Hope and Health: Luna’s Experience With Stage 4 ROS1+ Non-Small Cell Lung Cancer
Luna, a retired genetic counselor, was diagnosed with stage 4 lung cancer (non-small cell adenocarcinoma of the lung, ROS1+) in December 2012 at age 54, despite having no lung symptoms before diagnosis. She shares her story of discovery, her reaction to hearing that she had cancer, and the steps she and her medical team took afterwards.
Interviewed by: Taylor Scheib
Edited by: Chris Sanchez
The diagnosis was unexpected, as Luna had been active and healthy, with no risk factors for lung cancer. Her initial reaction was shock, but she subsequently maintained a practical approach, focusing on treatment options.

Luna underwent traditional chemotherapy and later got tested for the EGFR and ALK genetic mutations, for which she turned out to be negative. However, her doctors discovered that she had the ROS1 mutation. She was then given a targeted oral chemotherapy medicine that eventually stabilized her stage 4 lung cancer.
Luna finds hope and positivity crucial in managing her health, establishing a strong support system, and encouraging biomarker testing for comprehensive treatment plans. She emphasizes the importance of a positive attitude, a balanced lifestyle, and gratitude. Luna wishes to raise awareness about lung cancer, especially among non-smokers, and supports broader screening programs.
- Name:
- Luna O.
- Age at Diagnosis:
- 54
- Diagnosis:
- Non-Small Cell Lung Cancer (Adenocarcinoma of the Lung)
- Mutation:
- ROS1+
- Staging:
- Stage 4
- Symptom:
- None involving the lungs; severe abdominal pain
- Treatments:
- Chemotherapy
- Targeted therapy

We would like to thank The White Ribbon Project for its partnership.
This interview has been edited for clarity and length. This is not medical advice. Please consult with your healthcare provider to make treatment decisions.
- Introduction
- Before My Diagnosis
- My Stage 4 Lung Cancer Diagnosis
- How I Reacted
- Liver Biopsy
- My Treatments and Further Testing
- Hope is a Part of My Vocabulary
- It’s Crucial to Have a Positive Attitude
- My Identity Has Shifted Due to My Stage 4 Lung Cancer Experience
- What I Want People to Know About Lung Cancer
So much of it is an attitude of gratefulness. I feel gratitude every single day, and that feeling keeps me going for tomorrow.
Luna, Non-Small Cell Lung Cancer Patient
Introduction
I was diagnosed in December 2012 at the age of 54 with stage 4 lung cancer. I had a small lung tumor, but my liver was loaded, and it had seeded many of my bones.
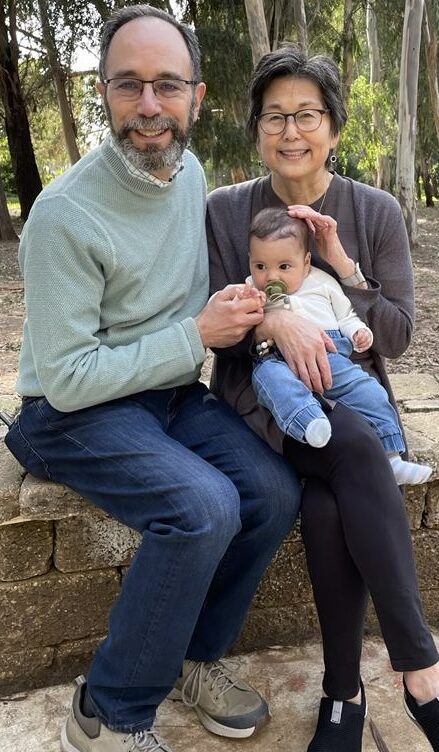
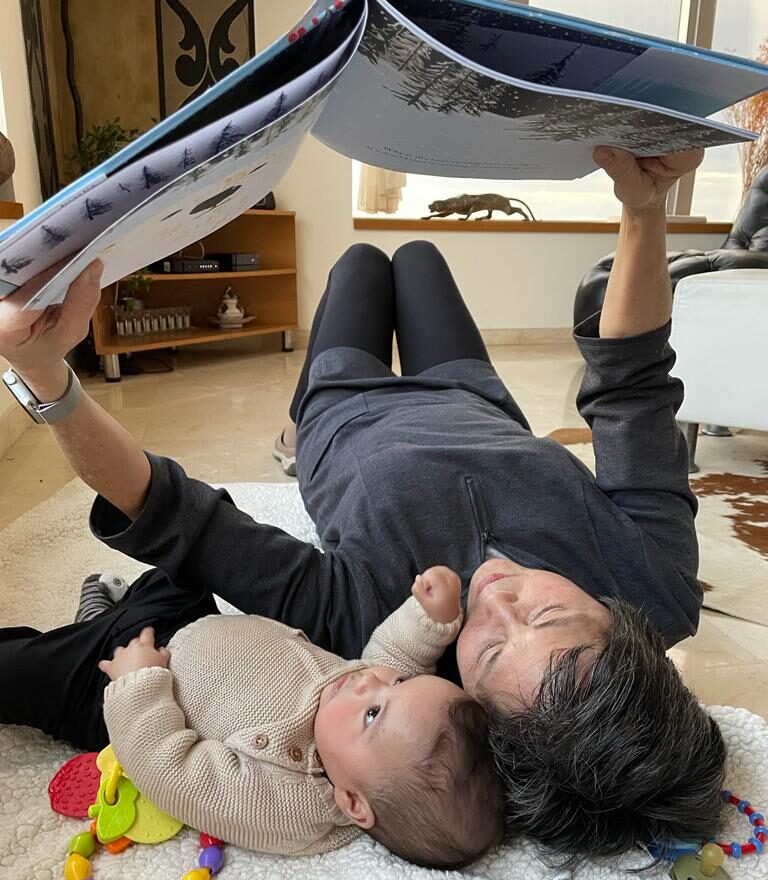
My husband is a pediatrician. We’ve been married for 38 years. We have two adult children, Nathan and Nina, and two grandsons, Nori and Kai. I used to be a genetic counselor and worked in pediatrics, prenatal genetics, and public health genetics. In 2024, I retired after 41 years of genetic counseling.
I’m grateful because I have such an incredible village of friends and family who’ve supported me not only after my cancer diagnosis but also pretty much throughout my life.

Before My Diagnosis
My stage 4 lung cancer diagnosis has a somewhat unusual history. I’ve never had any lung symptoms.
The week before my diagnosis, my family and I traveled to Machu Picchu in Peru. I had been training because I didn’t want to hold my family back. At the time of this trip, I was probably the fittest I had been in 20 years.
Two days after returning from that trip, I began to experience severe abdominal pain. I was convinced it was due to drinking contaminated water during my travels. I had to visit the ER. There, the doctors performed imaging and discovered that I had advanced cancer.
I’m grateful because I have such an incredible village of friends and family who’ve supported me not only after my cancer diagnosis but also pretty much throughout my life.
Luna, Non-Small Cell Lung Cancer Patient
My Stage 4 Lung Cancer Diagnosis
There was a small tumor in my lung. My liver was loaded and most of my bones had tumors in them as well.
We didn’t know how my stage 4 lung cancer started at the time, but I had no symptoms. No shortness of breath, nothing. I did experience some aches when I was training, but I thought they were due to my age and physical activity, so I brushed them off.

How I Reacted
The ER doctor took a long time to get back to my husband and me. I later learned from a friend of ours who works in the ER that this physician was looking at my imaging. He was having trouble coming in to talk to us about the findings.
When he finally did come in, he said, “We found lesions in your lung, liver, and bones. We’d like to admit you so we can figure out where these tumors came from.”
I said, “Time out. Are you telling me that I have cancer?” And he said, “Yes.” He never said the word itself.
I was stunned and couldn’t believe what he said. I was such a low-risk person for lung cancer and had always been such a healthy person. Again, we did not know how it started at the time. So, I was admitted for a couple of days and had lots of blood tests and more imaging.
I had no risk factors. Back then, I didn’t know that people who never smoked could still get lung cancer. I didn’t know enough about cancer itself, even about the stages of cancer. I was in that place of ignorant bliss. We were sitting with our friend who’s a surgeon and my husband was crying. I was so sad and said, “Don’t cry. Maybe this isn’t a big deal.” However, our friend said, “It is a big deal.”
That was good for me to hear. Here I was in this la-la land, thinking I could get over this and that it would go away. I got a pit in my stomach for the first time, but I wasn’t upset. I was grateful that he put it on the line like that for me. I’m a practical person and don’t want to read between the lines, so you don’t have to talk to me with a lot of fluff. Just tell me what’s happening.
I think I cried too because I was making everybody so sad. I think it’s somewhat cultural. My family is Japanese, so we want to know what the next step is with the realization that there is a circle of life and everything proceeds from one step to the next. I had this more practical approach to my stage 4 lung cancer diagnosis.

I was stunned and couldn’t believe what he said. I was such a low-risk person for lung cancer and had always been such a healthy person.
Luna, Non-Small Cell Lung Cancer Patient

Liver Biopsy
The next step was to do a biopsy. In 2012 and early 2013, they had just started testing for tumor markers. At the time, there were only two. Now, there are many more. However, two gene mutations were treatable with oral chemotherapy: EGFR and ALK.
We did a liver biopsy. I was hoping I would be positive for one of the mutations because the thought of having to take a pill a couple of times a day for my stage 4 lung cancer was appealing to me. However, I tested negative for EGFR and ALK. That was in mid-December to the end of December, about two or three weeks later. We had done all this testing, but we hadn’t done anything to fight the cancer.
My Treatments and Further Testing
Chemotherapy
I was getting anxious that my cancer was continuing to progress and I wanted to get something going. When we got the negative biomarker test results, I started traditional chemotherapy, a three-medication regimen.
My insurance hadn’t approved one of the medicines by the time I got to the chemo room. I would have to put it on my credit card. The cost stunned me — $7,800 for one dose. But if my insurance approved it and the practice received payment, I would be reimbursed.


I said, “Why don’t I just wait? I’ll come back and get that third dose when our insurance approves it.” My husband said, “No, no, no, we’re going to put it on the credit card.” But I said no. If worse came to worst, I didn’t want to leave any debt. Eventually, we put it on our card and my insurance ended up reimbursing us.
I had two rounds of that chemotherapy regimen and experienced all the classic side effects. Then when we did follow-up imaging, the doctors found that my stage 4 lung cancer had progressed, so the regimen wasn’t helping me at all. That’s when my doctor suggested that I get tested for this newly described gene mutation: ROS1.
I had no risk factors. Back then, I didn’t know that people who never smoked could still get lung cancer. I didn’t know enough about cancer itself, even about the stages of cancer.
Luna, Non-Small Cell Lung Cancer Patient
ROS1 Testing
ROS1 was new at the time and back then, they thought that it accounted for about 1% of people with adenocarcinoma of the lung. I thought, okay, that means a 99% chance that I won’t have this.
When I tried to get the pre-authorization from my insurance, they declined my request because I had already undergone gene testing for ALK and EGFR. It was going to cost thousands for us out of pocket. Again, my concern was not to leave debt in case things got bad. My husband and oncologist talked me into it. They said, “If you do have it, there’s an oral chemotherapy for it.”
The good news is that I was able to get this biopsy and turned out positive for ROS1.

In the last several years, every oncologist worth his or her weight in gold has been doing biomarker testing.
Luna, Non-Small Cell Lung Cancer Patient

Targeted Therapy and Successful Treatment
We wrangled with our insurance company and eventually got them to agree to cover my new medication, a targeted chemotherapy medicine. I’ve been on it for almost 12 years now and it’s controlling my stage 4 lung cancer. I ended up responding well to the medication and am among a handful of people who are getting long-duration on this oral chemotherapy.
There’s a bit of a backstory to it. Initially, the lab report came back saying that I was ROS1-positive. That was when we started scrambling. My doctor split the sample and sent it to another laboratory and the people there got back to us and said I was not ROS1-positive after all.
My oncologist called the director of the laboratory that conducted the test. They ran the test again and published a report saying that I was positive after all and that there had been a lab error. Once I got that reassurance from two separate labs that I had this mutation, I felt very confident.
The good news for me was that once I started taking this oral chemotherapy, I had tumor shrinkage. All my other biomarker tests went down within normal limits within a few weeks.
Currently, there are some side effects that I must manage, but I’m alive and my stage 4 lung cancer has been stable for going on 12 years. I’ve been lucky. I’ve had a bad disease that I’ve managed with good medicine and a lot of luck.
In the last several years, every oncologist worth his or her weight in gold has been doing biomarker testing. When I was first diagnosed, some oncologists were hesitant about it because they were waiting to see if it panned out. I get that because there were a lot of testing things that didn’t pan out in cancer, but this one was real.
At that time, when I was talking to fellow patients, I would urge them to get a young oncologist, someone who had training in their fellowship with genetics. Now, I don’t feel the need to say that because almost all oncologists will test for it.

There are a lot of people who have asked me, ‘Do you ever wonder: why you?’ I flip that a little bit and say, ‘Why not me?’
Luna, Non-Small Cell Lung Cancer Patient

Hope is a Part of My Vocabulary
Throughout my experience, I kept repeating this mantra: “I need a little more time.”
I felt that way because my kids were just being launched. They were in their early 20s and I felt like they were adults already, but I needed to let them know a few more things before I could check out and know that they were going to be okay. I did whatever I could to get a little more time with them.
Hope was wrapped up in all of that, but I also became very type A about my medications, vitamins, and exercise. I worked toward that mind, body, spirit triad, and its balance. That need for balance was my hope for my future.
It’s Crucial to Have a Positive Attitude
My recommendation for those facing stage 4 lung cancer and other cancer patients is to have a positive attitude.
When I started living longer than my “expiration date,” I wanted to be the healthiest-looking sick person I know. I planned to eat right, get enough sleep, and exercise every day. What happened to me when I got this new attitude was that I almost transformed. I felt much more positive about life, that I was not going to die of cancer, and that maybe I should get mammograms and restart my statin because I could die of something else.
So much of it is an attitude of gratefulness. I feel gratitude every single day and that feeling keeps me going for tomorrow. It is a positive way of looking toward the future.

The only risk factor I have for lung cancer is that I have lungs.
Luna, Non-Small Cell Lung Cancer Patient
My Identity Has Shifted Due to My Stage 4 Lung Cancer Experience
When I’m by myself, other than making sure I take my medications at the right time of the day, I don’t think about being a cancer patient. There are a lot of organizational things I must do, like scheduling CT scans and MRIs and taking care of my insurance. Those tasks eat up a fair amount of my week.
But do I identify as a cancer patient? I guess I do because when someone tells me they have cancer, especially if it is lung cancer, it automatically establishes a connection. I want to get to know them and their story as well. I guess when I think about it, I do identify as a cancer patient, specifically a lung cancer patient.
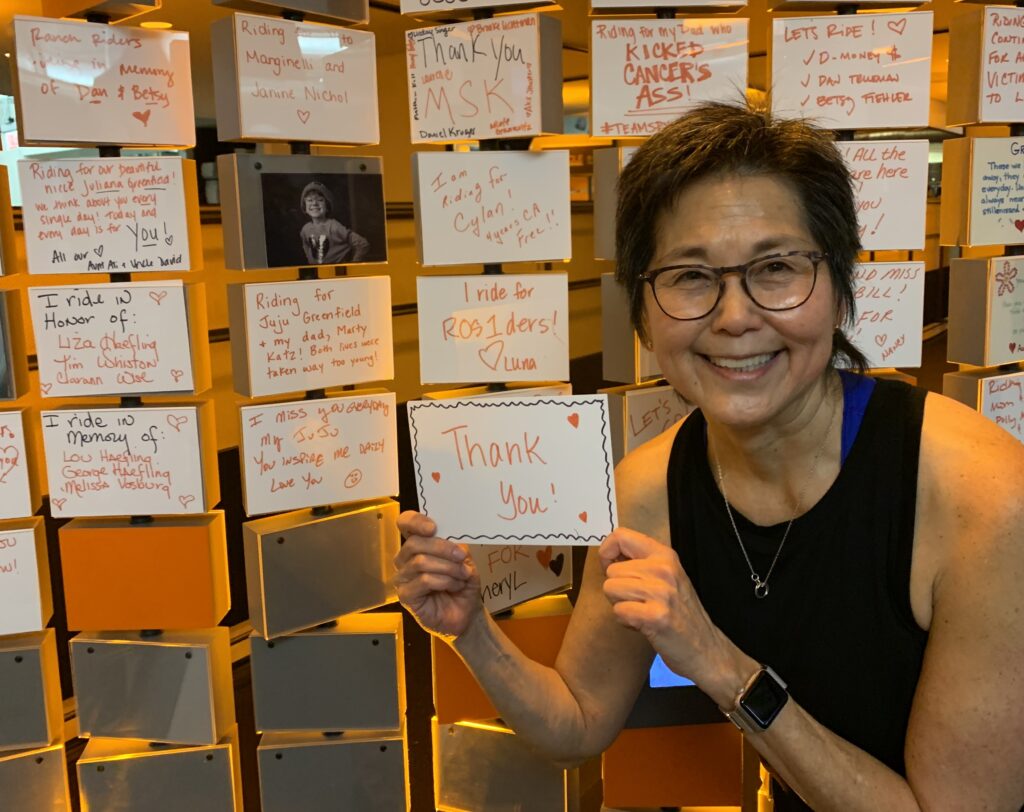
Moreover, when someone tells me that they are a ROS1 lung cancer patient, they get a hug. I joined a Facebook group called The ROS1ders. We are a small group because only 1% to 2% of individuals with lung cancer have a ROS1 mutation. In August, about 50 of us met in Colorado. We shared stories and contact information so that we could be in touch with each other.
Lung cancer can happen to anybody.
Luna, Non-Small Cell Lung Cancer Patient
There are a lot of people who have asked me, “Do you ever wonder: why you?” I flip that a little bit and say, “Why not me?” I feel that I’m human and vulnerable to disease, a very practical person, and a realist in terms of everybody eventually dying of something, so I never took it personally.
It’s better for me because I think there’s so much stigma surrounding smokers. Even if I were a smoker, I still wouldn’t deserve to have lung cancer. Some of my nurses have asked me, “Do you smoke?” My response is, “No, why do you ask?”
I try to educate them that roughly 40% of us have never smoked and the only risk factor I have for having lung cancer is that I have lungs. I don’t know why I have it. There’s an uptick in Asian women who have lung cancer. Maybe it has something to do with our pollution and that kind of thing, but there’s no single thing that I can put my finger on, so why not me?


What I Want People to Know About Lung Cancer
Lung cancer can happen to anybody.
I’m very supportive of screening programs. The current screening criteria are very narrow. You must have smoked for many years and be over 50. But if you’re concerned, if you have a family history, or if you qualify for screening, have testing done because lung cancer is a very treatable condition in its early stages.
Don’t just brush off any symptoms you might have. Seek medical care, take things in stride, and be brave and strong.


Inspired by Luna's story?
Share your story, too!
More Stories with The White Ribbon Project
Luna O., Non-Small Cell Lung Cancer, ROS1+, Stage 4 (Metastatic)
Symptom: None involving the lungs; severe abdominal pain
Treatments: Chemotherapy, targeted therapy
Calvin M., Lung Cancer, Stage 1
Symptoms: Frequent illness (monthly cycles of sickness), breathing difficulties
Treatment: Surgery (pneumonectomy)
Jill F., Lung Cancer, EGFR+, Stage 1A
Symptom: Nodule found during periodic scan
Treatments: Surgery, targeted therapy, radiation
Additional Cancer Stories
Stephanie K., Non-Small Cell Lung Cancer, ALK+, Stage 4 (Metastatic)
Symptoms: Persistent and intense cough, general feeling of sluggishness
Treatments: Chemotherapy, targeted therapy through a clinical trial, radiation therapy
...
Jennifer M., Lung Cancer, EGFR+, Stage 4 (Metastatic)
Symptoms: None per se; discovered during physical checkup for what seemed to be a sinus infection
Treatments: Radiation therapy (stereotactic body radiation therapy or SBRT), targeted therapy
...
Laura R., Non-Small Cell Lung Cancer, ALK+, Stage 4 (Metastatic)
Symptoms: Persistent cough, fatigue, bone pain
Treatments: Targeted therapies (tyrosine kinase inhibitors or TKIs, including through a clinical trial)
...
Ashley C., Non-Small Cell Lung Cancer, HER2+, Stage 4 (Metastatic)
Symptoms: Fatigue, breathlessness, persistent back pain, multiple rounds of bronchitis
Treatments: Chemotherapy, targeted therapy
...
Loryn F., Non-Small Cell Lung Cancer, HER2+, Stage 4 (Metastatic)
Symptoms: Extreme fatigue, persistent back pain, chest pain, joint pain in the feet, hips, legs, shoulders, and elbows
Treatments: Chemotherapy, radiation therapy (foot and elbow to help with mobility), antibody-drug conjugate
...
Clara C., Lung Cancer, MSH6, Stage 4 (Metastatic)
Symptoms: Pelvic pain, joint and bone pain, breast lump, extreme lightheadedness and dizziness, vomiting, fainting spells, swollen lymph node in the neck, neuropathy, headaches, unexplained weight loss, severe anemia
Treatments: Radiation therapy to the brain, chemotherapy, immunotherapy
...








