Nick Napolitano’s Polycythemia Vera Story
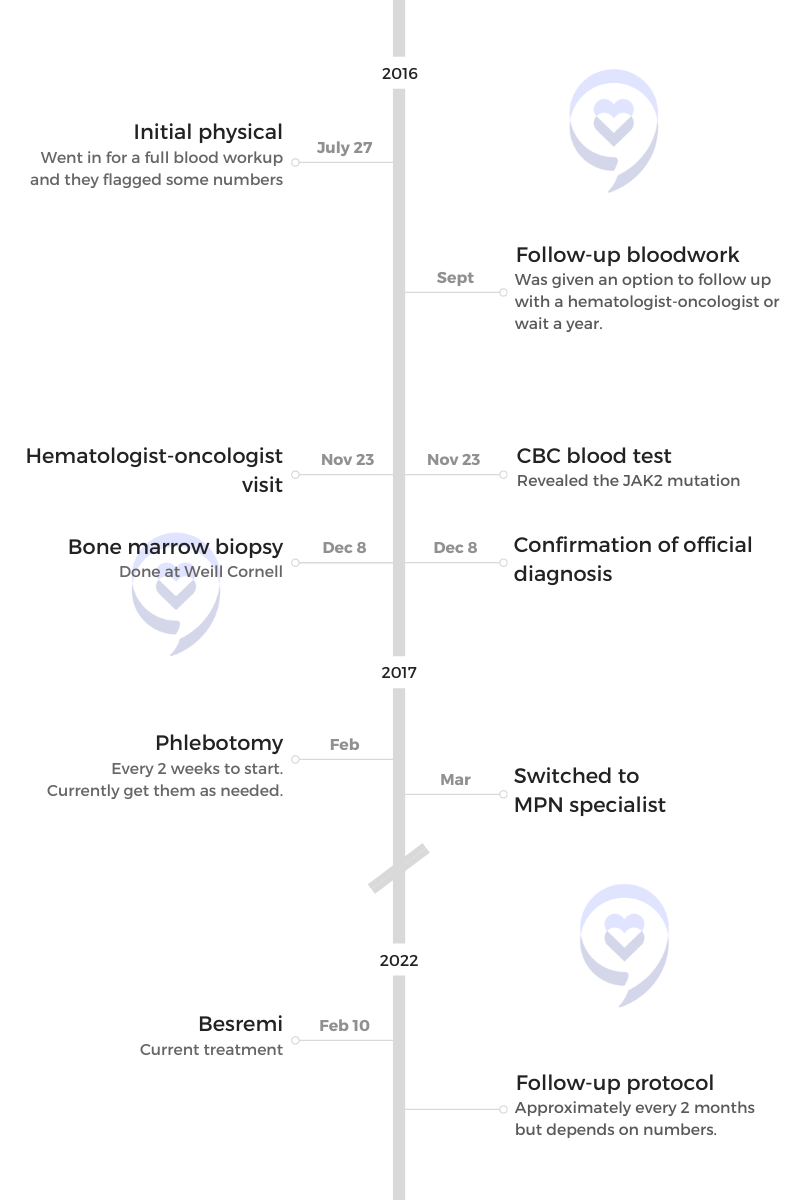
Nick Napolitano almost didn’t get the physical that eventually led to his polycythemia vera (PV), diagnosis. He had always been relatively healthy but he decided to take the day off to get a work-sponsored annual physical. After the exam, some numbers were flagged in his blood work.
He knew something was off when the doctor wouldn’t share his results over the phone. After a biopsy at Weill Cornell Medicine, Nick’s diagnosis of PV, a subtype of myeloproliferative neoplasms (MPN), was confirmed.
Polycythemia Vera (PV) is a rare, chronic blood disorder characterized by the overproduction of red blood cells in the bone marrow. Often white blood cells and platelets are overproduced as well.
After some initial hesitation, Nick found that sharing his story was the jumping-off point he needed to feel comfortable sharing his cancer journey. He’s since starred in a documentary about PV to raise awareness for MPNs.
He shares the journey of his day-to-day life with polycythemia vera, the emotional and mental toll of his diagnosis, and the importance of seeking and seeing an MPN specialist.
This interview has been edited for clarity and length. This is not medical advice. Please consult with your healthcare provider to make informed treatment decisions.
The views and opinions expressed in this interview do not necessarily reflect those of The Patient Story.
- Name: Nick N.
- Diagnoses:
- Polycythemia vera
- Symptoms:
- No symptoms, caught at routine physical
- Treatment:
- Phlebotomy
- Besremi (ropeginterferon alfa-2b-njft)
- Follow-up Protocol:
- Approximately every 2 months, but depends on the numbers
You have to look at it as a whole and really be in it for the long term.
- Introduction
- Pre-diagnosis
- Diagnosis
- How did the meeting with the hematologist-oncologist go?
- What was your reaction to the diagnosis?
- How did you break the news to your family?
- What were the next steps for you and Kara?
- What was the emotional impact of the diagnosis?
- How did you manage your way through the polycythemia vera diagnosis?
- Why did you decide to go to Weill Cornell Medicine for cancer treatment?
- How was your bone marrow biopsy experience?
- How did you deal with all-consuming thoughts?
- Living with polycythemia vera (PV)
- Treatment for polycythemia vera
- Words of advice
Introduction
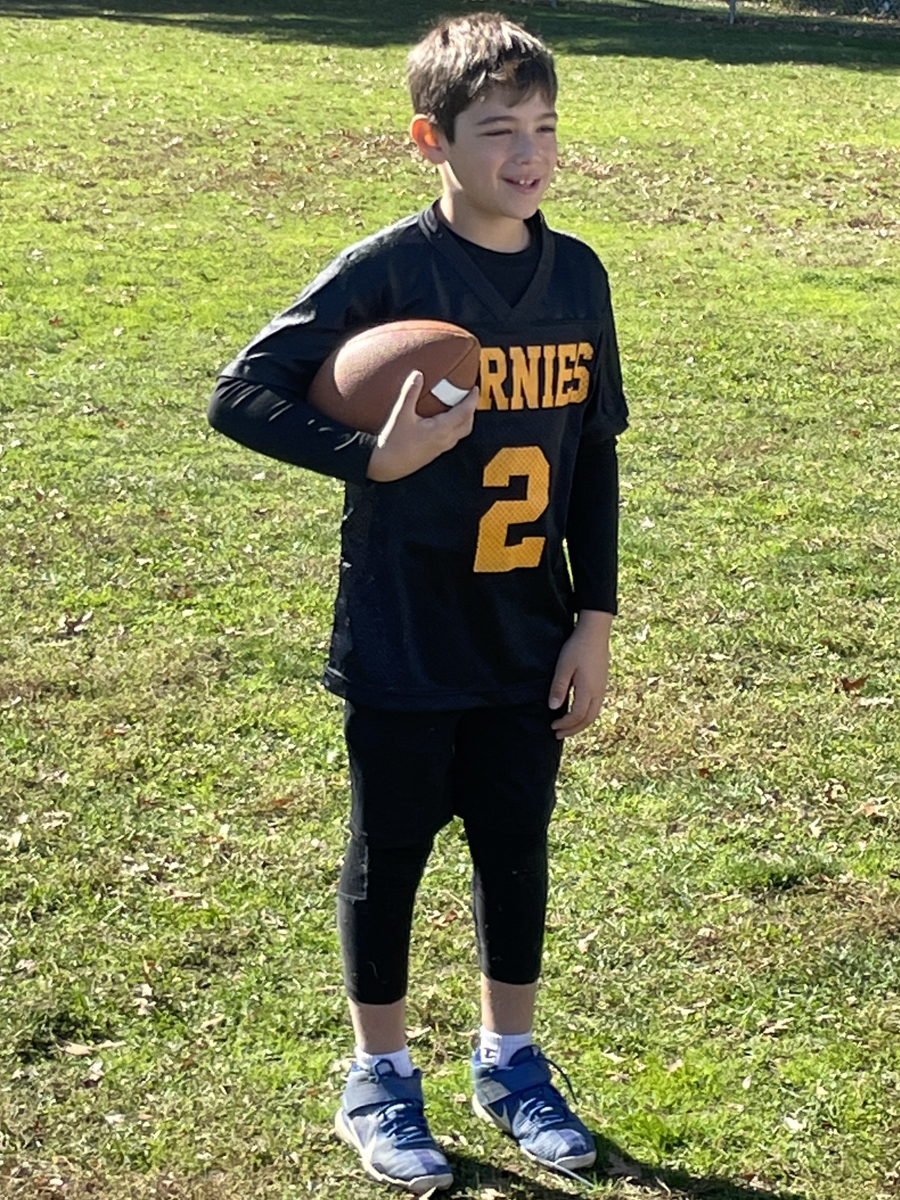
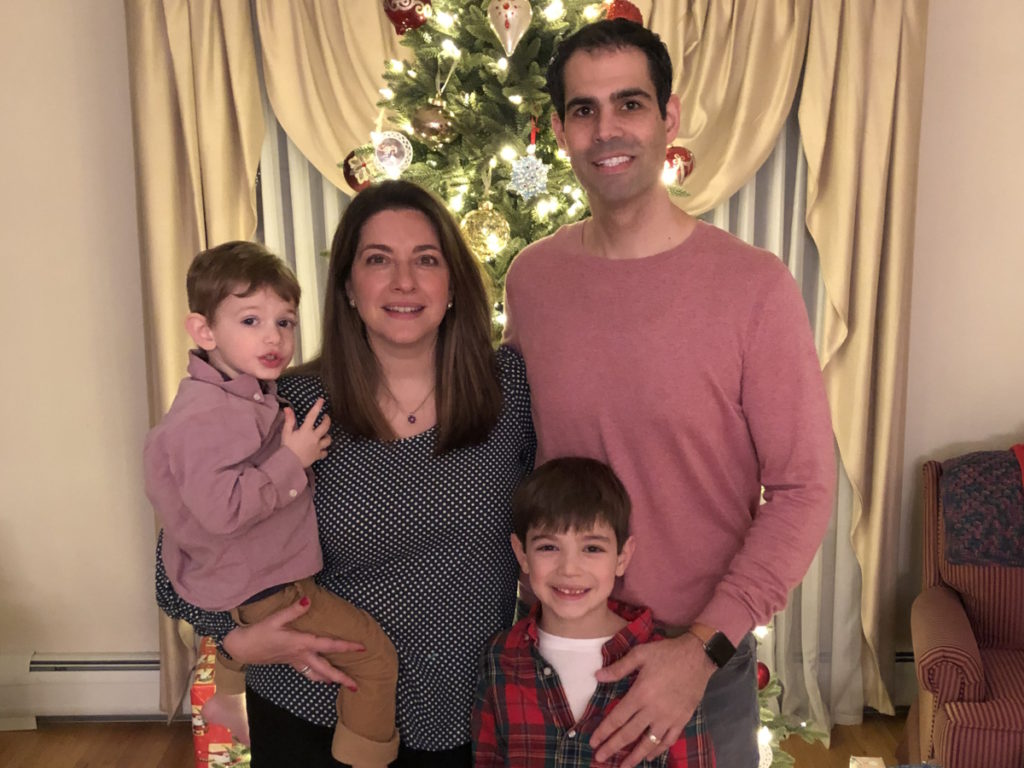
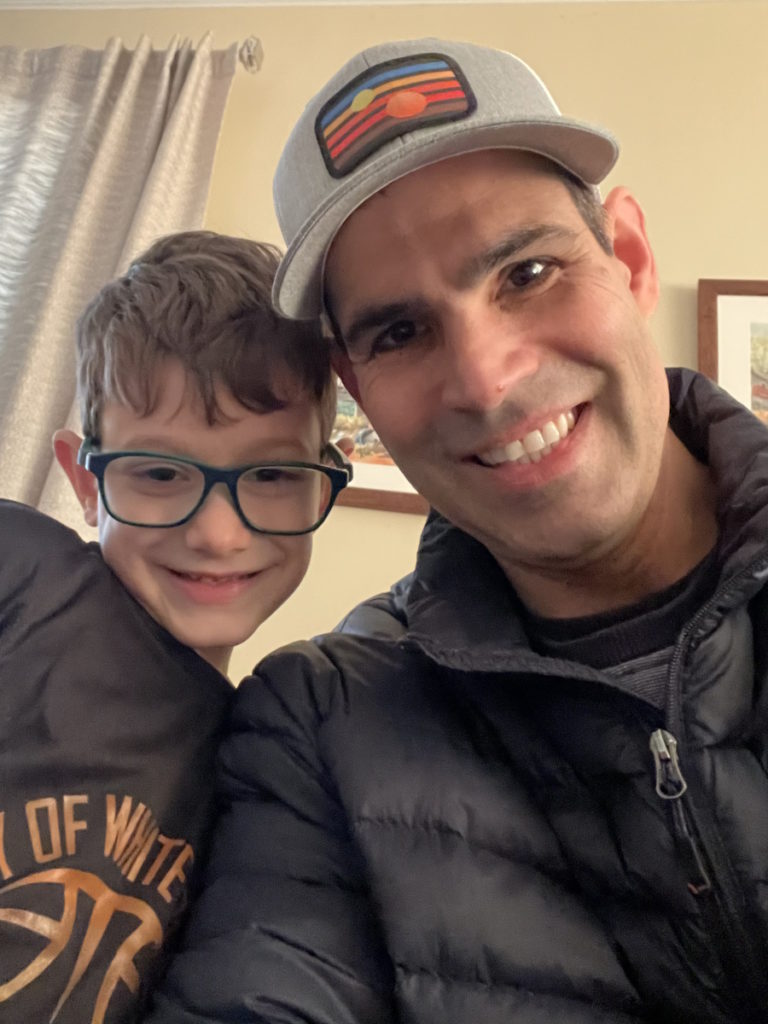
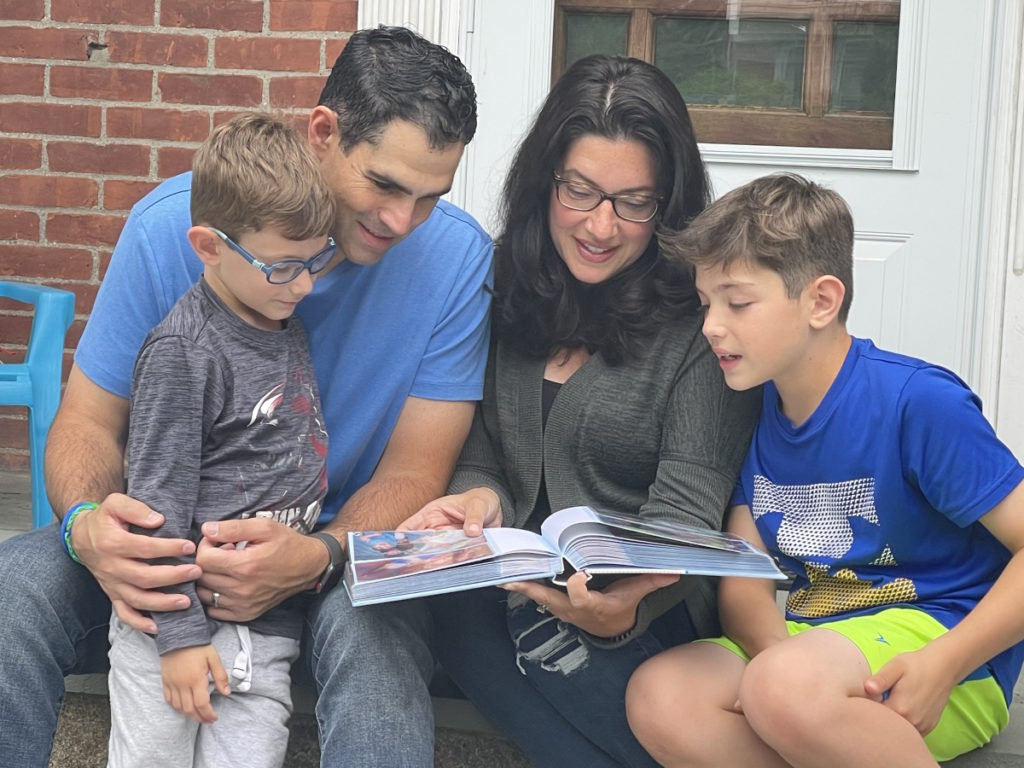
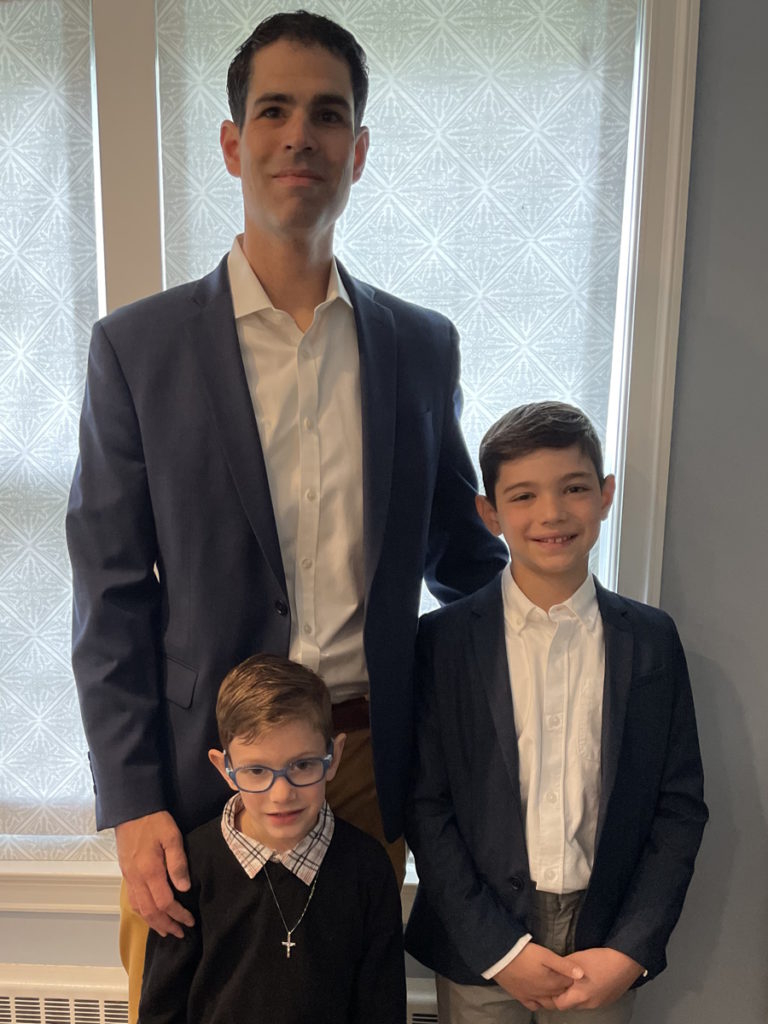
I’m very much a family man. I have two young kids, 9 and 5, [and] married to my beautiful wife, Kara, for 13 years. A lot of [my] life is centered around my family and just being there for them.
I love sports. I was a baseball player and basketball player [throughout] college.
I love to help people. Since my diagnosis, I’ve gotten involved in the cause, telling my story, [and] also hear other people’s stories and share perspectives.


I wanted to get pampered for a day… That’s the only reason why I went in for a physical.

Pre-diagnosis
Why did you go in for a physical?
My work pays for an all-day physical. The only reason I did that was [that] I wanted to get pampered for a day. They do the work up, you’re in a robe, and they have a whole area where you could sit and have snacks.
I kept hearing about that and I say, “You know what? I’m going to take a day off from work. I’m going to go do it.” That’s the only reason why I went in for a physical. Otherwise, I think it was five or six years since the last time I had a physical.
I felt like I wanted to stay ahead of any potential issues that would come up, which I haven’t been doing. Lesson learned big time.
Now, having the benefit of understanding what the disease is and what the symptoms are, I could point to points over the last 10 years and even going back 20 years where I probably felt some symptoms and just ignored them.
What led you to go to a doctor in the first place?
This is really part of the issue with polycythemia vera and MPNs in general. Sometimes the symptoms and what you’re feeling are nondescript [so] you can ignore them. That was very much the case with me.
I wasn’t really feeling too much. I went to a physical, got a full blood workup, and they flagged a few numbers. Even at that point, I didn’t really think I was going to follow up. I was kind of debating it. My wife really pushed me to follow up and that started the ball rolling [for] the diagnosis.
I can’t really point to one thing in particular [that] I was feeling. Now, having the benefit of understanding what the disease is and what the symptoms are, I could point to points over the last 10 years and even going back 20 years where I probably felt some symptoms and just ignored them.
What were some of your polycythemia vera symptoms?
Blurry vision and headaches — [those are] big ones I experienced throughout my life. I remember being at the dinner table, eating Sunday meatballs with my family, and just sort of going blank, thinking that I just needed two minutes. Hopefully, no one asks me a question or engages me in a conversation.
Itching for sure. Fatigue. I’ve learned how to pinpoint what’s just kid fatigue and what’s polycythemia vera fatigue. There’s a big difference in that. I’ve learned that over the years.
It’s the total body [fatigue]. It really prevents you [from being] able to function, which sounds crazy. People say, “I’m tired,” all the time but it is total body fatigue where your body is shutting down and saying, “I can’t go anymore and if you try and push me, I’m going to just get worse.”
»MORE: Myeloproliferative Neoplasms (MPNs) Patient Stories & Specialist Interviews
I kept trying to get the results over the phone. They wouldn’t give it to me. That should have been my first clue that something is wrong.
How did the conversation about your results go?
I didn’t have a primary care physician so lesson learned.
First and foremost, I’ve built a team. But at that particular point, it was a hematologist and oncologist that I had followed up with.
I kept trying to get the results over the phone. They wouldn’t give it to me. That should have been my first clue that something is wrong.
Finally, [on] the third or fourth attempt, they said, “No, you have to come in. We’re not giving you the results over the phone.” But even at that point, I still didn’t think anything was wrong.
The appointment was the same week that I found out that we were pregnant with Jake, my second child. I was totally consumed. The office I was going to was right next to where we would go for our gynecologist checkups. I didn’t even have a thought in my mind that something was wrong.
Was there any urgency in seeing the doctor?
I put it off for a little while but Kara was like, “No, you should get a checkup. We’re getting older and you should really follow through with it.”
They said, “Your hematocrits and your platelets are high.” Again, another aspect of polycythemia vera and MPNs that are nondescript is that hematocrits and platelets can fluctuate. If you’re [at] high altitude, your numbers can rise.
They gave me the option. They said, “You could follow up immediately or follow up in a year.” Kara was like, “What do you have to lose, right? Just follow up and see what the result is.”
I followed up and they flagged the numbers. They brought me in to have a discussion. Then from there, I went to Cornell and had a bone marrow biopsy to confirm it.

The doctor sat me down and said, ‘You don’t have leukemia, but you do have this other type of rare blood cancer.’ As soon as I heard that, I went blank.

Diagnosis
How did the meeting with the hematologist-oncologist go?
I did not have Kara with me. I just didn’t think anything was wrong.
The doctor sat me down and said, “You don’t have leukemia, but you do have this other type of rare blood cancer.” As soon as I heard that, I went blank.
I don’t remember too much. I remember him saying, “You have polycythemia vera and I’d like to do a phlebotomy now.” I didn’t know what phlebotomy was.
In my advocacy work, I’ve really tried to stress the importance of that moment. I call it a moment of truth. It’s not about the doctors and it’s not their fault.
That particular moment can impact a patient’s psyche [in] one way or the other. They’ll go down a rabbit hole or they can become really calm. I went completely the other way where I was just blank. Confused really is the right word to describe it.
What was your reaction to the diagnosis?
Immediately, my mind just went [to] death, to be honest. How long do I have?
Then you start to walk off the ledge a little bit once you become more educated about what you have. For me, it was a whole year before I really understood it.
I didn’t know how I got it. I didn’t know what the long-term prognosis was. It was just a very confusing time.
How did you break the news to your family?
I specifically remember where I parked in the parking lot. I monotonously walked to my car [and] spent about 15 minutes [inside]. All these questions flooded in, questions that I should have asked the doctor. The top one was, “How?”
How did I acquire this? Was it something I ate? Was it alcohol? How long am I going to live? Then you start doing the worst thing that you could possibly do, which is Google.
I called my brother, [who’s] a dentist, and asked, “What is this? You know what this is?” He said, “No, but I’m going to find out.”
I went home and told Kara. I remember she was in the front room playing with Nicholas at the time and we just stared at each other.
It was just a confusing name — polycythemia vera. It’s a confusing moment. That’s the only word that I could really use. I didn’t know how I got it. I didn’t know what the long-term prognosis was. It was just a very confusing time.
What were the next steps for you and Kara?
We wanted a second opinion so we [went] to Cornell. That doctor was really great and really [broke] it down, explaining exactly what it was and how it would evolve.
I don’t know if that put us at ease. Walking into Cornell and seeing people that are just a lot further along than I was or had different types of blood cancer, I had to leave the room. I got really, really emotional.


What was the emotional impact of the diagnosis?
I’m getting emotional thinking back [to] that particular moment. That’s where the sadness kicked in. It went from confusion to sadness.
It brings back all the moments, all the thoughts about my kids and not being there. My wife [was] pregnant at the time [and] looking at her and not being there for her. We’re supposed to be life partners.
I developed anxiety over it. I still get anxiety. It was difficult.
I think it was seeing people at Cornell who were older but also some young individuals that were struggling to walk and needed a lot of support. It was tough to see that because I envisioned myself as that person and my wife having to help me walk.
I like to be active. I coach my kids’ baseball teams. I kind of played out life’s moments and the fact that I was no longer able to do that. It really hit me hard.
It’s not supposed to be that way. You go from angry [to] sad. At that moment, I was angry.
I really struggled with communicating… I felt like I would be looked at like I’m a complainer.
How did you manage your way through the polycythemia vera diagnosis?
I don’t think I managed very well. I internalized everything.
I started to recognize the symptoms more so not only was I dealing with some mental health issues, depression, and anxiety, but also I started to recognize the symptoms.
I really struggled with communicating. How am I supposed to tell Kara I’m tired or I’m itching or I have bone pain or I have blurry vision? I felt like I would be looked at like I’m a complainer.
I internalized everything and it ate at me. It even affected my personality.
It changed me. It’s not supposed to be that way, but life doesn’t always work out perfectly. There [are] so many quotes out there that say, “It’s [not] how you get knocked down, but it’s how you get back up.”
It’s tough to realize that [at] that moment. Some people can, some people take a while. It took a while for me to realize that.
Why did you decide to go to Weill Cornell Medicine for cancer treatment?
The local doctor recommended someone at Cornell. I’ve changed doctors since then. I figured [going there] would be a good first step. It was a very well-known institution so I felt comfortable going there and validating the diagnosis.
The great thing about this particular doctor was [that] he got up on a whiteboard and sketched out where it came from — the bone marrow, the particular body part, the long bones, and the evolution of the stem cell mutation.
He really took the time. We were there for three or four hours [with] him just explaining it. I also had the bone marrow biopsy but a good portion of that was him explaining it and answering our questions. We didn’t feel rushed at all, which was great.
How was your bone marrow biopsy experience?
I thought about the greater good. That sounds odd, right? But the way it was explained to me was there will be a portion that will go to research for your particular cancer.
I dove right in because I wanted to find a cure at that point so I would say it’s almost a necessary thing. Just think about the greater good. The more times they do [bone marrow biopies], the more research they’re able to [do], and then ultimately find a cure. That’s really what we’re driving towards.
Telling someone I didn’t know my story was such a freeing experience that it just made it okay to get it out and tell people really how I was feeling.
How did you deal with all-consuming thoughts?
I would say it took maybe a year plus. I relate it back to being on the Voices of MPN website, signing up for the patient advocacy group the CHAMPNs, and then getting a call from someone I didn’t know about telling my story.
telling my story [to] someone I didn’t know was such a freeing experience. It made it okay to get it out and tell people how I was really feeling.
It was that particular moment, a year in, [when] I shared my story for the first time [with] someone and that was the jumping-off point where I loved how that felt. It was a freeing feeling and I wanted to continue to do that. That’s what led to the documentary that we filmed, which was life-changing.
No one has to film a documentary. No one has to sign up for a CHAMPN. You can just communicate [with] your significant other or family member and that’s it. That’s doing a world of good, just communicating.


PV is so much more than the numbers. If you’re going in there having a conversation with your doctor about just numbers, then that’s the wrong conversation.
Living with polycythemia vera (PV)
What people see vs. what you’re actually feeling
A lot of patients look great, but they get beat down by the symptoms. Every single day, very severe. That has an effect on your mental state and your ability to deal with it. But it doesn’t necessarily come through in the physical appearance.
A lot of times, we get dismissed so that’s why I make it a point to talk about it often [with] my doctor. We talk about how I’m feeling. I don’t know what is relevant and what is not. I’ve learned that but I give him everything.
I’ve had an experience prior to this current doctor where I was dismissed. I was viewed as a complainer. I have an experience now where that’s the complete opposite, where we actually have a dialogue about that.
How does polycythemia vera affect daily life?
I would talk about fatigue and itching. One time, he says, “Well, you have kids, right? And you work?” I’m like, “Yeah, but doctor, this is different. This feels different.” [He] was just writing it down and moving on to the numbers.
PV is so much more than the numbers. If you’re going in there having a conversation with your doctor about just numbers, then that’s the wrong conversation.


You can experience symptoms that are not related to the numbers being elevated or low or high or in between. People deal with the mental aspect of it more than they like to talk about because it is a constant. It could be a very constant, long-term thing that is tough to deal with on a day-in, day-out basis.
You can’t look at someone’s numbers and say, “You’re good. You should go home today.” That’s not the way the conversation should go. There should be a greater conversation about how you are feeling [and] how you are handling this on a day-to-day basis.
I would wake up, saying, “What’s going to happen today?” I would almost feel something every single day. Either a combination of things or one would be very severe and the others would be very low. It’s really difficult to deal with.
I internalized it. I dealt with it from a mental standpoint and it would distract me. It would really distract me.
I was hanging by every day. What’s going to happen today? What’s going to happen tomorrow? Am I going to progress tomorrow? Are my symptoms are going to be bad? Are they going to be low? It was just consuming.
[The doctor] described the fact that it would be a long-term disease and that didn’t put me at ease. That meant I would have to deal with this for the rest of my life potentially.
He talked about the fact that this is a [slowly] progressing disease. I didn’t want to hear that. I hear, “If I have it at a young age, that gives me more time to progress earlier than someone who is diagnosed a little bit later in life.”
He talked about the randomness of the symptoms. They may pop up when your numbers are high, but they may pop up when they’re not. You may get a whole bunch of symptoms. You may get a few symptoms. They may be severe. They may not be.
It was almost like from that point, I was hanging by every day. What’s going to happen today? What’s going to happen tomorrow? Am I going to progress tomorrow? Are my symptoms going to be bad? Are they going to be low? It was just consuming.

What were you nervous about happening?
Progression into myelofibrosis. I actually researched and pulled numbers from the last few physicals I had. Basically, 10 [to] 15 years prior to diagnosis, my numbers were high then.
You start to think, I’ve had this a lot longer than when I was actually diagnosed so I’m further along on the progression trail. One day, I’m going to wake up and I’m going to have myelofibrosis. That’s really what I was worried about.
I’m still worried about it if I’m being honest. I think about that weekly. I used to think about it daily. But now, I’ve trained myself to think about the good things.
Focusing on the here and now
I focus on the present. I focus on my kids, my wife, [and] the good things in life. There are so many good things about life that we should be in the moment and not get too far ahead of ourselves.
There are a lot more options now, front-line options, with PV than there ever were before.
Treatment for polycythemia vera
The exciting thing is that there’s been a lot of advancement in treatment options for polycythemia vera.
When I was diagnosed, it was a wait-and-see approach. Baby aspirin and phlebotomies every so often.
Phlebotomies can be taxing. My iron levels really dropped. I got into the habit of chewing a lot of ice and that’s directly related to iron levels and anemia. I would empty the fridge, literally, and just chew ice all day. It was really a wait-and-see approach.
I remember when I got to the doctor that I have now and we talked about drugs that are on the horizon. We talked about being a patient advocate or being an advocate for yourself in treatment. I would suggest doing research on what’s out there currently but also what’s to come and really having a conversation with your doctor.
We got to talking about a potential drug that is now FDA-approved that could be a more proactive approach to your treatment options. That’s the drug that I’m on now, Besremi. That also is supposed to slow progression, which was something that I was extremely worried about and a lot of PV patients are, too.
There are a lot more options now, front-line options, with PV than there ever were before.

What does it feel like doing something to prevent progression?
It feels like I’m actually doing something to help myself.
At a certain point, when I got comfortable with my diagnosis, I ate differently. I went with a very clean diet. I gave up alcohol because that’s inflammatory. I gave up some inflammatory foods thinking that would help with my symptoms.
At that moment, I said I was going to do everything that I possibly [could] to guard against this thing progressing. That’s what I felt like going on this drug in particular because I felt like I was being proactive about my disease and I was doing everything in my power to prevent it from progressing.
It helps me deal with this mentally, knowing that I’m doing everything I can to help. I didn’t want to leave anything on the table. That’s how I view it.
It feels like I’m actually doing something to help myself.
How is being on Besremi different compared to previous treatment options?
Sometimes I’d go months without a phlebotomy and then all of a sudden, I’d have to go every two weeks again. That’s the frustrating part because you can take that and overreact to it.
I equate polycythemia vera and MPNs to a baseball season and even a basketball season. A basketball season is 82 games. It’s long. You can’t overreact to any one game or one day, one loss or one win. You have to look at it as a whole and really be in it for the long term. It would be every two weeks, every three weeks.
Now, I inject every other week and my symptoms have gone away for the most part. I’m not chewing ice anymore. I feel a lot better. I have a lot more energy. I’m in a good place.

Words of advice
You really need someone who’s removed from the diagnosis [to receive] the information, ask questions, and think with a little more clarity than you.
[For] any doctor’s appointment, just prepare like it’s a business meeting and think through scenarios [and] questions to ask. Try not to get too far ahead.
Don’t go at it alone. I know there are people that struggle with this mentally. Just make sure that you have a support system. There is support out there.
Communicate. If you don’t communicate, it’s going to eat away at you. There are different ways to communicate. There’s written, email, social, [and] person-to-person.
There are a lot of great advocacy groups out there that I joined just to share perspectives. One of the great things about a support group is that you hear different perspectives. People deal with things differently and you gain just knowledge.
There’s support out there. Please, there’s support.
Importance of seeing an MPN specialist
One thing related to this, and what I would leave people with, is that there is a support system out there beyond family and friends. The MPN community is small, but it’s growing and there are people that are willing to help.
Through that community and the people I met, I got to know other doctors. I did my research and settled [on] one doctor in particular [who] really spent the time getting to know me beyond the numbers.
Dr. Heaney, who has recently passed, dedicated his life to helping people. I’m so appreciative [of] having known him for the three years that I did. He’s going to leave a big hole in the MPN community. I love Dr. Heaney. May he rest in peace.
I’m in between doctors right now. I see the difference right away where the current doctor doesn’t understand everything that goes into how we feel, the numbers, understanding of the drugs, and tweaking the drug. Higher doses, lower doses, what the impact might be, the drugs to come, new ways, even holistic ways, to deal with certain symptoms.
That completeness that Dr. Heaney and other MPN experts have is lacking right now. I’m in the process of looking for a new doctor in the same way that I found Dr. Heaney.


Communicating with your partner
I remember having the conversation with Kara and just starting small. I still wasn’t ready to have an in-depth conversation. You will be surprised [by] the positive reaction, support, and love that will come your way and that’s a great feeling.
Please don’t be afraid to share with someone that you care about and love because you’re going to get that right back. I guarantee it.
Don’t go at it alone. I know there are people that struggle with this mentally. Just make sure that you have a support system. There is support out there.
Inspired by Nick's story?
Share your story, too!
MPN Specialist Conversations
Your MPN, Your Journey: How New Discoveries Will Impact Personalized Care
Dr. John Mascarenhas of The Tisch Cancer Institute at Mount Sinai and patient advocate Andrew Schorr share the latest breakthroughs in MPN care.
Srdan Verstovsek, MD, PhD
Role: Director, Clinical Research Center for MPNs at MD Anderson; Section Chief, MPNs; Prof., Dept. of Leukemia
Focus: Myeloproliferative neoplasms (MPN)
Institution: MD Anderson
Myelofibrosis Highlights from ASH 2022
Dr. Serge Verstovsek and Dr. Naveen Pemmaraju discuss cutting-edge treatments and therapies, and combination therapy as a focus in treating myelofibrosis.
Clinical Trials and You: How to Navigate Treatment?
Patient advocate Ruth Fein Revell, experts Dr. Angela Fleischman and Dr. Ruben Mesa, together with clinical trial nurse Melissa Melendez delve into the cutting-edge realm of myelofibrosis clinical trials.


One reply on “Nick Napolitano’s Polycythemia Vera Story”
Hello
I just watched the webinar from July on Managing Symptoms. I would love to connect with Nick Napolitano as his story felt quite similar to mine. Can you put me in touch?