Humor, Gratitude, and Community: How Jennifer Deals with Stage 4 EGFR+ Lung Cancer
Jennifer, a Boston-area resident and mother of teenagers, received a life-changing diagnosis of stage 4 EGFR-positive lung cancer when she was 48. Her cancer was discovered by accident when she had scans for what she thought was a sinus infection. Her story underscores the unpredictability of lung cancer and highlights the fact that “anyone with lungs” can be affected, regardless of age or lifestyle.
Interviewed by: Keshia Rice
Edited by: Chris Sanchez
Jennifer’s EGFR-positive lung cancer experience did not just revolve around treatment but extended deeply into her family life, emotional processing, and the impact of COVID-19 isolation. The timing forced her to navigate cancer and uncertainty while the world also faced a pandemic. She credits finding the lung cancer community, including organizations like Lungevity, GO2 Foundation, and Lung Strong, with helping her truly realize that she was not alone. These connections provided the strength and resources needed to cope and ultimately thrive, despite ongoing challenges.

Her EGFR-positive lung cancer story is one of transformation. Once blindsided by the diagnosis, Jennifer became an educator and advocate, breaking down lung cancer stigma and advancing awareness that this disease is not just a smoker’s cancer. Through advocacy work, joy in everyday moments, and humor, even when facing “scanxiety,” treatment side effects, and painful losses, Jennifer centers gratitude as her guiding force.
Above all, Jennifer emphasizes the importance of research, community, and personalized medicine made possible through biomarker testing. She calls for universal screening, increased research funding, and better support for families and children of patients. Through initiatives like the White Ribbon Project and her own creative projects, she honors the stories of everyone affected and encourages newly diagnosed patients to “find their community” and remember, “You are not alone.”
Jennifer’s video and interview transcript provide more detail about how:
- Lung cancer can affect anyone with lungs, regardless of age, gender, or smoking history
- Humor and gratitude are sustaining forces during treatment and ongoing care
- Connecting with others through advocacy and community provides strength and reduces isolation
- Biomarker and genetic testing are opening doors for targeted therapies and more hopeful outcomes
- Every patient’s experience can be transformed by finding meaning and connection
- Name: Jennifer M.
- Age of Diagnosis:
- 48
- Diagnosis:
- Non-Small Cell Lung Cancer (NSCLC)
- Staging:
- Stage 4
- Mutation:
- EGFR
- Symptoms:
- None per se; discovered during a physical checkup for what seemed to be a sinus infection
- Treatments:
- Radiation therapy: stereotactic body radiation therapy (SBRT)
- Targeted therapy
This interview has been edited for clarity and length. This is not medical advice. Please consult with your healthcare provider to make informed treatment decisions.
The views and opinions expressed in this interview do not necessarily reflect those of The Patient Story.
- My name is Jennifer
- The accidental discovery that I had cancer
- My reaction to my diagnosis
- How I processed a devastating diagnosis
- Why young women getting lung cancer is so surprising
- Addressing stigma in lung cancer
- Stressing about family risk, screening, and guidelines
- I balance motherhood and my terminal diagnosis
- Gratitude, progress in research, and grief for friends
- Living day to day: managing and thriving
- Advocacy and the White Ribbon Project
- Scrapbooking and seeing the world through a new lens
- What I want newly diagnosed patients to know
My name is Jennifer
I live north of Boston in Massachusetts. I was diagnosed with stage 4 adenocarcinoma, non-small cell lung cancer, at the age of 48. That was in January 2020, so I am excited that I am still here after more than five and a half years of being given a terminal diagnosis. The biomarker testing that was done revealed that I have an EGFR genomic mutation, which allows me to take a targeted medication every day.
I went to college for photography. Right out of college, I went into ophthalmic photography, working in a hospital setting as a technician and ophthalmic photographer. Photography has been a passion of mine, and being in the medical field is part of who I am.
I have a very positive outlook on life. Before diagnosis, I was always very much aware of the beauty in the natural world and was just a happy, happy person. I enjoy being with my family and friends, and I love stand-up comedy. I think that comedy is one of the things that has helped me on this journey I am on now, dealing with stage four lung cancer. I think it is important to still have humor, and it has helped me through this.
I just love comedy. I do not do stand-up, and I wish I did. I try to laugh every day. I have always been goofy, and that has served me well on this journey I am on now.
The accidental discovery that I had cancer
I did not have any signs. My being diagnosed was completely by accident.
I really did not have anything out of the ordinary. I was tired, but I was commuting into Boston to work, and I had two teenage kids. Any kind of fatigue, I just chalked up to my lifestyle, so there really was not anything other than that.
When I went to my primary care doctor for what I thought was a sinus infection, I was sent to get scans, which then showed that I had this big mass in my lung at that point.
My reaction to my diagnosis
Just absolute shock. How could it be lung cancer?
We are a very fit family, very healthy. We have a home gym. I was running 5Ks all the time, always very active. I ate healthily. I thought, “Oh, I do not have to worry about lung cancer.” You do your screening for the other cancer guidelines, and it was not on my radar that I would ever be diagnosed with lung cancer.
Now, being in this space and seeing that there are so many younger people being diagnosed with lung cancer under the age of 50, and predominantly women, it is just wild.
Being in this lung cancer community is a huge gift to me to be a part of the community. I think it is really important because you do not feel so alone. You see that there are so many of us. Unfortunately, we are all in this together, but it was definitely completely blindsiding.
Growing up, you think of the older person who has smoked their whole life and then would end up with lung cancer in their seventh or eighth decade. You do not equate lung cancer with young, otherwise healthy people. Now I am on treatment, and we may look healthy. I am lucky to be on a targeted medication, but there are side effects all the time that come and go, different side effects that we have to deal with.
We may not look sick. I do not look sick, but it is still affecting me. I still have the deadliest cancer.
How I processed a devastating diagnosis
In the beginning, there were a few months of really just being devastated, just being blindsided. It took a while to find the lung cancer community, and that really helped.
Once I found the lung cancer community and saw that I was not alone, we were able to have that support with one another. Without even having to say anything, you just know that these people know what you are dealing with and what you are going through.
To have that is the biggest gift — to be able to find the different organizations. I asked if I could name the organizations or not. To be able to find the LUNGevity organization, the GO2 Foundation for Lung Cancer, the Lung Cancer Research Foundation, and the really wonderful local organization Lung Strong that directly raises funds for Mass General, my local hospital, and Dana-Farber has meant so much. They raise money for research.
I met the amazing woman who ran Lung Strong, Diane Legg. She was like a mentor to me. She unfortunately passed away, but after living decades with lung cancer. She was a true inspiration. Just finding that community is everything. It is absolutely everything.
I had to navigate my diagnosis as COVID shut the world down. It was interesting because part of me was like, “I am miserable. This has turned our lives upside down.” But then I thought, “You know what? Everybody’s lives are upside down right now because COVID is happening.” I feel like everyone was experiencing the same thing. I think I dealt with COVID better. I was kind of okay with it and okay that we were all masking up and being careful, because that is what I wanted to do anyway: to make sure that I did not get sick from COVID or any kind of cold.
Everybody was hunkered down, and I just felt like cocooning too, being handed this diagnosis. It actually worked out well for me, interestingly. We were able to have Zooms so that, once I found the community, that was nice because we could still be together, the lung cancer community, on Zoom. That was a lifeline.
Why young women getting lung cancer is so surprising
I think people have it in their heads that smoking is equal to lung cancer, and they learned that from all the commercials back in the 80s and public campaigns. They do not realize that your lungs are an organ like any other. You can get cancer anywhere.
It can be from genetic mutations. It can be from environmental toxins. They are saying the air quality and the fine particulate matter are contributing to people getting lung cancer younger, particularly the type of cancers we are seeing. There are so many different types of lung cancer, which I do not think people realize, either; different mutations. People just think, “Oh, lung cancer, it is one thing.” Well, there is the ALK mutation, the ROS mutation, the KRAS mutation, and the EGFR mutation, which I have, and which is found to be predominantly in Asian Americans or Asians globally. I think it is important to try to be part of understanding why it is happening in so many people under the age of 50. The GO2 Foundation teamed up with the Bonnie Addario Foundation to do the epidemiology of young lung cancer, and I took part in that, which involved questionnaires and blood samples, to be part of finding out why it is happening.
I think that environmental exposures and the air quality definitely play into it, and I hope they come out and figure out why it is. I feel like it is an epidemic right now for young people, so it needs to be on everybody’s radar, no matter whether they have the risk factors or not. There is also radon, which is another huge cause of lung cancer. They are still trying to figure it out.
Addressing stigma in lung cancer
I have dealt with stigma. Nobody deserves lung cancer — or any cancer — regardless of their smoking history. There are many causes, some known and some still being figured out, especially for those under age 50. I don’t get upset; instead, I use every opportunity to educate — anyone with lungs can get lung cancer.
With fellow survivors, I’ve gone to the Boston Public Library and talked to people about the facts. I became a phone buddy through the GO2 organization and Cancer Hope Network, which has been fulfilling and helpful, both for myself and the people I connect with.
Stressing about family risk, screening, and guidelines
Yes, those are stressful for sure, especially being in this space and having been in this space for over five years now, I definitely want everybody to be tested.
I really think that guidelines need to change and that amazing people are working on that. ALCSI, the American Lung Cancer Screening Initiative, is working hard on that.
It is going to take a while to get there, but I feel like everybody should be screened just like we do colonoscopies or mammograms. I feel that a low-dose CT scan starting at 35; hopefully, we will get there, and the guidelines will change, but it is involved, and it takes a while.
I think if people are having symptoms, I hope that interviews like this will help people advocate for themselves and be able to go to their doctors and, even if they have to pay out of pocket, insist — if they are having certain symptoms — on a low-dose CT scan.
Again, as I said, I did not have any symptoms, and others may not either, but they should still insist on a low-dose CT scan.
I do know there is a study coming out also at Mass General that will be looking at children of people who are diagnosed with lung cancer and seeing about screening them. That is exciting to know that that will be coming out, and perhaps my kids will be able to take part in that study. There are a lot of people working on this.
Because in the lung cancer space, the oncologists and the surgeons and everybody — we are really trying to move that momentum and raise the awareness that anyone with lungs, all of us, can get lung cancer. We are all breathing the air. Again, like the radon or any job-associated exposures, veterans, people who have served in the military are at higher risk, firefighters, different occupations. We need to continue the conversation that your lungs are an organ, and you can get cancer there.
I balance motherhood and my terminal diagnosis
That is the worst part.
I feel like I can handle anything. I am going to keep going, and my reason is to keep going for them. But they are my biggest worry in all this, that mental part. The mental part is the hardest.
You worry because you do not want them to worry. I see that my kids, being older, my son was able to go on Google and look up the statistics and see that the outlook is not good, that the five-year survival rate is dismal. I did not even expect to be here, so that is amazing.
I just try to be really grateful. Being grateful has been the biggest piece for me and for my family.
Gratitude, progress in research, and grief for friends
I try to say, “This is amazing. Research has really taken off in the lung cancer space in the last ten years, especially.”
We have come so far. It is really exciting. It is amazing that I get to be on this targeted medication and that I have been doing well.
The hard part is losing friends in the community, as I have lost so many. They are with me. They are with me in my heart. It is a hard thing because you lose people all the time, and it is devastating, and then you are still here. I am so grateful.
To instill that in my kids and my husband, it has really helped him, too. Now he is like, “We are grateful for the time that we have had, absolutely grateful.” To put that spin on it is everything.
We try to look at it like that, always being grateful. Grateful for the time we have had and grateful for the research that is continuing to happen.
Cancer always finds a way around whatever treatment you are throwing at it. It is a wily coyote. It will find its way around, unfortunately. But to be grateful, to have that as your driving force, is everything.
Lung cancer is the deadliest cancer, but it receives the least federal funding, which is crazy. Recently, funding for several cancers, including lung and pancreatic cancer, was cut significantly. That’s upsetting, and it’s pushed our community to advocate — we’ve gone to Capitol Hill and met with Senators to share our stories and the importance of continuing to fund research. It’s essential that funding increases for lung cancer, and meeting with state representatives is huge; the cancer community is unified in this effort.
Living day to day: managing and thriving
It’s challenging; everything changes and evolves. Five years in, I’m different than I was two years into the journey. I try to focus on the first step, not the whole staircase; staying in the moment and not looking too far ahead.
I used to constantly research options for when my current therapy stops working, but I’ve learned to stop delving into that and instead stay present.
It’s hard not to plan far in advance, especially when friends talk about exciting plans. I circle back to food and supplements: initially, I cut out all sugar for about eight months, but there’s no evidence that sugar affects lung cancer, and my oncologists have told me that. Now, I enjoy my dark chocolate and ice cream, and I’m still here.
I stick to what my doctors recommend and focus on exercise as much as I’m able. Movement of any kind is important.
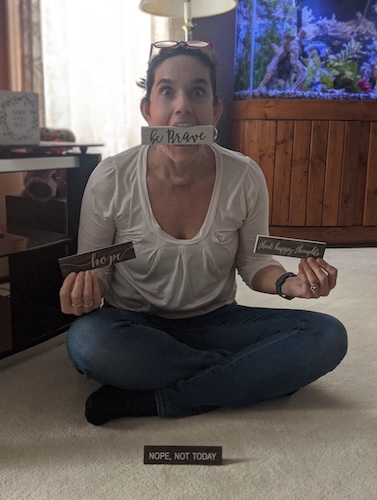
Advocacy and the White Ribbon Project
My shirt says “Got Lungs? Then you can get lung cancer.”
The white ribbons behind me are from the White Ribbon Project, an amazing grassroots organization started by Heidi and Pierre when she was diagnosed with lung cancer and wanted a big white ribbon. They mail wooden white ribbons to survivors and caregivers, which helps us start conversations and share that anyone with lungs can get lung cancer.
Wearing and sharing these ribbons brings people together.
Scrapbooking and seeing the world through a new lens
Making a scrapbook has helped me. It’s filled with positive notes to myself, articles about other survivors, and records of events and the people I’ve met. It celebrates survivorship and honors those we’ve lost. Every person and every story is important, and this is my way to remember and honor my lung cancer community.
People say they’re grateful to be diagnosed because it changes how they view life and the world, and it’s true. I was always positive and a photographer who noticed beauty, but this experience pushed it to another level.
I am even more grateful and awestruck by life and the world. I appreciate every interaction and am grateful for our community and this opportunity to talk. Every connection matters.
What I want newly diagnosed patients to know
You are not alone. All the organizations I mentioned have built a powerful community, and that is our greatest strength.
There is a lot of hope right now with more research than ever before. You can choose your level of involvement, whether being active or just reading posts — you’ll still feel supported.
Find the community; you are not alone, and that’s the biggest message I would share.

Inspired by Jennifer's story?
Share your story, too!
More EGFR+ Lung Cancer Stories
Jennifer M., Lung Cancer, EGFR+, Stage 4 (Metastatic)
Symptoms: None per se; discovered during physical checkup for what seemed to be a sinus infection
Treatments: Radiation therapy (stereotactic body radiation therapy or SBRT), targeted therapy
Samantha V., Lung Cancer, EGFR+, Stage 2, Grade 3
Symptoms: Breathlessness, hoarseness, sinus infections, fatigue, pain in left side
Treatments: Clinical trial (targeted therapy)
Natasha L., Lung Cancer, EGFR+, Stage 4
Symptoms: Hoarse voice, squeaky breathing, cough, weight loss, fatigue
Treatment: Targeted therapy
Jeff S., Lung Cancer, EGFR+, Stage 4 (Metastatic)
Symptom: Slight cough
Treatments: Surgery, radiation, chemotherapy, targeted therapy
Jill F., Lung Cancer, EGFR+, Stage 1A
Symptom: Nodule found during periodic scan
Treatments: Surgery, targeted therapy, radiation