Gautami’s Stage 3B Germ Cell Tumor Pediatric Ovarian Cancer Story
Gautami shares her stage 3B ovarian cancer story and how she got through getting diagnosed at just 13 years old. While she was in school, she had to undergo surgery and chemotherapy.
In her story, Gautami also dives into how she managed with hair loss and the issue of fertility preservation. She also gives guidance to other AYA (adolescent young adult) cancer patients. Thanks for sharing your story, Gautami!

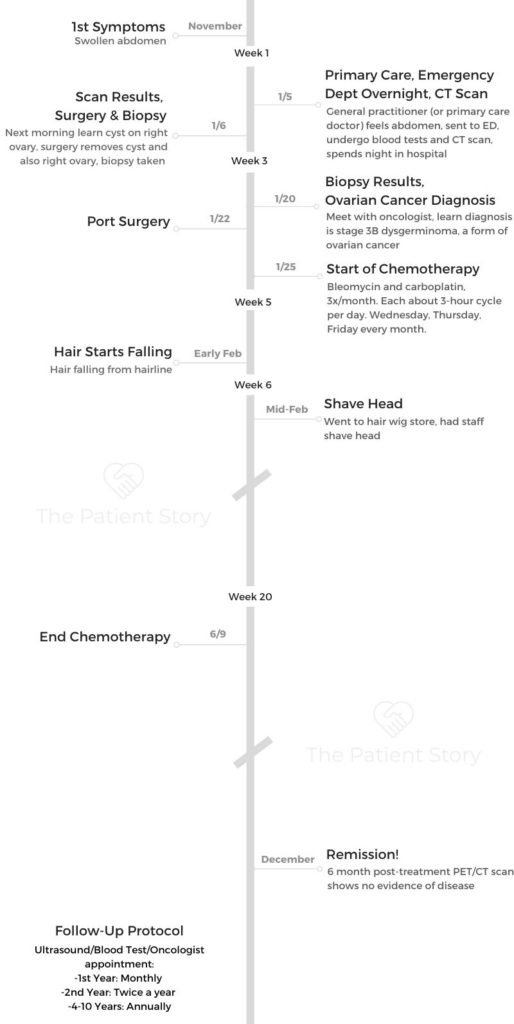
- Name: Gautami M.
- Diagnosis:
- Ovarian cancer
- Germ Cell Tumor
- Stage 3B
- Pediatric
- Ovarian cancer
- Age at Diagnosis: 13
- 1st Symptoms:
- Swollen abdomen
- How diagnosis happened:
- Went to doctor for abdomen swelling
- Immediately sent to emergency department
- Scan reveals cyst on right ovary
- Treatment:
- Surgery (to remove cyst and ovary)
- Chemotherapy
- Bleomycin
- Carboplatin
- Three days in a row each month
- Three-hour cycle per day
I’m not going to lie, cancer is a really tough experience. It has its highs and its lows. There are going to be days that are going to be terrible.
I think it’s about giving yourself the space to grieve, the space to experience it. It’s your story, and you get to choose how it goes.
Just give yourself that time to adjust. Be kind to yourself, knowing it’s only temporary.
Gautami M.

- First Symptoms, First Steps
- Surgery and Biopsy
- Ovarian Cancer Diagnosis
- Chemotherapy and Side Effects
- Describe the chemotherapy regimen
- How was the port surgery?
- You get blood labs before infusion
- What were the chemo side effects?
- What helps with the chemo side effects?
- Do the side effects get better or worse?
- What helped get you through chemo the most?
- When does your hair start to fall out after chemo?
- How did you decide to shave your head?
- What helped you process losing your hair?
- Scans and Results
- Getting and Giving Support
- Adolescent Young Adult (AYA) Cancer Patients
- Juggling school and chemo
- Immunocompromised
- Advice to young cancer patients on not having hair in public
- How did you approach the issue of preserving fertility?
- Polycystic ovarian syndrome (POS)
- POS medication side effect
- Body positivity and language
- What can we all do better?
- Message to parents of pediatric cancer patients
- Communication as a pediatric cancer patient
- Last message
This interview has been edited for clarity. This is not medical advice. Please consult with your healthcare provider for treatment decisions.
First Symptoms, First Steps
First symptoms
Because I was so young, I thought everything was fine and normal. It was really my mom that noticed that my abdomen was getting quite swollen. Apart from that, I didn’t really have any symptoms.
I was losing a lot of weight everywhere else except for my abdomen. That’s what prompted us to visit our general practitioner.
It was pretty noticeable. Honestly, looking back, I looked three months pregnant, and that’s obviously not what it was with someone who’s 13 years old.
Primary care visit
I went to my GP, and she instantly knew something was wrong. I could tell based on her face. She palpated my abdomen and said I had to go to the emergency department. Something was really wrong.
Because it was so swollen, she said she definitely could feel there was something inside. Whether that was fluid, a cyst, she didn’t specify. I think that’s where the train of thought was going.
From there, we went straight home, packed an overnight bag, and went straight to the hospital.
Checking into the emergency department
We got to the emergency department. I was still feeling pretty healthy and fine for the most part, so it didn’t feel like anything was wrong. We waited in the emergency department for a couple hours, then we went in, had a blood test, urine test. They asked me a whole bunch of questions.
I felt fine, so I was answering no’ to a lot of the questions they were asking me.
They said I was going to have an ultrasound, but because they were a bit worried, I instead had a CT scan. By this time it was probably 12 at night.
I went to the CT scan, and after that I came back [and] went to sleep. The next morning is when they told me they had to do surgery.
CT scan results
Woke up early the next morning. I had two doctors come in, sit me down with my parents, and say they found a cyst on my right ovary, and they had to remove it the next day because they were worried about the size of it.

Processing news of a cyst
I spoke to my mom about this because she came with me to get the CT scan. My dad was sleeping. She said she saw the doctors looking at the scan results, and they looked shocked.
She knew then that something was wrong. But when they were telling me, my parents were obviously really upset. That’s how I knew something was wrong.
I felt really calm, and I don’t know if that’s because I was 13 and couldn’t take in the full gravity of the situation.
I remember the doctors telling me, and I said, “Okay, sounds good.” They looked at me, and they were like, “Do you understand what we’re saying to you? Can you repeat it back to me just to make sure?”
But I felt relatively calm and okay. I think just being so young, it protected me from truly feeling the emotions that I was supposed to be feeling then.
There was shock as well, because things had happened so quickly. I still felt fine, so I think that made me feel like it was going to be okay.
They didn’t know it was cancer. I don’t know if they had any inclination to believe that. All they told me was there’s a cyst, and they were going to remove it. I know there was a plan to take a biopsy from it as well.
Surgery and Biopsy
Surgery to remove the cyst
I got moved to a different ward. The next day is when I was supposed to have my surgery. I woke up the following day, got wheeled straight into surgery, talked to the surgeons and nurses before I went in, and that’s when I had the surgery to remove the cyst.
They ended up removing my right ovary. Also, that’s when they took the biopsy. I think it was about six hours long.

How did you feel waking up from surgery?
I remember waking up, and it was the most drowsy I’d ever felt in my life. I also had an epidural and morphine, so I was really drugged up. I felt the most intense pain in my abdomen, and I remember crying because of how painful it was.
Heaps of people surrounding me as well, because I had all my family and extended family in the hospital room. It was all a very intense experience.
They sorted out my medication, and I started to feel a little better. I was numb for half of my body because of the epidural, so I couldn’t feel too much.
How long did the pain last?
The pain didn’t last too long because as soon as they adjusted the medication, I felt better. I had that for about a week.
Then they took out the epidural and lowered the doses of morphine as well. So, I’d say about a couple days.
Surgery recovery in the hospital
I was in the hospital for about three weeks. I needed the time to recover because I remember the day I went home, I was almost ready to be back to full health but wasn’t quite there yet.
Ovarian Cancer Diagnosis
When did you get the biopsy results?
It was three weeks later. I know my parents were told about it earlier, but I think they wanted to give me time to recover.
I was told on the day I was being discharged.
Ovarian cancer diagnosis, stage 3B
This is a day I remember quite well. I was sitting in this white room, a conference room, with my oncologist and one of the other doctors, my parents, and one of our family friends, who’s also a doctor.
I don’t remember it that clearly, but my doctor just told me that what they’d found from the biopsy was that I had stage 3B dysgerminoma, a form of ovarian cancer. That’s how I was told.
It was very overwhelming. I felt like time slowed down. All I could feel was the word ‘cancer.’ I don’t remember anything else except that word from that moment.

How did you process the cancer diagnosis?
I felt very scared but also reassured to know that I had a really good medical team and a really good healthcare system, all of the best medication being provided for me.
That definitely made me feel better. Especially being so young, you have this belief that everything’s going to be okay. Medication will help you, as it always had helped me in the past.
I just felt it was the same thing. I think I was in a state of shock. I only really felt the true emotions of it as the months went on in realizing how it affected my life.
I think the diagnosis itself is scary, but realizing how much it affects you, that’s when you actually get to react to the diagnosis.
Treatment plan
They said they would discharge me on the day and I’d come back about a week later. They would discuss my chemotherapy treatment plan at that point.
Waiting for cancer treatment to start
I remember going home, and it was a really beautiful day. I just felt annoyed because I felt my entire life had changed, and everyone was going about their lives as normal.
I was still recovering from the surgery and adjusting to the fact that I had cancer, that my whole life was different.
I found it really difficult, but at that point, it was really nice to have the family support and extended community support. I think that really got me through all of it and not just that week.
Oncologist meeting
I went back in. It was pretty clinical. They told me the types of medications that I would be having, how often I’d be having it, [and] how often I’d be having my blood tests, my scans. That was the process and opened the floor for me to ask questions.
Questions you wish you’d asked at that appointment
I wish I had asked questions about my fertility because that was obviously something, having ovarian cancer, that would be affected.
I wish I’d asked questions about my hair, how that was going to go, what to be expected from that. Also, just anything I could have done additionally to treatment to help myself.
The question I wish I’d asked the most was getting support for my mental health because it’s a thing I didn’t think about.
I potentially was briefly asked about it during treatment, but I wasn’t open to it. I wish I had just known what was available to me to support me in that way.
Chemotherapy and Side Effects
Describe the chemotherapy regimen
I had bleomycin and carboplatin, the two chemotherapy drugs. I would have them three times a month. Each was about a three-hour cycle per day.
It’d be a mix of both of the chemotherapy drugs. It was three days in a row — Wednesday, Thursday, Friday — every month.
How was the port surgery?
I got a port inserted at the start. When I went back the week after the surgery, sometime around then is when I got the port inserted. I think it depends on your level of comfort on having something inserted.
Because I was relatively okay with medical procedures, I found that quite all right. But there’s no pain, there’s anesthetic, [and] you’re not going to feel anything. It is a little sore after you wake up, so you might feel some pain there. Apart from that, it’s a pretty easy process.
It is a bit weird because when you have the infusion, they do put a needle into the port. They numb it as well, but it is a weird thing to see, a live needle being inserted into you.
But the whole process should be painless, and if it’s not, it’s something you should talk to your medical team about.
You get blood labs before infusion
I would have them done before the first infusion just to make sure my immune system was healthy enough to handle the chemotherapy treatment.
What were the chemo side effects?
About a week after my first chemo cycle, I started feeling the fatigue to the point where taking a shower, I could not stand up or move. I’d be so tired.
I also felt bad breath was a part of it, which was not a good side effect. My nails turned gray. I did feel nausea in the first one pretty badly, so I was throwing up, but I was put on anti-nausea medication, which helped incredibly for the rest of my treatment.
I still got nauseous, but I didn’t throw up. So nausea and fatigue were my two biggest side effects.
»MORE: Cancer patients share their treatment side effects
What helps with the chemo side effects?
When I would start my treatment, that’s when I’d start to take my anti-nausea medication. It definitely helped.
It should be a relatively painless experience. The medication is there to help you.
Do the side effects get better or worse?
They were relatively the same, except for the nausea because of medication. Apart from that, the fatigue was there the whole time.
What helped get you through chemo the most?
Physically, it was having good, open communication with my medical team. Socially, my mom came to all of my appointments, and that definitely helped. I don’t think I could have done it without her.
Having a good support network was the most important thing throughout it, not just my family, but also having friends that knew what I was going through and being able to talk to them about it.
When does your hair start to fall out after chemo?
It was a couple weeks after (my first cycle). That was when I first started losing my hair. It wasn’t all of it. A month after my first treatment is when I noticed it was really falling out of my scalp.
You could see it coming out of my hairline. That was definitely one of the hardest things throughout the cancer journey.
How did you decide to shave your head?
When my hair was falling out of the hairline, that was when it was very noticeable, and I couldn’t cover it up anymore. That’s when I decided I needed to shave it off and I’d rather wear a wig instead.
It was more that I didn’t like how it looked, and I knew that there was no way I could hide it anymore. If I wanted to look more “normal,” it would be best to get a wig.
»MORE: Dealing with hair loss during cancer treatment
What helped you process losing your hair?
Just knowing from an early stage that this was something that was going to happen, just grieving the process of losing your hair. It’s something that I think you take for granted.
Giving yourself that space to think it is just hair, but it is really an important part of the way that you look. It’s okay to be sad about it. I definitely had more than one cry about losing my hair.
Being open in how you feel about it. I wish it’s something I had done more of and talked about it more with other people. Getting a wig helped a lot.
Scans and Results
Describe the ultrasound
I would have an ultrasound and blood test every month. It meant I’d have to drink a lot of water before, so that’s how the scans worked. The best way to do this is to drink about a liter and a half about an hour before your scan.
That way when you have your scan, you’re ready, instead of drinking lots of water right up until your scan, because you’ll really need to go to the toilet, and it’s not a fun experience.
The ultrasound was about 20 minutes. They would scan my lower abdomen and look around at my one ovary that was left and the space where the other one was, looking for cysts or any abnormalities there.
They said they needed to keep following it up because during the period, especially after I stopped my chemo treatment, to see what was happening and if the cancer was coming back, see if there were any changes they needed to get ahead of.
No evidence of disease
Six months after my treatment, it was official that I was in remission.
There was no evidence of the disease, so they were not going to restart me on any kind of treatment, and they were going to be following up.
Reaction to the news
When they told me, my parents were ecstatic. They were obviously so happy that this was coming to an end. It was interesting because when I think about the experience, I remember sitting in the room and them telling me this news.
I almost felt nothing. I knew I was supposed to be happy. I was happy that it was over, but I didn’t feel the sense of happiness. I felt this emptiness because you go through this whole process that’s incredibly life-changing and so emotionally draining.
You don’t even have enough time to stop and think about how you’re feeling.
All of a sudden it’s over, and everyone expects you to go back to normal life, be the same person when you’re really not. Not to sound dramatic.
I didn’t emotionally process it, to be honest. I felt a sense of wanting to go back to normal and wanting to be the same person I was before this. The only thing that really helped me through it was having my family and friends’ support throughout it.
Follow-up protocol
The follow-ups would be the ultrasound, blood test every month, and also an appointment with my oncologist. I had them monthly for about a year, and then it went down to six months for the next year, then yearly, then every two years. Now I’m done with all my scans, the start of last year.
Getting and Giving Support
Delegating communication to others
I was young, so my parents handled everything. I only told a couple friends. Apart from them, my parents told everyone else that needed to know.
I think if it is someone younger, it is better to direct the more intense questions to the parents. I wouldn’t want to repeat myself or think about it all the time.
Asking for support
Looking back, I don’t think I asked for help enough.
If I was to do it again, hopefully never, I would put in place a lot more mental health support systems and be more open to talk about what I was going through. It’s something I didn’t do enough of when I was going through it.
I wish right from the start I was talking to a counselor or therapist, someone in that field. Even if I wasn’t feeling the effects of it yet, it was something I was definitely going to feel and continue to feel after it was all over.
I think that would have been important. Having more open conversations with my friends and my family about what I was going through.
»MORE: What kind of support cancer patients say helped the most
Give patients some space
When someone is unwell, you obviously want to be there for them and know that it’s going to be okay, but I think holding off on that is important because it definitely was overwhelming, as much as I appreciated it.
In the moment, being so drugged up and in pain, it’s not what I wanted at the time, as much as I loved and appreciated everyone that was there for me. Possibly just coming in a bit later or waiting or coming in one at a time would have been a lot nicer experience for me.
I think the support is very, very important because I don’t think I would have been able to get through these three weeks without visitors coming and constantly pouring into my room. But I think right at that initial stage, it’s important to give a little bit of space while I was recovering from the intensity of it and just getting used to the fact that I was in hospital.
Just because of how fast things had moved, I needed time to adjust.

Adolescent Young Adult (AYA) Cancer Patients
Juggling school and chemo
It really helped because the school was very supportive, so they were open to me taking breaks or being able to go home in the middle of the day.
How my body responded to the chemotherapy was the biggest thing. It didn’t have this major effect on me, so I was able to continue doing things like that.
Immunocompromised
I took a couple of days off during the six months, but overall it was okay. My doctors were definitely nervous about it because if I got any kind of illness, it would be really bad.
That was just a risk that I was willing to take because I needed to have that routine. I needed to have school to feel normal to get through the treatment. I don’t think I would have gotten through it if I had to stay home or do something different.
Advice to young cancer patients on not having hair in public
I definitely would have looked into more options of having wigs because it is quite a wide range in having something more secure. When you’re in school, you’re moving around, going to PE, doing all that kind of thing.
Just having a wig that’s secure makes you feel comfortable and beautiful. It’s important, so putting some effort into that because it does matter how you look. It affects how you feel. Not writing it off as something that’s not as important as other things you’re going through.
How did you approach the issue of preserving fertility?
Personally, my fertility was a difficult experience throughout all of it. It was hard not knowing a lot of the time. The uncertainty that cancer brings is definitely a difficult thing to embrace. What I learned from it is a couple of things.
When I was going through it, I realized thinking about losing my fertility impacted me so much because I think so often we tie femininity to fertility.
We think losing one means losing the others. Learning those two aren’t as interconnected as we are told to believe. Realizing, ‘You know what? Even if I didn’t have my fertility, it doesn’t make me any less a woman or feminine and doesn’t mean I can’t have children.’
Trying to learn that at a very young age was very, very difficult. Given that point, it’s important to have those conversations with people you trust and with your medical team about the best steps you can take forward.
»MORE: Fertility preservation and cancer treatment
Polycystic ovarian syndrome (POS)
Along with the ovary being removed, I also have polycystic ovarian syndrome that also affects your fertility. I was on medication for quite a while to help with the symptoms of that.
Now I’ve been told that I don’t have to take any medications and my body should be okay. I should be okay to have children if that’s what I choose.
It’s a syndrome which means there’s an imbalance of hormones in your body, slightly more male testosterone than normal for a normal woman. The symptoms that come along with it are typically things like hair on the face, darkness (hyperpigmentation).
Those are the two that stick out the most to me. It’s typically something you might have forever, but they gave me medication to help with the symptoms.
That happened about nine years after I started taking medication, so it definitely was a very long time.
POS medication side effect
I was on a contraceptive pill from when I was 13 till about last year. I think that definitely had an impact on my mental health and how I was feeling. Just because I was on it from such a young age, it was hard to tell what was baseline for me and how the medication was affecting me in terms of my mental health.
That’s something that’s important to track if you start taking medication like that.
Body positivity and language
A lot of the advocacy I do now around ovarian cancer is just removing the taboo of talking about women’s bodies. I think that was a big barrier for me to talk about some of the symptoms I was experiencing.
There is a sort of shame that’s tied to having feminine problems and even having issues with your fertility, when they just shouldn’t be.
It’s about re-normalizing that, and even with parents and children, normalizing how you talk about your body. The names we call our body.
Just being able to have those open conversations because I think if I was able to do more of that growing up, I would’ve been able to talk a lot sooner about the symptoms I was having.
Obviously it’s not one person to blame. It’s just a societal issue that we do have, that we struggle to talk about. Things that are wrong with us, especially when it relates to your vagina, ovary, or things like that. It’s very hard to speak about.
What can we all do better?
Calling body parts what they are instead of giving them nicknames. That inherently implies that something’s wrong with them.
I think that would have been a really important thing to have, to just call body parts what they are.
Especially describing them to children, even when they’re young, and helping kids identify what’s normal for them and what’s different.
How your body should be functioning. If I had known what my baseline was, I would have known I was way off my baseline when I was diagnosed.
It would have helped me get diagnosed earlier. Even the conversations we have around fertility and the importance that‘s so tied to it. Reminding us that it’s not everything.
Message to parents of pediatric cancer patients
Just being supportive and open to listen to things. Reminding them it’s okay to grieve the process, that it’s okay to be sad throughout it.
Just creating those safe spaces for your children to come and talk to you, but also giving them that space to adjust and heal on their own. Not wrapping them in cotton wool and making sure they can’t do anything.
Having a routine and having a normal life was such a big part of my recovery. I don’t think I would have recovered as well if I didn’t have that. Letting them do as much as they can do, as long as they’re being safe. I think that’s important.
Communication as a pediatric cancer patient
Being open about everything that was happening and helping me make those informed decisions is important because although I was young, I think it’s important to have a voice in the treatment. Knowing at all points what is happening and what’s going to happen next. Just making sure the child is a part of the journey, too.
Last message
I’m not going to lie, cancer is a really tough experience. It has its highs and its lows. There are going to be days that are going to be terrible.
I think it’s about giving yourself the space to grieve. The space to experience it. It’s your story, and you get to choose how it goes. Just give yourself that time to adjust.
Be kind to yourself, knowing it’s only temporary.

Inspired by Gautami's story?
Share your story, too!
Ovarian Cancer, Germ Cell Tumor Stories
Gautami M., Germ Cell, Stage 3B
Symptom: Swollen abdomen
Treatments: Surgery (to remove cyst and ovary), chemotherapy (Bleomycin, Carboplatin)
...