. I would get that every three weeks as well. I was on a control arm, so it was put into my IV along with the other things, instead of it being put intraperitoneal, which I would have had through a different port in my abdomen.
At first I was upset that I was in the control arm. It just means that it’s the regimen you would normally have, along with the clinical trial material. They would normally just give things through the IV. They don’t just give me a placebo. That’s inhumane.
They were still giving me the normal stuff, and then the control arm for this clinical trial happened to be the clinical trial material given to me through an IV in my vein, instead of being put into my body cavity and swooshed around.
I was still getting some clinical trial material, a new drug, but it was being delivered in the old-fashioned way. At first, I was a little bit upset because I didn’t feel like it was tough enough, but it ended up being a good thing for me.

How long did it take to get the infusions?
On the day that I had to get all three (carboplatin, paclitaxel, Avastin), I was there six to eight hours for those infusions. I would write, I would read, and I would just talk. I’d doze. They had televisions, but I didn’t watch the TV. I’d go talk to people around. My mother and I also knitted these fuzzy hats.
Backstory: When I lost my hair, I wore this hat. A World War II nurse knitted it for me, and when she died a few years ago, my mother and I pledged to continue her ministry by knitting these for any cancer patients who would like one sent to them.
If you are watching this, we’d be happy to knit and send you one. When I lost all my hair, I had bumps on my head, and they hurt. This hat was the only way I could put my head on the pillow without hurting.
So I wore these all the time. I would go around, and I would give these out. We would knit them, and I would give them out.
What helped you get through the infusions?
They came around with snacks, so in the early stages, that was cool. By the other cycles where my mouth hurt so badly, I did not get snacks, but they would always bring them around.
The warm blankets are the bomb. Those are awesome. I would come in and immediately ask to be wrapped, cocooned in a warm blanket. They had these little heaters that they would put them in, and they’d bring them out.
They’re really wonderful. In fact, I’ll still use them at home. If my kids are not feeling good, I put one in the dryer and wrap them in a warm blanket. I got that from the hospital.
Tip: tell your medical team about all side effects
If you have any type of side effects, you need to be telling your nurse. There’s never a side effect that you should just keep to yourself, even the embarrassing ones.
They have heard everything, believe me, so there’s nothing that would shock them.
List of chemo side effects & what helped with them
- Head hair loss
- Folliculitis (infected hair follicles)
- Runny nose (loss of nose hairs)
- Eyelash & eyebrow loss
- Nails & teeth
- Loss in taste
- Mouth sores
- Sore throat
- Constipation & anal fissures
- Foot pain
- General nerve issues
- Note: Oxycodone
I think that the first chemo that I was on, which is the normal chemo regimen, is really fierce, at least for ovarian. I’m sure it is for the other cancers as well because they’re trying to hit it really hard at first to get rid of it.
The clinical trial material was not nearly as bad, so when I stopped the 18 weeks of the really hard stuff, things got a lot better. They did not get all the way better, but they did get somewhat better.
I’ll just give you an idea of some of the side effects that I had. This is just to let you know what could be happening, what might happen, and where you should feel like, “Oh, okay, this sounds like something that does normally happen when you’re on chemo,” versus, “Maybe I really should go see a doctor.”
Head hair loss
When you’re losing your hair, it’s a more gradual thing sometimes. They’ll give you an idea of when you can expect it to start to happen, but on the same treatment I was on, there were some women who didn’t lose all their hair. It just thinned.
Mine was definitely falling out. You lose hair, of course, almost everywhere. I still have some pubic hair, but it’s very, very thin. Nothing like what I’d look like normally.
»MORE: Dealing with hair loss during cancer treatment
Folliculitis
I lost my hair and got a rash on my scalp, so folliculitis was one of those things. It would hurt for me to put my head on the pillow because they were infected hair follicles actually.
Solution: I wore a hat like my fuzzy hat, which helped me be able to put my head down on the pillow.
Runny nose (loss of nose hairs)
The weirdest thing, though, was losing my nose hairs. You don’t really think about it, but your nose hairs stop your nose from running. My nose seemed to run all the time because there was nothing to catch it or to stop it a bit. That was really kind of weird.
Solution: I always had tissues with me.
Eyelash & eyebrow loss
I had a blog post that I wrote; it was called “Ode to the Last Eyelash.” My last eyelash fell out two weeks after I finished my last chemo, so the hair follicle had died but hadn’t shook lose yet. Then it finally fell out. When I went off of the kind of chemo that makes your hair fall out, they did start to grow fairly quickly. They did grow back, which is interesting to watch them each day get a little longer.
Solution: My eyebrows were still out, but there was still a ridge here, and you could use some eyeshadow and pencil them in so it didn’t look so strange.
Nails & teeth
Things like my nails were turning brownish and kind of coming loose. I was on a neurotoxin chemotherapy, so it was hurting the nerves in my body. My teeth ached because the nerves in my teeth were all being damaged. I wasn’t supposed to floss. That was hard, as it was. They just didn’t want me to cut myself.
Loss in taste
My taste buds went away, a lot of them. One thing I want to mention with the no taste buds that surprised me: I couldn’t taste my tears. You know, the salt? I would cry, I’d lick my lip, and there’s nothing.
It was infuriating to me. It just felt like I was being robbed of being able to cry. I couldn’t even taste my tears, so I would cry in the shower in the hot water. It just washed away.
Then the kids couldn’t hear me crying either, so it was good. It was comforting, so I took like three showers a day, and I’d cry in there. That was surprising, how angry I was that I couldn’t taste my tears.
I could taste some sweet, so I ended up wanting to eat sweet because it’s what I could taste. Things oftentimes tasted like dirt. Of course, they talk about the steel spoons.
Solution: To eat with a plastic spoon sometimes is better because that tang of the steel is picked up.
Mouth sores
I got mouth sores and cracks in the corners of my mouth that would bleed, so I couldn’t open my mouth very wide.
Solution: I was constantly putting coconut oil on my lips and inside my nose with a Q-tip to try to keep the dryness at bay.
Sore throat
When you have cuts and you’re on chemo, they don’t heal very well, so I had abrasions all in my throat. I had a sore throat for the whole five months that I was on [chemo].
Solution: I drank this thing called Carafate that was like a chemical band-aid that you would drink, and it would go down. It tasted terrible. I think I mentioned that I don’t do well with bad taste, so I learned how to drink the Carafate and then rinse my tongue. I did gargling in my mouth with warm baking soda water. That helped some of the sores in my mouth, but I would have them, and they just did not like to heal.
Constipation & anal fissures
At the other end of my digestive tract, I got an anal fissure, and it’s as much fun as it sounds. It’s a cut right there, and it bleeds like crazy. It would not heal while I was on chemo. When you’re taking all these chemo drugs, it can make you constipated, which then, of course, makes it even worse.
I would call my nurse and say, “You gotta fix my butt. You’ve just got to fix it because it just bleeds every time I go to the bathroom.” We tried ointments, and we tried laxatives. We tried so many things, but basically, it just would not really heal until I got off the chemo. It was just something I dealt with, and it was very painful.
Solution: You’ve got a numbing ointment that I would have to apply before I had a bowel movement, just so I would not feel like I was gonna black out from the pain of that.
Foot pains
I had foot pain forever. It seemed like even eight months after I finished chemo, the nerves in my legs and feet were still healing, and I thought I would never be able to walk without pain again. Let me tell you, it does happen. I did get my walking ability back. I do Tabata now and do Zumba, and my feet aren’t screaming at me.
General nerve pain
One thing that was interesting was I had this patch on my leg that would feel hot and wet. I would look down thinking I had peed and it was on my leg, but it was dry and fine there.
It was a nerve thing. There were nerves there that were triggered as if there was warm water being splashed on my leg, and it would happen every once in a while. When my nerves started to grow back, I started getting itchy. I’m at dermatologist appointments, and they would give me ointments. Finally, they said, “It is internal. This is an itch that you cannot get rid of right now.”
Solution: We tried Lyrica, which is a nerve pain thing for fibromyalgia. I did not like Lyrica. You may do fine on it. For me, it just made me run into walls and fall over. I was so dizzy. I could not take it. It was harder for me to take it than to deal with the nerve pain. But I would scratch my legs until they bled because they itched. I would do it in my sleep.
I started sleeping with long socks on, all the way up my legs. Somehow, the pressure on them confused the nerves. Even compression socks or socks, anything covering it helped it a little bit as long as it wasn’t rubbing against it to start the itching happening.
Note: Oxycodone
For two years there, I was on oxycodone because nothing else would allow me to walk. The oxycodone, unfortunately or fortunately, did help, which was a whole ‘nother can of worms because there’s no way you can take oxycodone that long without becoming addicted to it.
I have addiction in my family, and I was very open about that up front. There are some people who can handle chemo and the neuropathy without any painkillers. I am not one of those people. I tried very hard to deal with the pain. It was chronic. My shoulders would ache.
I had to constantly shift. I could never sit still because the body’s constantly trying to figure out a position that wasn’t hurting. I had to take it. I would take half the dosage of what was prescribed because I did not want to get addicted, but you just do.
I didn’t get emotionally addicted because I still was always in pain, but it was enough to take the edge off to where I could walk up to the bus stop, occasionally, to get my kids.
All I could do was lay my cards on the table, be totally honest about it, and my nurse just kept very close track with me. When it came time to where my pain started to finally ebb off, she helped me get off that oxycodone.
It took four full months, and it’s not like I was taking it all the time. At that point, I was only taking one pill a day, but it still took me four months to get off that one pill. I would cut it in half, then a quarter, then an eighth, then a sixteenth, and then a thirty-second.
Then I was licking dust, because if I didn’t lick the dust, I would be up all night with cold shakes and just couldn’t settle down and was up all night with insomnia. It was a detox.
But it saved me a lot. I could walk; I could drive. Things like that. I had to be totally honest with it, and they had to know exactly how much I was on and how much I had to take and how to get off of it.
There were times I was constipated. Oxycodone makes you very constipated.
Solution: I was always on MiraLAX, always dealing with that stuff.
If you’re having problems like that, please tell your nurse. They’re there to work with you. They’re your team. They’re going to try to help even embarrassing parts of you.
No one is going to laugh or snicker or anything because they have seen it all, and it’s all natural parts of your body that are just injured from this life-giving poison that you’re having to take.
»MORE: Cancer patients share their treatment side effects

When did your hair start to fall?
It was actually not to the second cycle yet when my hair started to fall out. I didn’t notice it until after I went to take a shower after gardening, I went like this, and it all came out, spiderwebs in my fingers.
I had already gotten my hair cut short because I had huge, long hair. I got it cut first, and then I did it really short, which was kind of neat because no other time in my life would I cut my hair short. My hairdresser actually didn’t even charge me. She’s like, “It’s all gonna fall out, so I’m not gonna charge you.”
Go for it. If you wanna try a mohawk, go for it. It’s gonna fall out. When else are you gonna do that? So we had fun with it.
I went to wash my hair, this really short hair, and it just all came out in my fingers. It’s a release of your worries, really. But it’s huge. It’s a huge visual thing that something’s happening.
I was pretty determined to put a positive spin on it, even though I was crying.
I called my girlfriend, I said, “I know I’m really strong and this is all good, but my hair’s falling out, and I’m freaking out.” She talked me down. She’s like, “That’s normal. Of course you’re gonna be like that.”
We met, and I could show her I could just pull it out, pluck it out. My kids, my four-year-old, would pluck it out, make a wish, and blow. We would make wishes on my hair. We have videotapes of us making wishes on my hair.
The next day, I called any friends that could come over, and we went out back. I had my one friend give me a pair of pink boxing gloves, and I came out to the sounds of the ‘Rocky’ theme. I came out in a cape, and with that, we shaved my hair.
I wanted to say, “Hey, I’m taking charge of this. I’m not gonna mourn the loss of my hair because every hair follicle dead is a cancer cell dead.”
I decided to celebrate it.
It was difficult at first because I was all about hair. From the time I was little, I had this long, beautiful, wonderful hair. It was tough.
But we did it as positively as we could. The kids were all in on it. My son shaved his head, too. My husband shaved his head. My long-haired girls shaved their heads. We got through that.
What helped most with styling your head?
I got really cool scarves. People would tell me I looked fabulous even with a bald head. Even if I didn’t look fabulous, they all told me that I did.
You could buy the biggest earrings, and everybody thinks they look great. I got the most audacious, fun earrings, and it was great.
I’d wear my little hat because it was easy to put on. Kids would ask me if this was my hair, and so I’d explain to them. Other kids, I’d say, “No, I’m taking some medicine. Made my hair fall out. Don’t you think it’s cool?”
I really have lots of great stories about showing people at Target how to wrap their heads because they saw me.

What helped with the hair loss?
I went to the “Look Good, Feel Good” program. These are free programs, at least in the U.S., at hospitals, and I do recommend going to those. It was nice to spend a day with people going through something similar that I was going through. You learn things like how to wrap your head with a scarf, and I definitely think that’s a good idea.
Were there side effects to the clinical trial (Avastin)?
Things like nose bleeds. That’s typically because it’s dealing with your vascular system. They wanted to make sure that my heart was in good order.
I did an EKG (my heart was fine). Some of the steroids would make my heart palpitate, so they were always watching my blood pressure. I had a blood pressure cuff at home. I would take my blood pressure a lot because [Avastin] could also make your blood pressure go up, and I believe mine did go up with the Avastin.
Other than that, I just still felt kind of icky. Avastin let my hair grow back, so I started growing my hair back after the first five months, even though I had ten more months to go with just Avastin.
It was a good thing I did it. It was good thing emotionally, too, because I felt like I was doing everything I possibly could.
I also felt like I was watched closer because I was on a clinical trial. They really wanted to get into the nitty-gritty of how you’re feeling. I was getting CT scans every six months to watch for any possible recurrence. That was ultimately the reason why I stopped doing the clinical trial.
Although I finished all the drug, they wanted me to continue to do CT scans every six months. But a CT scan is very high in radiation, and I had ten of them in two years. I said, “Okay, you guys are going to give me lymphoma or something with this.”
That’s when I quit the clinical trial. I felt like being on it, they really are watching you very, very closely. Even more than I felt a regular treatment would be. That’s why I liked it as well. I felt like I was doing everything I possibly could to stay with my kids.
»MORE: Dealing with hair loss during cancer treatment
Getting into a Clinical Trial
How did you learn of the clinical trial to begin with?
It was as Duke University, so they know a lot. I was very lucky to live close to Duke. There are several: MD Anderson, Brigham Young.
You can do your own research, and there are advocacy programs out there for people who do not live near a center like that, who can do their own search for it. But it’s just so hard, and so do ask those questions.
If you ask your doctor, or call clinical trial [programs] at these different universities and maybe ask about them. I was very lucky that my doctor was very attuned to it because she was the physician involved in the clinical trial.
Was it easy to understand the clinical trial (Avastin)?
What it does is it stops, hopefully, tumor cells from being able to grow (cancerous) blood vessels. It kills blood vessels around tumors. It starves them, so they have to do it for a really long time.
I was on Avastin for 15 months because the whole idea is that you have to go long enough to starve anything that’s [cancerous]. Because of that, the informed consent was so big. The other thing is I used to write informed consents, and I did not understand a word of this one.
It wasn’t because it was poorly written; it was very nicely written. It was because I was a patient now, and I was panicked. I didn’t know what to do. I had to initial every single page.
I really didn’t understand, so I had to have one of my girlfriends who actually audits clinical trials come over and explain it to me, line by line, and drew it out for me.
If you don’t understand it, really dig and ask questions. Have a parent, someone with you to ask those questions.
Because I am someone who should’ve understood everything because I’ve written them. And I understand very little. There were seven pages alone of serious adverse effects that could happen to me. One of them was death, which is not an effect, anyway. That’s an outcome.
»MORE: Read more patient experiences with Avastin
You worked as a clinical trial manager before the diagnosis
When I was a clinical trial manager, I read so many patients’ information logs. Of course, the names are all covered and everything. No one knows who you really are; you’re just assigning numbers.
After reading all those and all the different series of bad events that could happen on a clinical trial, I thought that I would probably never go on one. But you’re reading a subset, so it’s different than when you really look at the real safety profile of different clinical drugs.
There is a risk, and they’re going to make you aware of that in what they call an informed consent, which is a very large document. It can be like 30 to 70 pages — detailed down to every single thing that happens to you.
You’re supposed to go through it with a nurse and she reads it word for word to you. You have to initial every page so that they know that you’ve gone through it.
I used to help write those, and they write them in layman’s terms. But what I found as a patient was as soon as something was even a 1% chance hope for me to increase my survival, I jumped at the chance to do it.
That informed consent was difficult because there were seven pages of serious adverse events that could have occurred to me, and my mom’s sitting right with me. She was definitely not happy about those. I had to keep saying these are worst-case scenarios.
These are things that might’ve happened in one or two people that they need to include in the overall spectrum because they don’t know exactly what this drug is going to cause. Going through that was scary, and it was hard to understand because I was still so emotionally flipped upside down.
What made you choose to pursue the clinical trial?
It was more of, if it all went downhill fast and I died, I wanted to be able to feel like I did everything possible. That’s why it wasn’t to give data for further studies, which is a good reason to do it. But it was really selfish, and that’s okay. A very selfish reason for doing it.
One, I felt like they were going to follow me closer. It may not have been true, but I just felt that way because I know that often with local trials, they want to know everything, every little thing. I felt like I might be followed even closer.
Then I was being given an opportunity just to something new that might work better. Hope is a very strong medicine.
For someone going through a very tough regimen and stuff, having hope in anything — that you increase that hope — is something worthwhile.
»MORE: Learn more about the process of clinical trials from one program director
Any advice to others about to go on a clinical trial?
I had a friend come over who audits clinical trials, and she actually diagrammed it out for me so that I would really understand each of the different treatments that I could be on and what it would require of me. That really helped.
My suggestion if you’re going to go onto one is, even if you think you know what they’re asking of you and what’s going to happen and what the possible side effects could be, if you have any questions at all or if you could ask them to write it down and diagram it out for you, the nurse should be able to do that.
The clinical trial nurse has a very intimate understanding of the trial, and that’s part of her job or his job. You should never feel bad about asking for them to give you more information.
Work & Finances
Were you able to work through treatment?
I’ve talked to some cancer patients, and they pour themselves into their work when they’re going through treatment, and that is sort of an escape for them. They can feel normal that way.
For me, I’m a writer. I write fiction. I create worlds in my head, and the only thing that my head could focus on was how I was going to beat this. I tried to start writing these other worlds.
I write historical, so they’re like 16th or 17th century, and there was no way I could concentrate on it. I had to tell my agent at the time that I was going to have to take some time not writing my books. She was wonderful, very understanding, although she works for me. It’s a little different than having an employer.
She gets a percentage of what I earn, but she can decide not to be my agent. It was really hard to get an agent in the writing business, but she was like, “Heather, I know you’re going to beat this. I’m just going to continue to sell your books that you already have out.”
I work longer timelines when we do sell to get the edits done and things like that. She was always very onboard with me and trying to help me as much as I can. I was totally honest with her about where I stood in that there was nothing coming out of this brain except how was I going to live.
Because I am a writer, if I don’t write, I’m miserable. My husband realized that pretty quickly and said, “Okay, then write what you’re going through. Just write.”
So I did. I started to blog, and I blogged all the way through treatment. I am eventually going to make that all into a book for cancer patients.
How to survive treatments in the best way possible and to have a set yourself up to win if at all possible, and it’s very possible. I could not write my regular job, my regular work. In fact, [I was in] the middle of the book, and I just had to stop completely for at least the treatments for 15 months. Probably a little bit after that, I started to get back into it.
»MORE: Working during cancer treatment
How was dealing with finances for treatment?
We were very blessed to have a really good health insurance plan. My husband works for a large company, and so they had a pretty good plan. I was told that they ended up paying for that first year like $250,000 or something crazy. We ended up paying about maybe $18,000 out of pocket that first year.
The clinical trial material and any additional things that they did are supposed to be covered. The Avastin that I was on [and] the clinical trial material was definitely covered.
I think I should’ve probably advocated a bit more to get some of the scans covered by the clinical trial, because I don’t think that my doctor would’ve necessarily asked me to get scans every six months if we were just a regular patient. I ended up having to pay a certain portion of this.
I think my husband dealt a lot with his company about trying to get us some more flex spending taken out of his account so that it was not taxed and that we could use that and help pay off the bills.
It did take me several years to pay off our bills, because every CT scan I got, I would get another $2,000 added to my bill.
Any tips on how to help manage the finances incurred from treatment?
I finally called them. Please know you can do this. Call and ask or talk with their people. I got on a $25-a-month plan, and they didn’t charge me any interest.
As long as I was paying $25 a month, they weren’t charging me interest, nobody was bothering me, and it was totally doable.
It took a long time, and if I did well on a book or something, then I could pay more. I finally paid it off this year.
I have a car that is 15 years old, and we don’t have tons of extra stuff, but we were nowhere near devastated like some people can be if you don’t have health insurance.
We were really blessed, but do know, though, that you can get on one of those plans. The hospital wants to just get some of the money coming in. They would much rather have that, even $25 a month.
Ask about that or have somebody else ask about it. You as a patient should just be worrying really about getting well. That’s your job.

Support & Relationships
Did you have to self-advocate through treatment?
My clinical trial nurse was the one who was my main contact all the time. We talked several times a week. I became so dependent upon her that I would even have nightmares that if I couldn’t find nurse Donna, then I was going to die.
I was searching for her or wanting her, and she would call me immediately if she had results and things like that. She was so very important. My whole team was wonderful.
Towards the end, after I finished the clinical trial material, they still wanted me to do follow-up CT scans. The amount of radiation you get from a CT scan is equivalent — at least this is what they wrote in the informed consent — equivalent to four extra years of regular radiation from being in the world.
Well, I had ten of them. That was like four years of extra radiation. At some point, I said, “Okay, the CT scans have all been good, and I don’t want to just keep doing them because it’s in the protocol for the clinical trial.”
I did have to advocate a bit on my end, and in fact, when I go in and my doctor’s like, “Well, it’s been years now since we’ve done a CT scan. Should would we do one?”
I’m like, “Okay, look, the blood test, the CA-125, if it continues to stay low, which means that there shouldn’t be any active ovarian cancer, then I don’t want to give myself more radiation.”
I had to say nicely but firmly that unless there’s a change in either symptoms or my CA-125 starts going up, I don’t want to do it. They’ve been okay with that.
You just need to think some things through and maybe talk with a friend about it to figure that all out. I talked a lot with my husband about it and talked with other cancer patients about it, and that’s what we finally decided — that I was going to stop all that radiation anyway.
»MORE: How to be a self-advocate as a patient
How did you talk to your kids about the cancer?
When you get diagnosed, you feel like you’ve been hit over the head, smacked in the face, you’ve been run over by a truck, [or] whatever you want to call it. It’s like your whole world is turned inside out.
When you have kids, especially when they’re still in the house, I think it’s even more traumatic because their energy and worry feeds into you and your worry. I can’t hide things, so we let them know what was going on immediately. There was no way they could not see Mom blithering on the couch.
We started telling the kids the plan, and that’s how we referred to it, because different kids would deal with different things depending on where they are emotionally and their level of maturity.
My 12-year-old daughter, this became her mission. Everything became teal, which is the color for ovarian cancer. She was raising money, and she was dedicating anything she did to me and to the cause.
That’s how she wanted things to do, so I asked her to make me posters that we put up in my bedroom. I kept them up for five years, and every day when I woke up, I’d see, “I am strong,” “I am healthy,” “I am growing stronger every day,” [and,] “I am living a wonderful life.”

These posters of positive affirmations, which is another tip eventually I’m going to give. They’re very powerful, and I lived on them during that time. A positive statement that were ‘I can’s,’ so it was like I was reading it to myself.
I asked her to make me posters so that she and her friends went together, and they made colorful posters for my bedroom wall. It gave them something to do.
My middle child, my son, wanted me to promise, “Promise me, Mom, you’re not gonna die.” Don’t promise that. That’s not what you promise. You can’t promise that because he knows mom would never lie. What happens if I did? You just don’t know. You could get in a car accident, so don’t promise that.
What I promised him, though, is that I will always keep him informed and let him know what was going on.
I said, “The plan is Mom is going to do this medicine, and this is what is going to happen to me. I’m going to lose my hair. I’m going to have a really hard time. You’re going to help me, and we’re gonna work. We’re going to fight this together, and the plan is that I will recover.”
But I never promised that I was not going to die. Him knowing what the plan was, that was his form of taking a little bit of control. He is a very sensitive boy, and if I was crying, he would come to my room and ask, “Mom, is it the cancer, are you hurting, or are you just upset?”
I’d be like, “I’m just upset; I’m just scared.” “Okay, okay, do you want me to go get Dad?” Very intuitive, and it made him feel like he was helping me.
My four-year-old is a whole different story. When they’re four, they don’t understand a lot, but she was pretty bright. One tip I wanna give: they ask a lot of questions.
She one time woke up in the middle of the night crying. I went in to see her, and she said, “Mommy, who are you going to play with in heaven if I’m not there with you?” How do you answer that?
Unfortunately, it was three in the morning, and I was groggy, so I think I said something like, “Well, all the other people who have died.” That was not the best thing to tell her, but the thing was that she was scared.
She was very frightened. One thing that we realized that she was frightened about is that I would go to this place every week, and I would come home and be passed out on the couch.
They were apparently doing terrible things to Mommy at this place every week.
We had a cancer patient picnic at the infusion center, and I asked if she could go see where I sit when the other patients weren’t there because patients can look scary to kids — without hair, and maybe either grimacing or something like that.
It was when it was empty, and I was able to bring her in with the nurse, sat her in my chair, and got her a hot chocolate. I suggested that they had cupcakes for the kids. Let them come sit in the chair, look out at the garden, have a cupcake, [and] realize that the people here are smiling. Nobody is out to get me and torturing me, and things like that.
It was amazing because her nightmares stopped after that, especially whenever Mom had to go to the hospital. It wasn’t this big terrible thing any more because she just thought of that chair and getting a hot cocoa while sitting there. “Oh, okay, Mom.” I’m there, gonna come back from there, and sleep for a while.
That really helped in letting her see where I was going. I suggest if you have kids and they’re scared and want to see it, hopefully your hospital has a program maybe where your child can come when it’s an off day, like a weekend, and see the suite where you’re sitting, actually sit in the chair, see it’s comfortable, [and] see that there’s a TV and things like that.
Through the whole thing, we tried to involve them but not scare them. They didn’t need to know all the little tiny things that I was going through.
But there did come times as my treatments went on where I would have to remind them, ‘Mommy is on chemo. Mommy cannot just jump up and run around.’ They would forget that I was in treatment and stuff. That was a good thing; that was a really good thing.
I didn’t want them always remembering that I was hurting or in treatment or scared, but I did have to remind them sometimes. You really have to take care of yourself so you can keep taking care of them. It has to be a little bit more even.
»MORE: Parenting with cancer
You had to be more careful with germs
My mother lived close to me, thank goodness. The [kids] were at three different schools, so I had three schools worth of germs coming home with them.
As soon as they walked in, they wiped their hands. My mother would go through the house, and she would wipe down things. It was amazing. During that whole 15 months, we were like the healthiest we’ve ever been because there were no germs getting into the house, not with my mother at the door.
That’s something also to keep in mind, that you need to be a little bit aware of the germ factor that comes with kids.
Did you have to get outside help with the kids during this time?
Yes, I have an army of help. My youngest was in preschool, and the preschool teachers would take her home with them after school numerous times, especially if was having chemo that day. I would have somebody take me to chemo, and then I’d have other people taking care of my youngest.
My older ones were a little bit more self sufficient, ages 10 and 12. They were a little bit easier. Again, my mother lived right around the corner, so she was here on a daily basis making sure. She took over “being Mom” a lot of the time.
My husband would do as much as he could, but we needed him to keep working to provide that great insurance.
For four months, three days a week, people brought in a meal. A counter was set up by a neighbor. People that I didn’t even know were sometimes bringing us stuff. It was fabulous.
The outpouring of love is one of the perks of cancer. I have a lot of perks of cancer, one of them being that you can wear really big earrings. Everybody thinks they’re cool.
The other is the outpouring of love that you see in people. It fills you up.

How did the cancer impact your relationship with your husband?
I’ve seen some relationships go down the tube because of cancer. Unfortunately, I’ve seen people split up. Some of the people I was in therapy with [and] treatment with, they ended up in divorce because the husband, wife, or whatever couldn’t handle it.
I was lucky when it comes to that. My husband worked really, really hard to battle this with me. He would take really good care of me. If I couldn’t walk, he would carry me up the stairs and help me. I think that it really brought us closer together, actually, in a way that nothing else could.
We were fighting tooth and nail — literally, because my teeth were loose, and my nails were falling out. We were fighting to keep me going, keep me alive, and keep our world from falling apart even further. I do remember laughing a lot with him, him helping me that way, and him also holding me and letting me just sob.
One thing that was really helpful to me is that I would go to him and just say, ‘I need to hear the words.’ He would hold me and say it would be okay, ‘We’re doing this. It’s okay; what you’re feeling is okay. You’re strong.’
He had a litany of things that I just needed to hear again. One time I said, “I am so scared,” and I’m just crying. He says, “Look, I’m on the other side, and I’m terrified, so I can’t even imagine what it’s like being in your shoes, being that terrified.”
Just him knowing that and I guess validating my feelings that it was okay to be so scared — that I wasn’t a weak person because of that — was so important. That just helped me. He was a very caring person, but he does joke a lot.
I watched no news. I watched nothing that had sad stories in it. Oh my gosh, I accidentally started watching a movie that had a mother die of cancer in the beginning. It just threw me off. He was very careful then after that, watching for those type of things.
»MORE: 3 Things To Remember If Your Spouse/Partner Is Diagnosed With Cancer
Cancer’s impact on the sexual relationship
Our relationship was great. It really was. Now, sexually, everything was downhill. He was afraid to touch me because I’m hurt everywhere.
First of all, I wasn’t allowed to for a while. Nothing you’re going through makes you feel sexy at all. I’ve lost my hair, I’m on so many steroids, I had gained 40 pounds on steroids, I had a moon face, and I’m almost like a hunchback from the steroids.
I was on too many steroids because I couldn’t walk without them, and my body was just reacting very poorly to the chemo. But he still said I was beautiful and stuff, and that was nice. There’s nothing sexy about cancer.
I was also in instant menopause, so I was having hot flashes, like sweat-through-everything hot flashes, continually. Compared to chemo stuff, it was nothing. It was fine. I’d sometimes have to change the sheets in the mornings because I’d sweated through everything during the night, and he would help me.
One time, I would stand on one foot and then the other because my feet hurt so bad from nerve pain that I couldn’t stand on my feet for very long. I’m standing at the counter, one foot up. Then I stood on another foot, and he made a joke about me being a flamingo.
I started to laugh, and I said, “Don’t make me laugh because my bladder’s full.” If you’re on chemo, that’s another side effect, that your bladder’s not as strong. All your muscles are not as strong.
I said, “Do not make me laugh,” and of course he did something else to make me laugh. All of a sudden, I just peed all through my clothes, just whoosh. I had this pee all the way through my clothes.
I was in the kitchen, I looked at him, he looked at me, and we both just started cracking up, just laughing hysterically, which of course made me pee even more.
He sent me up to take a shower, he cleaned up the floor, and I knew right then and there that that was true love. That’s what true love looks like right there.
Cancer is a horrible, horrible thing, but another perk for me was that it made our relationship even stronger because we were working together and trying to help each other.
I was trying to help him deal with remembering his mom dying and that I was not his mom, and I was trying to get him not to keep looking at the internet. He even went out and planted me a garden so I could sit in it. He hates yard work, so I know that that was a [release].
He said later he just couldn’t be in the house all the time; he needed to get that energy out.
It’s important caregivers take care of themselves
I did ask him to please go talk with your friends and things like that, and he didn’t want to join a support group for anything, although I do know some spouses that do that.
That’s a good thing. It is definitely an up and down sort of thing, but I’ve always felt like he was right there with me, which is something that not everybody gets, so I was very lucky with that.

Ask people for support — they want to help
When you’re diagnosed, people are devastated with you — your family, your friends. I ended up hearing stories later about how they heard and how they started crying and all this.
I was a very independent woman. I had it all together. I could drive my kids, I could take care of them, I got the dinner on the table every night, and I was working. It was really hard for me to let go of some of that.
But the thing I want you to know is that these people who are all so devastated need something to do. They need something to feel like they’re contributing and helping you, because they’re lost. They’re lost for your loss.
If you say, “Meals for my family would be great. If you could try to set up something on CaringBridge or a meal plan, that would really help out,” that gives them something to work on that they feel like they’re contributing to helping you.
If they can drive you to chemo or they can sit with you for your six-hour infusion, hold your hand when you get stuck, those types of things.
Even cards. I have a hundred cards, and I saved them all. I stick them on the door to my bedroom. Even if somebody would cut me flowers from their garden and leave them on my front porch. Someone left bagels on my car.
There are all these little things that people did to just let me know that they were rooting for me, and they really did want to help because it gave them something to do. They felt not as powerless as they were feeling when you got diagnosed.
Just ask for help.
Any last advice to people dealing with their own diagnosis?
I did write a blog post. It’s called “Don’t Look at the Rock.” When I was newly diagnosed about three weeks after my surgery, my best friend took me for a walk, and we were walking around while the kids played.
She had her arm linked with mine because I would get these spasms where I suddenly couldn’t breathe, because it was still healing. I’d say, “It’s the fear. This fear, I just can’t get away from it, and I just keep looking at this fear.”
She was a bike rider, and she said:
Heather, have you heard about the advice called ‘don’t look at the rock’? When they go mountain biking, if there’s a rock in the path, you know you have to get around the rock. If you stare at it, there’s a really good chance you’re gonna hit it.
And the same goes if you’re walking in the mall and you see someone coming at you. You’re looking at them and you’re trying to go around them, and you end up dancing back and forth because you don’t know which way to go. It’s that same thing. You stare at something; you tend to move toward it.
I’m not saying that you’re going to move yourself to cancer, but what I’m saying is that the fear is there, and it’s like the rock. And if you stare at it, you just fall more and more into it, and that doesn’t help you physically. It really doesn’t.
So you want to look beyond the rock, around the rock. You know it’s there, but stop writing the obituary in your head.
I’m a writer, so my obituary is going to be fabulous because I’ve written it so many times in my head. That is not a good thing to do when you’re scared and when you’re going through all that. You want to look beyond.
I think one piece of advice is create your healthy, older self in your head. Come up with a picture of how you view yourself as an older human being, maybe in your 80s or whatever, and a healthy person [at that age].
So I created this picture: We have a house up in Maine on the ocean that we inherited and we were rebuilding, so my happy place is a picture of me. I’m older, I have gray hair, and I have a long braid down my back, and I’m standing wearing a cardigan and loose trousers with elastic because that’s what older women wear.
I’m standing, looking over the ocean, and I can hear my grandchildren running around me. They’re diving their hands into my cardigan pocket to look for the sea glass that I always keep in my pocket.
I can hear the seagulls calling overhead, and my husband is standing there holding my hand. And that is me as a healthy 85-year-old, and I’ve beaten the cancer.

When I would start to hyperventilate and get really scared again, I would look past that rock, and I would look at that happy place. I would focus on it, and I would hear my grandchildren laughing, which I don’t have yet, so I think they’re made-up grandchildren. I would hear the seagulls calling.
That became such an important thing to me that my husband even flew me up to Maine when I was in the middle of chemo. In between those weekly chemos, he got me up there for three days so that I could stand there and put that in my head, because it’s such a powerful tool, trying to look beyond that fear, beyond that rock into a successful outcome, telling yourself every day with positive affirmation, “I am living a long and healthy life.”
Those things that you beat into your brain as a mantra is extremely powerful medicine that you can do yourself. It’s setting you up to succeed, and that’s what we wanna do.
The doctors are fighting the fight with the medicines and all that, and you are fighting the good fight with your emotional medicines. Do try to do something like that because I really felt that that helped me.

Inspired by Heather's story?
Share your story, too!
Ovarian Cancer, Epithelial Stories
Heather M., Epithelial Ovarian Cancer, Stage 2
Symptoms: Extreme bloating, pinching pain in right side of abdomen, extreme fatigue
Treatments: Surgery (total hysterectomy), chemotherapy (Taxol once a week for 18 week, carboplatin every 3 weeks), concurrent clinical trial (Avastin) every 3 weeks
...
Jodi S., Epithelial Ovarian Cancer, Stage 4
Symptoms: Extreme bloating, extremely tight skin, changes in digestive tract, significant pelvic pain, sharp-shooting pains down inner thighs, extreme fatigue
Treatments: Chemotherapy (pre- & post-surgery), surgery (hysterectomy)
...

One reply on “Heather’s Stage 2C Epithelial Ovarian Cancer & Stage 1A Uterine Cancer Story”
Would love to chat – was diagnosed in September 2020 with ovarian cancer – have been praying and seen doc x