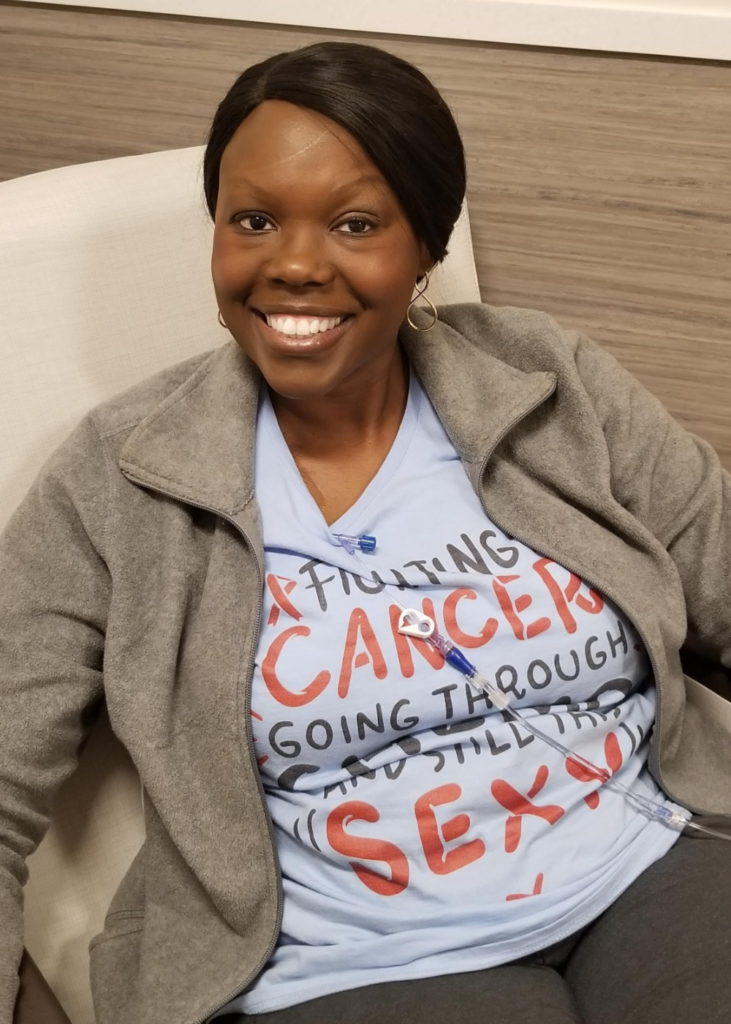
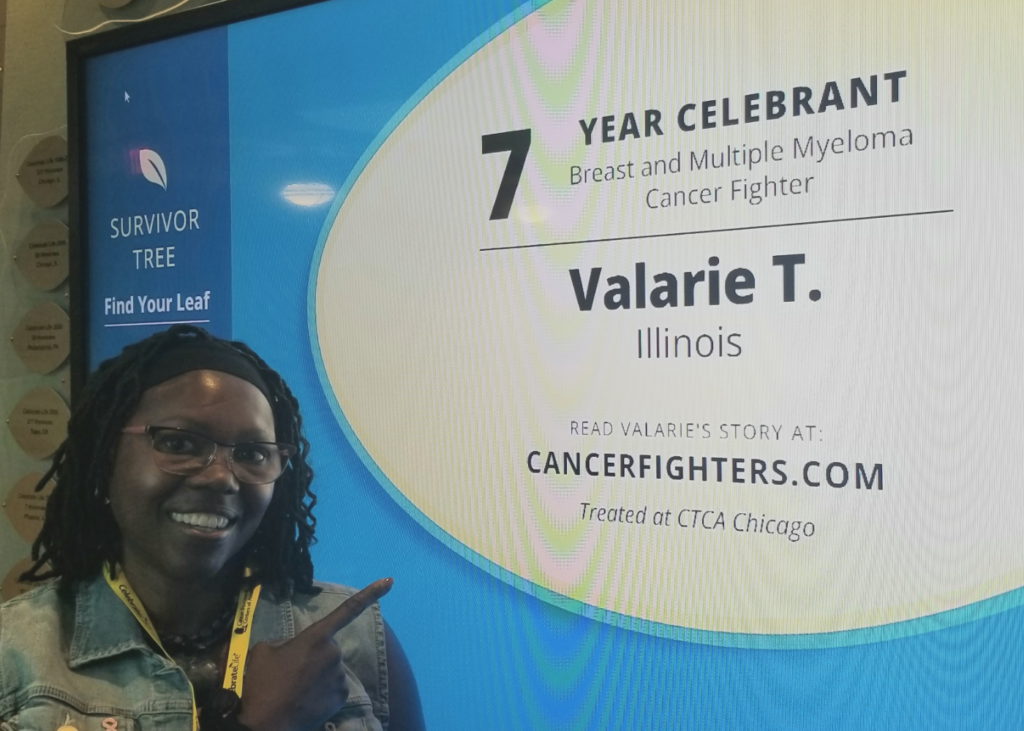
Valarie Traynham:
My Multiple Myeloma Story
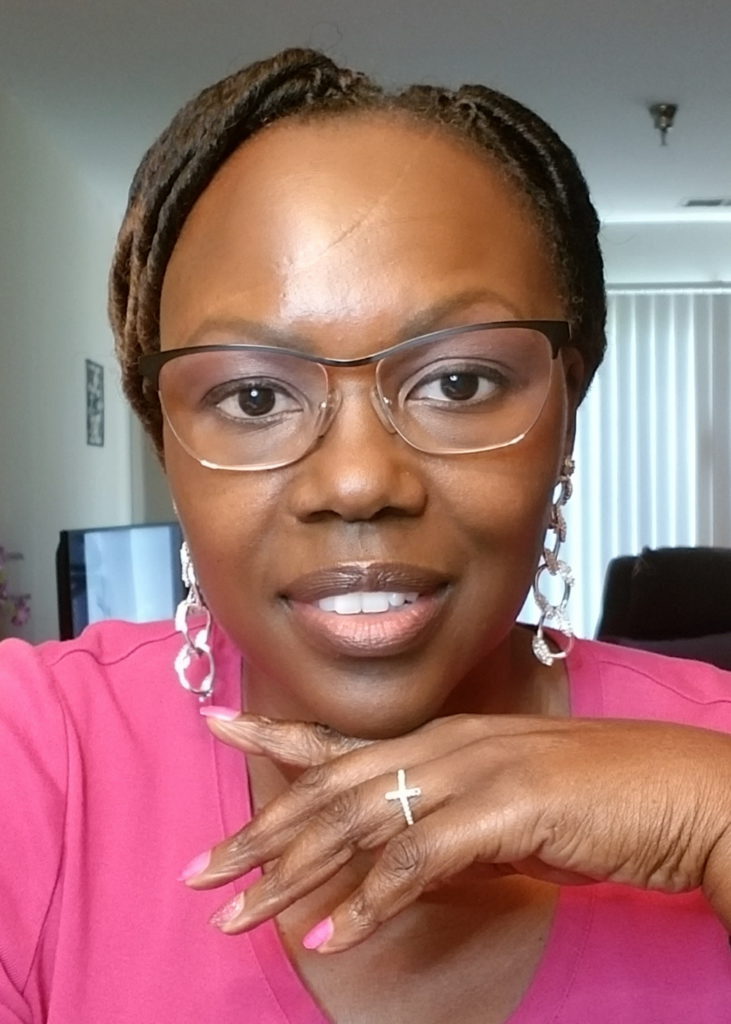
Before being diagnosed with multiple myeloma and breast cancer, Valarie Traynham worked in the human resources field. Since being on the cancer journey, her focus has shifted to patient education and advocacy.
As a cancer survivor, her goal is to learn more about the diseases, educate others and bring light to health inequity. She wants to use her voice for those who cannot speak up for themselves to ensure that they receive equitable access to good healthcare, clinical trials and proper treatment.
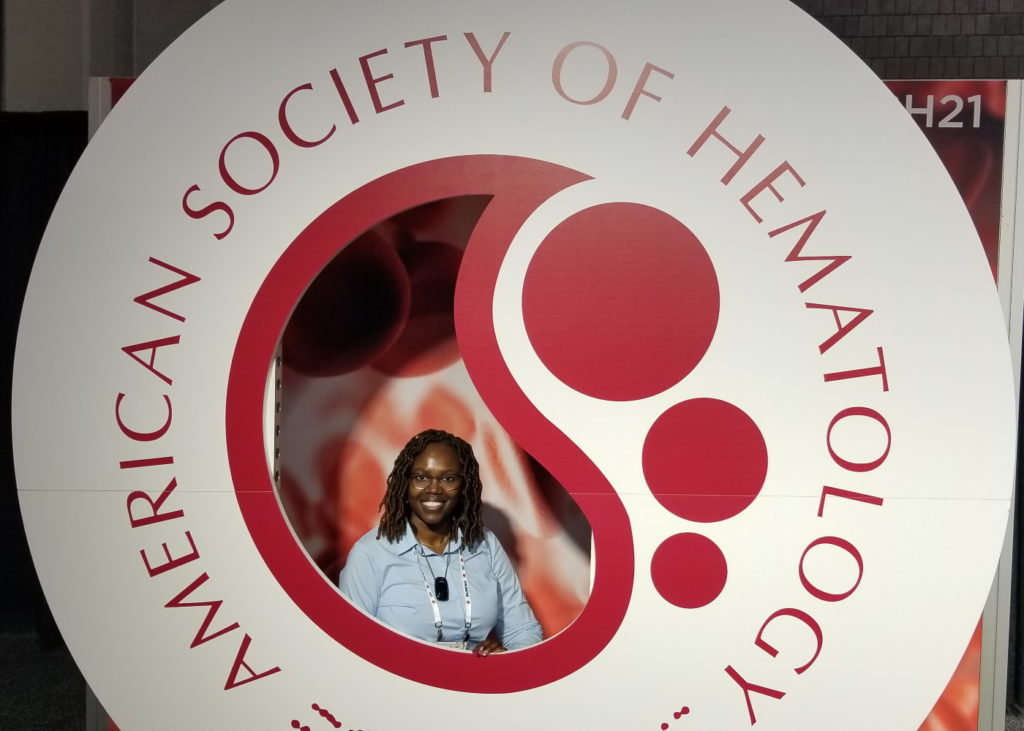
Valarie’s journey in patient education, mentorship and advocacy began when she became a support group leader. She is now a myeloma coach, mentor angel and leader of the Black Myeloma Health Community. She has had the opportunity to talk about disparities myeloma patients face and looks for solutions through partnerships with healthcare providers.
- Name: Valarie T.
- Primary Diagnosis:
- Multiple Myeloma
- Initial Symptoms:
- Nose bleeds
- Fatigue
- Back pain
- Treatment:
- Chemotherapy
- Stem cell transplant
- Secondary Diagnosis:
- Breast Cancer, Triple-Negative
- Staging: 1A
- Initial Symptoms:
- None; caught at a regular screening mammogram
- Treatment:
- Chemotherapy
- Mastectomy
Get educated about your disease. Understand what it is. Knowledge is power. When you get that knowledge, do something with it. Learn how to advocate for yourself. You have a voice. Your voice deserves to be heard so use your voice.

This interview has been edited for clarity. This is not medical advice. Please consult with your healthcare provider for treatment decisions.
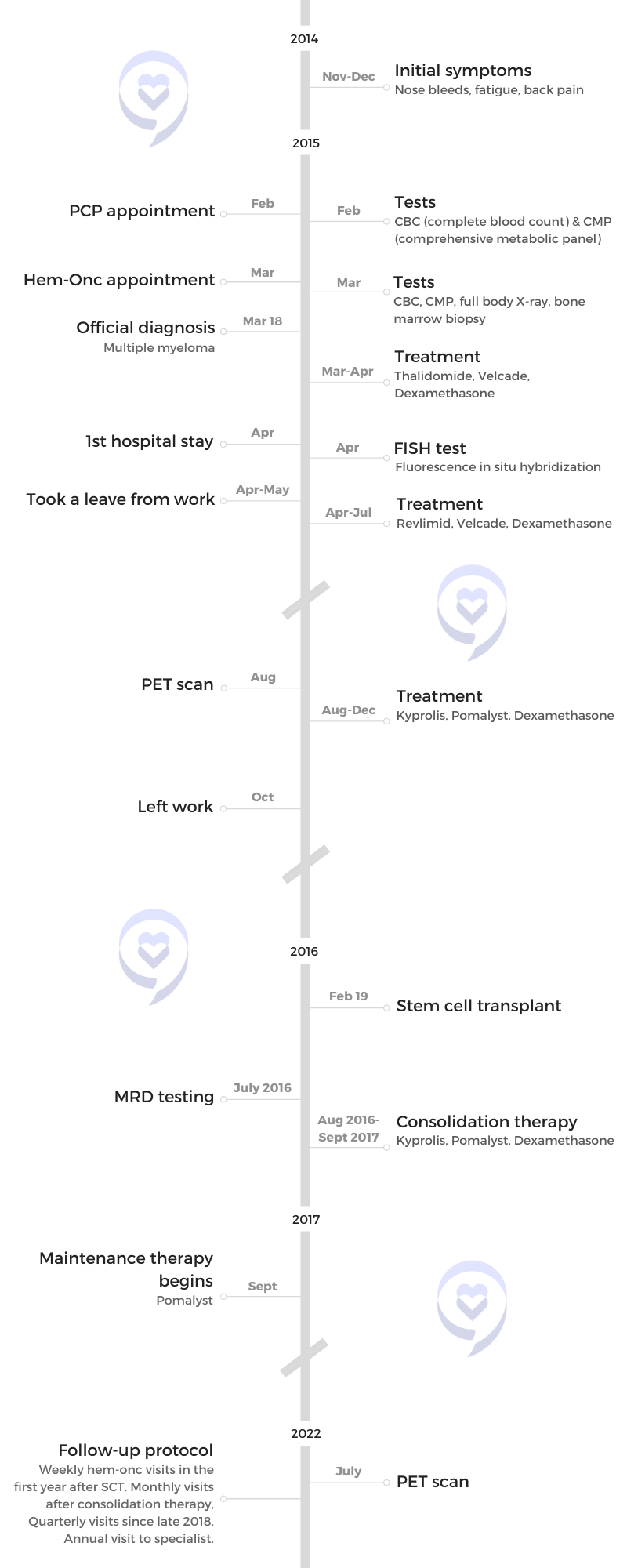
Pre-diagnosis
Introduction
I’m [a] pretty down-to-earth person. I enjoy the great outdoors when it’s warm [and] spending time with friends and family.
What I do is work that’s around myeloma and patient education. I also enjoy doing things at my church. I’m really involved with my church and that brings me great joy.
Initial symptoms
It was late 2014. The first incident happened around Thanksgiving. I went back to school. I was studying and working on some homework on my computer [when] I got a nosebleed. I didn’t think anything of it. I just stopped for a little bit, held my head back, and [it] kind of dissipated [so] I got back to doing what I was doing.
The exact same thing happened [again] a couple of weeks later but this time, it bled a little bit more, a little longer than the first time. I still wasn’t concerned. I thought it was the weather. I’d asked some of my friends, “What do you think’s going on?” And they’re like, “Oh, it’s changing seasons and you probably got just some dry sinuses.” They told me to “just put a little Vaseline in there. You’ll be okay and keep going.” I did that and I thought it was working.

When I got a bout of flu, it just wouldn’t go away.

About a month later, I got sick with the flu and I just felt tired, overly tired. At that time, I was working full-time in HR. I was overly tired when it came to work, but I didn’t think anything of it. I was working, doing schoolwork, [and] very involved in church, so I just chalked it up to just trying to do too much at one time.
But when I got a bout of flu, it just wouldn’t go away. I went to the doctor. I got all the things that you take [that] should [make you] feel better. It was Christmas Day [and] I couldn’t even celebrate because I was sick in bed so I knew something was going on. I went over to my local [pharmacy]. They gave me more meds and said, “If you’re not better by Monday, go see your primary care.” And that’s what I did.
I went to see my primary care physician. I told her what was going on with the tiredness. At that time, I did have some back pain. It was nothing major. I told her about the back pain and the nosebleeds. She listened to what I had to say. She ran a complete panel of blood work and that came back showing high protein so immediately, she sent me to see a hematologist-oncologist. That’s how things started.
When she sent me to the hematologist and I saw ‘oncologist’ tagged on, I knew something was not like it should have been.
Initial hematologist-oncologist appointment
When my primary care referred me to the hematologist, I didn’t think anything of that because I had been diagnosed with anemia many, many years ago and I was taking iron supplements.
It wasn’t until I went to see the hematologist and found out that he was an oncologist as well. I’m like, “Why would I need to see an oncologist?” It was something that snapped in my head at that moment. This is a little bit more than what I’m thinking, but I still didn’t think anything too drastic.
I make this joke all the time. I tell people, “I went to see my hematologist thinking I was going to get a prescription for iron and I came back with a cancer diagnosis.” That’s literally how it happened.
When she sent me to the hematologist and I saw “oncologist” tagged on, I knew something was not like it should have been.

I heard the term ‘biopsy’ and I’m like, ‘Okay, this is really serious.’

Testing
They were a little suspicious from the blood work. At this time, they were still doing the full body X-ray. It was when they did the full body X-rays and the bone marrow biopsy [that] all the pieces started to come together.
Another incident that let me know it was a little bit more serious [was] when they asked me to come back. I went and did blood work for the hematologist early one morning and before I had gotten home, the nurse called and said, “We need you to come back. The doctor wants to do some more tests.” I’m like, “Well, what does he see? What is he expecting?” She wouldn’t say anything so that was another thing. Something’s going on because I haven’t even gotten home and you want me to come back right away.
She told me to come back because they needed to do a bone test. I didn’t know what that was. Little did I know that that was a bone marrow biopsy. When I got there, I heard the term “biopsy” and I’m like, “Okay, this is really serious.”
Importance of a good support system
Luckily, my friend went with me. She said, “I’m not going to let you go back over there by yourself.” I did have some support when things started to unfold.
I remember the doctor talking to me and I heard the words, “You have myeloma. It’s incurable.” I went blank for a minute. It is always helpful to have someone with you [to] maybe ask some questions that you wouldn’t even think to ask [or be] a second set of ears, second set of hands. You want to have somebody there.


Diagnosis
Reaction to the diagnosis
It wasn’t as shocking because I had just learned about my chart. I had been looking at every single test that had come back. If this is high, what does it mean? Multiple myeloma kept coming up and I’m like, “What in the world is that?” But I still put it out of my head.
It wasn’t until that moment I went into the office and was sitting there and heard those words. It was like somebody kicking me in the gut. What? Cancer? An incurable cancer? And that’s when the flood of fear came. I’m going to die. I’m too young to die. Why me? All of those range of emotions. How am I going to tell my family? What do I say? Where do I even start to talk about this?
My friend, Judy, went with me to that appointment. She’s a cancer survivor as well so she was like, “I’m not going to let you go by yourself.” That was very helpful to have someone who has heard those words before. She knew exactly what I could have been feeling so she was there to help me keep it together.
Breaking the news to loved ones
It was hard. I didn’t do it right away. It [took] a couple of weeks. I knew they would have questions that I didn’t know [the] answers [to] or where to even begin.
My friends see me every day and they want to know what’s going on. It was easier for me to say, “Hey, this is what’s going on,” and just left it at that because I didn’t know what to expect.
I don’t live near my family so it was a little difficult. It was hard because I didn’t know what to tell them. I didn’t know the answers. That was one of the most difficult things to do. I finally got the courage to just say, “I’ve got multiple myeloma and this is what it is. I don’t know where it came from. I don’t know anything, but this is what I’ve got. This is what I’m looking at.”




What was very helpful to me was the advocacy agencies… Places like that are very good to provide information.
Learning about multiple myeloma
It was tough to begin with because [of] the shock that you have myeloma. But I learned very, very early. I wanted to learn as much as I possibly could about whatever was invading my body. If I can learn about it, I can at least try to get one step ahead.
For me, I always say it was just a control thing. I felt the more I knew about it, at least I would have some control. That was my mindset so I went on this mission to find out whatever I could about the disease.
It just stuck with me, actually, this whole time. I’m always on a mission to find out a little bit more about the disease.
Finding the right information
It’s different for everyone. What was very helpful to me was the advocacy agencies. I went to the IMF (International Myeloma Foundation) website to find out what you’re going to need to know and some questions. They have some cool tip cards and brochures.
I utilized the MMRF (Multiple Myeloma Research Foundation) website [and] found out what was going on. Places like that are very good to provide information.
At that time, HealthTree was just coming up so I was looking to see what I could find that was going to help me figure out what to ask at what point in the journey.
What is health literacy and why is it important? »
Treatment
I got diagnosed and they wanted me to start treatment the next day. I was like, “Okay, I guess I should go ahead and do this,” because what do you do when you get cancer? You want to get it out of you.
I didn’t start right away. It was probably a week or two later when I went in. I followed what they said because I didn’t know the right questions to ask. I went along with what the doctor [said]. I hadn’t sought a second opinion. I didn’t realize that I needed to see a specialist.

I was in really bad shape at this point. I had to have a wheelchair to get from the car to inside the facility.

Deciding to get a second opinion
About three treatments [in], I just felt horrible. At the urging of my family, they were like, “You got to get a second opinion. You have to. You’re up there where all those doctors are. You have the ability to do that.” I decided to get a second opinion and it’s one of the best things that I could have ever done.
I saw a hematologist at a local hospital. He treated other cancers as well so I realized that that was not the best thing for me.
They started me out with Thalidomide, Velcade, and Dex — that was my treatment regimen to begin with. I didn’t realize that was an old regimen that wasn’t being used and my doctor probably didn’t realize that either that’s why he gave me that. I did about three- or four-week cycles worth and by that time, I was able to get that second opinion.
I was in really bad shape at this point. I had to have a wheelchair to get from the car to inside the facility. I knew something was wrong because that was not me at all. Two months ago, I could still walk and was coherent.
Where I live, there is a facility called the Cancer Treatment Centers of America. Everyone was like, “You’ve got to go there. That’s all they do — cancer, cancer, cancer. You’re going to be in good hands.” I decided to go there.
It was[then] I started learning a lot more about myeloma and the different treatments available. It was through them that I got connected with the specialists.
I came to find out that my hemoglobin was at 4.6 so that’s why I was feeling horrible. I learned that [my regimen] was not the latest treatment. [It] was standard of care, but there was something better.
I also learned about stem cell transplant. We talked about [it] and what that looked like. I learned a lot more than what my local oncologist shared with me. I feel that with my local oncologist, [there] was a lack of communication. I was told, “You’re going to do four cycles of this, then you’re going to go for a stem cell transplant, then you may do a couple more cycles, and then you’ll be back to your new normal.” And I was like, “Oh, okay, so maybe [in] a year things will be back to normal?” And that was not the case.
When I got to the other doctor, he really explained what the process entailed and [that] there’s no certain time. It’s not like you’re going to do this and you’ll be back to your normal life. It was eye-opening because I wanted to believe what I had been told. It sounded so much better and it would have worked for me if that were the case. But life’s not like that.
At first, I was a little angry. How does this even happen? But it happens. It helped me understand that there has to be more done when it comes to awareness and letting people know about myeloma. Letting people know that this is what myeloma is, but also letting them know what treatments are out there, what you should be getting and what [is] probably not the best thing for you to be receiving either.


Side effects
When I switched from Revlimid to Pomalyst, it took a little bit of getting used to because my body was like, “Oh, I don’t think I like that.” I had major GI issues and most people don’t have GI issues with Pomalyst but that’s something that I was struggling with.
Taking those in combination, I had shortness of breath [which] slowed me down even further. I was concerned. There’s the risk of cardiac issues when you’re taking Kyprolis. I got afraid. I’m like, “I don’t want to take that because it may be doing something to my heart. I’m having shortness of breath already.” They sent me to see a cardiologist a couple of times just to make sure everything was okay and [it’s] one of the side effects. I eventually adjusted to that. That’s just part of the new normal so I adjusted and kept going.
I was very vocal. Even if I thought it was a side effect, I would say something because I didn’t know. I looked at the list of everything that could happen but maybe this is something that hadn’t been reported. It is possible.
With Velcade, I did have some neuropathy in my toe area to start with. My doctors would always ask, every week when I would come in to get it, “Are you feeling any numbness, tingling, or anything of that nature?” Even if it was a small amount, I would make sure that I said something so they could do something about it and that was very helpful.
Velcade is a subcu (subcutaneous injection) and I’m sure most people would have those little spots on their abdominal area wherever the shot was given. Sometimes it could be painful and I would tell them so they could guide me on what to do. [There] wasn’t a whole bunch they could do. It’s just unsightly. It’s a reminder of what you’re going through but still, I was very vocal in letting them know what was going on.
With Revlimid, one of the first things that scared me is I woke up itching one morning. It started as an itch on my legs. Did something bite me? Is it a mosquito bite? Before the end of the day, I was just itching all over uncontrollably. The more I scratched, the worse it got. Nothing would take it away. I called the doctor and they called in a prescription that would help. But people need to be aware of that. I didn’t know that could happen. I was surprised. What the heck is going on? It was really bad.
I realized that I’m not in control of this or anything else.

Dealing with treatment roadblocks
It was that word: control. It was then that I realized I’m not in control of this or anything else. I did all the things that I was supposed to do. I got my knowledge. I have no control.
All of those feelings, I just sat with them. I didn’t try to push them away. I just said, “You’ve got to deal with this. You’re going to have to deal with this.” And I just dealt with it.
My faith played a very important role. I had my prayer partners praying and that helped me tremendously. And I sought some therapy because I knew I can’t do this by myself. It’s not something that I can just pray away. I really needed some outside help.
I needed somebody that was going to listen and just listen. I couldn’t talk to my friends because they didn’t understand. They just hadn’t been there. They didn’t know. Therapy was one of the best things I could have done because my therapists helped me through the process.
My faith played a very important role… And I sought some therapy because I knew I can’t do this by myself.
Stem cell transplant
Preparing for stem cell transplant
I did four cycles of treatment thinking it was going to bring down the disease burden to where I could move forward with [the] transplant. At the end of my four cycles, I’m thinking, “Yes! It’s [the] transplant.” It didn’t happen. I hadn’t eliminated enough of the cancer cells in order to move forward.
Then comes the conversation of [needing] to do more therapy. We’re going to continue the induction therapy. That’s when I found out about myeloma clones. Never heard of that until I was about six months in. It’s those little things that if you know, then you can be better prepared.
I wasn’t prepared to be told [I] can’t go to transplant. It’s so funny because I went and shaved my head. I was like, “I’m going to shave it all off before it happens.” And they’re like, “No, you can’t. You’re not ready for that yet.” I was disappointed, a little angry, [and] just bewildered. What’s happening now? Another gut punch.
Find answers to popular stem cell transplant questions and experiences »
Induction therapy
I got switched to Revlimid, Velcade, and Dex. I did four additional cycles. [When] it wasn’t working anymore, I was switched over to Kyprolis, Pomalyst and Dex, and I had [an] immediate response. That’s what really got me ready for the transplant.


Expectation setting
Going into the transplant, I was told what I could expect. I used to follow The Myeloma Beacon. I started following Pat Killingsworth and listened to what he said. I got his book about stem cell transplants. I read the book and I’m like, “I’m going to make sure I do everything that they say to do.”
Follow the advice of your doctors and nurses. They do this every single day. They can tell you how to prepare. I listened and followed some of the big names out there. These people know what’s going on and that helped me prepare for the transplant.
The week before the transplant, I found out my insurance was not going to cover [it] where I wanted to do it. That was something else that had to be worked out. Eventually, we got it taken care of but that was a very stressful time just trying to figure [it] out. What am I going to do if the insurance is not going to cover it here? What do I do?
Dealing with insurance issues
I was working with the stem cell transplant navigator at the hospital. She was such a godsend because I didn’t know what to do. I did not need the stress. She was like, “Hey, this happened. We’re going to take care of it,” and she just knew the right things to do.
I had everything in place. My family was coming out to spend time with me. A couple of my friends had taken off work. They had taken vacation time to be there for me. So when I heard this, I’m like, “Whoa, everything’s in place. It can’t just not happen because it’s going to affect other things.”
She helped me get it all worked out. Have somebody working on your behalf. Don’t try to do it all by yourself. If you’re one of those people [who thinks] you don’t need help, you do need help. Someone to help you with paperwork, to make phone calls for you, to do that type of work for you. People want to do that so let them.
The stem cell transplant navigator was excellent. My other friend, Karen, was excellent [at] making phone calls and doing things. I didn’t have to stress a lot because they made sure that things were taken care of. They [took] the pressure off of me.

Don’t try to do it all by yourself. If you’re one of those people that think you don’t need help, you do need help. People want to do that so let them. When things come up, let them.

Stem cell transplant process
It was a little scary at first. I was going into the unknown. I didn’t know what to expect. They told me, “On this day, you’ll go in. You’ll get the high-dose Melphalan. Make sure you chew ice chips. Then you’ll have a rest day and then you’ll get your stem cells back.”
A couple of weeks before, they give you shots that stimulate the stem cells. I had to give myself those shots in my stomach and that was a process because I never had to give myself shots before.
After four days of shots, I went to the facility to harvest the stem cells. They put this big catheter in your neck, which feels really, really weird. It was very painful for me to do the apheresis and get the circulating stem cells from the blood. That process was a little scary because you don’t know what to expect. You’re laying in bed hooked up to this machine and you see the blood going out of your body and being flushed back in.
I was very fortunate. I got all of the cells I needed in two days so I didn’t have to come back. They told me it could take four days to collect the cells.
I didn’t go for the transplant right away. I waited a couple of weeks and something was going on with my schedule and I wasn’t able to go.
Then came the insurance issue. My cells were frozen for a couple of weeks. I [went] back to the facility and had to reinsert the Hickman port — very uncomfortable to go through that process.
I’m admitted to the hospital. They test for C. diff (clostridium difficile infection) and lo and behold, I’m positive for C. diff so there’s another component that you don’t expect. That means I’ve got to be isolated in addition to the transplant. Other precautions had to be taken as well.
I remember it was a Wednesday evening. It was a very long day. I get the high-dose Melphalan and I’m chewing on ice chips. Thursday was my rest day. Bright and early Friday morning, the nurse comes in, checks all my vitals and she’s like, “This is it. This is the big day.”
A couple of hours later, the other nurse came in with this little bag of cells and I’m like, “This is the life-sustaining things that I’m going to get back.” At that time, a couple of members of my family had come up. My friends had taken off work to be there for me, supporting me. They kept a chart to let me know what was going on outside of the hospital.
I received my cells back. It was Friday morning [at] about 11:40, [I] celebrated my new birthday and the rest is just waiting to see what happens.
Recovering from the stem cell transplant
One of the most trying times was waiting for that engraftment period. I didn’t feel too bad the first couple of days. [On] the third day, I could start to feel something’s going on. The fourth day [was] okay.
On the fifth day, my head started to hurt. Every time I would run my fingers through my hair, it would just hurt tremendously. I’m like, “What the heck is going on?” Little did I know that was the beginning of the hair getting ready to fall out. And that was tough, even though I knew it was going to happen. It was still tough when it did happen.
Like clockwork, on day five, all my numbers bottomed out. I was feeling horrible [and] had the worst diarrhea that you can imagine. I felt that I was going to die. I woke up that morning and I was like, “Oh my God, I could die from this.” At that time, I was alone. My visitors hadn’t come in yet and I was just sitting there like, “I could die. If I get an infection, I could die. There’s no way I can fight it off.”
There was another patient undergoing stem cell transplant [who] had been there a few days before I’d gotten there, caught an infection and didn’t make it. Just knowing that on top of everything else, I was a basket case.
But I had great doctors, great nurses [and] a great team of people [who] took care of me and pulled me through it. They would come in every day, check on me, do what they had to do, and say, “Hey, you got to keep positive. You will get through this.” And I believed them because they do this every day. Why would I doubt them?
Recovery was really hard. The thing that surprised me most was the overwhelming fatigue. I would get up, sit on the side of the bed and go, “Oh, I can’t do this today,” and lay back down for a little bit. Then realize, “Okay, you’ve got to get up. You can’t just lay here in the bed. That’s not going to be helpful to you,” so I managed to get up. Then it was like, “Okay, let’s get to the shower,” so I would manage to get a shower, but I [got] out of the shower and I [had] to lay back down again. I’m like, “What in the world is going on? I can’t even hold my arm up.” That went on for a pretty good while.


I didn’t have to worry about cooking, cleaning, or anything like that. My friends were very good with making sure I was taken care of [so I could] take my time and get better. I made myself get out, walk to the mailbox, [and] walk around the block just to get some exercise. When I did that, I did feel better. There were times when it was 1:00 or 2:00 in the afternoon and I felt I needed a nap. I listened to my body.
Maintenance therapy post-SCT
We talked about what was going to happen after the transplant and we agreed on consolidation therapy. That was very popular at the time. Some doctors were doing it, some were [not]. We talked about doing consolidation for about two to three months after the stem cell transplant.
Consolidation therapy is just a continuation of the therapy you were on before you went for the transplant. You just do it a little bit longer to deepen the response to try and get rid of more of the disease burden.
When you look at that myeloma iceberg, consolidation therapy chips away at that iceberg a little bit more. We talked about doing that for two to three cycles more and that eventually turned into a 12-month cycle.
I really didn’t fully understand that at first. “We talked about two to three months. What are you talking about?” But when they explained to me how we want to deepen the response, I’m like, “Oh, okay. I guess I can go through this a little bit longer.” In my mind, that’s going to give me a longer remission, help me live longer, [and] help me live as much as normal life as I possibly can. I fought it at first but when I saw the risk-benefit, why not?
Consolidation therapy
We talked about what’s next long before the end of 12 months because I [didn’t] want any surprises. We talked about just doing Pomalyst, going on a single regimen for maintenance.
[While] I was going through consolidation therapy, I did MRD testing. I did find out I was MRD negative, which I was really excited about. I understood what MRD negative meant so I [asked], “Do I still need to do maintenance?” Because we had talked about going on maintenance indefinitely.


Side effects from Pomalyst
Once I completed the consolidation therapy, I went right into maintenance therapy. I didn’t have any problems with it [initially] but eventually, it did weaken my immune system to a greater magnitude to where my counts were always low.
I was doing monthly blood work. I had to do that in order to get Pomalyst. My counts were consistently low. I was having to get the Neupogen [and] Neulasta shots to build my ANC (absolute neutrophil count) up.
At that time, my hemoglobin was still borderline. I was still often fatigued. I had a conversation with my doctor about that and they were like, “Okay, maybe we can do a dose reduction.” We talked about that, what that meant and what it looked like. I did a dose reduction and that did help improve my numbers to where I was not as bad all of the time.
I stayed on that particular dose for a couple of years then the same thing started to happen. I was experiencing bone marrow suppression. It was really bad so we did another dose reduction. I told him what was going on, how I was feeling, [and] how it wasn’t improving. You could see it in my blood work. Every month, it was the same thing.
We decided to do another dose reduction and found a happy spot where I’m comfortable. I can live freely, so to speak. I’m comfortable doing things without fear my counts are low. And this is before COVID. You have to go out in a mask and it’s like, “I don’t want to do this.” You [can’t] participate in events because you’re afraid. If I get this least little thing, I’m going to be sick and down for days. It relieved that. It made things better.
Testing for minimal residual disease (MRD)
MRD stands for minimal residual disease. It is the test to determine if they can detect any myeloma cells after transplant or induction therapy. It wasn’t something they did on a regular basis back [then]. When I had that test done, I was very happy to hear that I was MRD negative.
My doctor and I had talked. “After you finish consolidation therapy, we’re going to put you on a single agent Pomalyst as maintenance.” My question was, “What if I’m MRD negative? You just said I don’t have any traces. Why should I take this? Why should I want to continue with the maintenance again?” They explained to me [that] the goal is to get rid of as much myeloma as possible, chip away at as much of that iceberg as possible.
When I saw the benefits, I made that [decision]. It was ultimately up to me if I didn’t want to do maintenance. All I had to do was say, “No, I don’t want to do that.” The doctors would have been okay with that.

That’s one thing I learned: shared decision-making. You have to have a say in it because ultimately, it’s your body, it’s your quality of life so make sure you have a say in what’s going on. Don’t just go along with it.
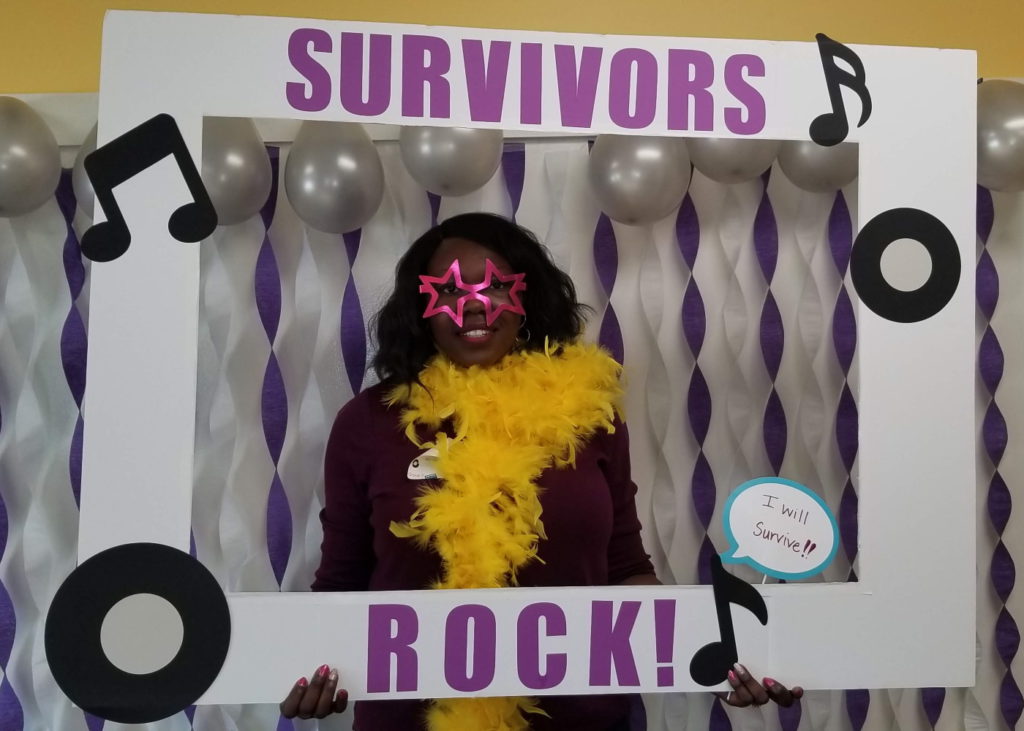
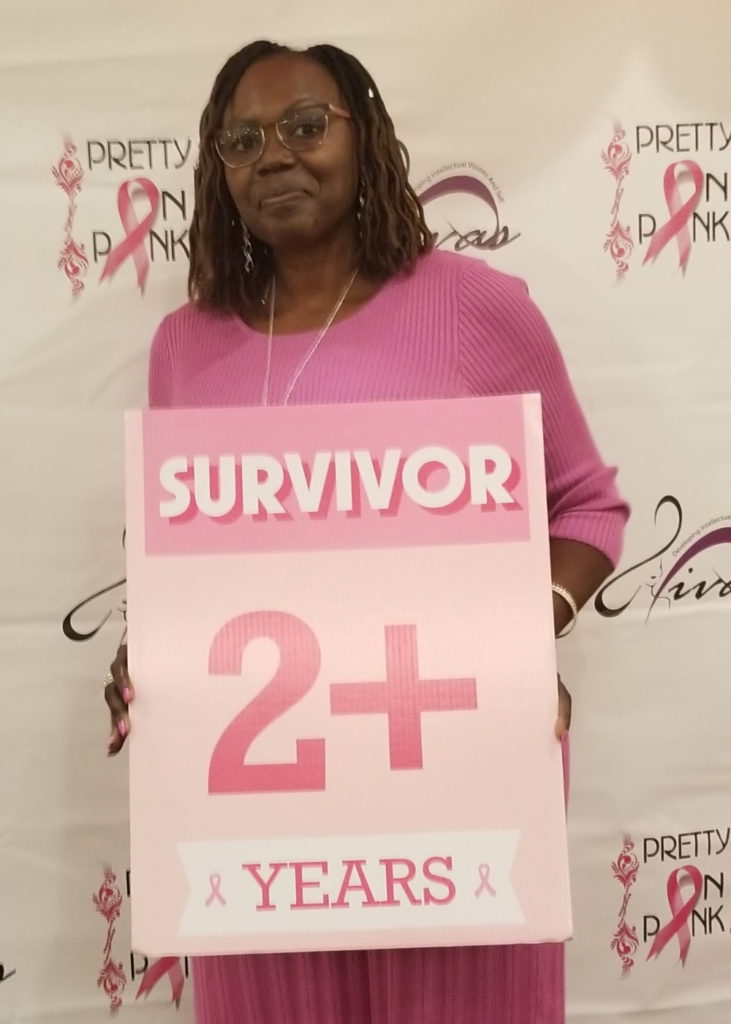
Receiving a second cancer diagnosis
I was doing well, trying to get back on track to my new normal and along came a breast cancer diagnosis. This was out of nowhere.
I was going for my yearly mammograms and always was told, “You have dense breasts. Just keep an eye out for things and we’ll see you back next year.” At this particular time, I went for my mammogram and got a callback. They [said] “We want you to come back. We need to do an ultrasound.” I didn’t think anything of it. I’m going to go back and they’ll do an ultrasound and tell me I’m good. That was not the case this time.
They picked up something on the screening mammogram [so] they pulled me back for a diagnostic mammogram and ultrasound. When they did the ultrasound, they did see a couple of things that were not on the previous year’s ultrasound so I was sent for a biopsy.
I’m not saying the treatment was easy — it wasn’t — but knowing the right questions to ask at the right time, I knew how to advocate for myself a lot better.
I was scared. At that point, I knew what biopsy meant. They’re looking for something. They don’t just send you for a biopsy. It was breast cancer. Here I am again, that whole gut kick. Again? Really? Where did this come from? What did I do to deserve this?
But I will say, having been on the myeloma journey and knowing a little bit more, it was a little easier to manage this. I’m not saying the treatment was easy — it wasn’t — but knowing the right questions to ask at the right time, I knew how to advocate for myself a lot better than I did going into the multiple myeloma. That’s been an added step to my journey. I’d like to say [that] myeloma prepared me for the things that I went through with breast cancer.
Dealing with a second cancer diagnosis on top of myeloma treatment
With the breast cancer diagnosis, I was terribly scared. I’m going to have to get treatment for this. Is that going to trigger something in the myeloma? That brought about this fear. Am I safe to do this?
The breast cancer diagnosis was very early stage — it was stage 1A. There was no lymph node involvement but the location of the tumors [meant] I [had] to have a mastectomy. That is a whole ’nother beast. The blood cancer was almost like an invisible cancer. It was something that was going on within your body.
With breast cancer, it was a lot different. It was harder. Having to have [my] breast removed was very difficult for me to accept in the beginning. This was just too much. I can’t go through this. I just can’t do this. It’s just the thought of amputation. I was very fearful.

Even though I was prepared as a patient, I was still very fearful because I didn’t know what the treatment would bring. I didn’t know [what] the side effects would be. Again, I tried to be positive about things and look for the silver lining.
My breast cancer was triple negative. There’s no pill that I can take to suppress anything. Again, I was very fearful. What if I go through all this — I have this chemo and I have my breast removed — what if it’s still there? What if it comes back because it’s triple negative and it’s not as easy to treat? I was dealing with a lot of fear in that instance as well, just like I was with the myeloma.
What helped me was I just sat there in the fear. I acknowledged that fear. I was thinking, Okay, you’ve gotten through myeloma. You can get through this, too. It’s very early stage. I was in a good position, if that makes sense. I don’t [think you’re] ever in a good position with any cancer, but I was in a good position where I wasn’t too concerned.
My doctor assured me early on. “We can take care of it. This will not take you out, Valarie.” That was very reassuring to hear. The oncologist said that the surgeon said the very same thing. Very supportive and [guided] me through that process as well.


How culture influences health care
There are so many things that vary from culture to culture. A lot of times, cultural beliefs prevent people from moving forward with a certain treatment. Not just stem cell transplants, but certain treatments. Receiving blood — certain cultures just don’t do that. Those things have to be acknowledged.
You have to understand someone’s culture in order to understand why they would make certain decisions. Culture is a big influence on decision-making in many instances.
Dealing with the healthcare system as a black woman in America
Being a myeloma coach, I get to talk to myeloma patients, many [of] who have been newly diagnosed and [have] been on the journey for a while. I get to hear a lot of what they have been through or how many times they had to go to the doctor to get a proper diagnosis.


I realize that I’m very fortunate. My primary care knew the tests to run, picked up on the high protein, and sent me to see a hematologist. I know that is not always the case. People may have to go to the doctor two or three times before they even are heard to say, “Hey, this is what’s going on.”
I talked to many people who, when they get to the doctor, find out that they’re in kidney failure. On top of having the disease, it’s the shock of how you are told that you have the disease. Those are the types of things patients deal with.
I was talking to this lady. She went to the doctor [and] finally got the diagnosis, but they wanted her to wait to start treatment. They didn’t want to start treatment right away. Why would they want you to wait? That doesn’t make sense. I see that that doesn’t make sense, but as a patient who doesn’t know how things are supposed to work, that may seem normal.
I was told about [the] stem cell transplant early on in the process. There are patients [who] are not told about that. They’re just told, “We’re going to utilize this treatment and if this doesn’t work, then we’ll go to something else.” This was before we had so many novel therapies so it’s not like you had a lot to choose from. It was just assumed you don’t want a stem cell transplant, you may not be able to get to the facility, or you may not have the support to go through a transplant. It’s just varying things that patients have to deal with when it comes to health inequities.
As a doctor, you have to talk to your patient and find out where there is hesitancy. You can’t make the assumption that someone just doesn’t want to do it because they just don’t want to do it.
Sometimes it’s not discussed simply because it’s not talked about. And that’s very unfortunate because of the bias. You’re making that assumption just because I live in a certain zip code that maybe I shouldn’t do this, I wouldn’t want to do this or I don’t have the ability?
A lot of it is just access to care. We [have] to make sure that we’re getting the patients to the right place at the right time. We have to break down those barriers.
I’m not a doctor, but as a doctor, you have to talk to your patient and find out where there is hesitancy. Let’s say you talk to someone about a stem cell transplant and they decide they don’t want to do it. You have to find out why. Is it that they don’t want to do it or [do] they have other things creating barriers [that don’t allow] them to do it?
Child care. If you have children, you can’t just say, “Hey, I’m going to shut down for two weeks to be in the hospital and then I’ve got 100 days of recoup time.” Who’s going to take care of things? Who’s going to take care of the house, particularly if it’s not a two-person home? Getting back and forth to the clinic [for] follow-up visits. All of those things need to be taken into consideration. You can’t make the assumption that someone just doesn’t want to do it because they just don’t want to do it. There may be underlying reasons.

People need to understand that they play a very important role in their treatment decisions. You don’t have to just go with the flow.

Importance of shared treatment decision-making
It’s a game changer, particularly for patients who are accustomed to just going along with what the doctors say. In the African-American community, that’s kind of the norm. The doctor knows best. He knows more than you do about the disease. You need to follow what you’ve been told. That’s just instilled in a lot of us. But that’s not the case. It doesn’t have to be like that.
People need to understand that they play a very important role in their treatment decisions. You don’t have to just go with the flow. You don’t have to follow what the doctor is saying blindly because you don’t think you can say anything. You can say something and you should. Because again, it’s your life. You have to live with the side effects. You have to live with the treatment schedule so you want to have as much say as possible in that.
All of those feelings that I was still in, I just sat with them. I didn’t try to push them away.
Words of advice
It was my faith that really pulled me through and knowing I’m going to get through this. I believe that I’m going to get through this. I’m trusting the process, as they say. Just trust the process.
You have to acknowledge those feelings that you have because if you don’t acknowledge them, they would just eat away at you. Tell somebody. I told my friend, “I felt like I was going to die this morning. I really felt that. I didn’t know what was going to happen, what could happen.” And that was very helpful when I let that out, when I released that and said something.
You can’t ignore your feelings because they are not going to go anywhere. They’re going to be there. They want to be acknowledged. I acknowledged every thought that came. I’m scared. I might die. It was just getting it out there and releasing it. Having that release was very helpful in my situation.
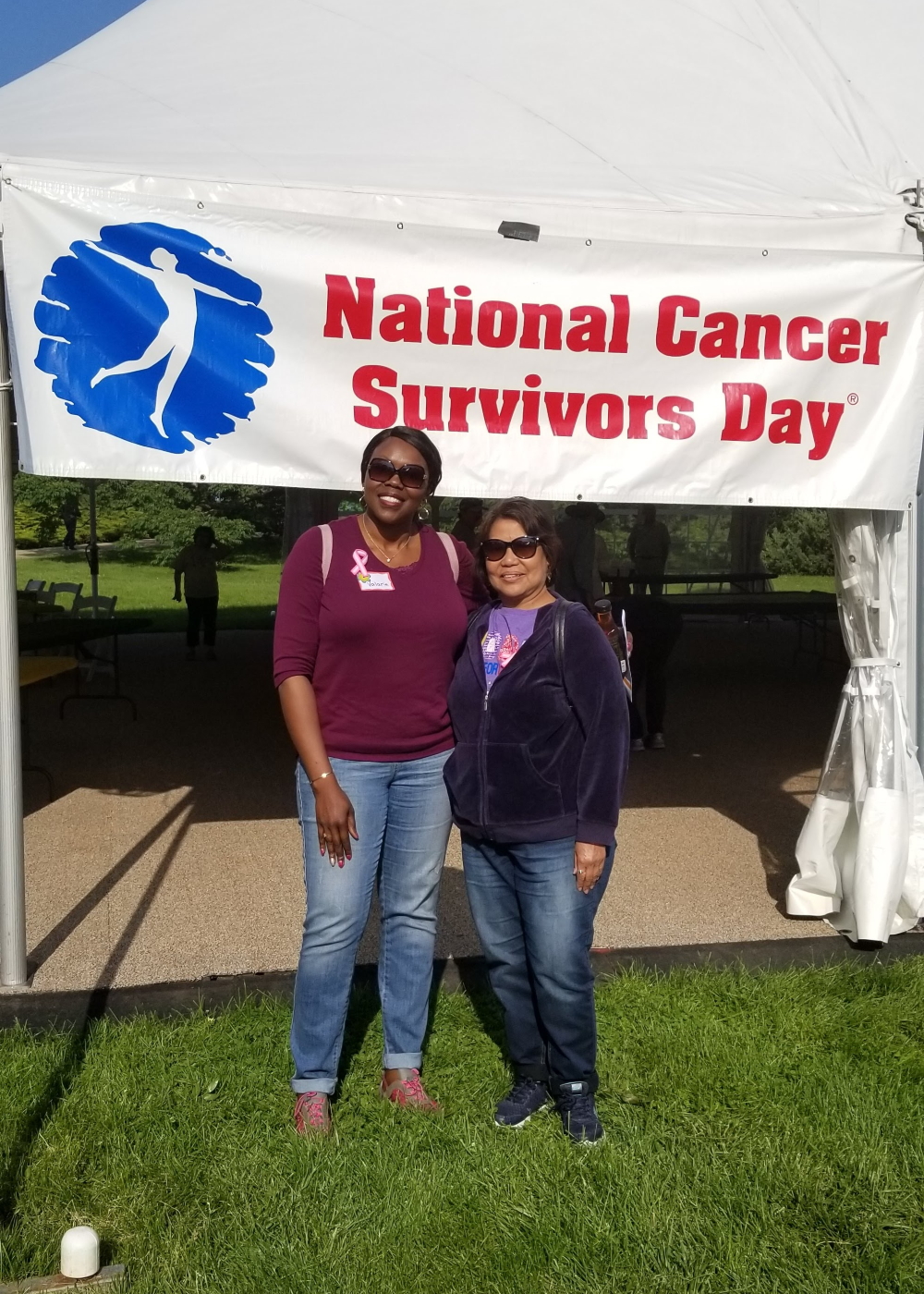
Find something that’s going to give you hope. Very early on with the myeloma, I got connected with others [who] were on the journey. Get connected with others that have been on the journey.
About six months into my diagnosis, I met a 26-year survivor and that just brought me so much joy. I was like, “26 years? You lived? I can do that, too! It’s possible for me, too.” Meeting that individual gave me so much hope.


Don’t think you’re alone in this. You’re not alone. There are so many people dealing with a lot of the same things that you’re dealing with. Reach out to those people. Get connected. Whether it’s through a support group or a group at your church, get connected.
One thing that you don’t want to do is shut yourself off from people. Don’t shut yourself off because that’s not going to do you any good.
Make your needs known. People don’t know what you need. They can speculate. “Oh, she’s going through cancer. She may need this,” or “Oh, she just got out of the hospital. She may need this,” but don’t make people guess. Let it be known because people want to help. They’re willing to help but a lot of times, they just don’t know what to do so you got to tell them.



Get educated about your disease whether it’s myeloma, breast cancer or any other kind of cancer. Find out about the disease. Understand what it is. Don’t just listen to what people tell you. I’m not saying you have to be this research advocate. Knowledge is power.
When you get that knowledge, do something with it. Don’t just sit on it. I think that’s where we make the mistake a lot of times. We have all this knowledge and then we don’t do anything with it. Learn how to advocate for yourself. You have a voice. Your voice deserves to be heard so use your voice.
Look for the positive. I try to be positive about everything. [There’s] a silver lining somewhere. Find that silver lining.
Listen to your body. Don’t think that you have to get back to life. You have to heal. You have to listen to your body and take the time that you need to get well.
Sometimes, people are afraid to speak up because of embarrassment. “I’ll just deal with it.” Don’t suffer through. There are things that can help you get through so take advantage of those things. Utilize those things. Communicate with your doctor. I know a lot of people are not comfortable talking to their doctors. Talk to the physician’s assistant. Talk with the nurse practitioner. That’s what they’re there for.
You [have] to speak up. If patients are heard or feel they are heard, that would change the whole dynamic. A lot of people, if they feel they’re not heard, they’re going to stop talking. It’s not going to benefit them.

Listening and understanding — listening for understanding and not just listening to say, “Well, I heard what they say. It still doesn’t make sense to me.” It may not make sense to you, but it’s still acknowledging what the patient said, what’s been said.
Find others on the journey. Connect with others. Educate yourself. Knowledge is power.
Don’t think you’re alone in this. You’re not alone.

Inspired by Valarie's story?
Share your story, too!
Multiple Myeloma Stories
Clay D., Relapsed/Refractory Multiple Myeloma
Symptoms: Persistent kidney issues, nausea
Treatments: Chemotherapy (CyBorD, KRd, VDPace), radiation, stem cell transplant (autologous & allogeneic), targeted therapy (daratumumab), immunotherapy (elotuzumab)
...
Melissa V., Multiple Myeloma, Stage 3
Symptom: Frequent infections
Treatments: IVF treatment & chemotherapy (RVD) for 7 rounds
...
Elise D., Refractory Multiple Myeloma
Symptoms: Lower back pain, fractured sacrum
Treatments: CyBorD, Clinical trial of Xpovio (selinexor)+ Kyprolis (carfilzomib) + dexamethasone
...
Marti P., Multiple Myeloma, Stage 3
Symptoms: Dizziness, confusion, fatigue, vomiting, hives
Treatments: Chemotherapy (bortezomib & velcade), daratumumab/Darzalex, lenalidomide, revlimid, & stem cell transplant
...
Ray H., Multiple Myeloma, Stage 3
Symptoms: Hemorrhoids, low red blood cell count
Treatments: Immunotherapy, chemotherapy, stem cell transplant
...




