John’s Stage 4 Follicular Lymphoma Story
John, a 63-year-old diagnosed nearly a decade ago with follicular lymphoma, shares his journey. Initially, he did not follow a typical diagnostic path. His wife and others noticed swollen lymph nodes in old photos, helping lead to the realization that the cancer had been present since 2001. Due to the nodes’ waxing and waning nature, John spent 14 years unaware that he had cancer.
Interviewed by: Taylor Scheib
Edited by: Chris Sanchez
Upon diagnosis, John’s primary care physician, also a long-time friend, could not meet John’s eyes, sparking John’s suspicion. The confirmation came from a third doctor, who explained follicular lymphoma‘s indolent or slow-growing nature and presented various treatment options. John’s diagnosis prompted him to reevaluate his life, focusing on living rather than fearing death.

John consulted lymphoma specialists from prestigious institutions in Chicago. He learned more about his condition, discovering that the average lifespan post-diagnosis was 18 years, which has since improved due to advances in medicine and technology.
Eventually, after evaluating his options, John elected to participate in a clinical trial involving an exploratory drug. The trial was risky, and the documents openly stated potential fatal outcomes. His brother, with a background in microbiology, offered some support. John learned to navigate medical literature and ask critical questions, becoming actively involved in his health decisions.
Living in Chicago facilitated John’s participation in the trial, though the impact on his business was significant. He went from working extensively to being incapacitated, sleeping up to 19 hours daily. Fortunately, he had saved money, preventing financial hardship.
The trial initially yielded positive results, eradicating most of the cancer, but the effects were short-lived. After failing 6 different treatments, John and his doctors creatively combined 2 drugs, despite insurance challenges. Drug manufacturers supported the cost of the second drug, leading to a successful treatment. In July 2022, John achieved his first complete remission, and by May 2023, he ceased oncology treatment, awaiting further clinical evaluations.
John’s journey taught him to understand and empathize with those who choose to quit fighting cancer. He emphasizes the importance of self-advocacy and the importance of overcoming one’s fears. John underscores the necessity of trust in clinical trials, stating that he aims to help others through his experiences and involvement in his own clinical trial.
- Name:
- John S.
- Diagnosis:
- Follicular lymphoma (non-Hodgkin lymphoma)
- Staging:
- Stage 4
- Initial Symptoms:
- Swollen lymph nodes
- Treatments:
- Clinical trial
- Chemotherapy


Thank you to Genmab for their support of our patient education program! The Patient Story retains full editorial control over all content.
This interview has been edited for clarity and length. This is not medical advice. Please consult with your healthcare provider for treatment decisions.
I decided to give something back and help others through joining [a] clinical trial.
One of the things I think all of us want to do is to matter in some way and shape, whether it’s small or large or however it winds up being.
Introduction
My name is John.
I was diagnosed almost 10 years ago now, and at the age of 53, with follicular lymphoma.

Pre-Diagnosis
I wound up not having a typical pathway.
Some years ago, my wife at the time had pulled out a picture of us with our daughter at Disney World.
My wife goes, oh, look at your neck. You know, you could see that I had swollen lymph nodes.
And through checking through other old photos, where my lymph nodes were waxing and waning and so on, we were able to infer that I’d actually had cancer since 2001.
Not that any of the doctors I was seeing then ever did anything wrong, because that’s pretty normal when you get sick. Your lymph nodes grow and then they shrink. So if they do grow and then normalize after 2 or 3 weeks, we just shrug them off.
So I had at least 14 years of not knowing I had cancer.
Diagnosis
My cancer was diagnosed almost 10 years ago now.
I went through the process, talked to my primary care physician, who had been my friend for 10 or 15 years at the time as well as being my doctor.
Some of my background is reading body language, and I kind of figured something was not quite right. He couldn’t look me in the eye.
So I started suspecting that something was going on. It wasn’t until I got to speak to a third doctor that I knew for sure that something was up.

I was active as a youngster, you know, broken bones, surgeries, all that kind of good stuff. So I’m used to walking into a doctor’s and being told that, say, my arm is broken and we’re going to put it in a cast.
So I walked in there and received my diagnosis of follicular lymphoma. Some cancer diagnoses are pretty well defined, but follicular lymphoma at the time wasn’t.
So I had a conversation with him, and that’s when I came to understand that it is incurable, but is also an indolent form of cancer, one that’s slow-growing. That it wasn’t something I needed to get out of my body immediately.
The third doctor I saw, who had diagnosed my cancer, pulled out the NCCN guidelines, what I call the “oncologist encyclopedia”, and he had photocopied some pages for me, to help me learn more about follicular lymphoma.
He also explained the different treatment options available to me. He basically said, there are 4 options available to you, whenever you want to start. In my mind, I was like, wait a minute, you’re the doctor. Why are you giving me options? This was yet another of the lessons I needed to learn about follicular lymphoma and cancer in general.
I had a lot to learn about follicular lymphoma.
I decided to start living life versus fearing death.
Reaction to the diagnosis
So when you’re hit with this diagnosis, you all of a sudden start to examine your life. You start looking at things and evaluating them differently.
I started to understand that there’s a finish line here on Earth and it applies to all of us. And whether you have faith or not, it becomes irrelevant.
Once you hit that finish line, there’s no coming back, no redoing anything.
So for me, I decided to start living life versus fearing death. Or trying to avoid death versus moving forward.
For me, it was a blessing because it helped me look at things differently.
Treatment options and plan
The third doctor also told me that I should consult some experts in lymphoma.
At the time, I lived in Chicago, and some pretty reputable doctors and facilities were available to me, like Northwestern, the University of Chicago, and Loyola. And he also gave me some of the names of the top lymphoma specialists — one of whom, it turns out, is actually one of the top experts in the world in this sphere. And so I started to reach out to them.
I had no idea what to ask these experts, but ask them I did, and by the time I had gotten to the third doctor, I had a better idea of what questions to ask them.
I had also learned that the average lifespan of a follicular lymphoma patient at that point in time was 18 years after diagnosis — although this has now changed given the advances in technology since then and is closer to the lifespan of a healthy person.
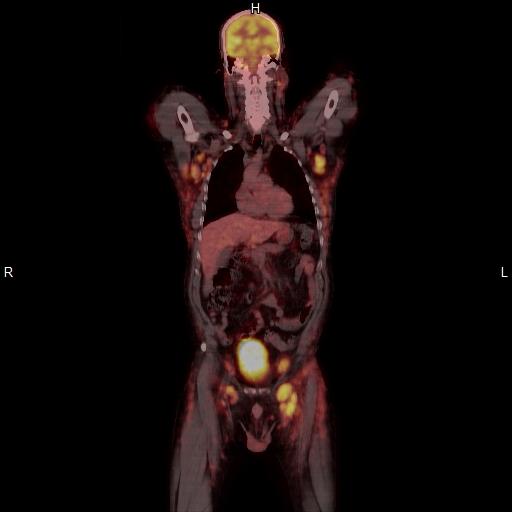
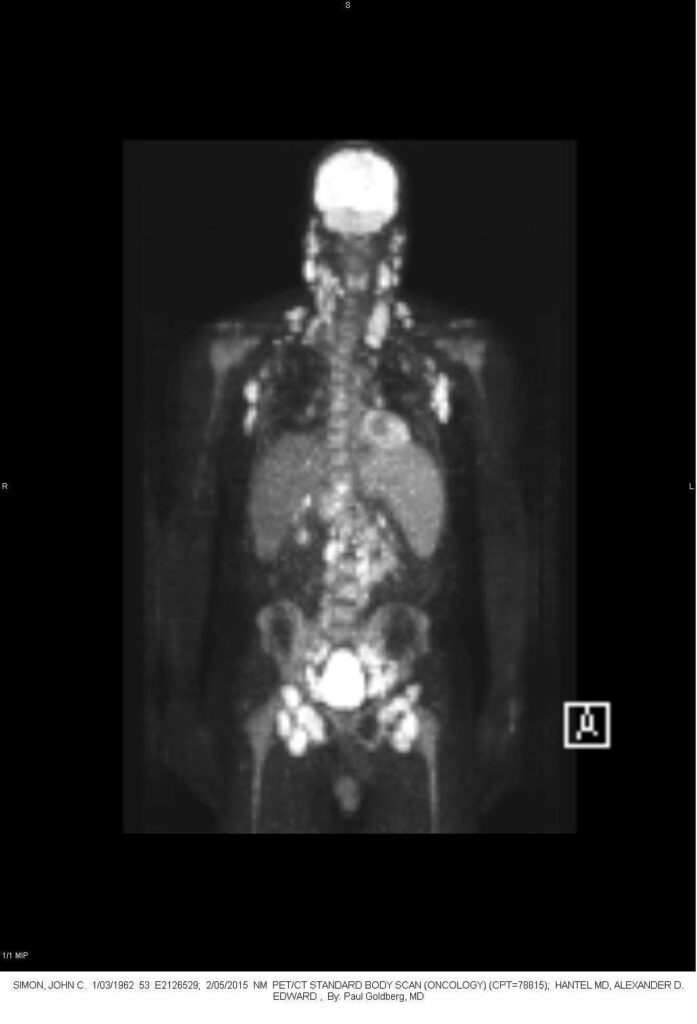
I literally lit up like a Christmas tree at my Pet scan. That was enough to unsettle me a bit. But the doctors all were of a mindset that this is borderline watch and wait, because of the indolent nature of my cancer. They said, you don’t really need to do anything.
Though when I talked to my third doctor and asked her what the prognosis was, she said to me matter-of-factly, we’re going to beat it down.
It’s going to come back, and when it does, we’ll beat it down again, and we’re going to continue this until we can’t beat it down any longer.
And as we continue down the pathway, they’re generally going to be shorter and shorter remissions, and it’s going to come back more aggressively each time.
So when you’re hit with this diagnosis, you all of a sudden start to examine your life.
You start looking at things and evaluating them differently.

Clinical trial
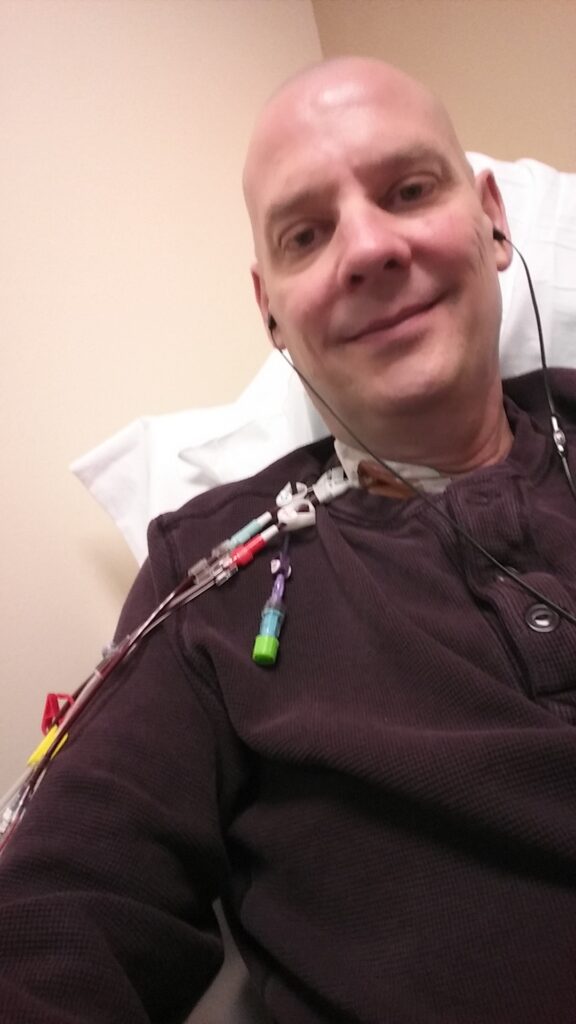
One of the options for me was to undergo a clinical trial, and this is what I ended up doing. It involved a pretty benign exploratory drug, and I was the 8th or 9th person to join the trial, which put me in the 3rd cohort.
That being said, though, the trial is serious stuff. The documents and literature they provide are open about the possibility that people who join the trial could die from its effects.
It’s also about making decisions about things that you don’t know about, and which your doctors don’t know about either. And they’re upfront about it — look, we don’t know if this will or won’t work or if it will or won’t help you. That’s why the drug is in a clinical trial.
It helped a little bit that my brother has a background in microbiology and has been in the field for about 40 years — not as a researcher, but in the business side of things — and also has a lot of contacts.
But I also started to delve into reading medical papers, not that I understood them all. I had to use Google quite a bit to define some terms, but I did start to get a better understanding of things and what possibilities there were for me.
The clincher for me was that I decided to give something back and help others through joining the trial. One of the things I think all of us want to do is to matter in some way and shape, whether it’s small or large or however it winds up being. And in my particular case, one of my bucket list items was to help other people learn, and to use the time I had left wisely.
So that’s why I decided to go down the clinical trial path.
Making informed decisions and becoming the CEO of his own health
Since I was going to have to make an informed decision regarding the follicular lymphoma clinical trial and of course moving forward, I was going to basically become the CEO of my own body. That’s the way I would like to describe it.
You’ll get competing points of view from different doctors and experts. It’s not that they’re in disagreement with each other. It’s that they have different patient experiences.
You have to get comfortable dealing with uncertainty, with the unknown and your fear of it. And understand that since you’re going to have to make an informed decision, you’ll need to properly educate yourself. And, of course, learn to ask questions.

One of the questions I’d ask every single one of my doctors, whenever they’d put a possible option forward, is: why do you think that’s the best option?
And in addition: what are the other options that are out there, whether or not you have access to them?
Since I was going to have to make an informed decision regarding the clinical trial and of course moving forward, I was going to basically become the CEO of my own body.

The logistics of joining the clinical trial
It really helped that I was in Chicago at the time. Had I not been there, having to relocate to join the trial would have been quite challenging and time-consuming.
It’s good, though, that there is help available for those who need to travel to get treatment.
Some of the hospitals and cancer centers can help with ambulances, including flight ambulances, and there are a slew of charitable organizations that can also help make a pathway for you.
This sort of help could do nothing to offset the impact on my business. I was doing quite well before I got sick, and I basically went from making what I was making to zero. I basically went from working 70 hours a week to having to sleep about the same length of time because of my treatment. There was a point in time that I was sleeping 18 or 19 hours a day.
I was very fortunate that I had put away some money. A lot of people run into financial hardships because of these kinds of things.
Treatment progression
So under the trial, I had 4 little shots of the drug.
I experienced some CRS and had to go to the emergency room for a little bit, my temperature kept going up, and my heart rate kept going down too. And other things happened, like my neck got swollen, though that subsided.
But the results were pretty good. It wiped out nearly all the cancer.
Sadly, the good effects only lasted a month or a month and a half. The cancer came back.
So we ended up switching treatments and trying different lines of treatment. Some ended up working for a little while and others just didn’t work at all.
You have to try to overcome your fears.
That’s a big thing when it comes to cancer and cancer treatments.

Trying other options — and success
All told, I ended up failing no less than 6 lines of treatment in less than 4 years, and chemotherapy hadn’t worked.
Based on my doctors’ experiences, they judged that it would be better to start trying different things. And of course this was no less than a life-threatening situation.
So we decided to get creative and put two drugs together.
I’m thankful for the support we had for this. My insurance said they could pay for one drug but not the other. And that’s where the drug manufacturers stepped in and supported the second drug. They provided the medicines free of charge for the next 3 and a half years. They were just looking to help out.
The idea to do this was based off my situation, which was unique. And it finally worked.
After about 3 and a half years on the protocol, I achieved my first true complete response. A clean scan in July 2022.
May 31, 2023 is when we stopped all oncology treatment. And we did one more scan and we haven’t done one since. We’re going to kind of go clinically to see where this goes. They’ve told me that if I want to have a scan, we can do one.
Words of advice
You’ll find that when it comes to cancer, there are people who want to fight and there are also those who want to quit.
I never used to understand those who want to quit, but I’ve learned to do so. It’s important to try and not be judgmental about it.
Clinical trials aren’t for everybody. That’s for sure. If you’re going to do them, you need to be comfortable with the unknown, as I mentioned.
If you decide to join a clinical trial, you should feel comfortable with your doctors and trust them with your life, even though they’re pretty open that they don’t know how things will go with your trial. And you need to find a team you’re comfortable with.
You have to try to overcome your fears. That’s a big thing when it comes to cancer and cancer treatments.
For me, as I mentioned, joining a clinical trial had a great deal to do with wanting to give back, with helping others learn.


Special thanks again to Genmab for their support of our patient education program! The Patient Story retains full editorial control over all content.

Inspired by John's story?
Share your story, too!
Related Cancer Stories
Follicular Lymphoma Stories
Hayley H., Follicular Lymphoma, Stage 3B
Symptoms: Intermittent feeling of pressure above clavicle, appearance of lumps on the neck, mild wheeze when breathing and seated in a certain position
Treatments: Surgery, chemotherapy
Laurie A., Follicular Non-Hodgkin Lymphoma, Stage 4
Symptoms: Frequent sinus infections, dry right eye, fatigue, lump in abdomen
Treatments: Chemotherapy, targeted therapy, radioimmunotherapy
Courtney L., Follicular Lymphoma, Stage 3B
Symptoms: Intermittent back pain, sinus issues, hearing loss, swollen lymph node in neck, difficulty breathing
Treatment: Chemotherapy
John S., Follicular Lymphoma, Stage 4
Symptom: Swollen lymph nodes
Treatments: Clinical trial, chemotherapy



One reply on “John’s Stage 4 Follicular Lymphoma Story”
Great stories! I have been a follicular lymphoma patient since 2020.