Doubling Down on Hope: Kim’s Experience with Stage 4 Clear Cell Ovarian Cancer
Kim’s experience with ovarian cancer demonstrates the complexity and unpredictability of this diagnosis. She was previously diagnosed with stage 2 clear cell ovarian cancer, the least common ovarian cancer subtype, and it has now progressed to stage 4. She describes not only the physical challenges presented by the disease, but also the emotional and personal hurdles navigated alongside her family and care team. From her initial diagnosis to multiple recurrences and rare skin involvement, her story highlights the importance of early detection, clear communication, and a strong support system.
Interviewed by: Keshia Rice
Edited by: Chris Sanchez
After initial treatment and periods of remission, Kim faced several recurrences, with the ovarian cancer spreading to lymph nodes in her groin, lungs, and near her heart. One of the most striking aspects of Kim’s clear cell ovarian cancer case is its manifestation on the skin, a presentation affecting less than 1% of patients. Navigating her treatment path, Kim and her care team carefully weighed the risks and benefits of continuing chemotherapy, ultimately deciding to pursue a clinical trial, seeking both effectiveness and a better quality of life.

Throughout her experience, Kim has leaned on her wife, parents, and extended community. The emotional impact of her diagnosis and recurrences was matched by practical concerns around managing side effects, family conversations, financial matters, and the uncertainties of clinical trials. Kim candidly discusses the challenge of shifting from caregiver to receiving support, particularly as a woman often focused on taking care of others.
Kim’s story is a testament to the resilience of patients facing clear cell ovarian cancer. By sharing her daily struggles, moments of hope, and personal reflections, Kim encourages fellow patients and their families to seek support, stay connected, and remain open to the possibility of brighter days.
Watch Kim’s video and read her story below to learn more about how:
- Quality of life considerations are central when making treatment decisions, especially after multiple recurrences
- Support systems, both family and medical teams, play a vital role in sustaining a person through each stage of the cancer experience
- Every patient’s experience is unique, and openness to clinical trials may lead to expanded options and new hope
- Patients are not alone. Seeking help and sharing their experiences can foster connection and resilience
- Kim moved from being a caregiver for others to accepting care herself, demonstrating courage and grace in vulnerability
- Name: Kim C.
- Age at Diagnosis:
- 40
- Diagnosis:
- Clear Cell Ovarian Cancer
- Staging:
- Stage 4
- Symptoms:
- Coughing
- Incontinence
- Severe bloating
- Nighttime pain
- Hard lump on right side
- Appearance of rash on chest
- Treatments:
- Surgeries: radical hysterectomy, lymphadenectomy
- Chemotherapy
- Radiation therapy
- Immunotherapy
- Clinical trial


Thank you to AbbVie for supporting our patient education program. The Patient Story retains full editorial control over all content.
This interview has been edited for clarity and length. This is not medical advice. Please consult with your healthcare provider to make treatment decisions.
- About Me
- Discovering That My Cancer Had Recurred
- Receiving Prognosis and New Treatment Recommendations
- Deciding About Chemotherapy
- Joining a Clinical Trial and Finding Hope
- Self-Advocacy During Treatment
- The Impact on My Family
- Program Highlight: A New Era in Platinum-Resistant Ovarian Cancer Treatment Options
- The Importance of a Supportive Care Team
- Platinum-Resistant Cancer and Treatment Options
- Lessons I’ve Learned About Myself
- My Message to Others Facing a Recurrence
- Navigating Identity as a Woman and Caregiver
- My Final Reflections: Staying Hopeful Through Hard Times
When you go through a storm, you’re not alone.
Kim C. – Ovarian cancer patient
About Me
Hi. My name is Kim, and I am from Arkansas.
I was previously diagnosed with stage 2 clear cell carcinoma of the ovary, and it is now stage 4.


Discovering That My Cancer Had Recurred
We have the CA-125 test, which is a diagnostic test, and that started to go up. I’ve had three or four recurrences so far. The last time, I had a PET scan; it revealed a cluster of lymph nodes in my inguinal area, which is my lower right groin. Those just appeared. I had just had surgery to remove one, and then more popped up. The PET scan also revealed that I now have two cancerous lymph nodes in my lung and one close to my heart.
Then something odd happened. This is clear cell carcinoma, known as the zebra or unicorn of all ovarian cancers. I developed a rash on my chest. I had radiation earlier this year along my chest and under my arms, so I thought the rash was from that. They did a biopsy, and I now have clear cell ovarian cancer on my skin, which is extremely rare. We looked it up; maybe 0.9% of all ovarian cancers present in the skin, which is very odd.
Receiving Prognosis and New Treatment Recommendations
So, this was two or three weeks ago. We found this out and went to the doctor. I knew what this meant. I knew this was not going to be a good doctor’s appointment.
My parents and my wife, Jennifer, went with me. The doctor, as professionally as she could, told us, “We’ve been on this cancer journey for four years now, which is two years longer than what we anticipated.” She said, “I could put you on chemo. It might work. You’ll probably feel sick. Your quality of life really isn’t going to improve. We might buy you a little bit of time. What I really suggest you do while you’re feeling ‘good’ is take this time off work. Go on long-term disability. Do all the fun things you’ve ever wanted to do while you feel good enough.”
I work for an amazing company with amazing benefits. That’s what I did. We are getting ready to do some fun things and have some special plans.
Deciding About Chemotherapy
When I heard the doctor say we could do chemo, she had tears in her eyes. She said, “I am worried.” I felt it. It was like an out-of-body experience.
I knew with this cancer, it wasn’t if this time would come, but when. We had come to terms with the idea that this would be treated more like an autoimmune disorder, where our goal was just to stay ahead with treatments. When she told me that the only other option was harsh chemo, it was numbing. I’m still processing it. It’s a scary feeling when a doctor tells you that. My family was there, and they kind of went through a similar experience, just, “holy cow.”
It’s a quality-of-life issue, because I’ve already had chemo in the past; one round of six cycles as frontline chemotherapy, then another six cycles more than a year later. Each time, it was really harsh on my body. I was hospitalized because my platelets and other counts crashed. I had blood transfusions. To put my body through that again might be even worse this next time.
You have to weigh it out: Is it worth it for just a little more time? Or do you want quality of life, great memories, and to do all the things you can?
The doctor also said that there was a medication, a pill that could target a certain gene mutation I have, but she didn’t have high confidence in it. She really wanted to get me into the clinical trial over chemo because chemo is just so tough on the body.
Joining a Clinical Trial and Finding Hope
In all this craziness, there is some good news. We found a clinical trial for me. I’m in the process of all the necessary testing to make sure I qualify for it, and that what they’re testing is likely to work. If everything goes well, I’ll start treatment in the clinical trial in less than a month.
We are really praying, hoping, and keeping our fingers crossed that everything will work with minimal side effects. Because chemo is really hard, and I don’t want similar side effects, but that’s where we are right now.
At first, I was thinking, “It’s a trial. The FDA is still working on it. It’s a science project.” And it is truly science; they need people to go through these trials to ensure that the medicine works. On one hand, I’m honored to help the future of women with this terrible disease, but on the other hand, I wonder what it will do to my body. Will I have side effects, or will I just buy a little more time?
With chemo, you go through six rounds, and by round four, you feel really bad, but you know, “I just have two more.” This clinical trial is indefinite: you can opt out if your body can’t handle it or your tumors aren’t shrinking, but the goal is to shrink the tumors. It’s kind of a gamble. You feel like you’re rolling the dice, but I’m feeling pretty lucky.
I have a strong faith in God, my family, and myself — we believe God brought us here. He opened up one spot in the clinical trial, and I was able to pursue it just in the nick of time.
I really feel like this is meant to happen.

You have to weigh it out: Is it worth it for just a little more time? Or do you want quality of life, great memories, and to do all the things you can?
Kim C. – Ovarian cancer patient

Self-Advocacy During Treatment
How I’ve advocated for myself: I have done some research, but I really have to give so much kudos to my wife, who has done a lot of it.
I feel like we’ve had doctors who are bulldogs about getting medicines approved. I’ve done immunotherapy in the past. Asking a lot of questions and noticing changes in my body is a big way I advocate; paying attention to all the little changes and bringing them up.
I have some brilliant doctors in whom I have complete trust, and they’ve truly done everything they can. They’re learning a lot, as this is new to them. I hope that for future generations, this will help the learning process.
The Impact on My Family
My wife has been an angel. It’s been very difficult for her. Everyone processes emotions differently; she processes them differently than I do. It’s been very, very hard. I’ve even said to her, “Wow, you did not sign up for this.”
Every day, I feel like I owe her an apology, but I know this isn’t something I caused. I can see how worried she is.
Jennifer, my family, my dad, stepmom, her family, and a huge community of friends; they’re all worried, but they are right there with me, encouraging me. Jennifer is right here, and anytime I have a tough moment, so is she. It’s been really hard.
My grandkids are eight, four, and a brand-new baby. We haven’t really talked about cancer with them. The eight-year-old was four during my first chemo rounds and saw me lose my hair. She calls me Mimi and said she didn’t like my hairstyle, which made me laugh. With our son, her dad, we’ve talked in depth, but we’re leaving it up to our kids to talk to their kids when they feel the time is right, using the right words.
We are here for questions, but as grandparents, we’re not in the position to explain cancer unless they ask. I’ll answer carefully, but they’re still young, so we haven’t had big discussions.
They sure have been a bright light to us. They visited a couple of weekends ago, right after we got bad news. Holding the newborn and playing with them lightened the load in my mind.
We have two sons, one is 21 and one is 31. They’re strong men, but handle it in different ways due to their personalities. The 31-year-old is a rock. I can talk with him in depth, and he shares things he’s heard about science. We brainstorm and discuss a lot. They want to know every detail, so we plan when and how to tell them. The 31-year-old lives six hours away with his family, and the 21-year-old lives with us. He’s been amazing. He gives random hugs and prayed with us last night. That made me feel good. As a family, this has been a growing experience.
We’re learning to lean on each other, that it’s okay to feel weak or to cry, ask questions, or worry — but most importantly, to be honest and truly lean on each other.
My Ovarian Cancer Story Continues Below
Program Highlight: A New Era in Platinum-Resistant Ovarian Cancer Treatment Options
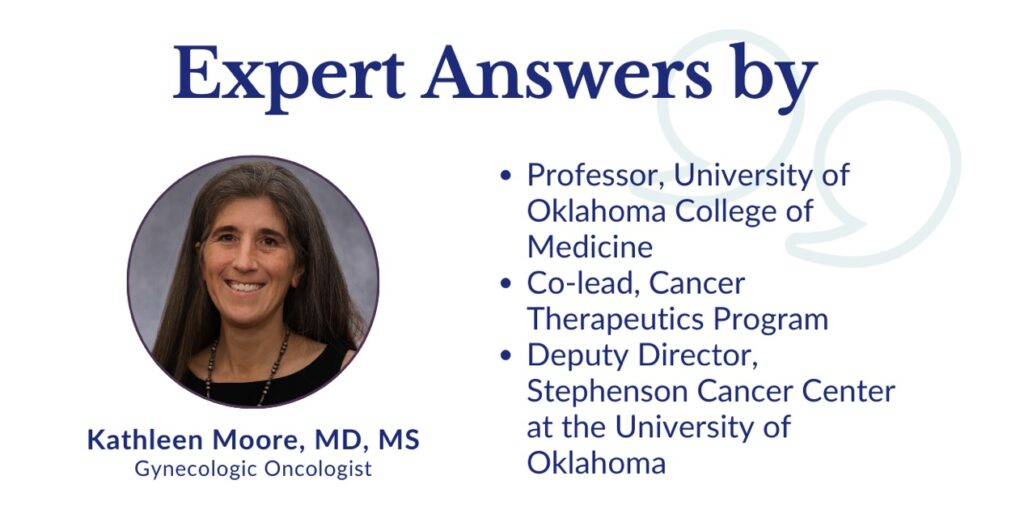
Navigating a diagnosis of platinum-resistant ovarian cancer can feel overwhelming, but recent advancements and clinical trials are bringing new hope and more personalized treatment paths. This program offers empowering information on the latest therapies. We are joined by Dr. Kathleen Moore, an internationally recognized leader in gynecologic oncology from the Stephenson Cancer Center, who breaks down what you need to know about where treatment is heading.
Dr. Moore will help break down some of the more complex ideas regarding ovarian cancer treatment. Go beyond the words and hear from an oncologist who treats patients every day.
What to expect:
- Understand Platinum Resistance: Learn what this diagnosis means and how it shapes your treatment options
- Discover Emerging Therapies: Hear about the promise of antibody-drug conjugates (ADCs) and other new drugs that are improving survival
- Learn About Biomarker Testing: Find out how tests for markers like folate receptor and BRCA can unlock personalized treatment paths
- Explore Clinical Trials: Get clear answers about how to find and access clinical trials for new and promising ovarian cancer treatments
- Personalize Your Care: Learn how oncologists are sequencing therapies to create more effective, individualized treatment plans
- Advocate for Yourself: Gain insights on communicating with your doctor and the questions to ask to ensure you get the best care

Dr. Kathleen Moore: The next big challenge for us is going to be… say these [new treatment options] are all approved. Which one do I get first? Does it matter?… It’s really going to be the next big challenge for us — individualizing for our patient so they get the best drug for them, best tolerated.”
Making sure patients feel seen and heard
Dr. Moore: “Patients present with months and sometimes even longer, of just not being believed or being bounced around or given this or that medicine, So they arrive at our door with some varying state of trauma that I don’t know that we’ve ever really addressed up front. But I’m trying to start acknowledging that at least.”
Dispelling myths about clinical trials
Dr. Moore: “People don’t want to feel like a guinea pig… They want to participate in clinical trials, and I want to run clinical trials that I think are going to work.”
Helping more patients get access to the latest therapies
Dr. Moore: “There are a lot of community sites doing very high-quality clinical research. Trying to figure out where that is in your community can be the first step… Getting access to these sorts of medications as compared to Topotecan — 100%, I would want that for my mom.”
For the rest of this interview, watch our program replay ON DEMAND.
Learn what’s changing, how it impacts treatment decisions, and what it all means for patients today.
Back to My Ovarian Cancer Story
The Importance of a Supportive Care Team
My care team has been amazing, led by my doctor and including the nurse practitioner. They’ve always been honest. Jennifer prefers to know, “If this doesn’t work, then what?” I just want to know, “Is this working?” We’ve each approached the doctors differently, but they have always wanted the best outcome. I truly believe our doctors want to cure cancer and want us to live. You have to believe in your medical staff, from the doctor to the nurse practitioner to the nurses in the infusion center where I get treatment.
Those nurses are so supportive. If I get bad news, they’re there. I remember having a rough day, and they gave me a blanket inscribed with words; one of them is “battle.” I call it my battle blanket. Each nurse in the infusion room came by, hugged me, and said a word of encouragement. We are all in this together as a team.
Now, I’ll be switching to the clinical trial team, which is a little scary. It feels like losing my security blanket with my current team, though I know the new team is excellent. My current oncology team will still get updates from me. It’s amazing to have this community and see all the helpers coming from everywhere. When you go through a storm, you’re not alone.
Platinum-Resistant Cancer and Treatment Options
There’s platinum resistance, which involves frontline chemotherapy medicine. To be platinum-resistant, you think, “Oh great, now no chemo is going to work,” but there are chemotherapies that aren’t platinum-based. Knowing you’re platinum-resistant cuts out a large portion of available therapies, which can be scary.
But I don’t focus on that. With clear cell, being platinum-resistant is so common. What worries me more is that this cancer is so rare; even doctors are still learning about it. Science and funding need to catch up so we can study and find more therapies, including more non-platinum options for all cancers. I hope I’m correct in my science, but basically, being platinum-resistant means we need more therapies.
Lessons I’ve Learned About Myself
I’ve always said I wanted a purpose in life, and I feel like showing love to others has always been my purpose. Cancer has given me an even greater sense of purpose. I now have a platform to inspire and bring hope to people. People ask me how I do it, where I find my strength. I believe God gives me the inner strength and the drive exactly when I need it, which He has proven again and again during this journey.
I’m now faced with real mortality, knowing that if things don’t go well, this could be it. It’s hard to process. But with my faith in my medical team and in God, and belief in this clinical trial, I’ve learned to stay calm. I don’t have control, anyway.
Take a deep breath, don’t panic, keep going, and do your best every day. It’s okay to not have a good day, and to let people know, so they know it’s okay for them, too. I’ve learned no matter the outcome, it’s going to be okay.

Take a deep breath, don’t panic, keep going, and do your best every day… I’ve learned no matter the outcome, it’s going to be okay.
Kim C. – Ovarian cancer patient

My Message to Others Facing a Recurrence
Yes, the cancer has come back. Everyone’s kind words, encouragement, and prayers mean so much. I’m not giving up, I’m not losing hope, and I’m going to keep pushing. I don’t want anyone to look at a recurrence and think, “Never mind.”
Just don’t lose hope. Keep hope with your medical team. Science will hopefully come up with the right therapies. The encouragement has meant so much; please keep encouraging, and encourage others who need it.
I don’t want people to lose hope that cancer can’t be cured, or that miracles don’t happen, because I believe in miracles, and I want others to believe too. The encouragement keeps me going. We’re going to keep fighting.
Navigating Identity as a Woman and Caregiver
To keep showing up for others, despite what I’m going through mentally, has really helped me. I love to make people laugh and bring a smile. It keeps me going.
Being in a position where I’m the one needing care is difficult because I’m used to caring for others, and I love to help. But now, I need help. It’s an odd feeling. It’s hard to ask for help, but often people just show up intuitively.
I’ve stayed in a community surrounded by friends and family. My wife is amazing. To have her care for me in such a different way than you would expect as a spouse is hard, but I want to continue to show up for her and my family as much as I can. Being able to still do that makes me feel good.
My Final Reflections: Staying Hopeful Through Hard Times
Even though this cancer has recurred again, and this is a really tough recurrence, I want people to know that even in the toughest times, like what I’m dealing with right now, you can’t really know exactly what someone else feels.
But even in your darkest times, open your eyes, look around, and find your people. Find your helpers. Find encouragement. Try your best to find someone to talk to, vent to, or encourage. Just don’t give up in your toughest time. Whatever you’re facing, cancer, trauma — don’t go down that dark hole mentally. Be mindful of your mind. If your thoughts are getting dark, find a way to turn it around; help someone, encourage someone, be there for someone, pick up the phone, call someone.
Find resources: support groups, communities. There really is a lot of help. Sometimes you just have to search for it. Stay hopeful, don’t give up, and don’t let yourself go down that dark hole mentally. Look for people to inspire. Take it on as a chance to do good for others, to be a light. I really believe that’s important for people to know.
… even in your darkest times, open your eyes, look around, and find your people… Just don’t give up in your toughest time.
Kim C. – Ovarian cancer patient


Special thanks again to AbbVie for its support of our independent patient education content. The Patient Story retains full editorial control.

Inspired by Kim's story?
Share your story, too!
More Clear Cell Ovarian Cancer Stories
Sara I., High-Grade Serous & Clear Cell Carcinoma, Stage 3A
Symptoms: Random sharp pains, unrelated scan showed ovarian cyst
Treatments: Debulking surgery, chemotherapy (carboplatin & paclitaxel), PARP inhibitors (clinical trial)
...
Kim C., Ovarian Cancer (Clear Cell Carcinoma), Stage 2B
Symptoms: Coughing, incontinence, severe bloating, nighttime pain, hard lump on right side
Treatments: Surgeries (radical hysterectomy, lymphadenectomy), chemotherapy, radiation therapy, immunotherapy
...
Kim C., Clear Cell Ovarian Cancer, Stage 4 (Metastatic)
Symptoms: Coughing, incontinence, severe bloating, nighttime pain, hard lump on right side, appearance of rash on chest
Treatments: Surgeries (radical hysterectomy, lymphadenectomy), chemotherapy, radiation therapy, immunotherapy, clinical trial
...
