Mary’s Myelofibrosis Story
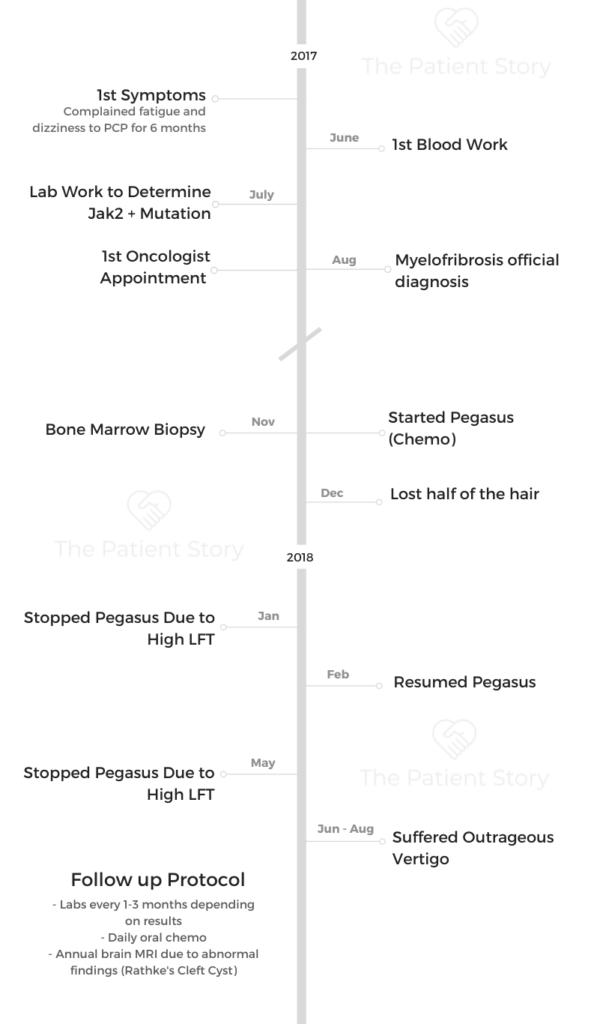
Mary spent several decades of her life as a nurse after getting her Master’s degree. She considered herself to be in full health when she started to feel strange symptoms like fatigue and dizziness. They worsened over time.
She started going to the doctor’s, beginning a multi-month stretch of fighting to get more testing done to figure out what was causing her these symptoms. It took a lot of fighting for herself to finally get to a specialist who confirmed Mary had primary myelofibrosis.
In this video series, Mary shares her story of patient self-advocacy to get the right diagnosis, going through treatment and side effects (Pegasys and hydroxyurea), and how she continues to live life to the fullest with myelofibrosis.
Thank you so much for sharing, Mary!

- Name: Mary L.
- Diagnosis (DX)
- Myelofibrosis (MF)
- Primary MF
- Type of myeloproliferative neoplasms (MPN)
- Myelofibrosis (MF)
- 1st Diagnosis:
- Age at DX: 55 years old
- Symptoms
- Fatigue
- Extreme dizziness (later diagnosed as vertigo)
- Tests for DX:
- Blood lab work to determine any mutations (JAK2+)
- Bone marrow biopsy
- Liver function test
- Treatment:
- Pegasys (Peginterferon alfa-2a)
- Hydroxyurea
- Introduction
- Path to diagnosis
- Patient self-advocacy
- Testing for genetic mutations
- The first cancer diagnosis
- First oncologist appointments
- Getting a second opinion
- A new cancer diagnosis
- Advocating for a third opinion
- First treatment: Pegasys
- MF Treatment VID
- Treatment Decisions
- First treatment: Pegasys
- Switching hospitals and doctors
- Treating the Primary Myelofibrosis (Hydroxyurea)
- Top takeaways on myelofibrosis treatment & side effects
- Living with Rare Cancer Video
- Patient empowerment
- Mental & emotional health
- Making the decision to "live well"
- Dealing with chronic pain
- Protecting your space
This interview has been edited for clarity. This is not medical advice. Please consult with your healthcare provider for treatment decisions.
The Long Path to Diagnosis
Mary spent decades as a nurse and had always considered herself “in good health” when she started feeling symptoms like fatigue and dizziness. Both started to worsen over time, so she went to the doctor’s office.
It would take many months of pushing back and self-advocacy to get more testing for Mary to finally get a diagnosis. Even then, it would turn out to be the wrong one.
Explore Mary’s story of how she would finally get her myelofibrosis diagnosis and her message about patient self-advocacy below.
Introduction
I’m 59, and until this diagnosis four years ago, I thought I was in pretty darn good health. I’m a mom to two adult sons, ages 29 and 31.
I’m a nurse. I’ve been a nurse for 36 almost 37 years now, but I haven’t practiced clinically in about 23 or 24 years because I’m administrative in health care.
I’m now the CEO of a nonprofit that does business as a life plan multilevel retirement community. I’m also an artist and I do a lot to do creative stuff.
I have a little puppy, 15 months old, we walk a lot. We’re outside. I’m newish to San Francisco this past year, so I’m outside, just exploring a lot.
A long time ago, I realized that the fatigue that I get as a side effect of my cancer is not helped by napping. For me, it’s helped by pushing through and and walking.
And that’s really been kind of treatment for me is to be able to keep my energy up by adding to it with walking.

Path to diagnosis
I’d probably had these symptoms for a couple of years, but being a nurse and health care professional, I kind of blew them off and just thought, oh, come on, keep going.
What were the first symptoms?
I’d probably had these symptoms for a couple of years, but being a nurse and being a health care professional, I kind of blew them off and just thought, oh, come on, keep going.
My symptoms were fatigue and a vague kind of dizziness, vertigo-ishness. But having never had vertigo, I just kept calling it dizzy. But it finally got bad enough in early 2017, the fatigue got so overwhelming that I would feel like I needed to take a nap by two o’clock in the afternoon on my floor of my office.
I wanted to just put my head down, shut my door and go out. I thought maybe I had mono or something like that. I thought I had something really simple. I kept feeling for my lymph nodes and things like that. It never occurred to me that I would have a major diagnosis. I thought I just was stressed or overworked when I went.
Dizziness vs. vertigo
So early on, I didn’t really appreciate what the difference was. I just knew that I felt lightheaded. I felt like sometimes the room was spinning, and on rare occasion it felt like the hand of gravity was coming out of the sky and just knocking me over.
That’s when I started realizing it was vertigo. So we’re used to dizziness. That’s when we feel off balance and our head spins when the room spins around you. That’s vertigo.
When the room is spinning, that’s vertigo in or when something external, I call it the hand of gravity. It felt like something external was pushing me, and I had no choice but to fall over. That’s what I was experiencing.
Patient self-advocacy
I said to my doctor, I’m not leaving until you draw blood. I didn’t know what that blood was going to tell, but I just really felt like we needed to do something.
Doctors’ responses to your concerns
In fact, my doctors didn’t really jump to cancer. It took me months of pushing that this was bigger than, you know, it wasn’t mono. They didn’t want to do much more. They kept saying, oh, you have a big job, you’re stressed or you have a lot. You do a lot, rest more.
At first, they looked at sleep apnea. It was like not sleeping well, and that’s why I was fatigued during the day. I didn’t have sleep apnea.
Advocating for tests
It wasn’t until finally June of 2017 I just put my foot down. I said to my doctor, I’m not leaving until you draw blood. I didn’t know what that blood was going to tell, but I just really felt like we needed to do something.
And that’s exactly what we did. We drew blood, and about three days later, I got a phone call and I could already see on my app that my platelets were high. I think they were about 800,000. So I was concerned and of course, Googling to see what my platelets meant.
I asked my doctor for some information over the phone when he called me to explain my platelets were high. He said, ‘Well, we’re sending your lab work off for some special testing.’ And I said, what kind of special testing
I will also point out, in fairness to the doctor, I’m a nurse and I think doctors sometimes think we know enough to be problematic, like we’re a little hypochondriacal. So they might have thought, you know, she’s exaggerating or something. So fair enough.
Testing for genetic mutations
Testing timeline
End of June, the labs were drawn and my platelets are high, I think in the 800000’s. And of course, I’m worried about it.
My doctor says to me, we’re sending the labs off for more testing, and I said, what more testing? He said special tests. And I said, can you tell me what and he said, I don’t want to worry you. We’re just sending it off for testing. I’ll get back to you as soon as we have more.
Well, it turned out that that special testing was they were sending those vials of blood off for genetic testing to a lab in Florida to see if I had any genetic mutations. That would would further be the differential diagnosis in my treatment and defined my treatment.
How long did it take to get results?
I waited all summer. That initial lab draw was, I want to say, June 20th or something. I would call my doctor periodically and say, Hey, do we know anything yet? And he said, no. As soon as you know something, you’ll get a call.
And I did get a call. I called him again on something like August 27th. It was a Thursday, I recall, and I said, Can we talk about this? And he said, No, you’ll get a call from a nurse admitting you to services shortly.
I got off the call with him and the nurse called me and she said, ‘Hi, this is Suzy from Hematology Oncology admitting you to services.’ And I was stunned that I was being admitted to an oncology service without anybody telling me I had any oncological disorder. That was late June with the lab’s, late August was when I was getting results.
The first cancer diagnosis
How did you learn the diagnosis?
The very same day that the nurse called me to admit me to oncology services, I called my doctor and clearly I think he really felt like this is bigger than me. I don’t even know how to talk about it, so I’m going to let those oncology people talk to you about it.
So he kind of blew me off, and literally seconds after I hung up with him, the phone rang and it was this nurse saying she’s admitting me to hematology oncology. And that was a Thursday, and I think I had the appointment the following Tuesday. My husband and I went in to meet with the oncologist.
Going down the Google rabbit hole
Well, you know, the hard thing about it is it’s excruciating because you just want answers, but you have this thing called Google, which can and cannot be your friend.
And I have a nursing background and I was a nurse at Johns Hopkins, Mass General. So I’m picking up the phone calling everyone I know. And of course, everybody’s telling me, look at this, do this. And so I had a whole lot of ideas of what it might be by the time I got to the office on Tuesday.
First oncologist appointments
I just looked at her and I said, I need to fire you. I need to get a second opinion because this isn’t how I need to be talked to.
The first oncologist meeting
This was a really interesting place. So we’re sitting in hematology oncology waiting room, and that’s unnerving itself because all of a sudden you see yourself labeled very differently. I get called in. My husband comes with me.
A female physician oncologist comes into the room. The first thing she said is, ‘I don’t want you to be afraid.’ And I said, ‘Should I be afraid?’ And she said, ‘Well, most people are afraid because they see the C-word written all over our department.’.
And I said, OK, it is the C-word, though, are we not talking about it? And she said, ‘Well, I don’t like to call what you have the C-word because it scares you too much. And the C-word just triggers things for people. So I don’t call it the C-word, we’re just going to call it ET,’ which is essential thrombocytopenia. And I said, Oh, OK, but isn’t it cancer?
‘Oh, I don’t like to say the C-word.’ That was kind of how she presented it. I’m thinking, this is crazy. So I looked at my husband and I said, can we stop for a second?
I said, listen, I’m 55 years old, I’m a nurse. I have a master’s degree in nursing, not just a bachelor’s. You know, you can talk to me, we can talk about it as cancer. We can we can talk about this. I Googled, I’ve read.
She said, no, I don’t like to talk about it that way. And the other word we don’t use is the treatment is also a C-word and it’s an evil, evil drug. So I don’t like to call that what it is either. And I just looked at her and I said, I need to fire you. I need to get a second opinion because this isn’t how I need to be talked to.
I wasn’t terrified of dying as much as I was terrified of not having the right information so I could live.
Importance of patient-doctor partnership
It felt so odd to be treated like with these kid gloves because I felt like I’m ready for this. What this oncologist didn’t know is my dad had a rare blood cancer and died in 1989. I know a little bit about this and what she didn’t also appreciate was that I’m pretty realistic.
I wasn’t terrified of dying as much as I was terrified of not having the right information so I could live. It felt so childish to call it the C-word and an evil, evil drug.
And when I asked her to not do that, and she continued, I just felt like this isn’t a good fit and this isn’t how I want to start this journey, right?
I felt really diminished by her in that in that respect. And I wanted to start out strong. I wanted to have a partnership with this oncologist because I felt like I was going into a fight here for my life and I wanted to really trust somebody.
Getting a second opinion
The resources that were helpful
Then what’s in the back of my head in this by now? By the time I got to that appointment, I had already found the MPN Research Foundation, for instance, online because I knew with platelets in the 800,000’s, I likely had essential thrombocythemia or ET.
I didn’t think I had myelofibrosis yet. At that point I was just thinking of it. And so I found the MPN Research Foundation and found out that the the insurance provider I was under, which is large in California, it’s an HMO in California. They had no MPN specialists period. The end. Zero listed through the research foundation.
So I knew that I was going to be getting kind of garden variety hematology oncologists. I go to this first appointment feeling like I kind of knew a little bit more than my doctor did. That was unnerving.
I said, please don’t don’t label me as like an asshole patient because I asked for a second opinion.
Meeting a new oncologist
So a couple of days later, I was brought in to her male colleague. My husband was with me and he said, ‘Why do you think you need to see me?’ And I said, oh wait a second, we’re not going to start off on this foot.
I said, please don’t don’t label me as like an asshole patient because I asked for a second opinion. Please, please. And I explained to him that she told me about the C-word and evil drug and all that. She also told me, ‘Don’t think of it as a cancer. Think of it like you’re a farmer who planted two crops of corn, but four crops grew.’
That was kind of what made me go, OK, we’re done. And when I told the second doctor that he said, wow, that was a bad experience, and he became much more human and listened to me and he was wonderful.
A new cancer diagnosis
He immediately said, I don’t think you have ET. Your platelets are high, but your red blood cells are high. And I said, no, they’re not. My red cells are still normal. My hemoglobin is normal. And he said, I think you have PV, polycythemia vera.
I said, I’m not understanding this. Why? And he said, well, your red blood cells and your hemoglobin are pushing to high. They’re high-normal.
Number one, trust your gut. If you if you think you have pain or vertigo or for fatigue, don’t let anyone talk you out of it because you’re right. You know yourself.
Introduction to Pegasys treatment
Right away he said, I think you’d you’d really do well on Pegasys, which is a pegylated interferon. This was the first anybody had talked to me about starting a treatment. The last gal had said you’re early in this, you’re not going to start treatment anytime soon.
And the second doctor really was pushing for me to get on pegylated interferon, which was a bit unnerving because I didn’t think I had PV, I thought I had ET, so then that started.
Guidance on the process of getting diagnosed
Number one, trust your gut. If you if you think you have pain or vertigo or for fatigue, don’t let anyone talk you out of it because you’re right. You know yourself.
Number two, find a physician that you can connect to who will listen to you and who values your input in the treatment plan. Connect yourself to a research foundation or a group that can find you experts or local support groups. Find those groups. There are Facebook groups. There are different hospitals that have groups, but find those groups, there’s patients.
There’s all kinds of stuff online to connect to and and connect to people who have gone the path before you because you need their advocacy as well. You need to learn from what they have gone through and above all, get to a center that has a specialist, an MPN specialist on their staff period.
Advocating for a third opinion
When doctor’s decisions still don’t add up
Before I started on Pegasys, I said to this doctor, gosh, everything I’ve read and everything that your colleague told me was that I shouldn’t be on treatment. Now you’re telling me to go on treatment. But what the MPN Research Foundation says is, before you start any chemo, we need to do a bone marrow biopsy because chemo should be titrated to the bone marrow cellularity, not the blood cellularity.
And he looked at me like I had a hole in my head and he said, ‘You’re not getting a bone marrow biopsy,’ like I wanted one. Who wants to have their hip drilled? It’s not exactly what you want. I said, oh no, no, you’re misunderstanding. I don’t want one. I feel like I need one.
And he said no. He said that’s if we needed a differential diagnosis. You’re JAK2 positive, you have the JAK2 mutation. That is the differential diagnosis. We know what you have. So I said, OK. So he wanted to start me on Pegasys and I said to him, your colleague just told me I didn’t need anything, probably for several years, that we were going to watch my bloods quarterly. And why Pegasys? He said. because Pegasys will turn down the volume on the platelet overproduction and it’ll buy you more time.
Pegasys is the drug. I said do you get a kickback for selling this Pegasys to me? And he kind of joked and I said, okay, let me just ask you this if I was your daughter, would you put your daughter on Pegasys right now with the platelet load I have? Because what I was reading was I should be over a million before I started on anything or a million point two platelets.
And he said, if you were my daughter, I would have you on it today. So we went home and thought about it and I said, yes, I’ll go on Pegasys.
First treatment: Pegasys
Describe the start of Pegasys
I started on Pegasys, what seemed to be quite a high dose, and I questioned that, that usually people start low and titrate up. He said, no, this is the dose. This is how it comes in a vial of this size. I said well we can squirt out, you know, you can give yourself half of the dose. He wanted me to be on that dose. So I started on it.
Reaction to Pegasys
I was on it maybe two or three months and my liver function tests (LFTs) got very elevated. I felt just lousy and and I don’t remember other than my hair fell out. A lot of my hair fell out.
I never lost all of my hair. In fact, this is still only about half of my hair. I had very kinky curly hair, and now I just have kind of some messy waves. Now I have about half the volume of hair. I have much less curl, more wave.
So my hair started falling out pretty significantly and I had some good spots of missing hair. I felt just so fatigued. And it turned out these LFTs were elevated. So they stopped the Pegasys and almost immediately felt better.
And that’s when I said, I’m stopping. I’m done. I’m not going to take any more chemo until I understand more what’s going on.
Restarting treatment
A month or two go by and he says, ‘Let’s get you back on.’ My platelets start climbing back up. So we put me back on and I said I’d like to start at a lower dose. And he said, no, this is the dose you’re starting at.
So I went back on the dose I was, and sure enough, went into the same, same sequelae and ended up with elevated LFTs. That was May of 2018. And that’s when I said, I’m stopping. I’m done. I’m not going to take any more chemo until I understand more what’s going on. I asked him for a bone marrow biopsy and he said no.
So I called him because he wanted me to go back on Pegasys, and I said it says I have this, says I have fibrosis. And he said, no, it says you have PV. I’m the doctor. And I said, OK, you and I are done. I’m not coming back. This was November of 18. And in January, I changed health providers. I changed insurance providers so I could go
And so I ended up in January, starting with Anthem Blue Cross Blue Shield I could go to Stanford, where there was an MPN specialist. So that’s the next kind of phase of this.
Myelofibrosis Treatment
MF Treatment VID
After months and months of medical appointments, Mary was finally diagnosed with primary myelofibrosis.
Explore below to read and watch Mary’s recount her first treatment of Pegasys and second (and current) treatment of hydroxyurea, along with side effects. She also discusses how hard it was for her to take her own first symptoms seriously and how she learned to advocate for herself.
Treatment Decisions
When doctor’s decisions still don’t add up
Before I started on Pegasys, I said to this doctor, gosh, everything I’ve read and everything that your colleague told me was that I shouldn’t be on treatment. Now you’re telling me to go on treatment.
But what the MPN Research Foundation says is, before you start any chemo, we need to do a bone marrow biopsy because chemo should be titrated to the bone marrow cellularity, not the blood cellularity.
And he looked at me like I had a hole in my head and he said, ‘You’re not getting a bone marrow biopsy,’ like I wanted one. Who wants to have their hip drilled? It’s not exactly what you want. I said, oh no, no, you’re misunderstanding. I don’t want one. I feel like I need one.
And he said no. He said that’s if we needed a differential diagnosis. You’re JAK2 positive, you have the JAK2 mutation. That is the differential diagnosis. We know what you have. I said okay.
So he wanted to start me on Pegasys and I said to him, your colleague just told me I didn’t need anything, probably for several years, that we were going to watch my bloods quarterly. And why Pegasys? He said because Pegasys will turn down the volume on the platelet overproduction and it’ll buy you more time.
And he said, if you were my daughter, I would have you on it today.
Mary L.
“Is this what you’d give your own family?”
I said, okay, let me just ask you this if I was your daughter, would you put your daughter on Pegasys right now with the platelet load I have? Because what I was reading was I should be over a million before I started on anything or a million point two platelets.
And he said, if you were my daughter, I would have you on it today. So we went home and thought about it and I said, yes, I’ll go on Pegasys.
First treatment: Pegasys
Describe the start of Pegasys
I started on Pegasys, what seemed to be quite a high dose, and I questioned that, that usually people start low and titrate up. He said, no, this is the dose. This is how it comes, in a vial of this size.
I said well we can squirt out, you know, you can give yourself half of the dose. He wanted me to be on that dose. So I started on it.
Reaction to Pegasys
I was on it maybe two or three months and my liver function tests (LFTs) got very elevated. I felt just lousy and and I don’t remember other than my hair fell out. A lot of my hair fell out.
I never lost all of my hair. In fact, this is still only about half of my hair. I had very kinky curly hair, and now I just have kind of some messy waves. Now I have about half the volume of hair. I have much less curl, more wave.
So my hair started falling out pretty significantly and I had some good spots of missing hair. I felt just so fatigued. And it turned out these LFTs were elevated. So they stopped the Pegasys and almost immediately felt better.
And that’s when I said, I’m stopping. I’m done. I’m not going to take any more chemo until I understand more what’s going on.
Restarting treatment
A month or two go by and he says, ‘Let’s get you back on.’ My platelets start climbing back up. So we put me back on and I said I’d like to start at a lower dose. And he said, no, this is the dose you’re starting at.
So I went back on the dose I was, and sure enough, went into the same, same sequelae and ended up with elevated LFTs. That was May of 2018. And that’s when I said, I’m stopping. I’m done. I’m not going to take any more chemo until I understand more what’s going on. I asked him for a bone marrow biopsy and he said no.
I called him because he wanted me to go back on Pegasys, and I said it says I have fibrosis. And he said, no, it says you have PV (polycythemia vera). I’m the doctor.
I said, OK, you and I are done. I’m not coming back. This was November of 18. And in January, I changed health providers. I changed insurance providers.
I ended up in January, starting with Anthem Blue Cross Blue Shield. Then I could go to Stanford, where there was an MPN specialist. So that’s the next phase of this.
I told the doctor that this was happening, they felt like they couldn’t reproduce it and that it was here in my head.
When doctors think it’s “in your head”
I think I put off going to the doctor at the beginning because I thought it was in my head or I thought, what is this? Do I have a cold or flu or something? But when it got to the point where the vertigo was overwhelming my life, I feel like I had no choice. I was starting to get injured, frequently injured.
I can remember one time this vertigo, this gravity comes down and it just sort of pushed me down I fell against the wall and I ended up being wedged between my sofa and an end table. And I didn’t know how to get myself up because I was in so much pain.
I didn’t know how to move. The world was spinning around me and I knew I needed help. But every time I told the doctor that this was happening, they felt like they couldn’t reproduce it and that it was here in my head.
Switching hospitals and doctors
New insurance opened up treatment center options
In January of 2019, I started with Anthem Blue Cross, which let me go to Stanford, but you still can’t get into Stanford unless you get a referral.
It took me a full year at the new insurance provider to get a referral to “The Wizard.” I call it seeing the wizard.
Another bone marrow biopsy to determine diagnosis
In January of 2019, the doctor said, we’re going to give you another bone marrow biopsy because this one looks like fibrosis and we’re going to do another one.
They drew new cells out of my hip and they called it “pre-fibrosis.” They said you have essential thrombocythemia (ET), which is elevated platelets with pre-fibrotic cells.
Ok, so finally, through the whole of 2019, I’m just coasting along and the vertigo is getting worse and nobody really wants to treat the vertigo. I think nobody really understood the vertigo as a symptom of the cancer. It’s very unusual.
I was relieved. Relieved to have the worst diagnosis, but because at least I knew somebody was looking at things from the right perspective, somebody with the right eyes was looking at that.
Changing treatment centers → right diagnosis
I finally said, can I go to Stanford? And I think in exasperation, they said yes. So I got in to see Stanford in January of 2020, and Stanford took both sets of bone marrow cells that had the slides from both sets of those slides that had been drawn before out of my hip and they re-evaluated them.
Stanford in January of 2020 said, you never had ET, you never had PV. You had primary myelofibrosis, based on those cells from from 2018 and 2019.
I was relieved. Relieved to have the worst diagnosis, but because at least I knew somebody was looking at things from the right perspective, somebody with the right eyes was looking at that.
He knew that I had not been treated well and he just took the time to make sure that all my care got pulled together in that one visit with him. It was stellar.
Feeling confident in the new treatment team
The real key thing at Stanford was when you walk through the doors at Stanford you’re at a different kind of place. Your shoulders go back, your head goes up, the air you breathe is fuller and people tend to you.
I was immediately signing into research studies and giving extra vials of blood, and I felt like I was part of something much bigger than myself.
When I finally got in, I was interviewed first by a nurse practitioner for almost 45 minutes and then I had the wizard himself, Dr. Jason Gotlib, an MPN specialist who’s just amazing. He was supposed to spend 15 minutes with me – he spent almost 45 with me, just answering all my questions, drawing out diagrams, putting things up on the computer.
He knew that I had not been treated well and he just took the time to make sure that all my care got pulled together in that one visit with him. It was stellar.
I felt for the first time, in two-and-a-half years of diagnosis, validated because he said to me, yeah, the vertigo is kind of unusual, but I’m going to send you to one of our ENTs. I said, I’ve been. He said, you haven’t been to an ENT who understands your blood cancer.
I said okay. I walked in and when I saw the ENT, he said I see 30 of you a week They put earphones and goggles on me, and they could figure out what was wrong with me in seconds.
The impact of having a doctor who listens to you
The biggest thing was I felt heard. I felt seen. Even if my symptoms were obscure, they were going to leave no stone unturned in trying to help me understand it.
At the beginning, I don’t think anyone really understood the vertigo until my platelets got really high and then we started treatment. My platelets became under 600,000 and boom, my vertigo went away. Now we understand it in the context of my platelets.
It felt like I knew I was in front of greatness and I have so much admiration and appreciation for Dr. Gotlib and his colleagues at Stanford.
Treating the Primary Myelofibrosis (Hydroxyurea)
COVID treatment delay
I only saw Dr. Gotlib in January of 2020, and then, of course, COVID hit, and all of my ENT stuff got pushed off till almost July. So the vertigo continued.
It was just because of COVID and the newness of it without a vaccine, without really understanding transmission, everything shut down. And those are things I couldn’t do over a video call.
Managing the MF symptoms (vertigo)
It wasn’t until July of 2020 that I saw the ENT and they put me into physical therapy for some neck manipulation and some work around that.
August of 2020, I had an event of some kind. I got up in the morning. It was always hard to get out of bed because the vertigo would make me often fall back in the bed. As soon as I stood up, I feel like the world was spinning.
That particular morning. I sat at the side of the bed and I felt like gravity was just pushing me. I mean, just throttling me back in the bed such that I tried to get up three or four times and ended up projectile vomiting. When I would look at the wall, my eyes would bob from 12 o’clock to six o’clock, they would just bob back and forth, up and down.
For the first time in years, I had none.
I intuitively knew that I had nystagmus, which is related to inner ear stuff and I thought the vertigo. I ended up doing my best to clean up my mess, but by crawling because I couldn’t walk. I went back to bed, I called out sick to work, and I ended up staying in bed for two days at that point.
As quickly as it came on, it seemed to have resolved, except that I did get my local oncologist to to draw blood because she was interested in understanding all that nystagmus and everything, and my platelets were over a million.
Treatment for the vertigo: hydroxyurea
She immediately put me on hydroxyurea to treat that. And here’s the gift. Within two weeks of being on hydroxyurea, my platelets came down under 600,000 and we were watching those platelets almost daily the first couple of weeks.
Then almost like magic, the day they went under 600,000, I had no vertigo. For the first time in years, I had none.
How long have you been on hydroxyurea?
Since August of 2020.
When and how often do you take the hydroxyurea?
It’s a pill. I take it at night, at bedtime.
What are the hydroxyurea side effects
Summary: nausea, dry skin
When I was taking it in the morning, the side effects were some nausea. The doctor said take it at night and I don’t notice anything.
My skin at the beginning got really weirdly dry, almost like a snake in that I had a layer of dry skin above my skin that I could kind of peel off. It really concerned my oncologist because apparently, especially on the legs with hydroxyurea, we’re prone to ankle injury, ankle skin breakdown from the hydroxy.
So she wanted me to start on some lotion on my legs twice a day with hyaluronic acid in it, which really calmed down the itching. And I have beautiful skin now. I don’t have any of that dryness or itching. That was the biggest thing, the weird skin for me.
I occasionally have a thing where when I get in the shower, the hot water makes my skin burn, itch. I don’t know how to describe it other than it’s a burning itching almost like it burns and itches so much that taking cold showers is kind of a gift, like you don’t even mind the cold shower. But I don’t get that very often. I’m pretty lucky. I’m pretty darn lucky with my symptom load.
What is the stage of your myelofibrosis
I’m considered stage one and it’s three stages, so very early stage. I could continue on like this for a really long time now. Right now, my platelets are running like 485,000, so almost normal platelets.
I get so excited. I only go every four months now for a blood draw because they’ve been pretty stable.
Monitoring the myelofibrosis closely
My oncologist always says to me it could turn in a minute. It could. It could go out of control in a minute. Either they can dive down because the scarring in the bone marrow could get to such a place where I can’t make cells anymore.
But I don’t have any splenomegaly, enlarged spleen, I don’t have any of that. I’m lucky.
Top takeaways on myelofibrosis treatment & side effects
Listen to your body
The biggest thing is a doctor you trust and who will answer your questions and take your weird symptoms seriously because I’ve got to tell you, I go to my primary care physician for things, and she says, that sounds like that’s your cancer. Go to your oncologist. And then my oncologist says, go to your primary for this. So there’s that kind of thing, and it just happened to me recently.
I think I may be developing gout in my right foot and an ankle, which is unusual place to have gout. But every now and then I get a flare up of my ankle really red, and it feels like there’s glass in the joint can barely stand a walk. Ice and elevation don’t do anything for it. It’s not injury related. It doesn’t appear to be. It might be three or four days of just pain. Then it goes away. It sounds like gout, which can be a side effect of platelet overproduction.
I called my oncologist and said, Hey, let’s just add uric acid to my next lab. And she said, go to your PCP. And I said, my PCP is going to send me to you. Can I just add this to my next lab?
There’s a lot of that kind of stuff. I guess the biggest thing is more pay attention to your body.
Dealing with fatigue
Fatigue is real. But there are ways to help the fatigue early on when the vertigo was bad. I managed the fatigue with a one on one pilates instructor. I had a pilates instructor who was very tuned into the fact that I had vertigo and gave me workouts that pushed me enough without pushing me over my limit and keeping my body in shape really helped.
If I stayed hydrated, if I drink plenty of water, and I always have a big glass of water next to me, and I eat kind of a Mediterranean diet, a clean, lean diet, I feel so much better than right now when there’s cookies and candies. It’s harder on the body, you know? And given that you already have something else going on, the cleaner diet really helps.
Taking care of sleep
The other big thing for me has been sleep and sleep hygiene. You know, being willing to turn off the phone and the computers at night and read a book or listen to a meditation tape or something like that, but have routine around sleep so that sleep is prioritized. Those things I think are keeping me as well as I can be.
Life with Cancer
Living with Rare Cancer Video
After discussing the difficult path to getting her primary myelofibrosis diagnosis through finally getting to the right MF specialist and treatment, Mary L. delves into the day to day of living with myelofibrosis.
She shares everything from living with myelofibrosis, the uncertainty of a rare cancer diagnosis, the need for self-advocacy as patients in your own care, and tending to both physical and mental health.
Patient empowerment
The importance of patient self-advocacy
Listen to your gut. Listen to yourself, you know your body better than anybody. Be persistent if you’re not listened to.
The importance of having an MPN (myeloproliferative neoplasm) specialist
Find an MPN specialist. I know people who travel five hours to a specialist. It’s that important.
It’s a great life. It might not be as long as I had hoped it would be, but I’m going to ensure that it continues to be a great life, even if it’s a shortened life.
Mental & emotional health
How is it dealing with the uncertainty of living with myelofibrosis?
First of all, being a nurse and also seeing my father have very similar cancer at an early age, we both were diagnosed with blood cancers at age 55, and he died at age 60, I’m pretty pragmatic.
I sat my children down early on, my adult sons, and they didn’t want to talk about it. They didn’t want to talk about the fact that I was going to die. I presented them with my will and my DNR (do not resuscitate), the kinds of things I wanted them to understand about my end of life.
They were having a really hard time with it, and I had to say to them, and it really helped me to do this. I had to put it in perspective. It’s a great life. It might not be as long as I had hoped it would be, but I’m going to ensure that it continues to be a great life, even if it’s a shortened life.
That really helped me a lot. Instead of framing it as ‘Why me? Why did this happen?’ Frame it as, ‘This did happen. My days are numbered to some degree. And use your time well, lady.’
That’s kind of the story, the narrative I have told myself. And that’s easier said than done.
But in the aftermath of that, that grief was so heavy. That grief was harder than the grief of getting cancer.
Dealing with people’s reaction to your cancer
I had to do some practical things early on. After my diagnosis, my husband left me. He decided that he didn’t want to stick around for the end. When it was turned out that this was myelofibrosis, he was like, you’re dead. You going to be out of here, and I don’t want to be around for that. We had only been married six years. It was a second marriage.
But I have to tell you, it was a great marriage. It was bliss. So it came out of the blue. It wasn’t at all something I saw coming. And he’s not a jerk. He panicked and and he left. We are still friends, if you can believe that, Anyway, that’s another story.
But in the aftermath of that, that grief was so heavy. That grief was harder than the grief of getting cancer. That grief was so heavy that I started some therapy and that therapy helped me process my diagnosis and my prognosis. You know, this notion that I’m not going to live forever.
Gratitude journaling
One of the things I did that year was I started, and it sounds so trite, I started a gratitude journal. I would get up every morning after I walked my dog, I would have a cup of coffee, and I would sit and write down what I anticipate were going to be great things about today, and what I was grateful for that happened in the 24 hours prior.
That flipping of the switch from, oh man, this is happening to me to hey, how do I make this a great day? What were the great things yesterday and how do I look forward to making this day great? Flipped something in the brain, it really does.
Making the decision to “live well”
I made a conscious choice to live well. That’s easy to say, because I feel pretty good right now. I don’t know if I’m still going to keep this up, but I’m practicing, right? I’m practicing a wellness and a wholeness and taking up space and gratitude because it’s who I want to be. When I am dead, I want my kids to be able to say, ‘She was still pretty cool.’
In spite of all of that, I don’t want my life to be marked by its end. And I also don’t want to give in to the ending by being a jerk through the last 10 years of my life.
When I was at Stanford, they told me I’d be dead by age 72. I don’t love knowing that, but I’m 59 – I have one full decade left, my 60s, and I intend to live it. I intend to. That’s why I took a new job as CEO of a company in March of this year. I didn’t slow down. I intend to continue to live and grow and contribute.
She said to me, ‘But you look fine.’ I said just because I carry it well, doesn’t mean it’s not heavy.
When people in your life “don’t get it”
The truth is, you don’t recover. You just choose to forgive. And I will say this for anybody who’s going through stuff because people are jerks. I had one friend who’d say, you always try to get out of stuff when we’re doing stuff. I said, you always plan things late in the evening. And I have told you that evenings are not my time. If you want me for dinner, 4:30 or 5 o’clock. I can’t do an 8 o’clock dinner because that’s bedtime.
But she was ragging on me. Ultimately, that friendship sort of went. She said to me, ‘But you look fine.’ I said just because I carry it well, doesn’t mean it’s not heavy.
The astonishing thing is, some people just want you to look sick and if you don’t look sick, they just want you to carry on. So I didn’t really lose friends, but I let go of things that didn’t feed me ultimately.
And my husband who left me and I are close, close friends. He has deep regret for what he’s done and he’s trying to get back with me. But I don’t know that I could at this stage of the game. But I don’t hate him. I feel sorry for him because he gave up something really amazing.
I look at it as my energies have to be put into [different things]. I have to stay whole and healthy and strong mentally and physically because I am a mother, I am a CEO, I am a nurse, and I’m a friend and I have roles that I’d like to continue to contribute to.
A focused mindset living with myelofibrosis
I have to, number one, take care of my mental and physical health to the extent that I’m able. Attitude is a lot of it. I do not feed myself negativity. I don’t and I will not pity myself because this is happening to me.
I remember when my father was sick, I said, Pop, do you ever ask ‘why me?’ And my dad never got really mad. But he said, ‘Mary, why not me?’ He said, ‘I’ll ask why me when it’s a six year old with brain cancer that’s incurable. That’s when you ask, why them.
Why me? Come on. I had a good life. I’ve seen my kids grow up. I have had a successful career. And so he really helped me with some of that. He was quite stoic. But then when he was dying and I was his caretaker at the end of his life. When he was dying, he died well.
And by well, I mean, he didn’t whine about dying. He took it all in. He died really purposefully and and he was pleasant to all of us around him. I think he taught me how to do that well. So in some ways, I’m grateful for that. You know, there were lessons there, and now I’m trying to teach my kids how to how to be graceful in the face of adversity.
My son and his girlfriend bought me a plaque from Frida Kahlo. It says something like we can endure much more than we think we can or something like that. I said, ‘What made you think of this?’ They said, ‘Because you’re tough, you are so tough.’ I said, I’m not tough at all. I’m not tough. But I want to be whole in the rest of the time I have. I don’t want to whine.
You know, it’s not easy. There are some days. Last night I was sitting watching a Hallmark movie because it was supposed to be smarmy and easy and make me smile, and I was sobbing, tears running down my face last night. I have no idea why something hit me hard. And it wasn’t a happy tears, it was kind of like “wah” tears. It happens.

Dealing with chronic pain
The one thing I learned is that chronic anything, when you think about when you’re sick with the flu, when you’re in bed for two weeks and or even a cold at the end of the two weeks, you are so sick of sneezing and rubbing your nose and your nose is raw.
Now picture that it’s bone pain that because your platelets are scarring your bone marrow and overproducing in your bone marrow, your bones feel like they’re expanding from the inside out and and your bones hurt all the time.
Do I feel like I’m going to die? Nah. But on a scale of 10 right now, I’d say my pain’s five or six, and at night it feels like a seven or eight because I’m alone with it in bed at night. It’s manageable, but over time, it sure does weigh you down, sure does make you feel like, ‘Another day of this?’
Recently, my feet really hurt all the time, the bones in my feet, and I found a podiatrist who’s really been helping me. We think it’s chemo related, but I love my chemo because it’s doing the right things for me.
Cancer is really beautiful in its clarity.
Figuring out solutions to side effects
So I’m trying to manage the pain in my feet I wear sneakers. I wear clodhopper sneakers. I’m the CEO. I dress nicely to work, but I wear orthopedic sneakers with dress clothes and it embarrasses me a little bit. I don’t love it, but I have to make adaptations to to get through my day. The real thing is you just make these accommodations so that life is easier.
I don’t wear mascara anymore. I never liked it, but now I don’t want to be bothered with sticky eyelashes because I have so many other things that bother me and not wearing mascara. Seems like a really dumb thing, right? It has given me quality because just little things like that, you just choose.
Protecting your space
This notion of boundaries or having a friend that you say this is enough. Cancer is really beautiful in its clarity. A terminal diagnosis is awful and wonderful. I mean, it’s awful because there’s an end. We’re all going to die, right? You know, there’s an end, but it’s wonderful because you get to be part of your end. You get to be part of how that how you lead into your ending.
I’m not dying by any means. I am living and I intend to live until I die. But knowing that my life is likely going to be shorter than it should have been or would have been, whatever that means, lets me choose better today. It lets me be in it differently today.
I’m kinder than I ever was. I see things that I didn’t see. I see stars, I smell crispness in the air that I didn’t know before, and there’s a beauty in every single person I meet that I didn’t have before because I feel like film was lifted off of my eyeballs in the clarity of a terminal diagnosis.
It’s that Garth Brooks ‘Live Like You Were Dying’ song. It sounds so trivial, but man. It’s so real to feel and smell and taste things just so fully. It’s a gift every day.

Inspired by Mary's story?
Share your story, too!
MPNs Specialist Conversations
Your MPN, Your Journey: How New Discoveries Will Impact Personalized Care
Dr. John Mascarenhas of The Tisch Cancer Institute at Mount Sinai and patient advocate Andrew Schorr share the latest breakthroughs in MPN care.
Srdan Verstovsek, MD, PhD
Role: Director, Clinical Research Center for MPNs at MD Anderson; Section Chief, MPNs; Prof., Dept. of Leukemia
Focus: Myeloproliferative neoplasms (MPN)
Institution: MD Anderson
Myelofibrosis Highlights from ASH 2022
Dr. Serge Verstovsek and Dr. Naveen Pemmaraju discuss cutting-edge treatments and therapies, and combination therapy as a focus in treating myelofibrosis.
Clinical Trials and You: How to Navigate Treatment?
Patient advocate Ruth Fein Revell, experts Dr. Angela Fleischman and Dr. Ruben Mesa, together with clinical trial nurse Melissa Melendez delve into the cutting-edge realm of myelofibrosis clinical trials.



6 replies on “Mary’s Myelofibrosis Story”
Mary,
Your story really helped me in many ways. I was diagnosed with Primary Myelofibrosis in March 2022. Had Bone Marrow biopsy, not being treated yet but every three months of bloodwork – you just don’t know. I have a deep dive bloodwork in 2 weeks. You are strong!!!!!!!! I am 63, in really good physical condition, but I have some symptoms….they seem to come and go. Right now I am just waiting to talk to my separate specialists in the coming month. I may get back to you…..you get it with this cancer, you really get it. Thanks so much. I just get down when it comes time for the bloodwork. I am stage 2 of 4? I know you said 3 stages…..I have literature from MPN and I am a faithful follower. Any advice????????? Thanks Tom……my wife Maria and I would appreciate if we could contact you to chat someday. God Bless You!
I am very moved by the truthfulness and the strength in Mary’s story. I have PV, then MF for 15 years. It is a continuing learning and struggling experience thru these years. Learn to understand the disease, appreciate life, and grateful that I am still here with the love and support of family, friends, doctors and online patient group’s.
Beautiful story. I get what you are saying as my husband has secondary myleofibrosis. He had polycythemia Vera for a few years and we always knew it would progress to MF. He has a super attitude about it but he is declining. He has chemo and takes an oral med daily. The last few weeks have been pretty tough on him. Hard for an active person to be reduced to extreme fatigue and all the rest of the complications of MF. Strong family with good support so we are lucky. He worries more about me and our daughters. Guess I just wanted to see how other people deal with it. Your story was enlightening to me and truly hope you are dealing with this crap you have been dealt.
Mary – Donn and I watched all of your story and were so moved by all you have gone through and your life insights. Thank you so much for sharing it. You are truly inspirational. We both wish you all the very best.
OMG Mary. Thank you for this, which will be helpful to everyone whose doctors talk baby talk to them. To me.
Thanks for sharing your story Mary.