Rachel’s Gastric MALT MZL Non-Hodgkin’s Lymphoma Story
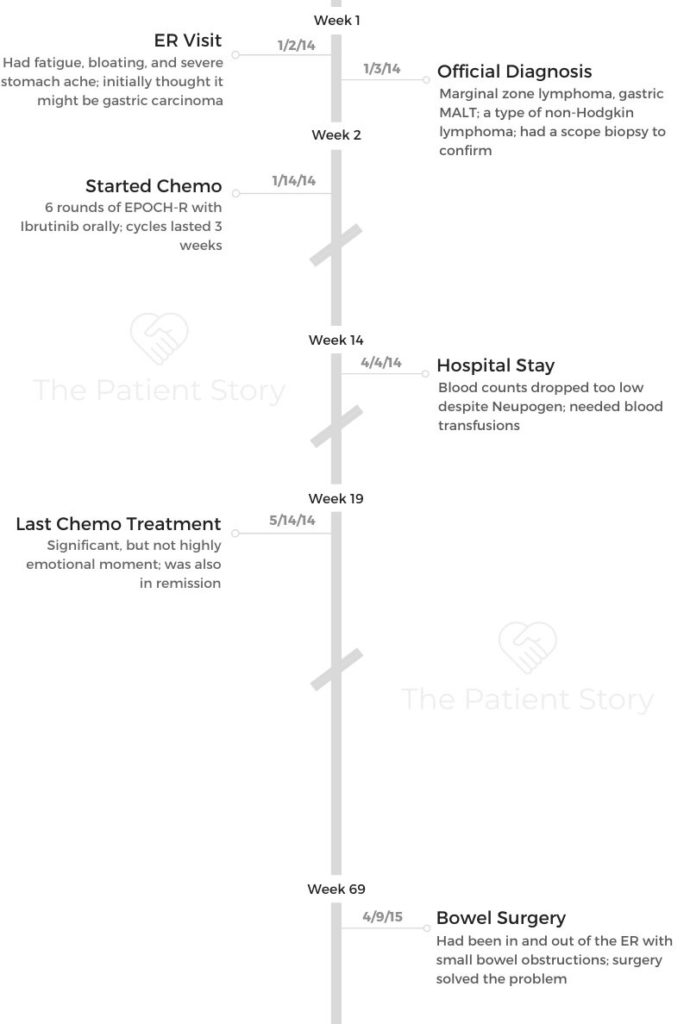
Rachel was diagnosed with a type of marginal zone lymphoma called gastric MALT, found in the stomach, eventually undergoing R-EPOCH chemo, targeted therapy (ibrutinib) and surgery.
In her story, Rachel also highlights losing hair to chemo, parenting with cancer and how the diagnosis impacted her marriage. Thank you for sharing your story, Rachel!

- Name: Rachel P.
- Diagnosis:
- Marginal zone lymphoma
- Subtype of non-Hodgkin’s lymphoma
- Gastric MALT at age 47
- Staging: N/A
- Symptoms:
- Bloating
- Fatigue
- Stomach Pain
- TreatmentCenter:
- Holy Cross Hospital
- National Institutes of Health (NIH)
- Treatments:
- Chemotherapy
- 6 rounds of R-EPOCH chemotherapy
- 96-hour continuous infusion once every 3 weeks
- 6 rounds of R-EPOCH chemotherapy
- Targeted therapy
- Ibrutinib
- Surgery
- Minor bowel resection
- Chemotherapy
This interview has been edited for clarity. This is not medical advice. Please consult with your healthcare provider for treatment decisions.
I hope you don’t have to go through the kind of chemo I did, but if you do, you’re going to make it. It put me in remission, and I’ve stayed that way for a long time.
I hope that gives you some comfort. You’re going to make it out to the other side, and you’re going to be okay.
Rachel P.
Diagnosis
1st symptoms of lymphoma
I was in denial for a long time. I had been having trouble buttoning my pants for a while. I started wearing flowy clothes. In December of 2013, someone asked me if I was pregnant. There was clearly something wrong, but I also had a hernia, so I just thought it was related to that.
I was pretty low energy for a while, too. When I’d work out, I would get tired faster than usual. The night of January 2nd, I had a really bad stomach ache, and I went to bed at 6:30 p.m. because I was just too tired.
The pain became so intense over the course of the night, and my husband was asking if I wanted to go to the ER. I kept saying, “No, it’s just a hernia. That’s silly.”
Finally, at about 1:30 in the morning, I wanted to go because I was in too much pain.

What happened at the ER?
When I got to the ER, they started going over all my symptoms, and they gave me an initial diagnosis of gastric carcinoma, which is luckily not what I had.
Some of the symptoms were indicative of that, but they decided to do a biopsy, and that’s how I was officially diagnosed.
I ended up staying in the hospital for a few days because of some advice from a friend. That friend worked at the hospital, and she told me if I wanted to get everything done, I should stay there and sit tight.
Otherwise, I’d have to get referred to a bunch of different offices.
What’s the biopsy like?
It was a scope that went down my throat. I wasn’t under general anesthesia, but I went to sleep. I had loopy medicine.
I’ve had many colonoscopies since, and they always tell me, “We just gave you the anesthesia that’s supposed to make you half asleep.”
Every time, though, I’m completely out. I do really well with anesthesia. It works great for me.
The biopsy really wasn’t bad because I don’t remember it. I just know they took a sample, and then we waited for results. It seemed to all happen pretty fast, though.
How did you process the cancer diagnosis?
I don’t actually remember getting diagnosed or getting the results of the biopsy. I’m sure my husband remembers everything crystal clear. I do remember at one point they told me I got a “good kind” of cancer.
I was shocked and very upset, but I wasn’t ever worried I was going to die.
It was unbelievable that I had cancer because I thought of myself as the healthiest person I know. I knew I had to go through treatment, but I knew I wasn’t going to die. I’ve always known I might relapse or might never, and that’s just the way it is, but here I am years later.
»MORE: Processing a cancer diagnosis
Getting a second opinion
There was something called caking on my omentum, which is a pretty unusual presentation for my kind of cancer. That’s a sign of gastric carcinoma, so that’s how everything snowballed into me being seen at the National Institutes of Health, or NIH.
We had seen an oncologist at the hospital and met with him in his office. My daughter’s best friend’s mother works at the National Institutes of Health in the cancer center, and I didn’t know that. She suggested I go there for a second opinion at least.
For reasons still unknown to me, they were very excited about me and my whole case. Even though I had a slow-growing cancer, I hadn’t been aware of it for so long that they were ready to start treatment, which is a terrible chemotherapy, but it’s their standard of care.
An oral drug called ibrutinib had been fast-tracked through the FDA and approved for use only at NIH, and they were planning to give me that, too.
We went back to the original oncologist, and he was like, “Yes. Go there. That’s the place you want to be treated if you can.”
It was a few days later when I started treatment. I met with this room of what felt like a thousand people.
The head of the National Cancer Institute was there. There were just so many nurses, doctors and everyone.


Cancer Treatment
Describe your chemotherapy regimen
I had 6 cycles of EPOCH-R chemo. It was 96 hours of continuous infusions once every 3 weeks. They give you a fanny pack of chemo to take home with you basically.
You come back the next day, they change your bag, and it goes on like that for 96 hours. I took ibrutinib orally as well. I was the first person with this kind of cancer to take ibrutinib actually.
They start in the infusion room with fluids, steroids and all the preliminary medicine. They start the chemo for you, and you take it home for the rest.
When you go home, they give you all these crazy instructions, like, “If that bag breaks, you should put a hazmat suit on.” It’s just crazy. You have to take all these precautions, not let anyone near it, and be careful not to bust the bag.
Bad reactions to the chemo
I had some pretty bad reactions to the chemo during infusions. It was an itchy thing. Then they taught my husband to give me the Neupogen shots, and the bone pain from that was the worst thing I experienced.
Each cycle, they’d up my chemo dosage a little. It was a step up every time until the end of it, when I had a backpack instead of a fanny pack.
What are the chemo side effects?
It was very cumulative for me.
As it went on, I had fewer and fewer good days. It’s not one of those chemos you can run a marathon on. I’m a fitness professional, and I was hoping to be able to walk to the end of the block by the end of it.
I got C. diff at some point. I got the flu. My immune system was just shot. I had a lot of trouble with constipation. All the meds they give you to counteract the nausea made me constipated, and the steroids kept me up at night.
Then Neupogen gives you that bone pain that’s so incredibly painful it’s hard to describe. It’s a deep aching that comes from inside your bones all over, and even your scalp hurts. During the bad days, I would literally just lay down in my room all day. It was not enjoyable.

On one hand, I got the good cancer, but on the other hand, I got the bad chemo. One lasting side effect I had was small bowel obstructions. I ended up back in the ER because of that.
They found that part of my intestines had been killed off by the chemo. For whatever reason, it just wasn’t working in that one little spot.
I went back to NIH, and they did surgery. They took out that part of my intestines, and everything has been fine since then.
»MORE: Cancer patients share their treatment side effects

Getting routine blood work and scans
During treatment, I would get blood work every 3 weeks. Sometimes I had scans, and sometimes I didn’t. I had an MRI of my brain at one point.
I had a bone marrow biopsy. They did a lot of testing. That was all throughout the course of treatment.
The nice thing is they were following something in my blood work. It was a marker called an M spike. Now, I just get the blood work, and as long as that thing doesn’t spike ever again, I never need another scan. I haven’t had one since about a year and a half out of treatment.
In remission!
At the end of all the treatment, I had no evidence of disease. I was in remission. I think I was in remission even before the chemo was done, but we had to finish the protocol. With this type of cancer, they don’t use the word “cure.” It may recur, or it may not.
I didn’t really have a highly emotional response to it. I was just kind of done at that point. The worst part about cancer was the treatment, and I was reassured by everyone that everything would be okay in the end, so I was just glad to get it over. I remember my last chemo treatment being significant to me, but it wasn’t surprisingly so.
Reflections
Can you talk about your support system?
I was surprised by who stepped forward and who did not. I think that’s a pretty common thing when you go through a significant life event.
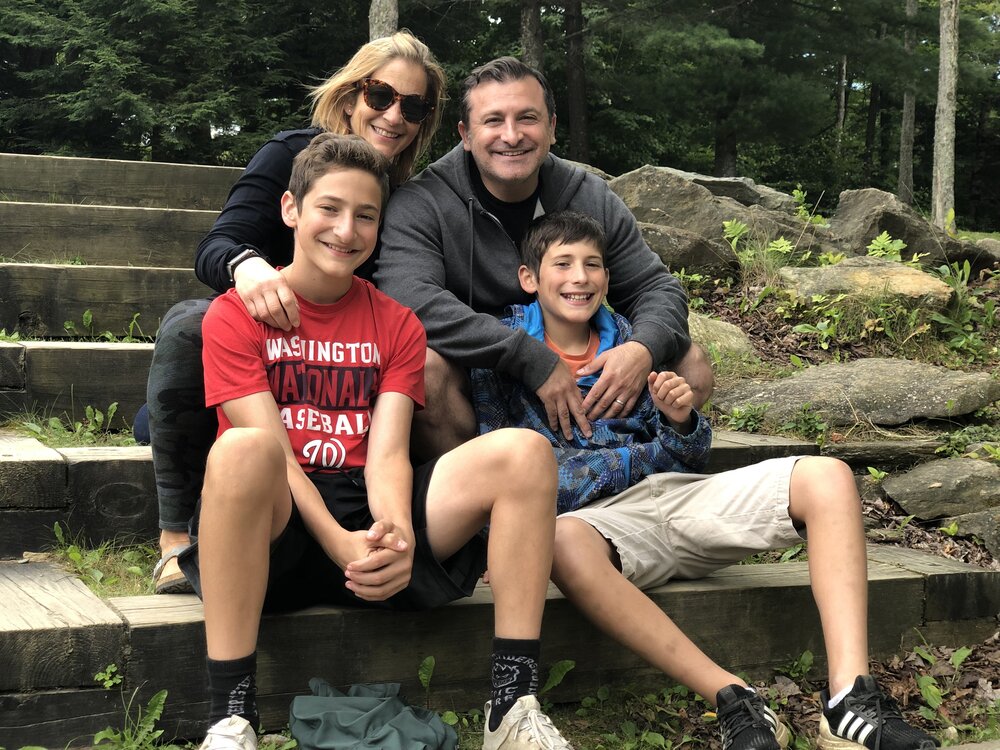
My husband was my caregiver, and it was a lot harder on him in some ways.
All I had to do was go in my room and cry or just lay there and feel bad. He had to take care of me, work, take care of the family, and fend off people who wanted to talk about it because I didn’t want to.
People want to help so much, but there was really nothing they could do for me. I didn’t even want my husband around all the time, and that was hard for him.
We had an au pair at the time. That was amazing because I don’t know how you do cancer and taking care of everything else at the same time. We didn’t have any family close by, so that was really helpful to have her.
One of my good friends had twins on December 31st, so she spent her maternity leave with me, and I spent my chemo leave with her. We would take a walk with her twins and my dog if I felt up for it. That was helpful.
We tried to do a food train, and I just got pissed off by it because people can’t follow directions. My freezer is only so big. People would bring way too much food, or they’d bring not enough food, or they’d bring food that little kids wouldn’t want to eat.
Sometimes, they’d knock on the door when I was home alone and didn’t feel like getting up, even though we said not to.

Advice for people who want to help but don’t know how
It’s so different in each situation. It’s so personal. A lot of people love the meal thing, but that didn’t work for us. Everyone’s chemo is different, and everyone’s experience is different.
For me, I needed a lot of hats, blankets and socks. It was wintertime and cold, and I was constantly cold. You have to take the lead from the person who’s sick or the person who is their communicator.
Follow their directions. If they say, “Please don’t knock on the door,” don’t knock on the door.
How to tell your kids you have cancer
My mom had died of lung cancer, so that was the only context they had, even though they were young when she died. We told them I had cancer but I wasn’t going to die. We were very open about it.
It’s interesting because they don’t remember as much of it as I thought they would. Children are self-centered humans, and I think that helped them because they really don’t remember a lot of it. Their lives continued pretty much as normal. That was really lucky for them.
I lived in fear that they would be traumatized by it, but I really don’t think they were.
»MORE: Parenting with cancer

How does cancer affect your relationship with your spouse?
We didn’t change much. He’s involved, especially for how much he works. At the time, I think I was just focused on feeling miserable and getting through it.
I don’t know if it brought us closer together. I don’t think so, but I know it didn’t pull us apart either. We just had to get through it. As a family, we’re just as close as we were.
»MORE: 3 Things To Remember If Your Spouse Is Diagnosed With Cancer
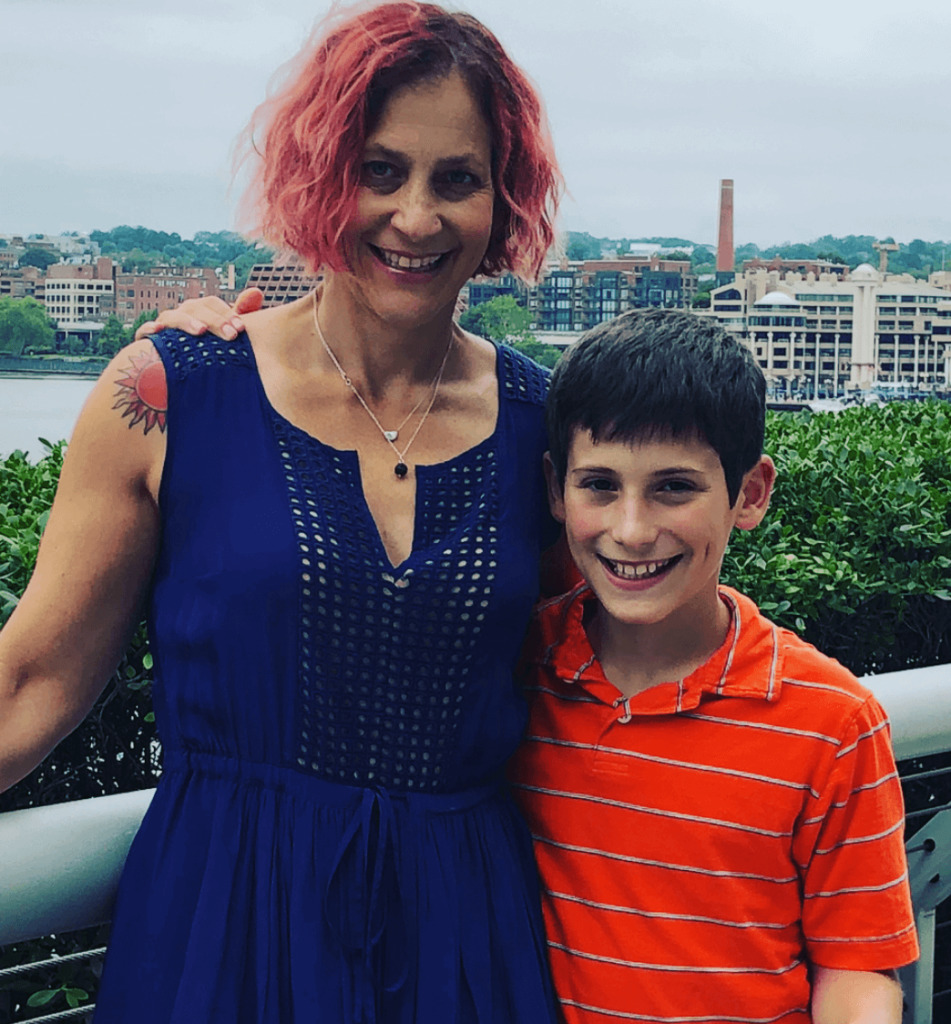
Describe the hair loss
I had really long, wavy, thick hair. They said I would lose it around the second treatment. Right before that, I cut it short.
That wasn’t a big deal, but then it really started falling out quickly. I had my husband shave it for me because it looked weird, and I didn’t want clumps coming out in the shower.
I thought I looked pretty badass once we shaved it, because I was still pretty fit at the time. I hadn’t dropped a bunch of weight yet.
I looked at some wigs, but I decided that wasn’t for me. I just stuck with hats because it was cold or went bald. I wasn’t trying to hide it.

I was walking through the grocery store one time, and a guy shouted over to me, “You go, sister! Fight the fight!” It took me a second to realize what he was talking about because I forgot I was bald.
I had so much going on. I was thinking, “Who has time to worry about being bald? I’m just trying to make it through the grocery store.” It was a cute moment. He was very sweet.
The hardest thing about the hair loss is that my eyelashes, brows and my hair didn’t come back as much as I was hoping they would. I’m sad about my eyebrows and eyelashes.
I grew my hair out, and it’s not nice anymore. It’s thin and fine. A month ago, I said to my hairstylist, “Let’s just find a hairstyle that works with this hair I have now.”
»MORE: Dealing with hair loss during cancer treatment

“New normal” after cancer
One of the ways that I have struggled the most is with fitness. Not only did I have cancer and lost 25 pounds of mostly muscle, but I’m also in my 50s now. I’ve really had to struggle with not being as strong as I was.
In the grand scheme of the general population, for a 53-year-old woman, I’m pretty strong. I just have to make peace with where I am when I work out.
My new normal is fine. I can’t open jars very well because of a little residual neuropathy. My feet hurt when I stand for a long time because of the same problem. I’ll take that for being alive, though.
My favorite saying is, ‘It ain’t chemo.’ I’ve never experienced anything like that. I’m alive. I’m healthy. It’s all good.
What advice do you have for someone who has just been diagnosed?
I hope you don’t have to go through the kind of chemo I did, but if you do, you’re going to make it. It put me in remission, and I’ve stayed that way for a long time.
I hope that gives you some comfort. You’re going to make it out to the other side, and you’re going to be okay.
Inspired by Rachel's story?
Share your story, too!
Marginal Zone Lymphoma Stories
The Importance of Positive Role Models
The example that Nick's father set for him as he was growing up taught him how to prioritize and advocate for his health.
Nick M., Nodal Marginal Zone Lymphoma
Symptoms: Daily hives, GI issues, weight loss, heart issues, night sweats
Treatments: Rituxan (rituximab), high-dose steroids
Kimberly O., Marginal Zone Lymphoma
Symptoms: None at first, routine blood work showed suspicious results, bad nosebleed
Treatment: Chemotherapy (bendamustine & rituximab)
Rachel P., Marginal Zone Lymphoma, Gastric MALT
Symptoms: Fatigue, bloating, stomach pain
Treatments: Chemotherapy, targeted therapy, surgery


